Copyright
©The Author(s) 2020.
World J Gastrointest Surg. Jul 27, 2020; 12(7): 307-325
Published online Jul 27, 2020. doi: 10.4240/wjgs.v12.i7.307
Published online Jul 27, 2020. doi: 10.4240/wjgs.v12.i7.307
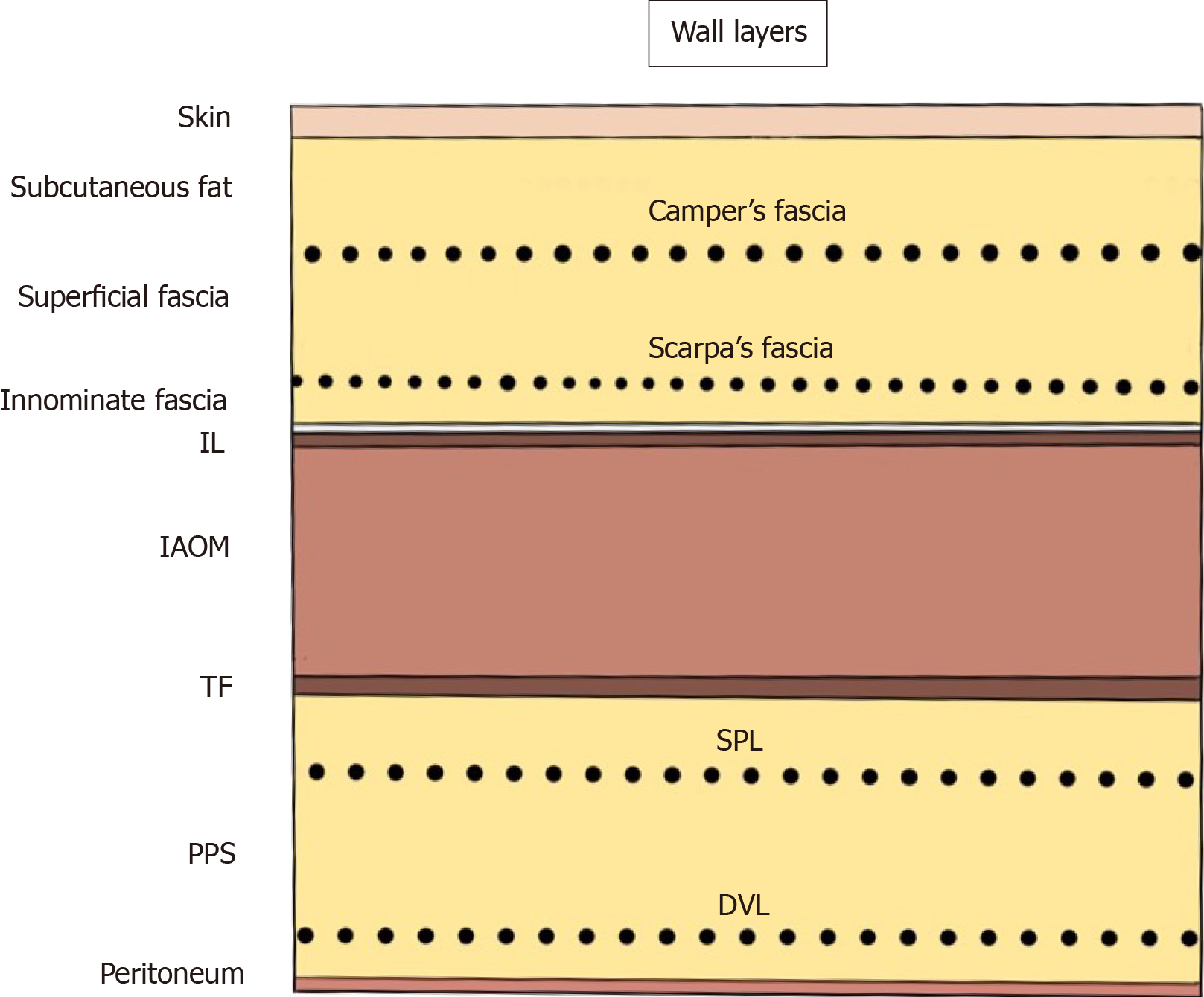
Figure 1 Abdominal wall at the groin.
The nine layers include the skin, subcutaneous fat, superficial fasciae (Camper’s and Scarpa’s fasciae), innominate (untitled) fascia, inguinal ligament, internal abdominal oblique muscle, transversalis fascia, preperitoneal space [superficial parietal layer (anterior subperitoneal fascia) and deeper visceral layer (posterior subperitoneal fascia)] and peritoneum. DVL: Deeper visceral layer; IAOM: Internal abdominal oblique muscle; IL: Inguinal ligament; PPS: Preperitoneal space; SPL: Superficial parietal layer; TF: Transversalis fascia.
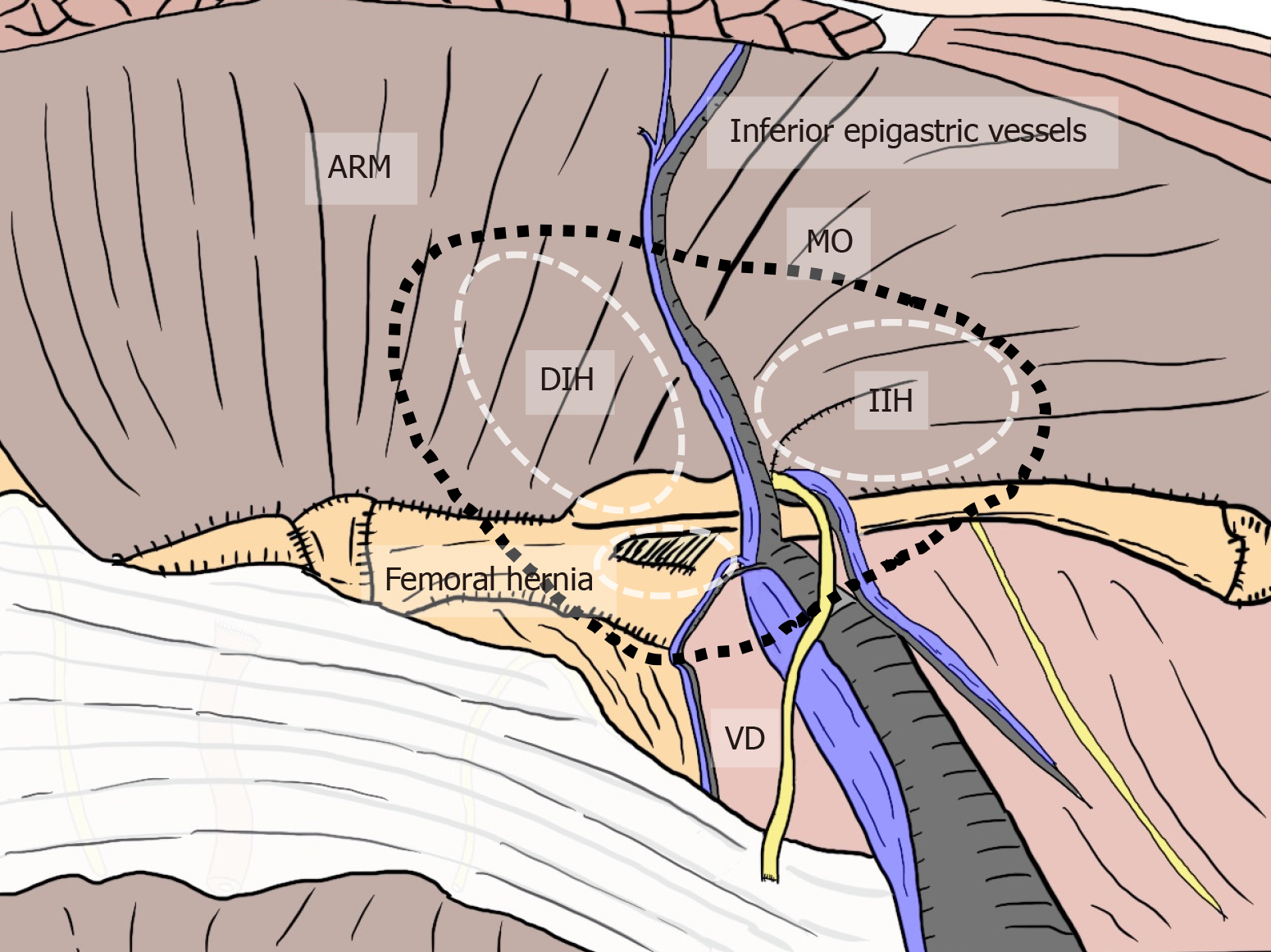
Figure 2 Relation between myopectineal orifice and all hernias (direct inguinal hernia, indirect inguinal hernia, femoral hernia) at the groin.
The oval myopectineal orifice (black dotted circle) is the origin of all groin hernias (white dotted circles). ARM: Abdominal rectal muscle; DIH: Direct inguinal hernia; IIH: Indirect inguinal hernia; MO: Myopectineal orifice; VD: Vas deferens.
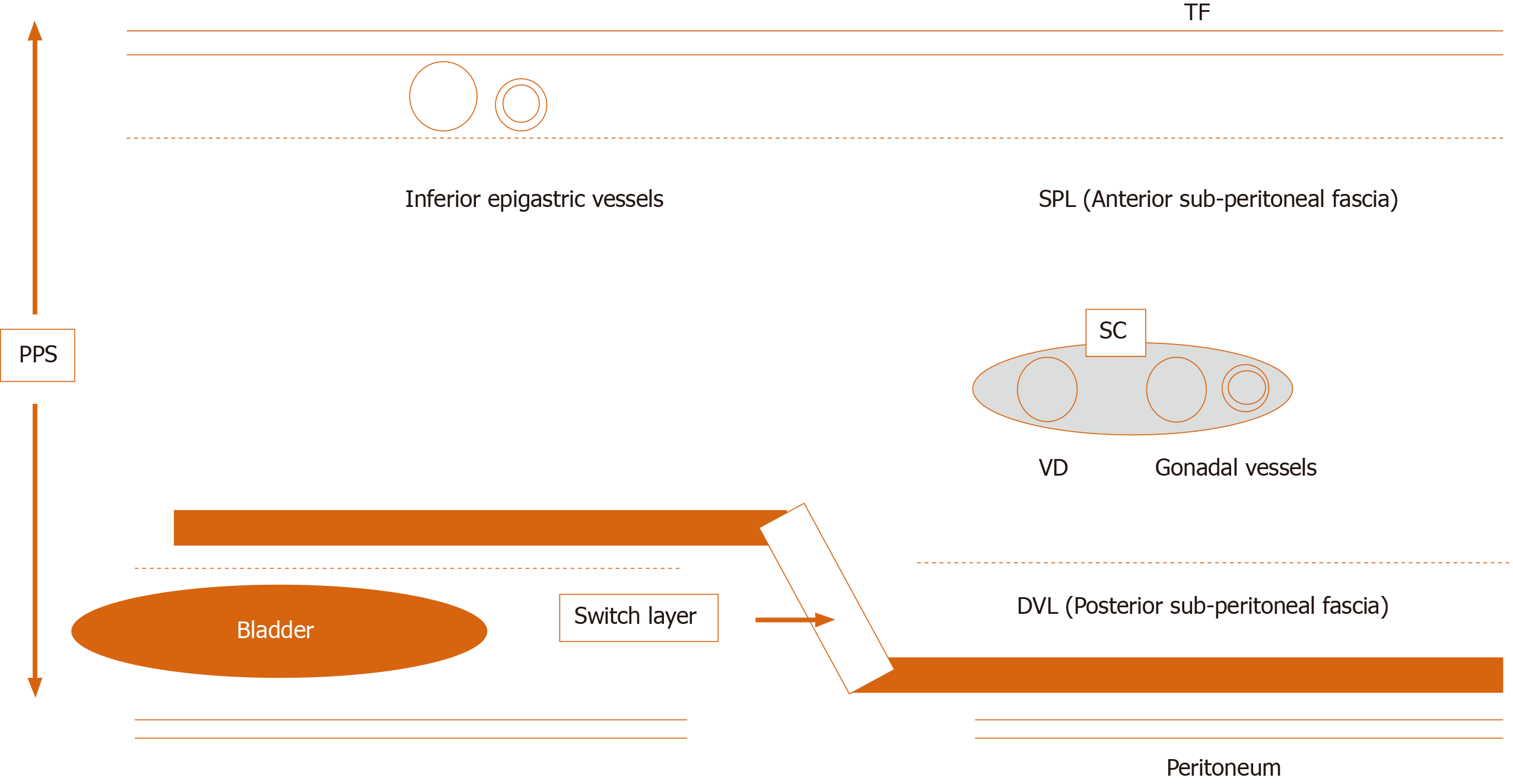
Figure 3 Current knowledge of the preperitoneal space and the adequate position of mesh placement during the transabdominal preperitoneal repair.
Anatomical identification of the superficial parietal layer (SPL) and deeper visceral layer (DVL) was a milestone for further developments in surgical repairs. The dissected layer should be adequately switched between the SPL and DVL. DVL: Deeper visceral layer; PPS: Preperitoneal space; SC: Spermatic cord; SPL: Superficial parietal layer; TAPP: Transabdominal preperitoneal; TF: Transversalis fascia; VD: Vas deferens.
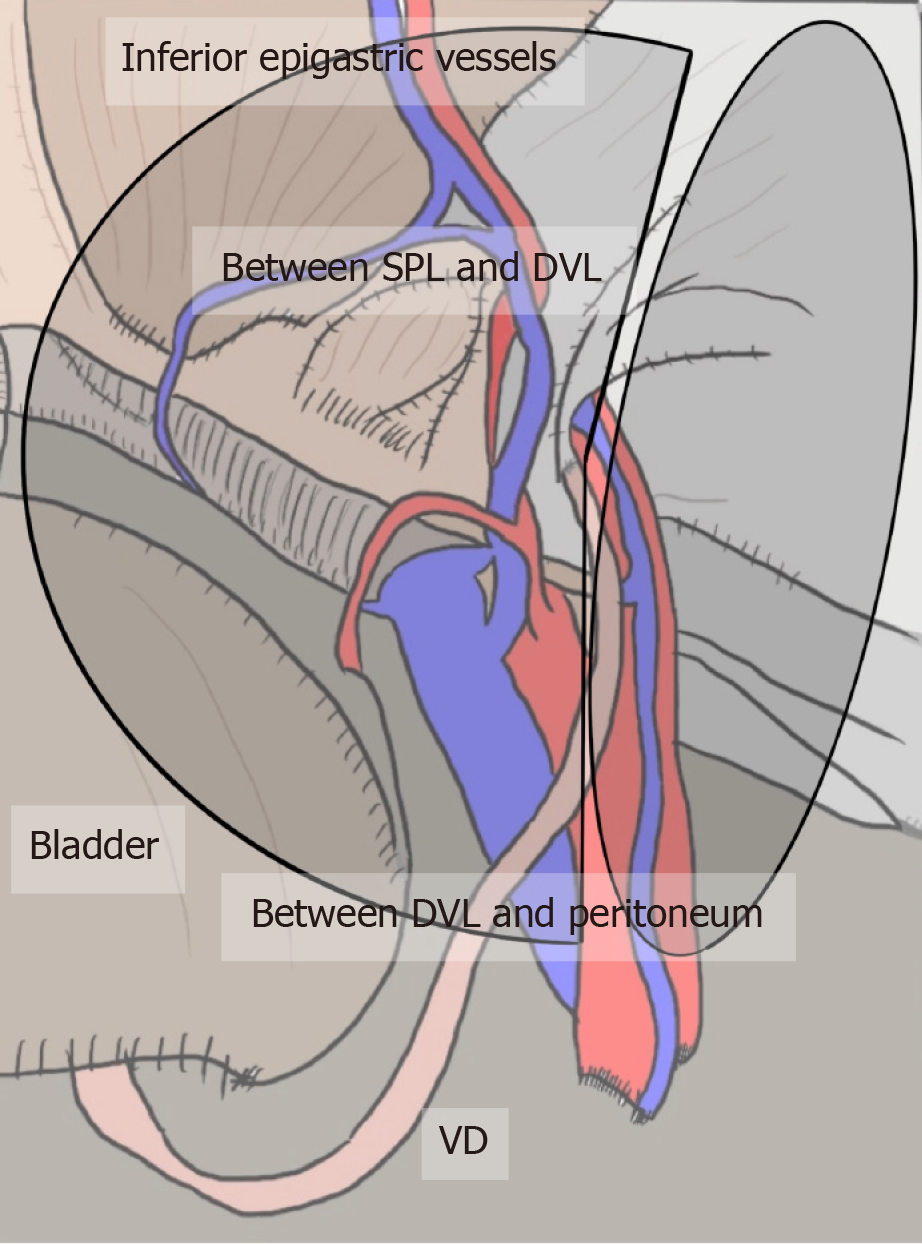
Figure 4 Appropriate layer and adequate mesh placement during a transabdominal preperitoneal repair.
Surgical mesh should be adequately placed in an appropriate layer to avoid hernia recurrence and bladder injury. The layer is dissected between the superficial parietal layer and deeper visceral layer (DVL) on the inner side, whereas it is dissected between the DVL and peritoneum on the outer side. DVL: Deeper visceral layer; SPL: Superficial parietal layer; VD: Vas deferens.
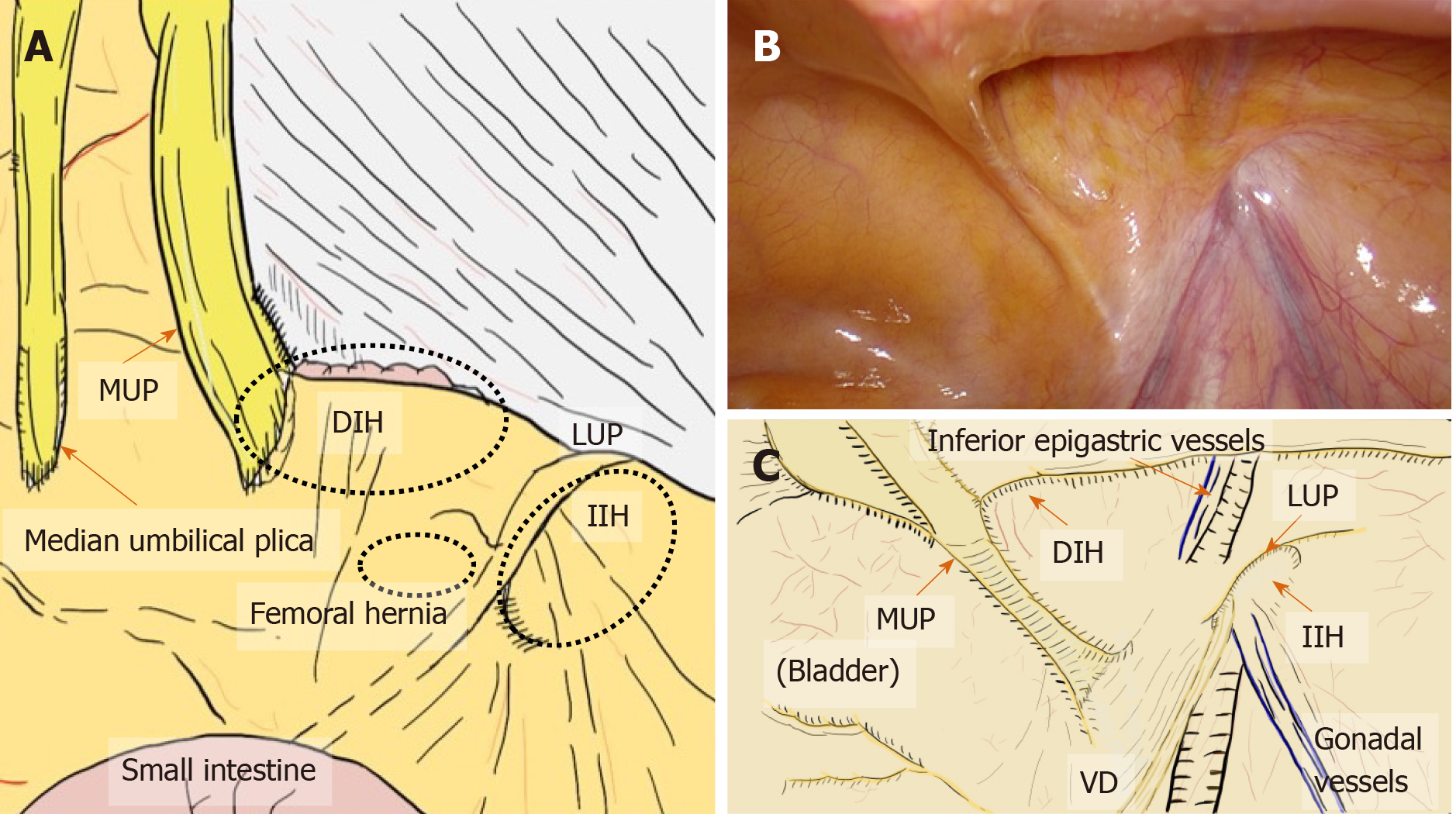
Figure 5 Laparoscopic view at the groin.
A: Laparoscopic view focused on the relation between the plicae and the hernial defect. B and C: The actual view (B) and schema (C) are shown. Laparoscopic view with pneumoperitoneum has a significant advantage for easy, accurate diagnosis without any missed evaluations because the plicae and fossae precisely indicate hernia defects. DIH: Direct inguinal hernia; IIH: Indirect inguinal hernia; MUP: Medial umbilical plica; LUP: Lateral umbilical plica; VD: Vas deferens.
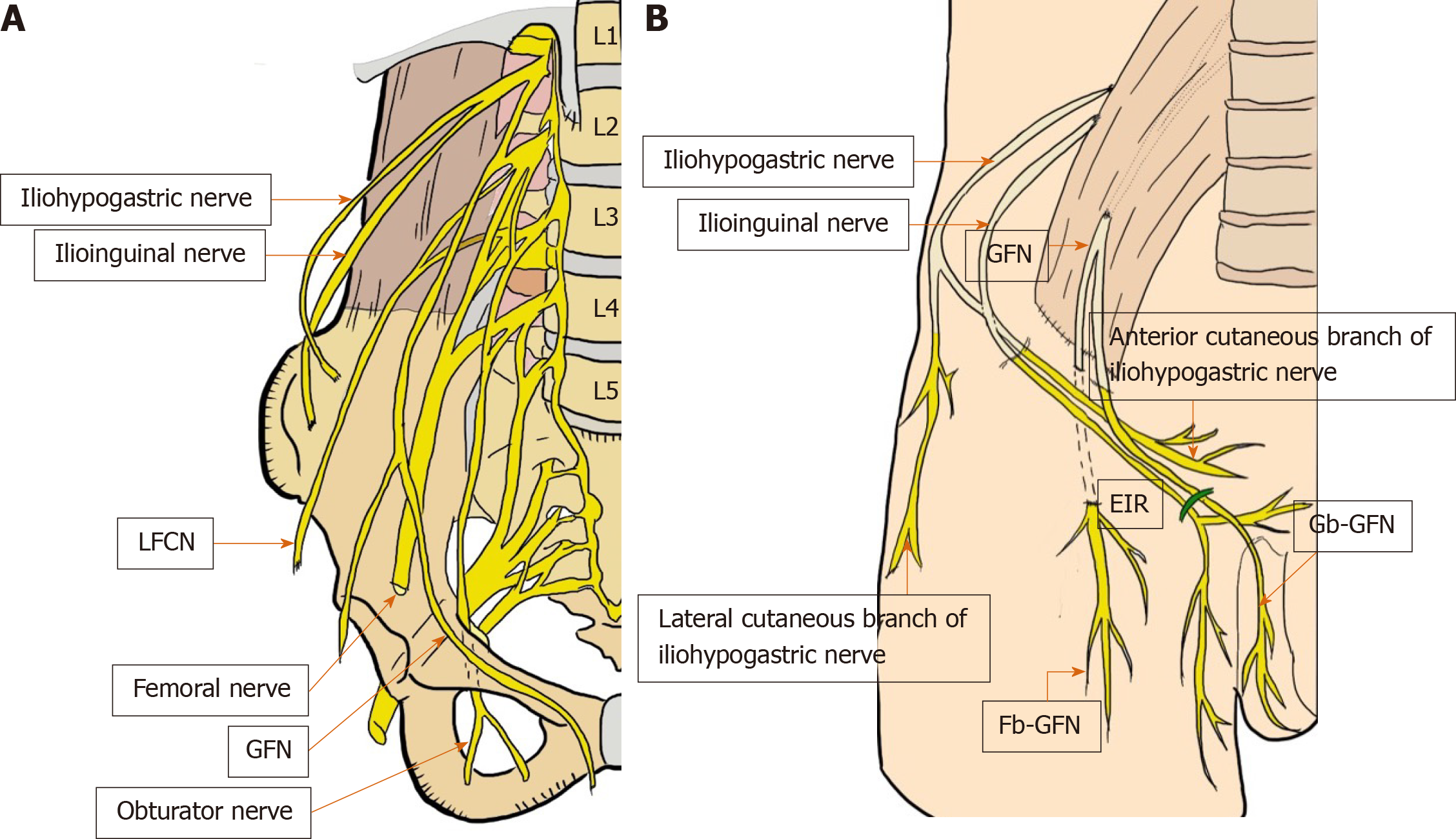
Figure 6 Critical nerves distributed in the field of the groin (A and B).
These six nerves of interest are the iliohypogastric nerve, ilioinguinal nerve, femoral nerve (including the anterior cutaneous branch), genitofemoral nerve (femoral and genital branches), lateral femoral cutaneous nerve of the thigh, and obturator nerve. EIR: External inguinal ring; Fb-GFN: The femoral branch of the GFN; Gb-GFN: Genital branch of the GFN; GFN: Genitofemoral nerve; LFCN: Lateral femoral cutaneous nerve.
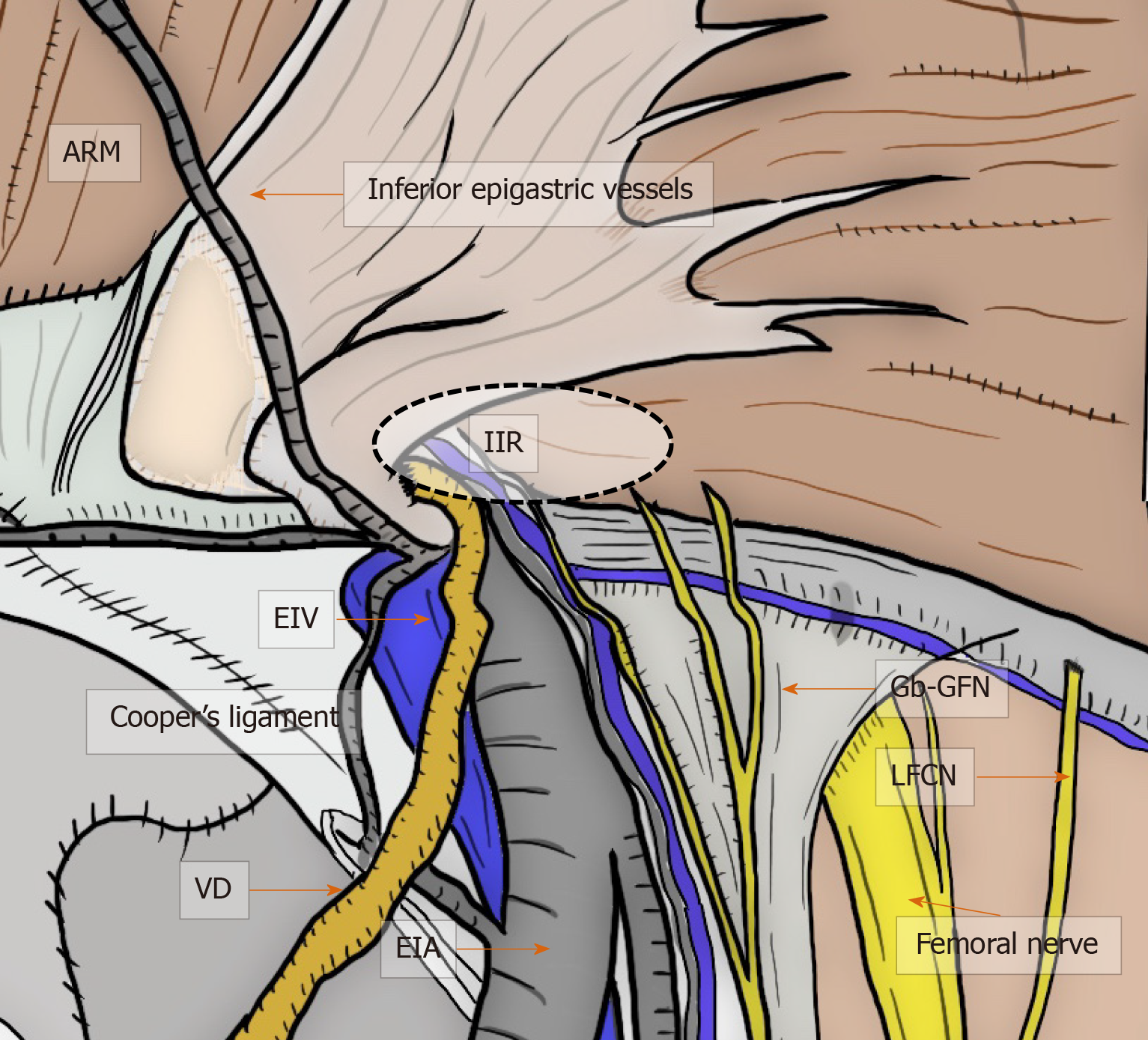
Figure 7 Critical nerves and other structures.
Laparoscopic view in the groin area focused on the relation between the critical nerves [especially genital branch of the genitofemoral nerve and lateral femoral cutaneous nerve (LFCN)] and the other structures. Although the genitofemoral nerves run to the lower limbs, the more common nerve injuries are unfortunately to the genitofemoral nerve and LFCN. Each of these serious injuries has disastrous consequences for the patient with intractable pain. ARM: Abdominal rectal muscle; EIA: External iliac artery; EIV: External iliac vein; Gb-GFN: Genital branch of the genitofemoral nerve; IIR: Indirect inguinal ring; LFCN: Lateral femoral cutaneous nerve; VD: Vas deferens.
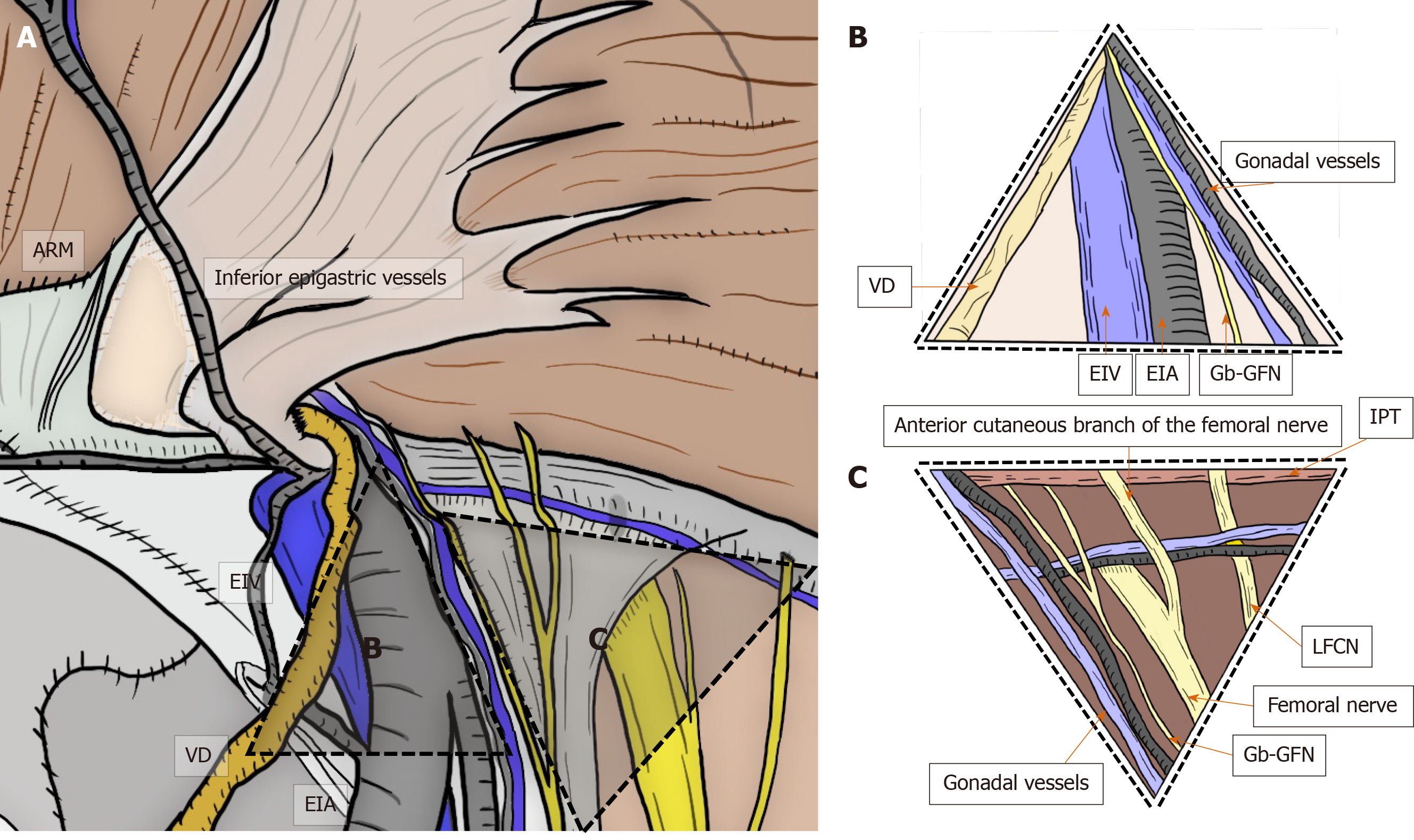
Figure 8 Triangle of doom and triangle of pain.
Triangle of doom and triangle of pain should be adequately recognized by the surgeon. Triangle of doom is an inverted V-shaped area bound laterally by the gonadal vessels and medially by the vas deferens in male patients, or the round ligament in female patients. The EIA, external iliac vein, deep circumflex iliac vein, genital branch of the genitofemoral nerve, and femoral nerve are involved in this area. Area of the triangle of pain involves the femoral branch of the genitofemoral nerve, lateral femoral cutaneous nerve, femoral nerve, and the anterior cutaneous branch of the femoral nerve. Even a subtle injury to the nerves located within the triangle of pain is a risk factor for intractable pain. ARM: Abdominal rectal muscle; EIA: External iliac artery; EIV: External iliac vein; Gb-GFN: Genital branch of the genitofemoral nerve; IPT: Iliopubic tract; LFCN: Lateral femoral cutaneous nerve; VD: Vas deferens.
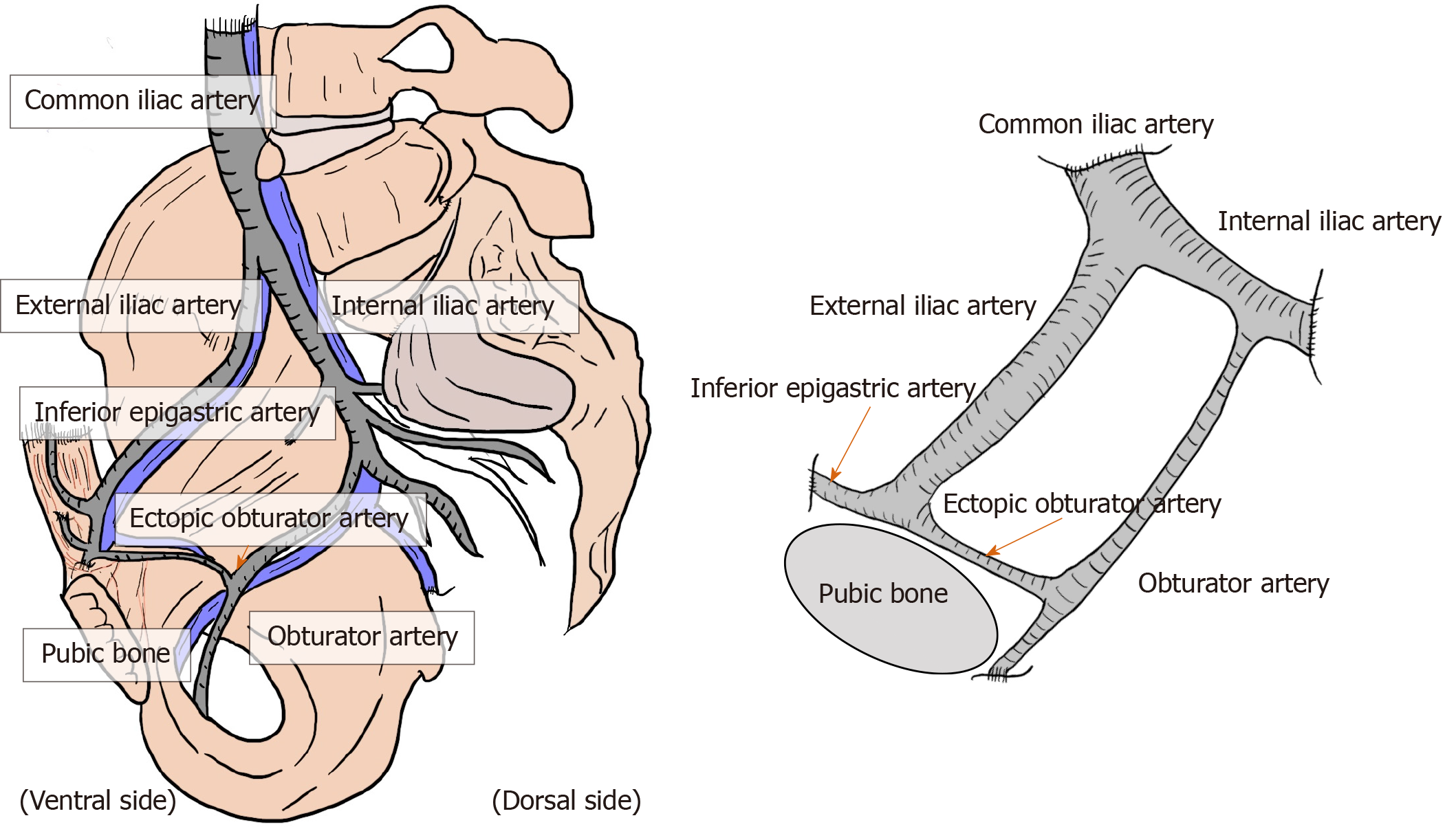
Figure 9 Corona mortis.
Corona mortis and complicated vascular connection between the epigastric and obturator vessels. The corona mortis is classically defined as the arterial anastomosis between the obturator artery and the inferior epigastric artery via the ectopic obturator artery. The existence of the obturator artery results in annular communication between the inferior epigastric artery, common iliac artery, internal iliac artery, external iliac artery, and obturator artery. There may be several variants of anastomosing vascular branches. Brisk bleeding is difficult to control because of the dual vascular supply from the obturator and iliac vessels.
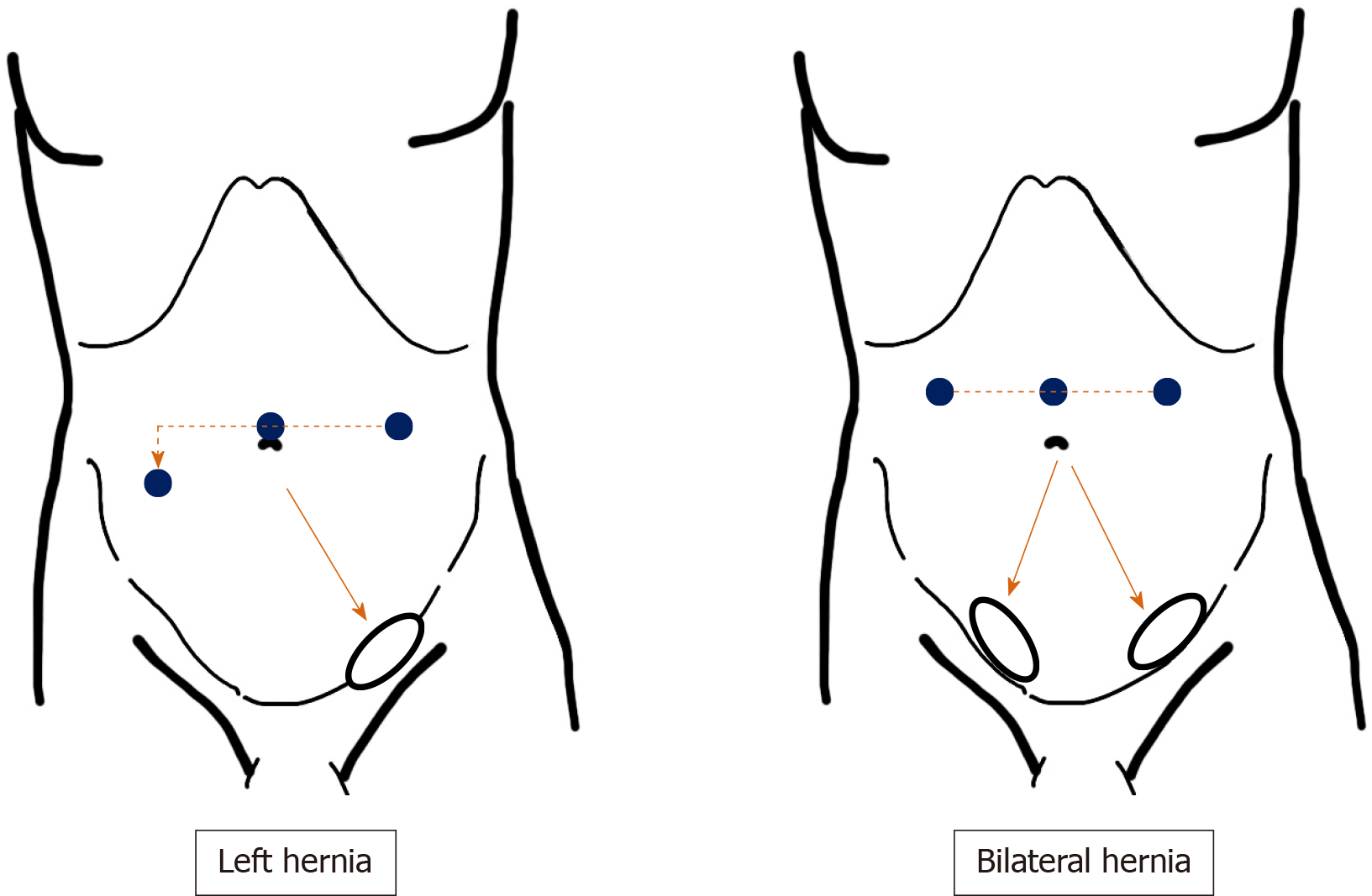
Figure 10 Port placement.
Placement of surgical ports recommended for transabdominal preperitoneal repair. Pneumoperitoneum is achieved through an umbilical port. Two working ports (3- and 5-mm ports) are placed, and forceps are inserted in each at adequate angles to the target site. The port at the side opposite the target site is set lower than the umbilicus. The 5-mm port is used by the dominant arm of the main surgeon.
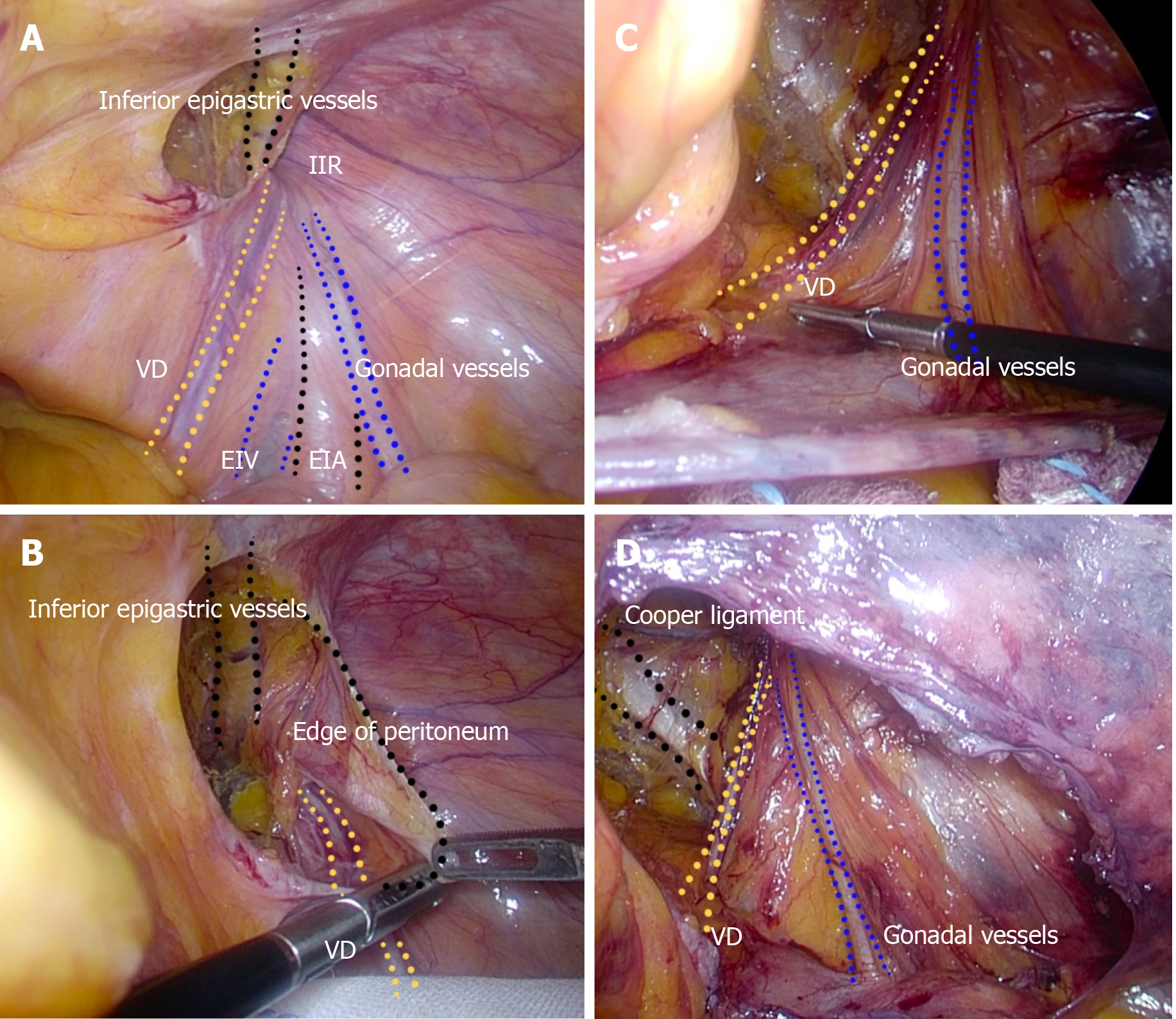
Figure 11 Complete preservation of the vas deferens and gonadal vessels.
A: Surgical procedure during dissection around the vas deferens (VD) and gonadal vessels. Familiarity with the important structures should be required. B and C: The VD and gonadal vessels should be completely preserved without any subtle damage. D: The VD and gonadal vessels are sharply dissected from the peritoneum without use of electric cautery or a coagulating scalpel, under an adequate overhead view. EIA: External iliac artery; EIV: External iliac vein; IIR: Indirect inguinal ring; VD: Vas deferens.
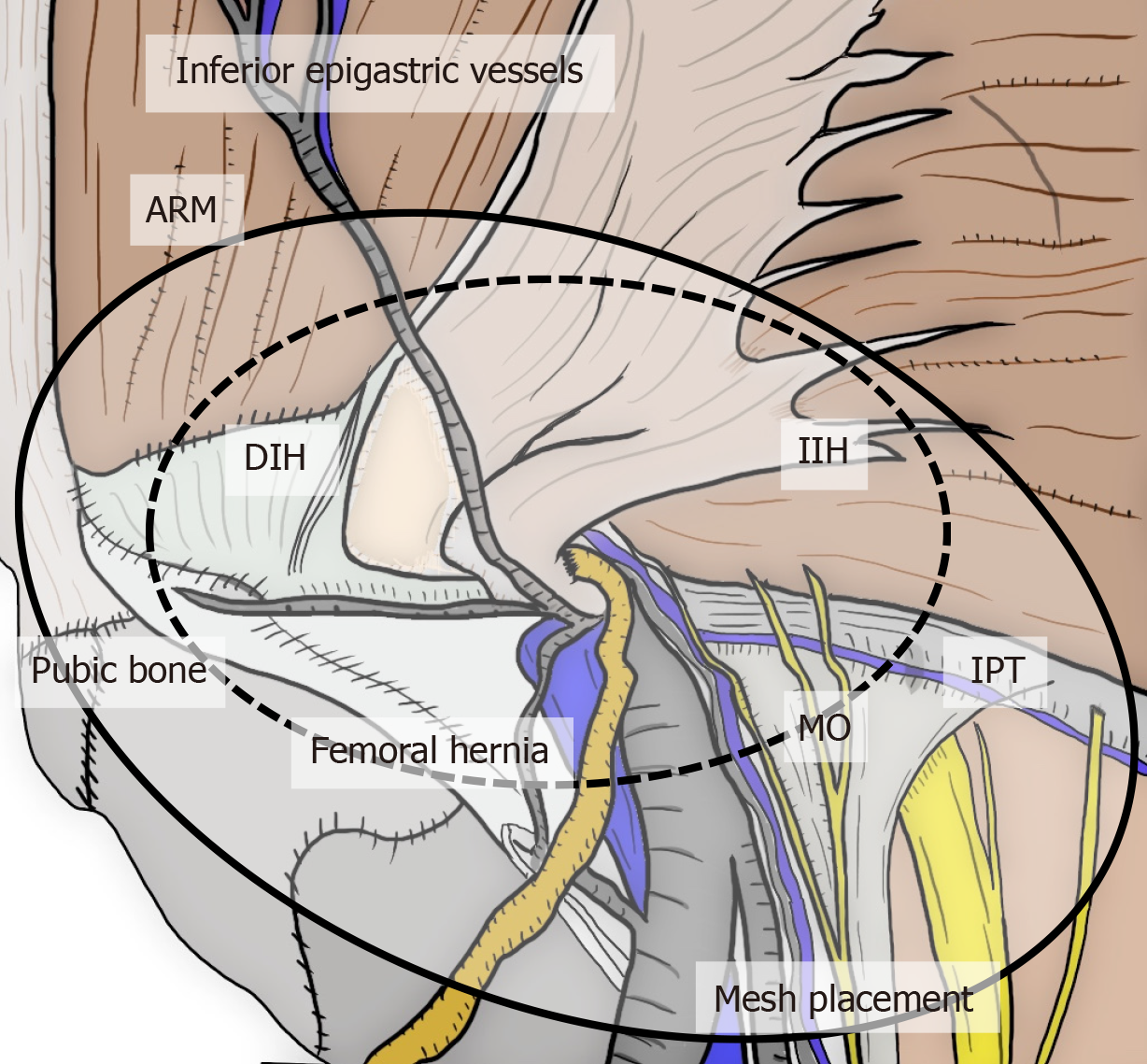
Figure 12 Adequate area covered by mesh.
The relation between the myopectineal orifice (MO) and an area adequately covered by mesh. The MO should be fully reinforced by mesh placed at the preperitoneal space during transabdominal preperitoneal repair. ARM: Abdominal rectal muscle; DIH: Direct inguinal hernia; IIH: Indirect inguinal hernia; MO: Myopectineal orifice.
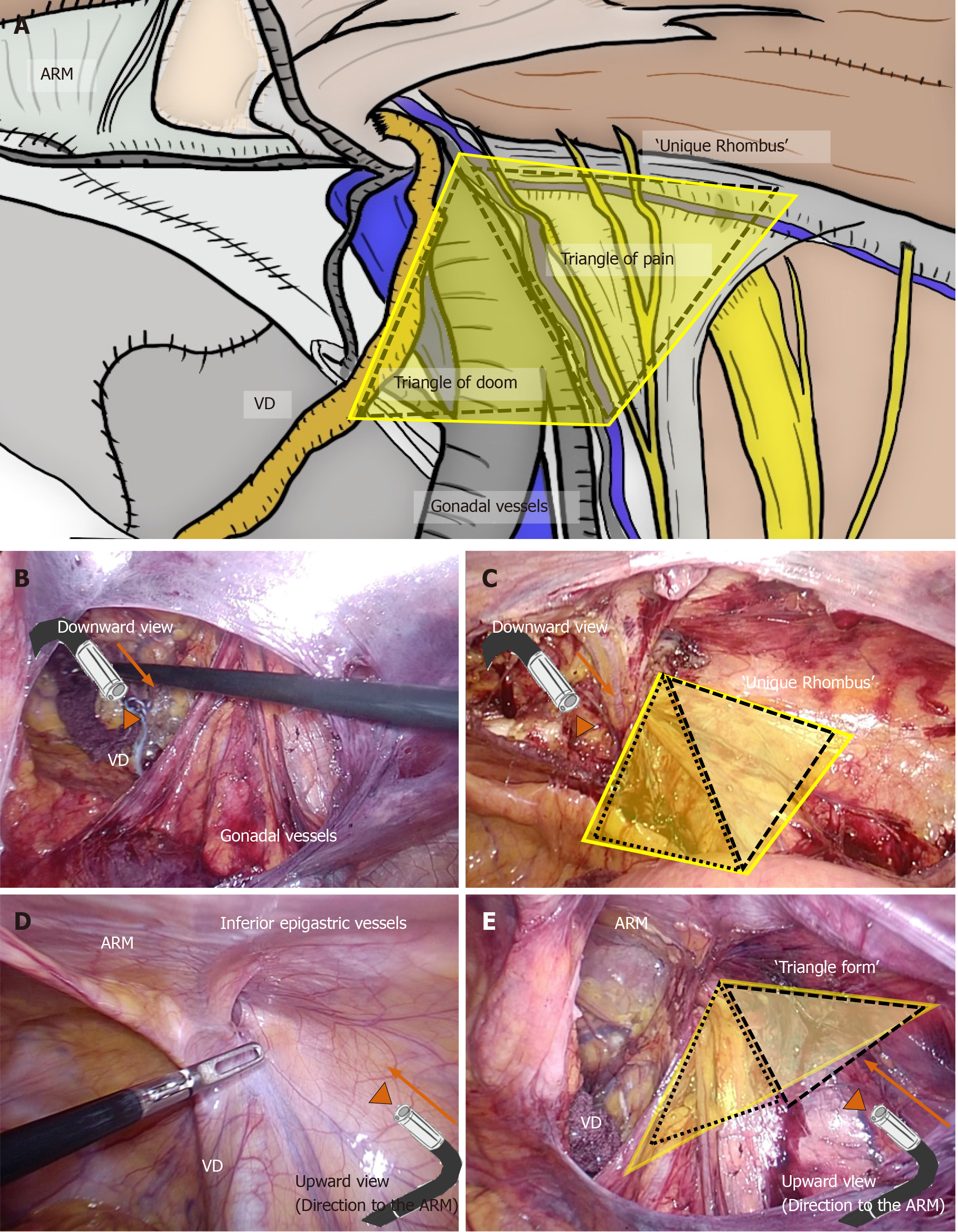
Figure 13 Importance of upward view.
A: The triangle of doom and triangle of pain configure a unique rhombus around the inferior epigastric artery (IEA). Adequate change of laparoscopic view during transabdominal preperitoneal (TAPP) is very important. B and C: Although downward view requires safe preservation of the vas deferens and gonadal vessels and sure exposure of Cooper’s ligament, downward view may easily mislead surgeons causing unexpected injuries of topographic nerves and vessels. D and E: Generally, a unique rhombus around the IEA seems to be a triangle on the upward view, and the abdominal rectal muscle (ARM) is simultaneously observed at the roof. Thus, intraperitoneal anatomy including the ARM should be simultaneously recognized by upward view, for optimal mesh placement during TAPP. ARM: Abdominal rectal muscle; VD: Vas deferens.
- Citation: Yasukawa D, Aisu Y, Hori T. Crucial anatomy and technical cues for laparoscopic transabdominal preperitoneal repair: Advanced manipulation for groin hernias in adults. World J Gastrointest Surg 2020; 12(7): 307-325
- URL: https://www.wjgnet.com/1948-9366/full/v12/i7/307.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v12.i7.307