Copyright
©The Author(s) 2021.
World J Gastrointest Surg. Oct 27, 2021; 13(10): 1285-1292
Published online Oct 27, 2021. doi: 10.4240/wjgs.v13.i10.1285
Published online Oct 27, 2021. doi: 10.4240/wjgs.v13.i10.1285
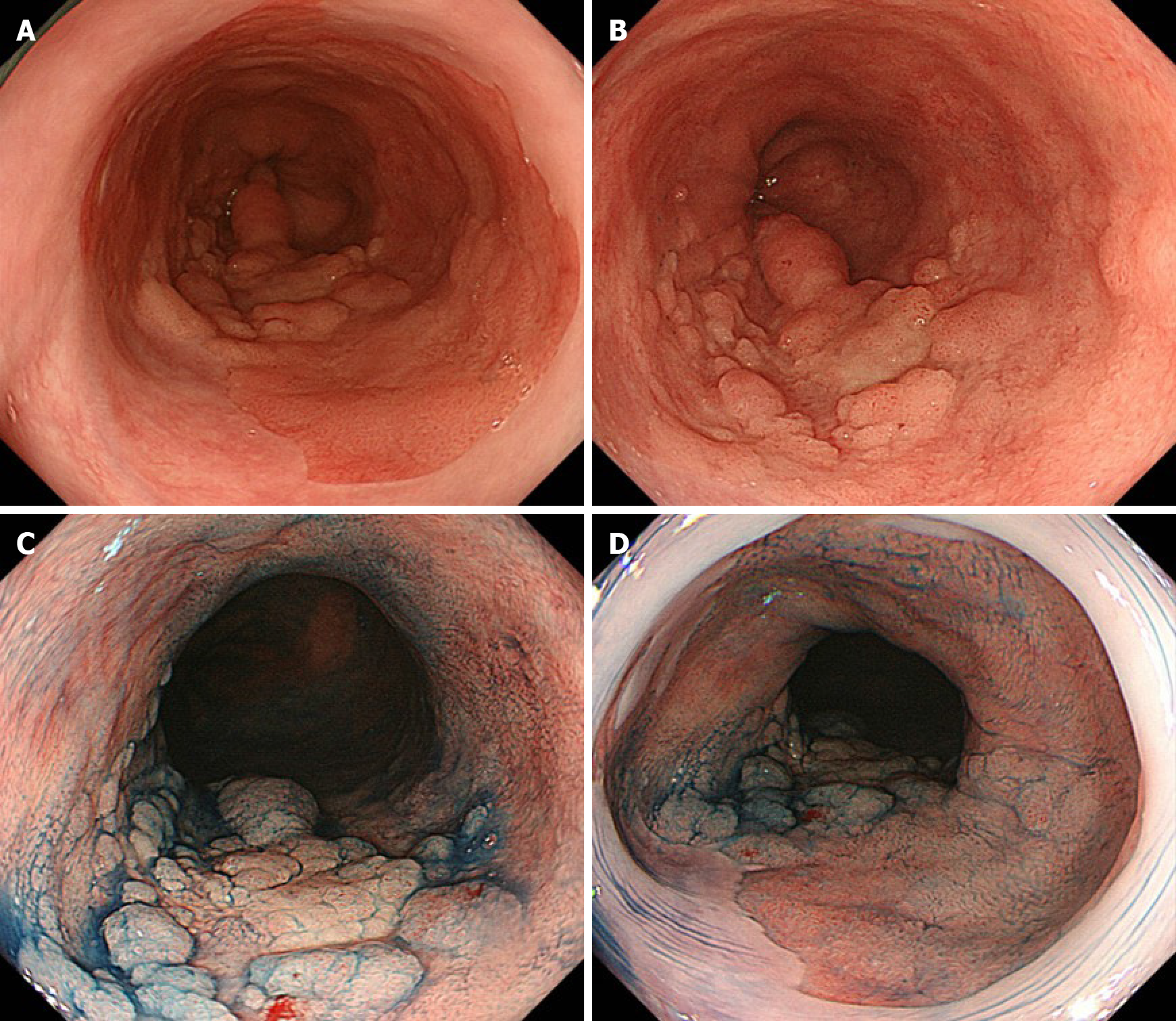
Figure 1 Images of esophagogastroduodenoscopy.
A and B: Conventional white-light endoscopy shows a nodular aggregated protruded lesion in the long-segment Barrett’s esophagus (C 3.5 M 4); C and D: Chromoendoscopy with indigo carmine shows the protruded lesion with irregularly sized granules. No obvious lesion was found in the mucosal surface of Barrett's esophagus other than the nodular aggregated protruded lesion.
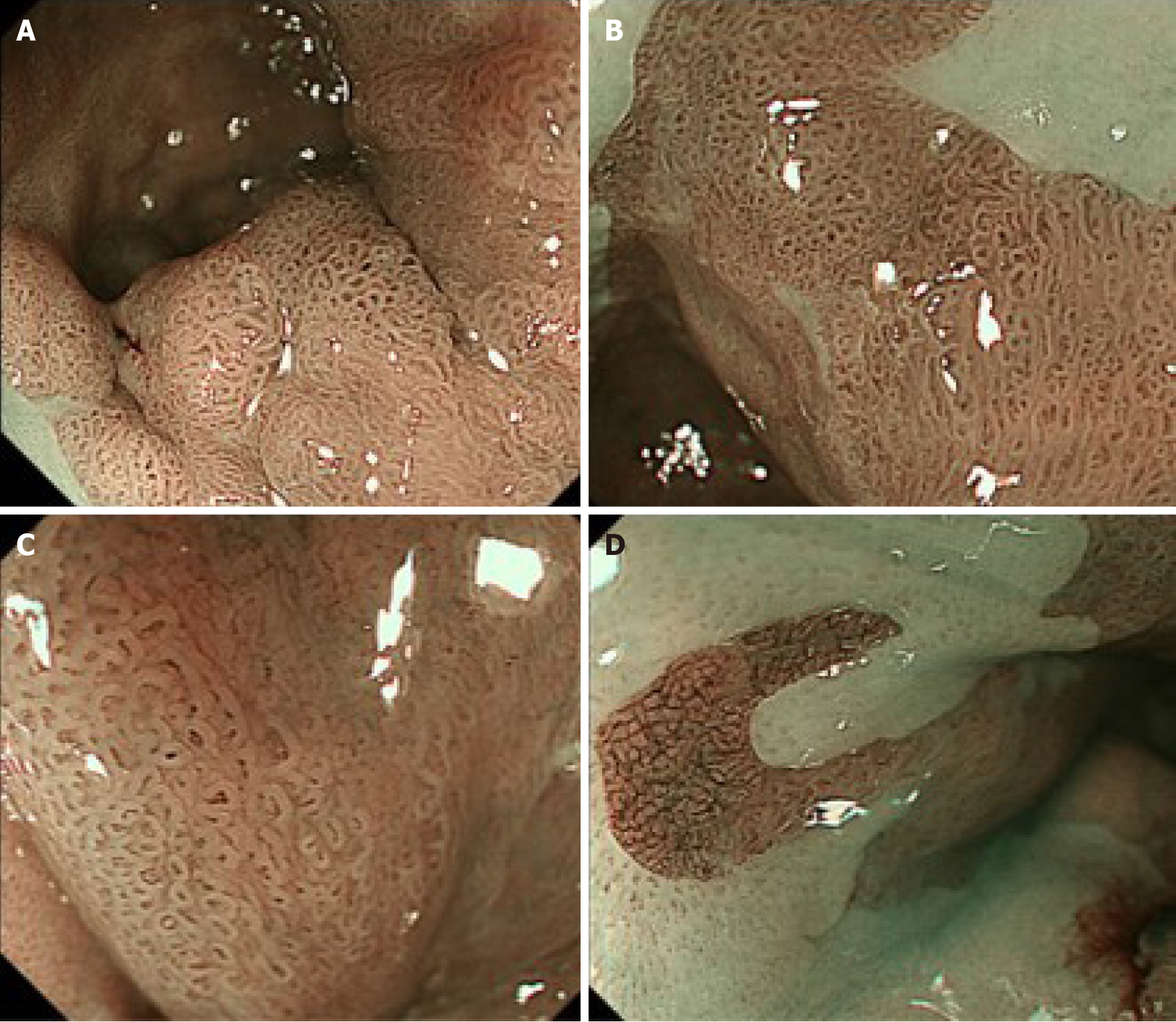
Figure 2 Images of narrow-band imaging magnification endoscopy.
A: Narrow-band imaging magnification endoscopy (NBI-M) shows a visible mucosal pattern with villous structures in protruded or elevated portions, as well as in the surrounding flat portions in the long-segment Barrett’s esophagus (LSBE); B: The villous patterns were rated as irregular because they showed variety in size and existed in a high density; C: In most of surrounding areas of the LSBE, mucosal patterns showed an irregular villous pattern [similar to the image (C)], and vascular patterns were rated as irregular because they showed a variety of forms and calibers under NBI-M observation with high magnification; D: In several flat areas, NBI-M demonstrated an invisible mucosal pattern with an irregular vascular pattern forming a network-like structure with a variety in caliber.
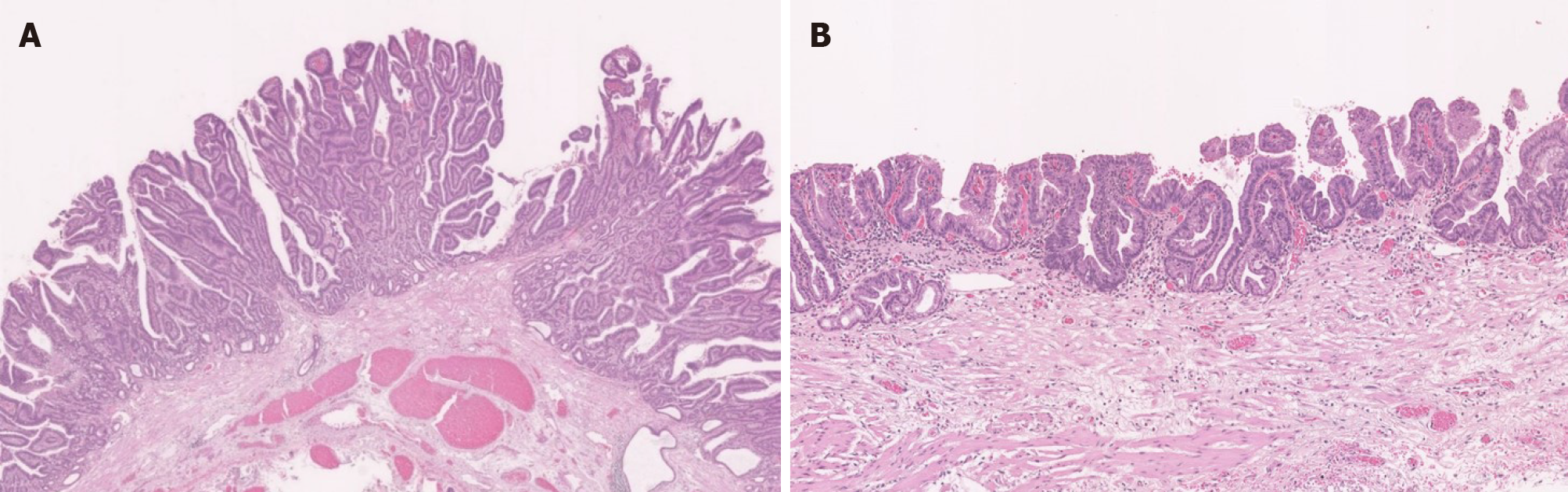
Figure 3 Pathological findings.
A: Papillary adenocarcinoma with cancerous crypts exhibiting papillary proliferation accompanied by structural atypia was observed in the protruded and elevated positions (magnification: 1.5 ×); B: Well-differentiated tubular adenocarcinoma with short papillary glands accompanied by structural atypia and nuclear enlargement was extensively observed in the extensive flat portions (magnification: 2.0 ×).
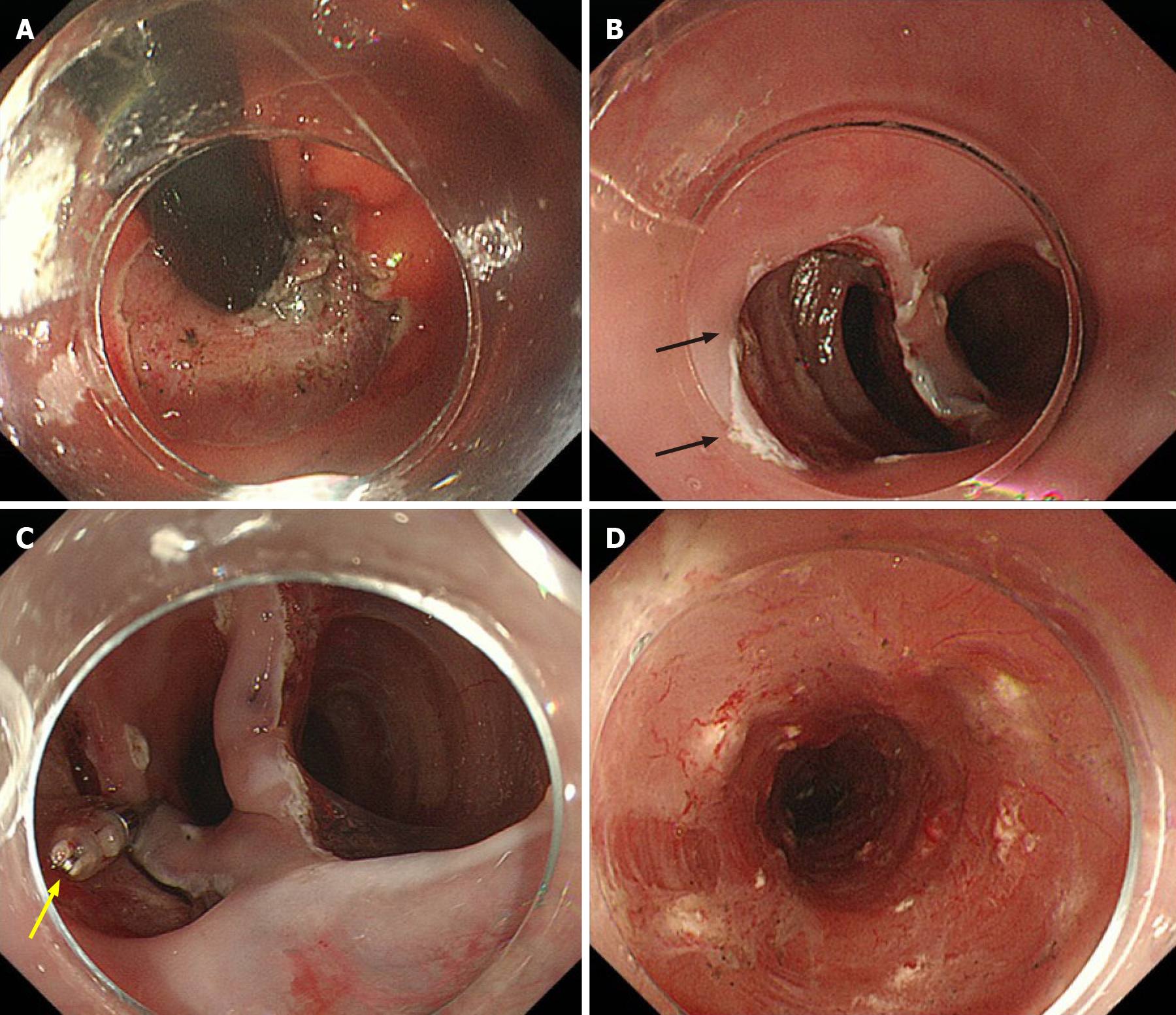
Figure 4 Images of intraoperative endoscopy.
A: Barrett's esophagus-related neoplasia appears to spread up to the gastric cardia. Endoscopic submucosal dissection (ESD) was started in this cardiac area; B: After resecting and dissecting the cardiac lesion, three submucosal tunnels were created from the oral side (black arrow is the first tunnel); C: A clip with a thread was attached to the mucosal edge of each of the three tunnels, and the dissected tissue of the tunnels was pulled toward the oral side (yellow arrow); D: Whole circumferential ESD had been completed. Steroid solution was injected into the remaining submucosa (white spots) immediately after ESD to prevent postoperative stenosis.
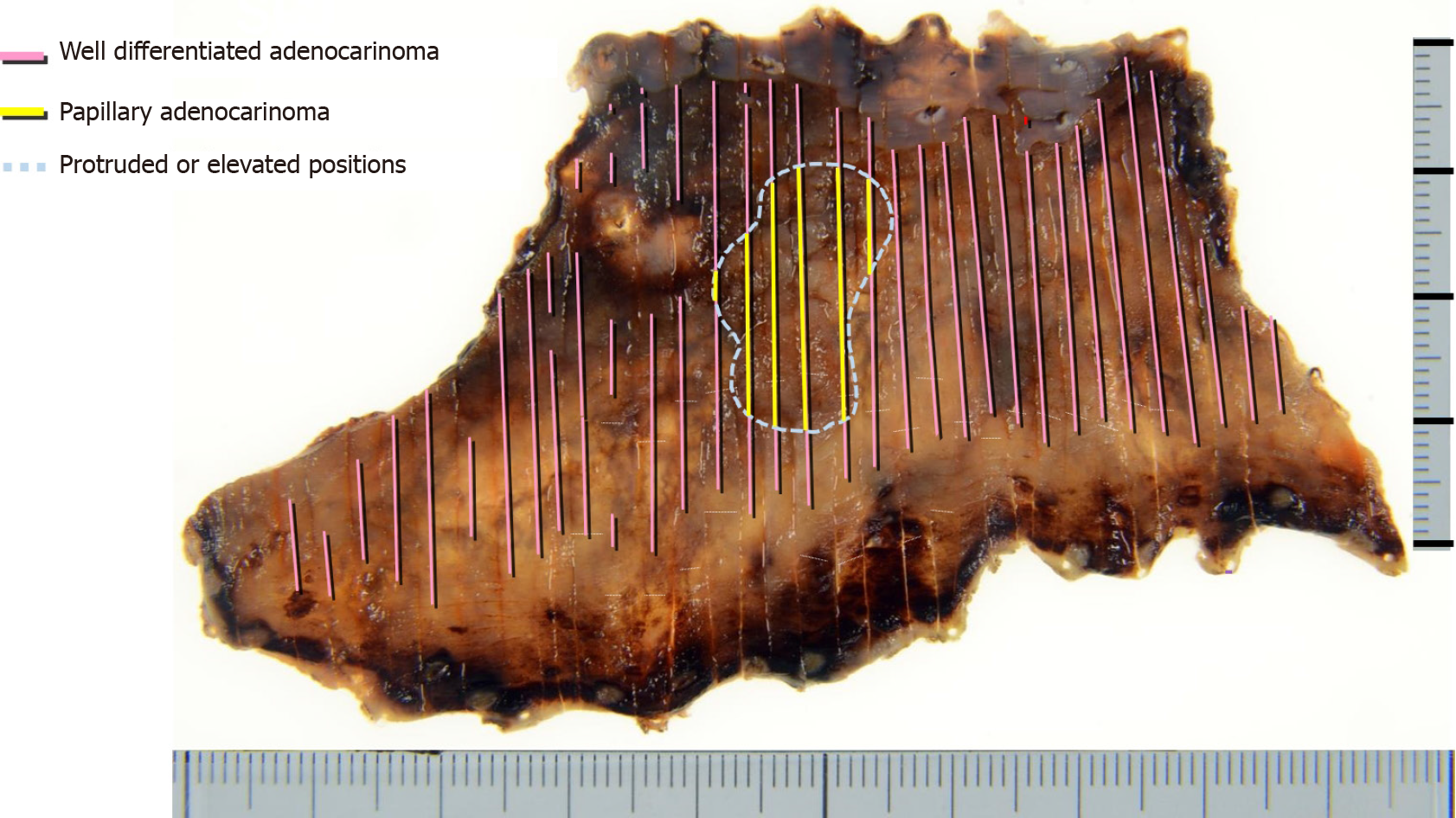
Figure 5 An endoscopic submucosal dissection en-bloc resected specimen and histological tumor distribution.
The superficial carcinoma consisted of papillary and well-differentiated tubular adenocarcinoma in the protruded and elevated positions and extensive flat portions, respectively. The adenocarcinoma lesion extended the whole circumference of the long-segment Barrett’s esophagus and was confined to the superficial muscularis mucosae.
- Citation: Abe K, Goda K, Kanamori A, Suzuki T, Yamamiya A, Takimoto Y, Arisaka T, Hoshi K, Sugaya T, Majima Y, Tominaga K, Iijima M, Hirooka S, Yamagishi H, Irisawa A. Whole circumferential endoscopic submucosal dissection of superficial adenocarcinoma in long-segment Barrett's esophagus: A case report. World J Gastrointest Surg 2021; 13(10): 1285-1292
- URL: https://www.wjgnet.com/1948-9366/full/v13/i10/1285.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v13.i10.1285