Copyright
©The Author(s) 2021.
World J Gastrointest Surg. Dec 27, 2021; 13(12): 1567-1583
Published online Dec 27, 2021. doi: 10.4240/wjgs.v13.i12.1567
Published online Dec 27, 2021. doi: 10.4240/wjgs.v13.i12.1567
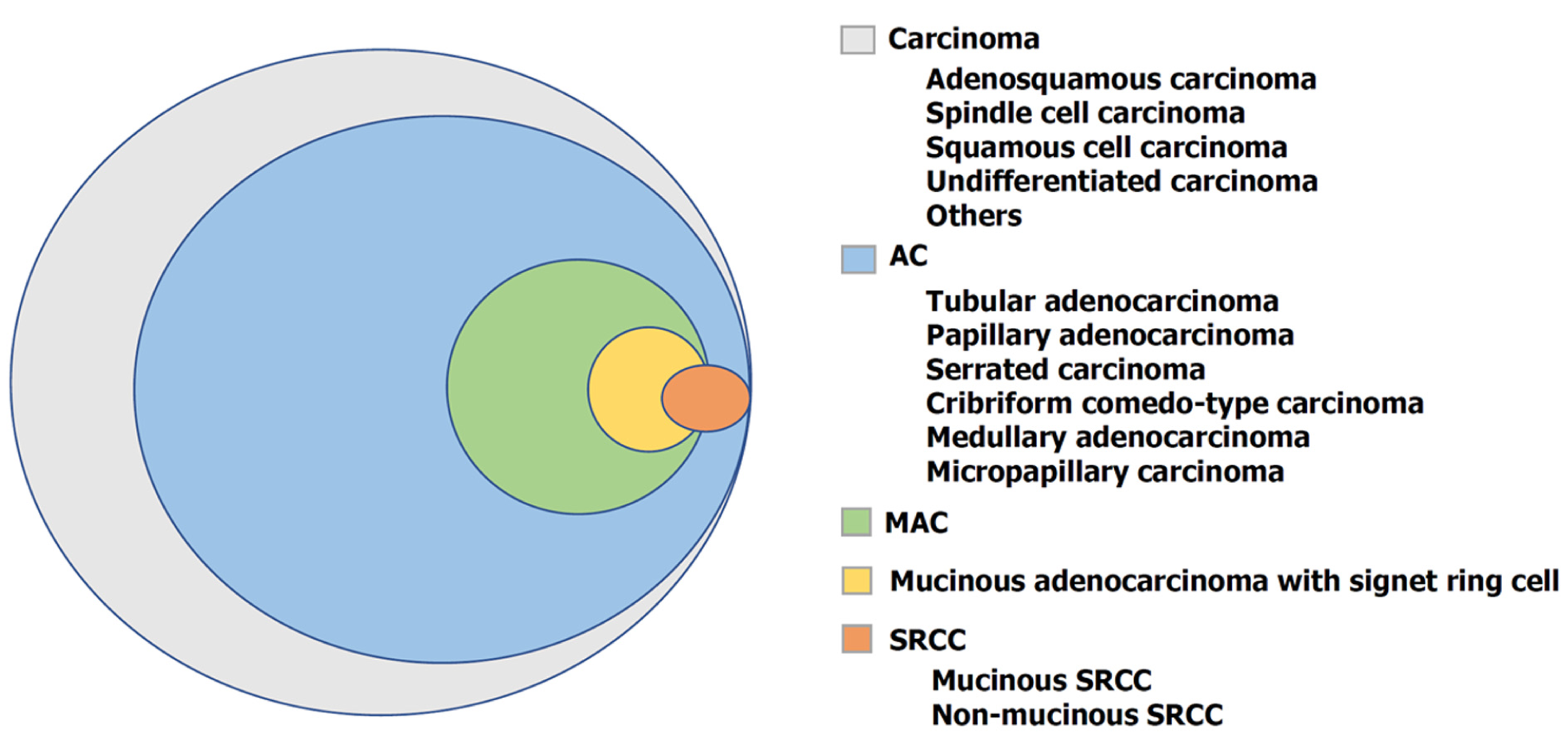
Figure 1 World Health Organization histological classification of colorectal carcinoma.
AC: Adenocarcinoma; MAC: Mucinous adenocarcinoma; SRCC: Signet ring cell carcinoma.
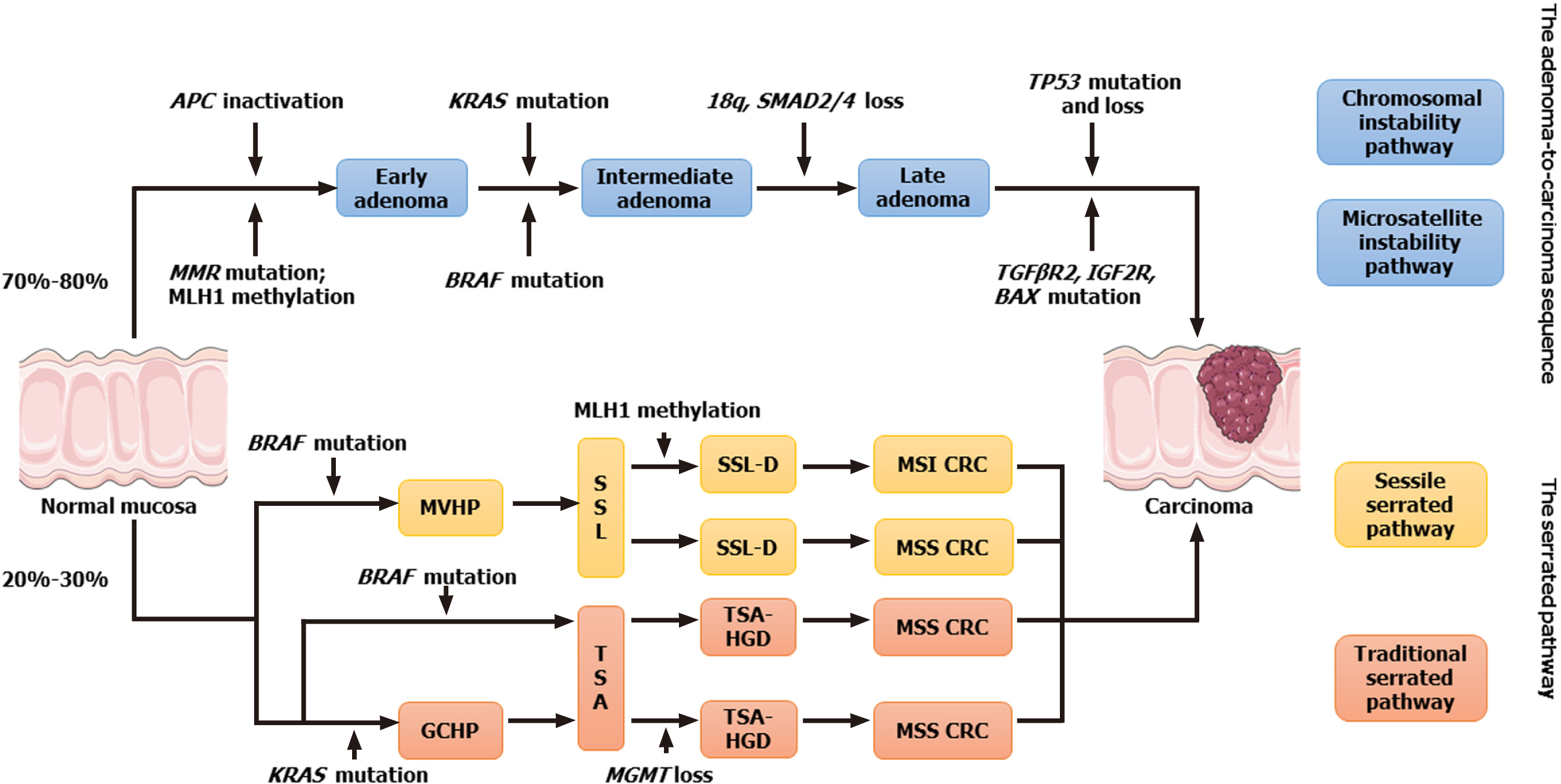
Figure 2 Main pathways for the occurrence of colorectal cancer and the genetic and epigenetic features involved in the development of colorectal cancer.
CRC: Colorectal cancer; MMR: Mismatch repair; MVHP: Microvesicular hyperplasic polyp; SSL: Sessile serrated lesion; SSL-D: Sessile serrated lesion with dysplasia; MSI: Microsatellite instability; MSS: Microsatellite stability; GCHP: Goblet cell-rich hyperplastic polyp; TSA: Traditional serrated adenoma; TSA-HGD: Traditional serrated adenoma with high-grade dysplasia.
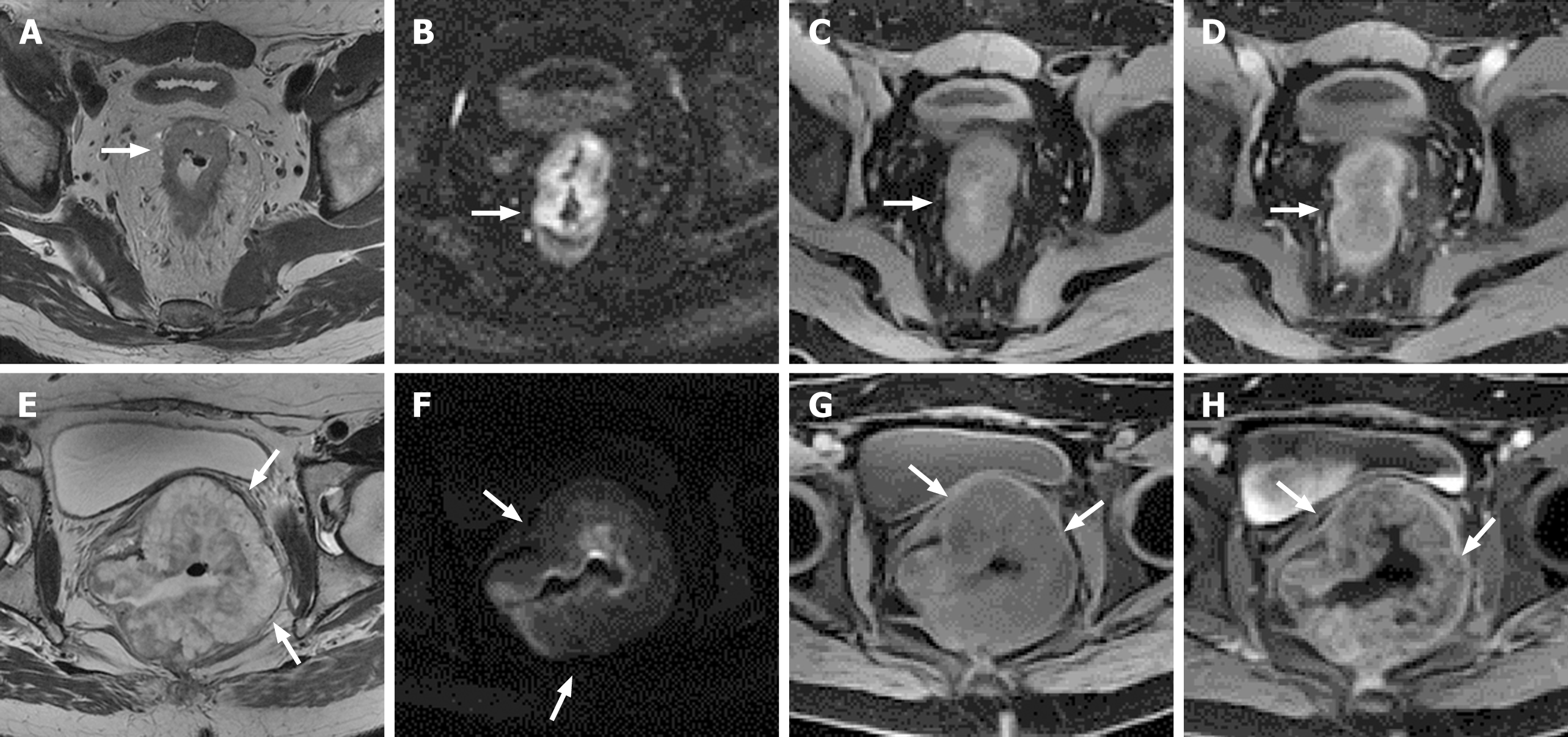
Figure 3 Magnetic resonance imaging of rectal adenocarcinoma and mucinous adenocarcinoma.
A-D: Rectal adenocarcinoma; E-H: Rectal mucinous adenocarcinoma. A: Axial non-lipid-suppressing T2-weighted imaging (T2WI) showing irregular circumferential thickening of the rectal wall, with slightly higher T2WI signal, lower than that of fat; B: Diffusion-weighted imaging (DWI) showing that the lesion was high signal; C: Low signal on plain T1-weighted imaging (T1WI); D: Axial enhanced T1WI showing moderate to high enhancement of the tumor; E: Axial non-lipid-suppressive T2WI showing that the rectal wall was thickened approximately three quarters of the circumference, and the left side wall was mainly with high signal on T2WI, which was close to the fat T2 high signal, with a low signal interlaced distribution; F: DWI showing that the lesion was mainly high signal; G: Low signal on plain T1WI; H: Axial enhanced T1WI showing enhanced tumor margins and low internal enhancement.
- Citation: Huang A, Yang Y, Shi JY, Li YK, Xu JX, Cheng Y, Gu J. Mucinous adenocarcinoma: A unique clinicopathological subtype in colorectal cancer. World J Gastrointest Surg 2021; 13(12): 1567-1583
- URL: https://www.wjgnet.com/1948-9366/full/v13/i12/1567.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v13.i12.1567