Copyright
©The Author(s) 2021.
World J Gastrointest Surg. May 27, 2021; 13(5): 476-492
Published online May 27, 2021. doi: 10.4240/wjgs.v13.i5.476
Published online May 27, 2021. doi: 10.4240/wjgs.v13.i5.476
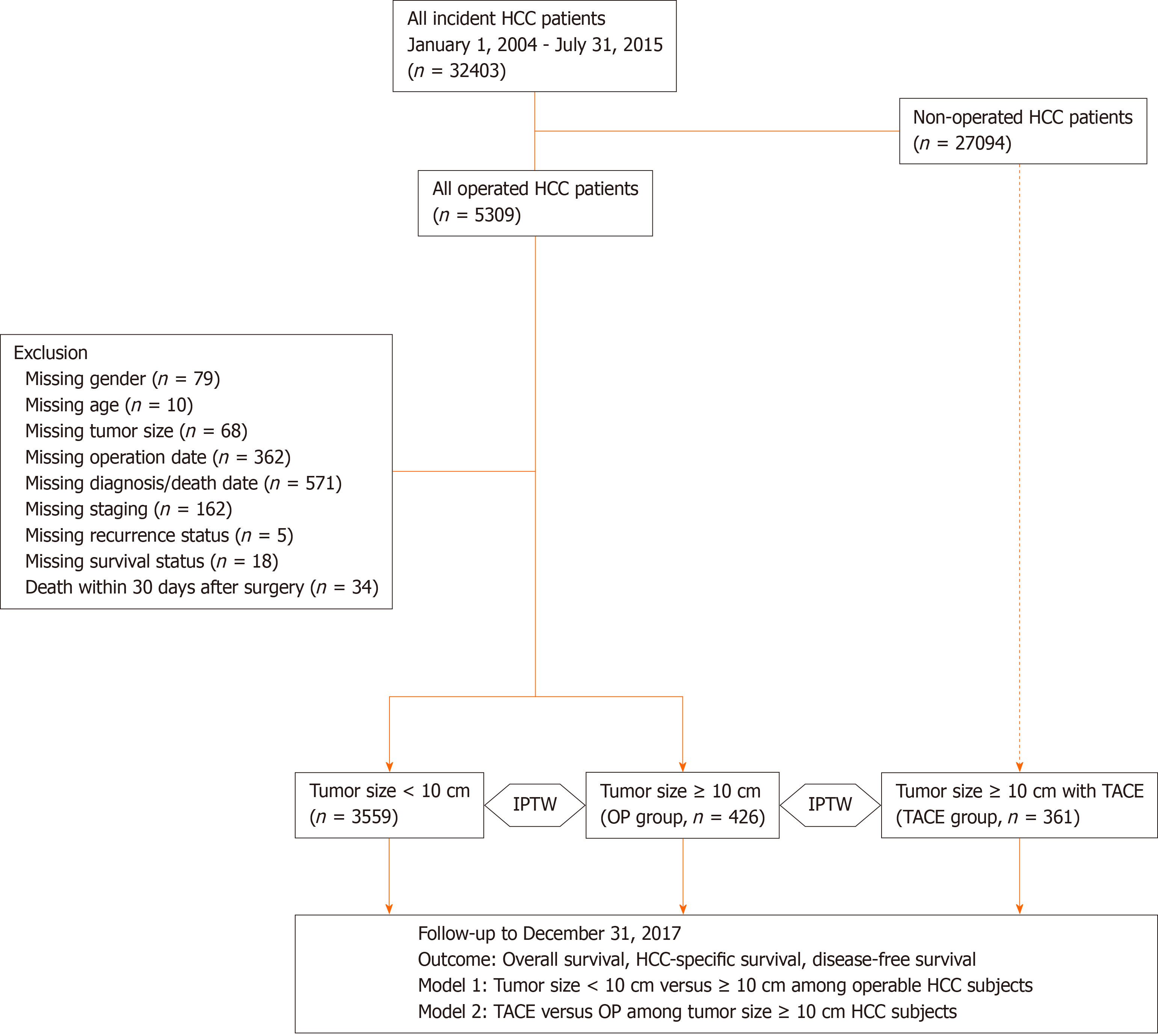
Figure 1 Flow diagram of the current study.
Hepatocellular carcinoma (HCC) patients diagnosed from January 2004 to July 2015 were retrieved from the Chang Gung Research Database (CGRD; n = 32403). Two models were designed for analysis: model 1, patients with HCC ≥ 10 cm (L-HCC; 426 patients) or HCC < 10 cm (S-HCC; 3559 patients) receiving liver resection; model 2, patients with HCC ≥ 10 cm receiving either liver resection or transarterial chemoembolization (TACE; 361 patients) as the primary treatment. The primary outcome was overall survival (OS), while HCC-specific survival and disease-free survival (DFS) were the secondary outcomes.
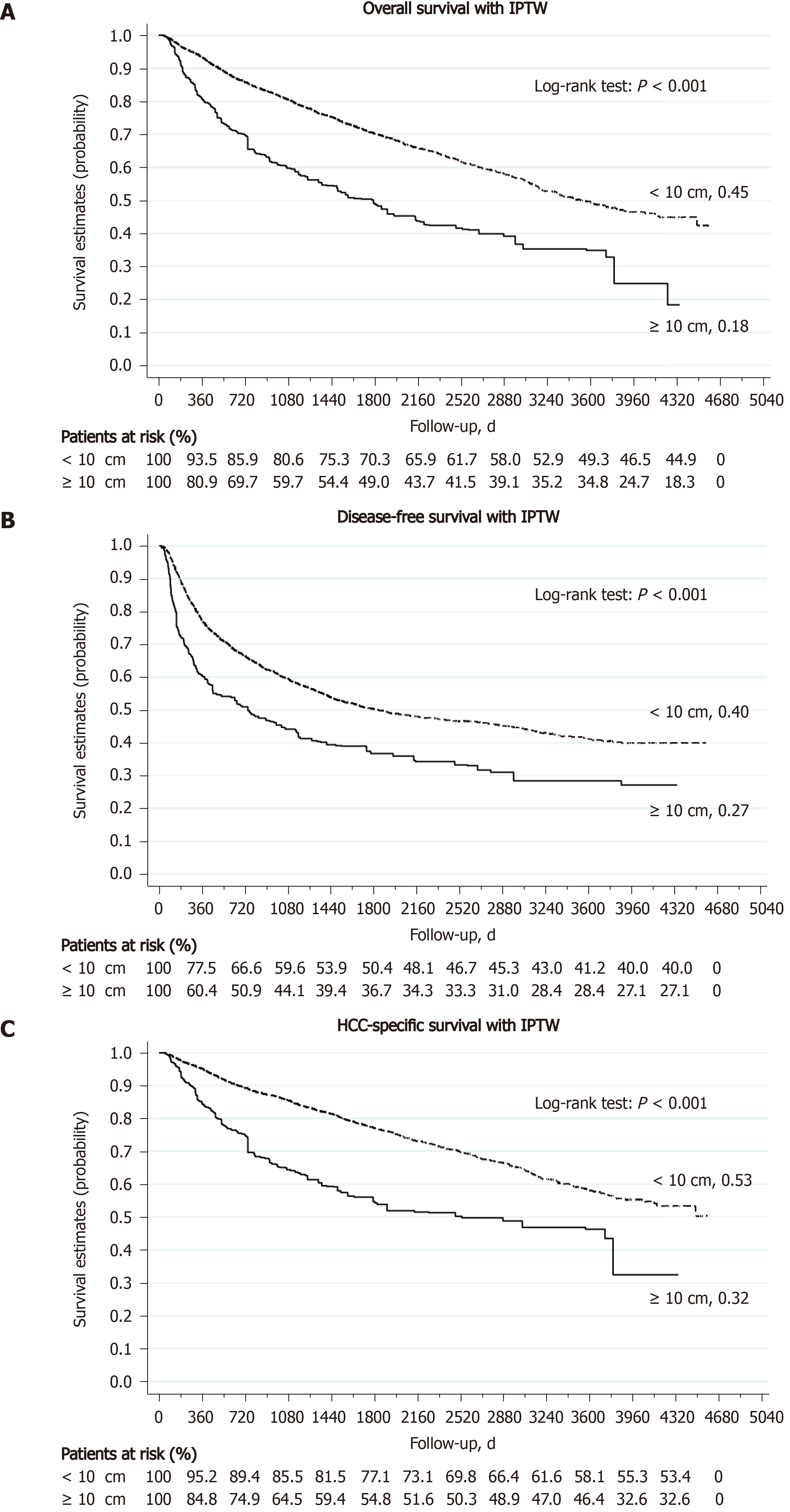
Figure 2 Hepatocellular carcinoma ≥ 10 cm patients had worse outcome than Hepatocellular carcinoma < 10 cm patients after surgery.
A: Overall survival; B: Disease-free survival; C: Hepatocellular carcinoma (HCC)-specific survival. Estimated with inverse-probability of treatment weighting (IPTW).
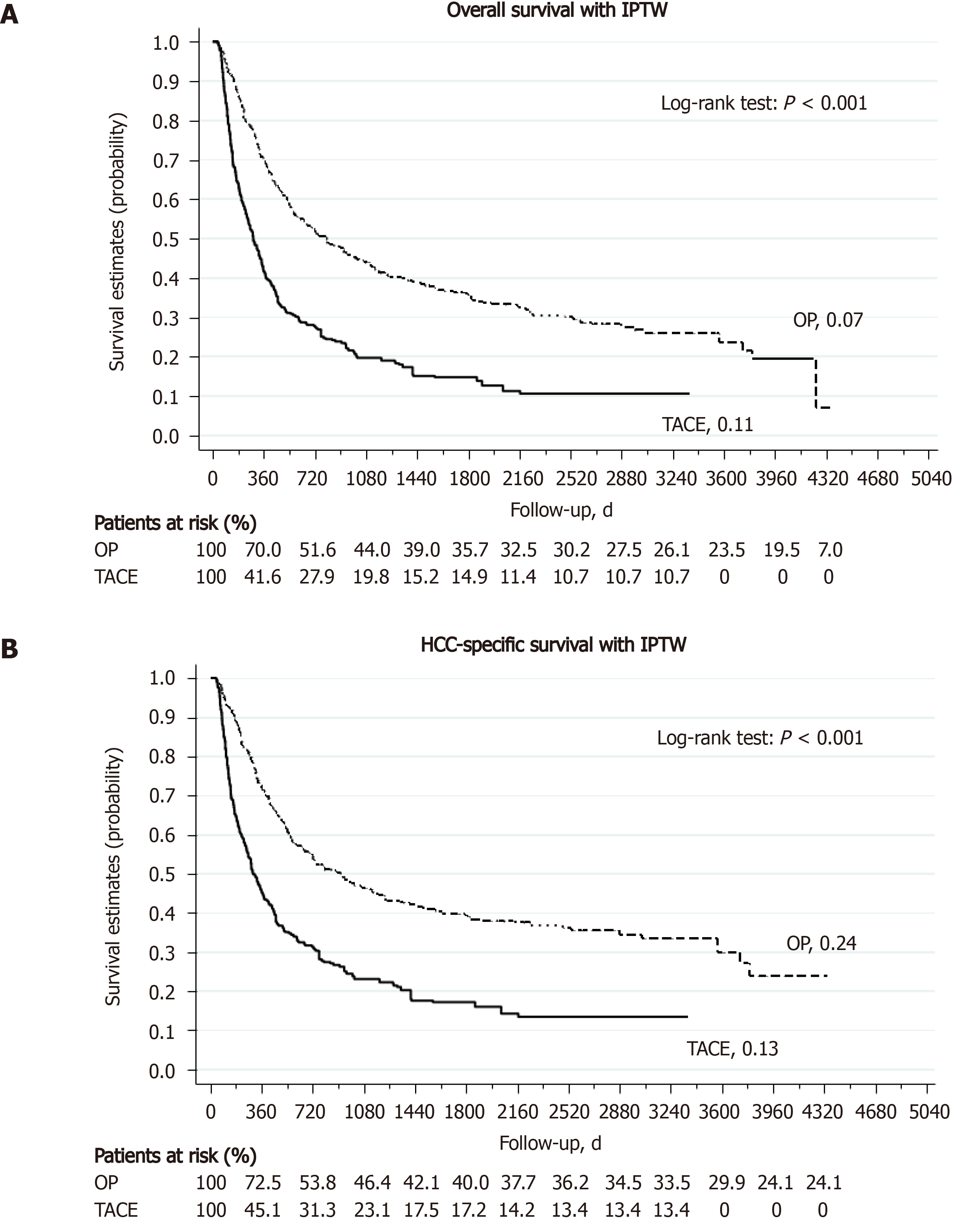
Figure 3 Liver resection, when comparing to transarterial chemoembolization, can provide a better long-term outcome for selected hepatocellular carcinoma ≥ 10 cm.
A: Overall survival; B: Hepatocellular carcinoma (HCC)-specific survival. Estimated with inverse-probability of treatment weighting (IPTW). TACE: Transarterial chemoembolization.
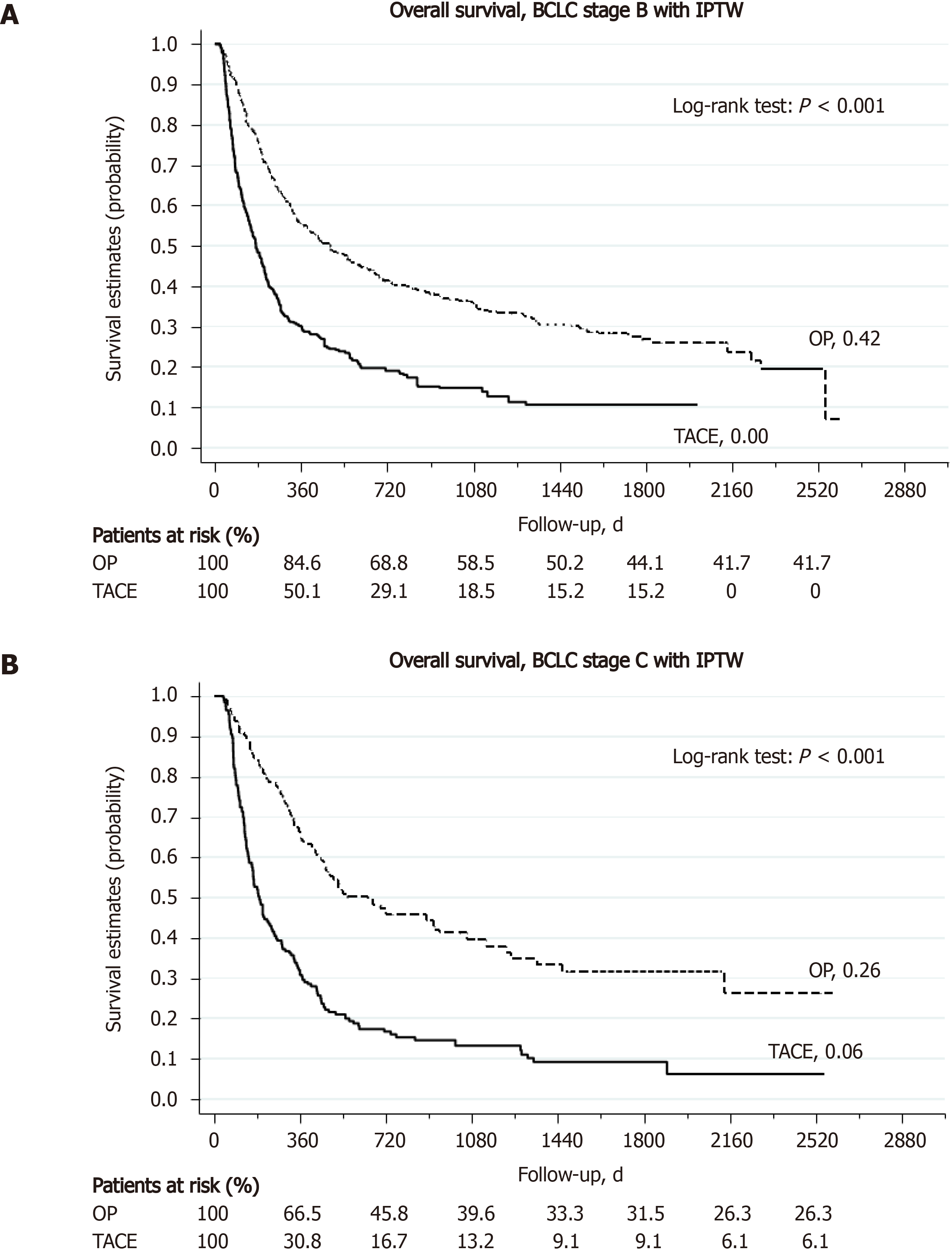
Figure 4 Liver resection is better than transarterial chemoembolization for selected Barcelona Clinic Liver Cancer stage B and Barcelona Clinic Liver Cancer stage C hepatocellular carcinoma ≥ 10 cm patients.
A: Overall survival; B: Hepatocellular carcinoma-specific survival. Estimated with inverse-probability of treatment weighting (IPTW). BCLC: Barcelona Clinic Liver Cancer; TACE: Transarterial chemoembolization.
- Citation: Lee CW, Yu MC, Wang CC, Lee WC, Tsai HI, Kuan FC, Chen CW, Hsieh YC, Chen HY. Liver resection for hepatocellular carcinoma larger than 10 cm: A multi-institution long-term observational study. World J Gastrointest Surg 2021; 13(5): 476-492
- URL: https://www.wjgnet.com/1948-9366/full/v13/i5/476.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v13.i5.476