Copyright
©The Author(s) 2023.
World J Gastrointest Surg. Oct 27, 2023; 15(10): 2123-2132
Published online Oct 27, 2023. doi: 10.4240/wjgs.v15.i10.2123
Published online Oct 27, 2023. doi: 10.4240/wjgs.v15.i10.2123
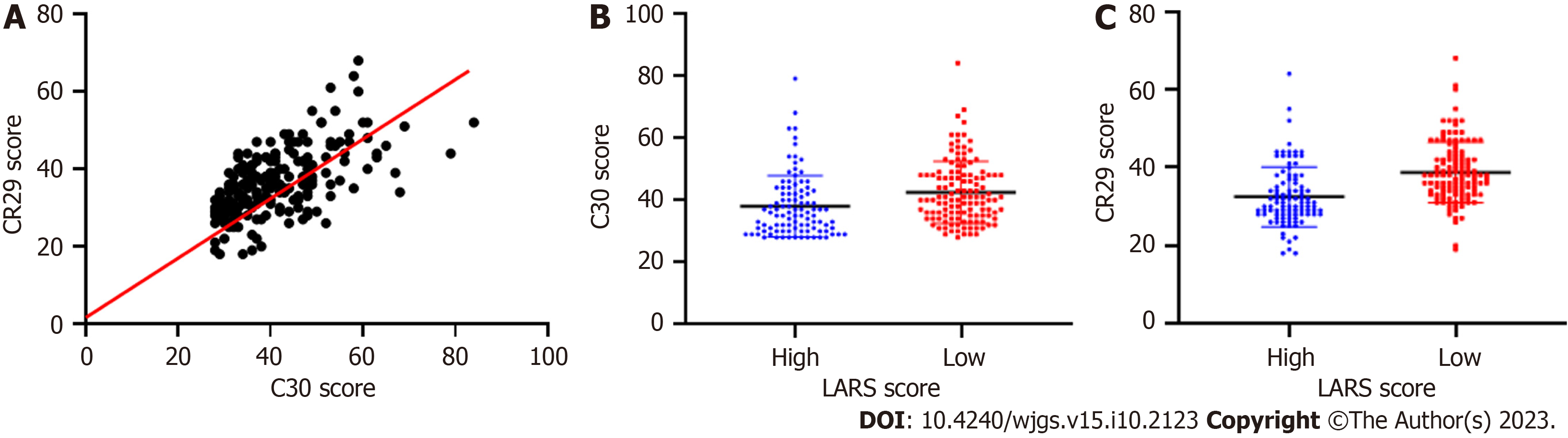
Figure 1 Relationship between low anterior resection syndrome scores and postoperative quality of life.
A: Scatterplot showing good consistency between the Quality of Life Questionnaire (QLQ)-C30 and QLQ-CR29 quality of life scores; B: Patients in the low low anterior resection syndrome (LARS) score group had lower QLQ-C30 scores, fewer symptoms affecting quality of life, and better quality of life (P < 0.05); C: Patients in the low LARS score group had lower QLQ-CR29 scores, fewer symptoms affecting quality of life, and better quality of life (P < 0.05). LARS: Low anterior resection syndrome.
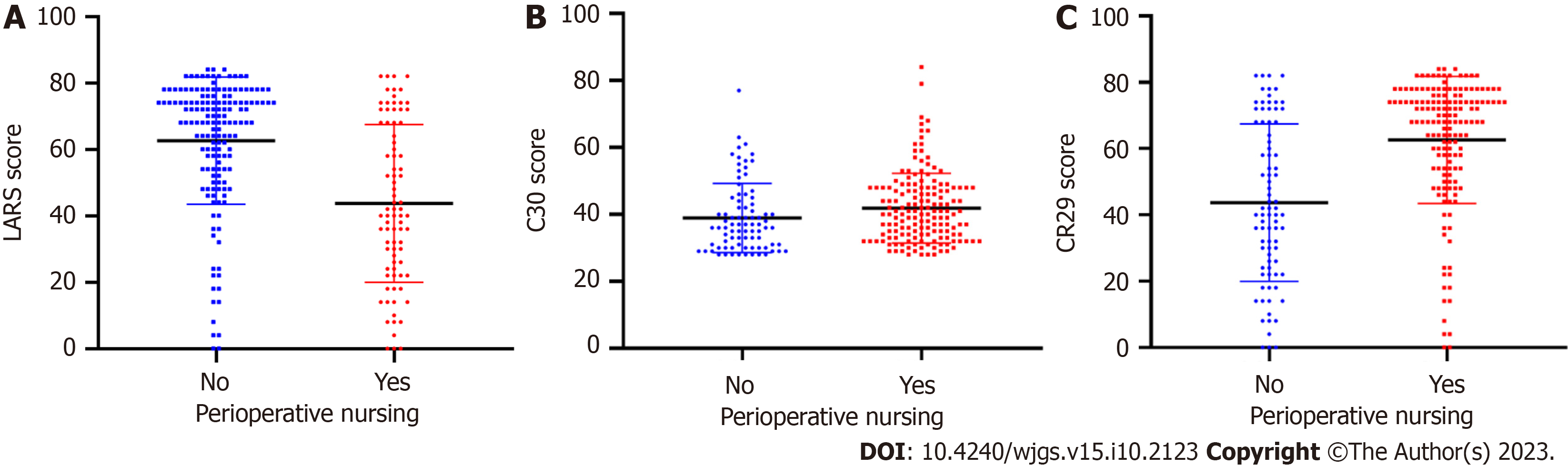
Figure 2 Relationship between perioperative precision nursing and postoperative quality of life.
A-C: Patients provided with perioperative precision nursing had (A) significantly lower low anterior resection syndrome scores (LARS) after surgery and a reduced probability of developing LARS (P < 0.05), (B) higher postoperative Quality of Life Questionnaire (QLQ)-C30 scores (P < 0.05), and (C) higher postoperative QLQ-CR29 scores (P < 0.05). LARS: Low anterior resection syndrome.
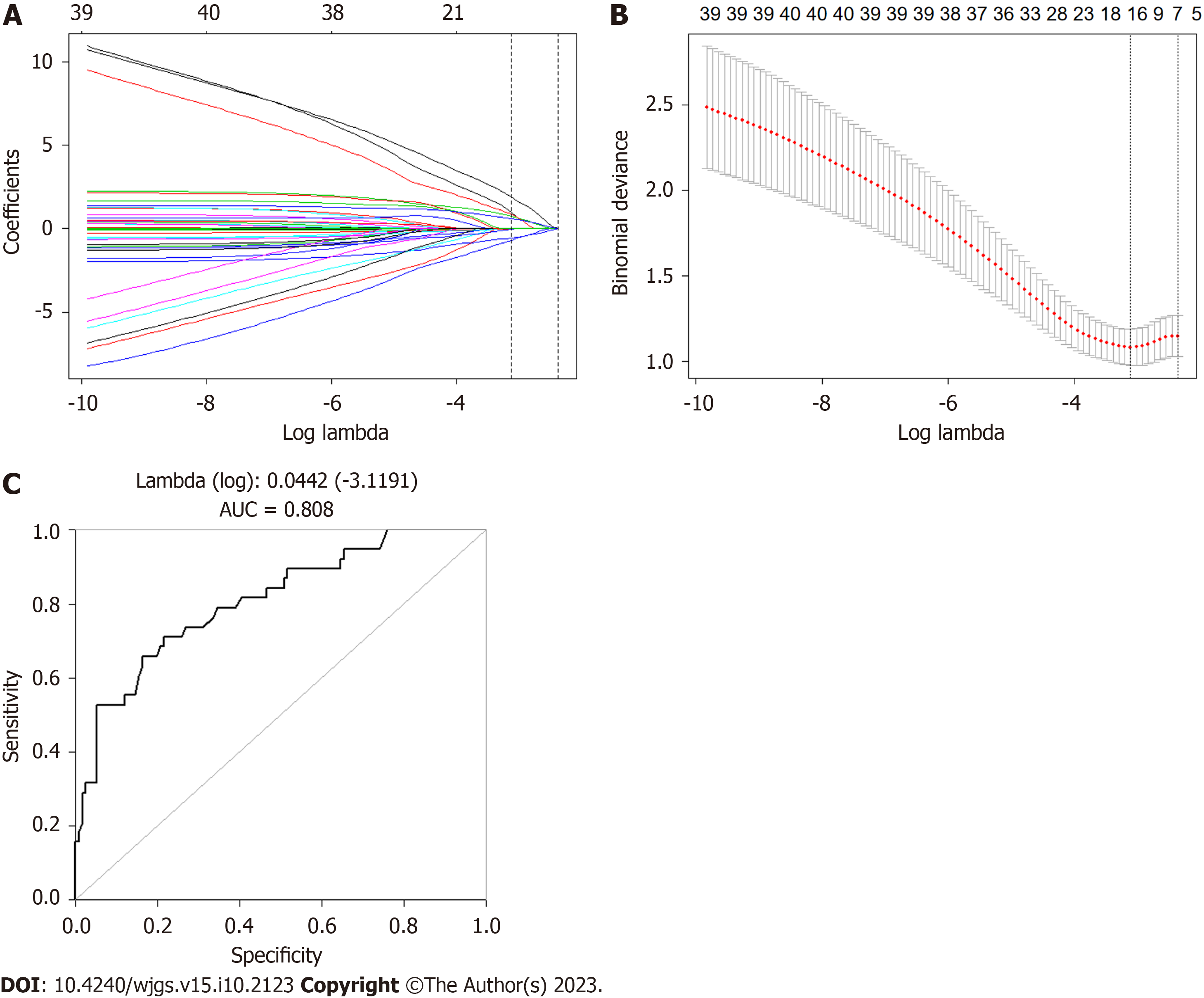
Figure 3 Low anterior resection syndrome prediction model established by least absolute shrinkage and selection operator regression.
A and B: Total/partial mesorectal excision, ostomy, preoperative radiotherapy, and neoadjuvant chemotherapy were identified as risk factors for low anterior resection syndrome (LARS) and were used to establish an LARS prediction model; C: The accuracy of the LARS prediction model reached over 80%. AUC: Area Under Curve.
- Citation: Jin DA, Gu FP, Meng TL, Zhang XX. Effect of low anterior resection syndrome on quality of life in colorectal cancer patients: A retrospective observational study. World J Gastrointest Surg 2023; 15(10): 2123-2132
- URL: https://www.wjgnet.com/1948-9366/full/v15/i10/2123.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i10.2123