Published online Feb 15, 2014. doi: 10.4239/wjd.v5.i1.76
Revised: December 2, 2013
Accepted: January 13, 2014
Published online: February 15, 2014
Processing time: 232 Days and 14.6 Hours
AIM: To describe baseline data of the optimal type 2 diabetes management including benchmarking and standard treatment (OPTIMISE) study in Greece.
METHODS: “Benchmarking” is the process of receiving feedback comparing one’s performance with that of others. The OPTIMISE (NCT00681850) study is a multinational, multicenter study assessing, at a primary care level, whether using “benchmarking” can help to improve the quality of patient care, compared with a set of guideline-based reference values (“non-benchmarking”). In the Greek region, 797 outpatients (457 men, mean age 63.8 years) with type 2 diabetes were enrolled by 84 office-based physicians. Baseline characteristics of this population are presented.
RESULTS: Hypertension was the most prevalent concomitant disorder (77.3%) and coronary heart disease was the most frequent macrovascular complication of diabetes (23.8%). Most patients were overweight or obese (body mass index 29.6 ± 5 kg/m2), exhibiting mostly abdominal obesity (waist circumference 102.6 ± 13.6 cm). Biguanides were the most prevalent prescribed drugs for the management of diabetes (70.1% of all prescriptions), whereas statins (93.5% of all prescriptions) and angiotensin receptor blockers (55.8% of all prescriptions) were the most prevalent prescribed drugs for hyperlipidemia and hypertension, respectively. Only 37.4% of patients were on aspirin. Despite treatment, pre-defined targets for fasting plasma glucose (< 110 mg/dL), glycated hemoglobin (< 7%), systolic blood pressure (< 130 mmHg and < 125 mmHg for patients with proteinuria) and low density lipoprotein cholesterol levels (< 100 mg/dL and < 70 mg/dL for patients with coronary heart disease) were reached in a relatively small proportion of patients (29%, 53%, 27% and 31%, respectively). In a Greek population with type 2 diabetes, the control of glycemia or concomitant disorders which increase cardiovascular risk remains poor.
CONCLUSION: Despite relevant treatment, there is a poor control of diabetes, hypertension and hyperlipidemia in Greek outpatients with type 2 diabetes.
Core tip: This is an epidemiological study assessing the prevalence of comorbidities as well as treatment control in a Greek population of patients with type 2 diabetes. “Benchmarking” is the process of receiving feedback and comparing one’s performance to that of others. The optimal type 2 diabetes management including benchmarking and standard treatment (OPTIMISE) study is a multinational, multicenter study comparing the efficacy of two follow-up strategies in the management of type 2 diabetic outpatients: “benchmarking”vs“non-benchmarking”. This paper describes the rationale and the design of the OPTIMISE study as well as the baseline characteristics of patients included in the Greek region.
- Citation: Kostapanos MS, Tsimihodimos V, Elisaf MS, Tzouvelekis E, Nikas N. Rationale, design and baseline patient characteristics of the optimal type 2 diabetes management including benchmarking and standard treatment study in Greece. World J Diabetes 2014; 5(1): 76-83
- URL: https://www.wjgnet.com/1948-9358/full/v5/i1/76.htm
- DOI: https://dx.doi.org/10.4239/wjd.v5.i1.76
According to the World Health Organization (WHO), > 180 million people worldwide suffer from diabetes[1]. This number is likely to increase by more than double by the year 2030. In 2005 alone, approximately 1.1 million people died from diabetes-related complications[1]. The WHO projects that without urgent action, deaths due to these complications will increase by > 50% in the next 10 years[1]. Type 2 diabetes, which is closely related to an unhealthy lifestyle and obesity, is associated with increased risk of micro- and macrovascular outcomes, including heart attacks, strokes and amputations of the lower limbs[1]. Furthermore, diabetes complications not only decrease life expectancy, but also markedly reduce the quality of life. These outcomes result in increasing health care costs[2].
This burden can be limited with effective treatment practices[2]. However, a marked variability has been documented in preventive and therapeutic approaches, suggesting that the level of diabetes care currently delivered may not produce the predicted health-related benefits[3]. Gaps between medical care as actually practiced and the recommendations derived from evidence-based research are large and widespread[3]. Approaches improving the quality of patient care include the development of guidelines, flowcharting, data collection and graphical data analysis. More recent innovations are benchmarking and computerized decision support[3].
Benchmarking is the process of comparing one’s performance with that of others[4]. This process begins with standardized and comparative measurement. It can go further to understand why there are performance differences between seemingly similar processes[4]. Benchmarking is practical and action-oriented in its analysis; it is not a rigorous research methodology. It is, however, a promising technology that breaks through the isolation that many clinicians report as the underlying cause of variation in clinical practice[4].
The optimal type 2 diabetes management including benchmarking and standard treatment (OPTIMISE, NCT00681850) study was a multinational, multicenter study assessing, at a primary care level, whether using benchmarking can help in improving the quality of patient care as compared with a set of guideline-based reference values. In this paper, baseline data of patients included in the OPTIMISE study in the Greek region are analyzed.
The primary objective of this study was the improvement of the quality of diabetic patient care, particularly the control of glycemia, lipids and blood pressure, with benchmarking over a set of guideline-based reference values (non-benchmarking). In this context, the percentage of patients in the benchmarking group achieving pre-set targets for glycated hemoglobin (HbA1c)[1], low density lipoprotein cholesterol (LDL-C)[1,5] and systolic blood pressure (SBP)[1,6] vs non-benchmarking group (control group) after 12 mo of follow-up was assessed.
Secondary objectives were to demonstrate that using benchmarking improves the control of diabetes, lipids and blood pressure (1) by means of the proportion of patients achieving pre-set targets for HbA1c[1], glycemia[1], LDL-C levels[1,5] and SBP[1,6] or (2) by determining the improvement in these parameters after 12 mo of follow-up. Other secondary objectives included (3) the preventive screening for several outcomes: retinopathy, neuropathy, dietary counseling, microalbuminuria, smoking habits, body mass index (BMI) and physical activity and (4) the measurement of physical activity by registering the number of steps and the distance walked per day.
Type 2 diabetic patients, followed by usual physician treatment, were recruited for observation. Selection criteria were male or female subjects (1) with a minimum age of 18 years; (2) with type 2 diabetes, treated or untreated, insulin dependent or not insulin dependent at the time of first visit; and (3) who signed an informed consent to participate in the study. Diabetes was defined by plasma levels of glucose (PG); fasting PG was ≥ 126 mg/dL or PG levels 2-h post-load was ≥ 200 mg/dL. Patients who (1) suffered from type 1 diabetes or gestational diabetes, (2) participated in any other clinical study or (3) were hospitalized during the study period (because it is a primary care study) were excluded from the study.
Investigators recruited for this study were physicians from all over the country who were willing to participate. A selection was based on the availability of sufficient diabetic patients in the physician’s practice and the motivation to fulfill the administrative procedures linked to the study. All participating investigators performed their usual monitoring, treatment and counseling of their diabetic patients. Investigators were randomized into two groups. The group that performed the usual monitoring of their diabetic patients by knowing the relative level of diabetic control of their patients compared with the patients of other investigators was defined as the benchmarking group. The other group (non-benchmarking) did not receive any information and behaved as a control group. The proportion of investigators receiving that information (benchmarking) vs the control group was 3 to 1.
All investigators received feedback on the risk factors of their patients. Additionally, in the benchmarking group, physicians anonymously received information on the level of control of cardiovascular risk factors for their patients compared with their colleagues. This possibly resulted in an additional motivational stimulus for investigators and patients to follow therapeutic advice and to improve their risk factors.
The time interval between visits in this study corresponded to the four-times yearly control visits for diabetic patients regarding blood pressure, fasting glycemia, HbA1c, body weight, smoking habits and physical activity, as recommended by the “International Diabetes Federation”[7]. Therefore, according to the study protocol, patients were followed-up in four visits. Baseline assessments were recorded at visit 1, and further data were collected after approximately 4 mo (visit 2), 8 mo (visit 3) and 12 mo (visit 4). The serum lipid profile [total cholesterol (TC), LDL-C, high density lipoprotein cholesterol (HDL-C) and triglyceride (TG) levels] was also recorded at baseline and at the same time intervals.
At each visit, blood pressure was measured with the patient in the sitting position following at least 5 min of rest with a manometer with a cuff of the recommended dimensions. The mean blood pressure based on three successive readings was recorded. Somatometrics, including body weight, height (only at the first visit) and waist circumference, were also measured during the follow-up. The patient ideally wore light clothing and no shoes during the weight measurement. Weight was given in kilograms, without decimals (to round up as from 0.5 kg). The patient ideally wore no shoes during the height measurement. Height was given in centimeters without decimals (to round up as from 0.5 cm). For the measurement of waist circumference, a measuring tape was placed in a horizontal plane around the abdomen at the level of the iliac crest. Before reading the tape measure, investigators ensured that the tape was snug without compressing the skin and parallel to the floor. The measurement was made at the end of a normal expiration.
After an 8-h overnight fast, two blood samples (7 mL) were obtained. The following parameters were analyzed at the central lab BARC (Industriepark Zwijnaarde 7b3, B-9052 Ghent, Belgium): (1) HbA1c, (2) fasting PG and (3) the serum lipid profile, including TC, TG, HDL-C and LDL-C levels. At visits 1 and 4, a urine sample of 4 mL was collected for analysis of microalbuminuria.
Pre-defined targets of treatment were (1) HbA1c < 7% and fasting PG < 110 mg/dL for glycemic control, (2) SBP < 130 mmHg and < 125 mmHg in the case of renal impairment and proteinuria > 1 g/24 h for blood pressure control and (3) LDL-C levels < 100 mg/dL and < 70 mg/dL for very high-risk patients (i.e., those with diabetes and coronary heart disease) for serum lipids control.
Patients were categorized according to fasting PG levels into (1) “normal” if fasting PG was < 110 mg/dL, (2) “borderline” if fasting PG was 110-125 mg/dL and (3) “diabetics” if fasting PG was ≥ 125 mg/dL. According to HbA1c levels, patients were classified into “good” if HbA1c ≤ 7% and “too high” if HbA1c > 7%. SBP levels divided the study population into: “good” if < 130 mmHg and “too high” if ≥ 130 mmHg. According to LDL-C levels, patients were categorized into “good” if LDL-C < 100 mg/dL and “too high” if LDL-C ≥ 100 mg/dL.
A four-point verbal rating scale was used to assess the following physical activity: (1) no weekly activity; (2) only limited physical activity during most weeks; (3) intense physical activity (activity that gives rise to shortness of breath, tachycardia and sweating) during at least 20 min, once to twice a week; and (4) intense physical activity (activity that gives rise to shortness of breath, tachycardia and sweating) during at least 20 min, three times or more a week.
Descriptive statistics (mean, median, number of observations, standard deviation, standard error, 95%CI, minimum and maximum) of all primary and other variables are presented in tables and, if appropriate and interesting, in graphs. This is applicable for the following variables: HbA1c, glycemia, LDL-C, SBP, TG, TC, HDL-C, diastolic blood pressure, waist circumference, smoking habits, microalbuminuria, BMI, physical activity (rating scale), degree of ophthalmic control and degree of dietary advice.
The null hypothesis for the primary objective is that the proportion of patients who reached targets after 12 mo in both groups is equal. The alternative hypothesis is that this proportion is greater in the benchmarking group compared with the control group. This analysis is performed for the following variables: HbA1C, LDL-C and SBP. For secondary objectives, the null hypothesis is that the proportion of patients who reached the target after 12 mo is the same as the proportion of patients who reached the target at baseline. The alternative hypothesis is that this proportion is even greater after 12 mo than at baseline. This analysis is also performed for HbA1c, LDL-C and SBP. Another null hypothesis is that the mean proportion improvement of these variables after 12 mo is equal to zero. The alternative hypothesis is that the mean percentage improvement is different from zero.
The study design and the global baseline results of the OPTIMISE study have been previously reported[8,9]. Additionally, the benchmarking process has been schematically described in detail above[8].
A total of 797 patients were enrolled in this study (n = 570 in the benchmarking group and 227 in the control group) by 84 participating office-based physicians across Greece. History data of the study population are shown in Table 1. Most patients were middle-aged and had a positive family history of diabetes (Table 1). A small predominance of male gender was noted in our population. Patients were middle-aged at the time of diagnosis of diabetes and presented after approximately a 10-year course of diabetes.
| Variable | Value |
| Age (yr) | 64 ± 11 |
| Male gender | 457 (57.3) |
| Positive family history of diabetes | 483 (64.2) |
| Family history of premature heart disease | 213 (28.4) |
| Time since diagnosis of diabetes (yr) | 9.2 ± 8.3 |
| Age at diagnosis of diabetes (yr) | 54 ± 11 |
| Smoking status | |
| Current smokers | 194 (24.3) |
| Ex-smokers | 171 (21.4) |
| Non-smokers | 432 (54.2) |
Hypertension was a common concomitant disorder in our population, present in approximately 8/10 patients (Table 2). Among macrovascular complications of diabetes, coronary heart disease was the most prevalent, followed by peripheral artery disease and stroke (Table 2). Only two patients have undergone amputation. Retinopathy was the most commonly observed microvascular complication of diabetes, followed by proteinuria (Table 2).
| Clinical condition | Value |
| Hypertension | 615 (77.2) |
| Coronary heart disease | 186 (23.8) |
| Stroke | 50 (6.3) |
| Peripheral artery disease | 85 (11.1) |
| Amputation | 2 (0.3) |
| Proteinuria | 38 (5.6) |
| End-stage renal disease | 1 (0.1) |
| Retinopathy | 54 (7.2) |
Table 3 shows the main clinical characteristics of the study population. The vast majority of patients were overweight or obese, as reflected by increased BMI. The predominance of visceral obesity was mirrored by abnormally raised measurements of waist circumference. Most patients (i.e., 77%) reported no or light weekly physical activity and the rest (23%) reported “intense physical activity” for 1-2 times per week.
| Variable | Value |
| Height (cm) | 167 ± 9 |
| Weight (kg) | 83 ± 16 |
| Body mass index (kg/m2) | 29.6 ± 5.0 |
| Waist circumference (cm) | 103 ± 14 |
| Systolic blood pressure (mmHg) | 138 ± 17 |
| Diastolic blood pressure (mmHg) | 80 ± 9 |
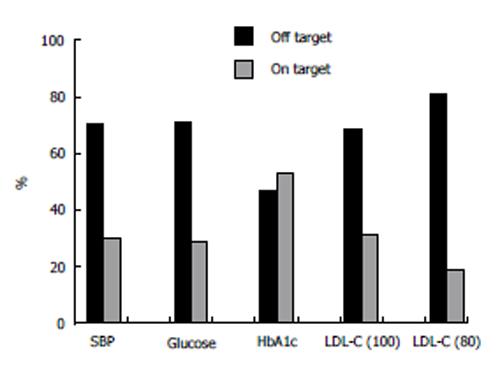
Both systolic and diastolic blood pressure levels were moderately elevated (Table 3). As expected, SBP was greater in patients with proteinuria than in patients without proteinuria (144 ± 19 mmHg vs 138 ± 17 mmHg). Only a small proportion of patients (27%) reached the pre-defined target for blood pressure, whereas most patients (72%) did not reach this target (Figure 1).
Prescribed medications are shown in Table 4. Biguanides were the most commonly prescribed antidiabetic drugs, followed by sulfonylureas. Approximately one fifth of the patients in our population were treated with insulin. The mean insulin dosage among insulin-treated patients was 48 ± 28 units/d. From all antidiabetic drug combinations, biguanide + sulfonylurea was the most commonly prescribed (20% of all prescriptions).
| Treatment | n (%) |
| Antidiabetic | 740 (92.9) |
| Insulin | 145 (19.6) |
| Biguanide (metformin) | 519 (70.1) |
| Sulfonylurea | 343 (46.4) |
| Glitazone | 142 (19.2) |
| Others | 104 (14.1) |
| Lipid-lowering | 553 (69.4) |
| Statin | 517 (93.5) |
| Ezetimibe | 53 (9.6) |
| Fibrate | 17 (3.1) |
| Others | 43 (7.8) |
| Antihypertensive | 591 (96.11) |
| ARBs | 330 (55.8) |
| ACEi | 202 (34.2) |
| CCBs | 242 (40.9) |
| Beta-blockers | 179 (30.3) |
| Alpha-blockers | 13 (2.2) |
| Diuretics | 220 (37.2) |
| Others | 19 (3.2) |
| Anti-obesity | 40 (5.0) |
| Aspirin | 298 (37.4) |
Almost all patients on lipid lowering therapy were taking statins (Table 4). Simvastatin was used by 34% of the statin-treated patients at a mean dose, atorvastatin by 36% and rosuvastatin by 24% at a mean dose of about 30, 20 and 12 mg/d, respectively. Statins with a mild lipid-lowering potency, including fluvastatin and pravastatin, were less frequently prescribed. The use of other hypolipidemic drugs was limited in our population. The dose of 100 mg/d was the predominant dose of aspirin, corresponding to 92% of all prescriptions.
Renin-angiotensin-aldosterone system blockade was the most popular antihypertensive strategy, with angiotensin receptor blockers (ARBs) being prescribed in more than half and angiotensin converting enzyme inhibitors (ACEi) in approximately one third of our population (Table 4). ARBs were the most commonly prescribed antihypertensive drug category, followed by calcium channel blockers (CCBs), diuretics, ACEi and beta-blockers (Table 4). From combinations of two antihypertensive drugs, ARBs with diuretics or CCBs were the more prevalent (each representing approximately 5% of all prescriptions), followed by ACEi with the same categories (approximately 3% of all prescriptions for each combination). ARBs, CCBs and diuretics combination were the most frequent among triple combinations (5% of all prescriptions).
Table 5 shows the glycemic control and serum lipid profile. Glycemic control was poor, with 71% of all patients being out of the pre-defined target according to fasting PG and 47% according to HbA1c (Figure 1). Interestingly, glycemic control was better when assessed by HbA1c rather than by fasting PG levels.
| Variable | Values |
| Glucose (mg/dL) | 138 ± 47 |
| HbA1c (%) | 7.2 ± 1.3 |
| LDL-C (mg/dL) | 112 ± 35 |
| HDL-C (mg/dL) | 50 ± 13 |
| TC (mg/dL) | 192 ± 42 |
| TG (mg/dL) | 154 ± 85 |
| Albuminuria (mg/g Cr) | 66.6 ± 249.2 |
Only 31% of patients reached the pre-defined target for LDL-C (< 100 and < 70 mg/dL for patients with coronary heart disease). This proportion was greater (i.e., 40%) for the target of LDL-C < 100 mg/dL and lower (19%) for a more aggressive LDL-C target of < 80 mg/dL (Figure 1). Consequently, the LDL-C target was not reached in the vast majority of patients with coronary heart disease (82%).
The OPTIMISE study is designed to compare two different strategies in the follow-up of type 2 diabetic outpatients regarding the control of diabetes and its concurrent morbidities. Benchmarking is a relatively recent innovation in the quality management sciences, representing a useful tool in the understanding of why there are performance differences between seemingly similar processes[4]. Feedback methods such as benchmarking in which clinicians receive reports of their performance compared with the mean performance of a peer group have been used and studied extensively[3,10]. One underlying theory holds that viewing personal performance within the context of peer performance is a powerful motivator for change[3,11]. In the OPTIMISE study, the hypothesis whether “benchmarking” is superior to a “non-benchmarking” follow-up strategy in the control of diabetes and concurrent morbidities is evaluated.
In the present paper, we discuss baseline characteristics of a relatively large population of type 2 diabetic patients in the Greek region participating in the OPTIMISE study. To the best of our knowledge, this study represents one of the larger diabetes registries in the country.
Type 2 diabetes is becoming an increasingly prevalent morbidity in Greece. In the ATTICA study, the prevalence of diabetes in 3042 subjects who were free of cardiovascular disease was raised from 8% in 2001 to 12.8% in 2006[12]. According to the same study, the age-adjusted five-year incidence of type 2 diabetes was 5.5%[13].
The mean age at diagnosis of diabetes in the OPTIMISE study was 54 years. This finding is in accordance with the “Aegaleo” studies in which the increase in diabetes begins in those > 50 years of age[14]. Interestingly, current data showed clearly that the prevalence is considerably increased after the age of 30 years[15]. Age was found to independently correlate with increased risk for diabetes (OR = 1.07, 95%CI: 1.06-1.08)[15].
In the OPTIMISE study, a mild predominance of the male gender over female was noted. This finding is consistent with epidemiological data from the ATTICA study in which the prevalence of diabetes was higher in men than in women (8% vs 6%, respectively)[16]. Likewise, in another analysis, male gender was recognized as an independent predisposing factor for diabetes (OR = 1.43, 95%CI: 1.04-1.95)[15]. The possible explanation for these sex differences may be that men are more susceptible than women to the consequences of indolence and obesity, possibly due to differences in insulin sensitivity and abdominal fat deposition[17].
Most of our diabetic patients had a positive family history of diabetes. It has been shown that Greek subjects with a positive family history of diabetes may have approximately a seven-fold higher risk for diabetes compared with co-responders without a family history of diabetes[15]. Approximately 1/4 of diabetic patients in our population (i.e., 24%) exhibited coronary heart disease, a proportion which is similar to that reported for the prevalence of diabetes among Greek patients who had suffered a myocardial infarction (i.e., 25%)[18]. Coronary heart disease represented the most prevalent disorder among all macrovascular complications of diabetes, with the rates for other forms of cardiovascular disease being relatively low.
The prevalence of hypertension was high among our subjects. Hypertension was considered as an independent contributing factor for diabetes in Greek adult subjects with self-reported diabetes (OR = 2.19, 95%CI: 1.60-2.99)[15]. The prevalence of hypertension in our population was greater compared with that recorded in an urban Greek population of self-reported diabetes (77% vs 51%, respectively)[15]. The great prevalence of hypertension among Greek subjects with metabolic syndrome (i.e., 71%)[19], which represents a pre-diabetic condition, may account for high rates of hypertension in type 2 diabetic patients.
According to BMI values, approximately all patients were overweight or obese with increased measurements of waist circumference. Being overweight and obese was associated with a two-fold increase in the risk for diabetes in a Greek population[15]. Abdominal obesity, which is present in 82% of patients with metabolic syndrome in Greece[19], may play a major role in the pathogenesis of type 2 diabetes by promoting insulin resistance[20]. Physical inactivity was another important finding of this study. The proportion of our diabetic patients who reported physical inactivity was greater than that recorded in the ATTICA study (77.41% vs approximately 50%, respectively)[19]. This unhealthy lifestyle pattern could be related to the development of obesity and diabetes.
The most important finding of this study lies in the low rates of patients who reached pre-defined targets of treatment for SBP, glycemia and LDL-C levels. Approximately 72% of patients were off target regarding SBP. This rate is in accordance with the Didima study, which shows that only 27% of treated hypertensive subjects reached treatment targets for arterial blood pressure in a rural Greek area[21]. In the EUROASPIRE II study, 50% of patients with coronary heart disease in 15 European countries (including Greece) had raised blood pressure levels[22]. Similar were the results of a Greek trial performed in patients with coronary heart disease of whom only 50% had desirable blood pressure levels[18].
Suboptimal control was noted for LDL-C levels. Seven out of 10 patients did not reach the pre-defined target of LDL-C levels < 100 mg/dL and < 70 mg/dL for diabetic patients with coronary heart disease. This rate was even lower for a more promising target of < 80 mg/dL. Interestingly, this was evident despite high rates of patients who were treated with statins (i.e., 65% of the total study population or 94% of those receiving lipid lowering medications), particularly the most potent ones. Nevertheless, few patients were treated with drugs that could offer further LDL-C lowering, including ezetimibe. Lipid-lowering drug combinations, which are currently underused, could contribute to a greater percentage of patients reaching the targets for LDL-C levels. In the EUROASPIRE II study, 58% of patients with coronary heart disease had elevated TC levels[22]. In Greece, the OLYMPIC study showed that only 26% of 2660 adults with dyslipidemia, who had been receiving lipid-lowering treatment for at least 3 mo (of whom 36% had diabetes), achieved the NCEP-ATPIII targets for LDL-C levels[23]. A greater proportion (i.e., 49%) of patients achieving the 2004-updated NCEP ATPIII targets was reported in the CEPHEUS (Centralized Pan-European survey on the undertreatment of hypercholesterolemia in patients using lipid lowering drugs). This study was performed in 1321 Greek patients who were on lipid lowering treatment for at least 3 mo were stable for at least 6 wk. Interestingly, 25% of these patients had diabetes[23].
In the OPTIMISE study, 34% of the statin-treated patients were on simvastatin, most of them at low doses (49% of them 20 mg/d and 9% 10 mg/d). If these patients were switched to a more potent statin (either atorvastatin or rosuvastatin), they might have reached the targets for LDL-C. Moreover, > 36% of patients on atorvastatin were using low-to-moderate doses (38% of them 10 mg/d and 44% 20 mg/d). It is possible that these patients would reach their targets if titrated to a higher atorvastatin dose or switched to a more potent statin, such as rosuvastatin. Finally, 24% of patients were treated with rosuvastatin (76% of patients used 5-10 mg/d and only 22% 20 mg/d). A higher rosuvastatin dose could potentially offer a higher proportion of patients achieving LDL-C goals. According to international recommendations, statin treatment should be optimized and if the target is not reached, then a second agent should be added. Nevertheless, it appears that statin treatment was far from optimal in the OPTIMISE population. An optimization of statin dose or switching to a more potent statin could help more patients reach the target. If the target is not reached, then the addition of a second agent could be useful.
Poor glycemic control was also noted in our population; only 30% according to fasting PG levels and 50% according to HbA1c levels. The results of the EUROASPIRE II study were similar among diabetic patients with coronary heart disease, with more than 70% being out of target for PG levels[21]. In a Greek population of 819 diabetic patients with coronary heart disease, only half of the patients exerted HbA1c levels < 7.5%[18]. Although insulin is considered as a first-line treatment choice for the management of type 2 diabetic patients, only one fifth of patients in the OPTIMISE study were treated with insulin. This could have attributed to low rates of glycemic control.
The OPTIMISE study was designed to compare the efficacy of “benchmarking” compared with “non-benchmarking” in the control of type 2 diabetes in an outpatient basis. In Greek participants of this study, poor control of diabetes, hypertension and hyperlipidemia were noted at baseline despite treatment.
The optimal type 2 diabetes management including benchmarking and standard treatment (OPTIMISE, NCT00681850) study was a multinational, multicenter study assessing, at a primary care level, whether using benchmarking can help more in improving the quality of patient care as compared with a set of guideline-based reference values.
Benchmarking is practical and action-oriented in its analysis; it is not a rigorous research methodology. It is, however, a promising technology that breaks through the isolation that many clinicians report as the underlying cause of variation in clinical practice.
The OPTIMISE study was designed to compare the efficacy of “benchmarking” compared with “non-benchmarking” in the control of type 2 diabetes on an outpatient basis.
Despite relevant treatment, there is a poor control of diabetes, hypertension and hyperlipidemia in Greek outpatients with type 2 diabetes.
The manuscript is well-written and its aim to confirm the importance of benchmarking to improve diabetes care in clinical setting is of interest.
P- Reviewers: Karadeniz M, Koya D S- Editor: Zhai HH L- Editor: Roemmele A E- Editor: Liu SQ
| 1. | Rydén L, Standl E, Bartnik M, Van den Berghe G, Betteridge J, de Boer MJ, Cosentino F, Jönsson B, Laakso M, Malmberg K. Guidelines on diabetes, pre-diabetes, and cardiovascular diseases: executive summary. The Task Force on Diabetes and Cardiovascular Diseases of the European Society of Cardiology (ESC) and of the European Association for the Study of Diabetes (EASD). Eur Heart J. 2007;28:88-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 411] [Article Influence: 22.8] [Reference Citation Analysis (0)] |
| 2. | Anselmino M, Malmberg K, Mellbin L, Rydén L. Overview of the importance of glycaemic control for cardiovascular events in the in-and out-patient setting. Rev Endocr Metab Disord. 2010;11:87-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Kiefe CI, Allison JJ, Williams OD, Person SD, Weaver MT, Weissman NW. Improving quality improvement using achievable benchmarks for physician feedback: a randomized controlled trial. JAMA. 2001;285:2871-2879. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 318] [Cited by in RCA: 320] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 4. | Loveridge N. Practical benchmarking. Emerg Nurse. 2005;12:12-14. [PubMed] |
| 5. | Cheng AY, Leiter LA. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Curr Opin Cardiol. 2006;21:400-404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 41] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 6. | De Backer G, Ambrosioni E, Borch-Johnsen K, Brotons C, Cifkova R, Dallongeville J, Ebrahim S, Faergeman O, Graham I, Mancia G. European guidelines on cardiovascular disease prevention in clinical practice. Third Joint Task Force of European and Other Societies on Cardiovascular Disease Prevention in Clinical Practice. Eur Heart J. 2003;24:1601-1610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1176] [Cited by in RCA: 1084] [Article Influence: 49.3] [Reference Citation Analysis (0)] |
| 7. | IDF Clinical Guidelines Task Force. Global Guideline for Type 2 Diabetes: recommendations for standard, comprehensive, and minimal care. Diabet Med. 2006;23:579-593. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 297] [Cited by in RCA: 308] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 8. | Nobels F, Debacker N, Brotons C, Elisaf M, Hermans MP, Michel G, Muls E. Study rationale and design of OPTIMISE, a randomised controlled trial on the effect of benchmarking on quality of care in type 2 diabetes mellitus. Cardiovasc Diabetol. 2011;10:82. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Hermans MP, Brotons C, Elisaf M, Michel G, Muls E, Nobels F. Optimal type 2 diabetes mellitus management: the randomised controlled OPTIMISE benchmarking study: baseline results from six European countries. Eur J Prev Cardiol. 2013;20:1095-1105. [PubMed] |
| 10. | Merlani P, Garnerin P, Diby M, Ferring M, Ricou B. Quality improvement report: Linking guideline to regular feedback to increase appropriate requests for clinical tests: blood gas analysis in intensive care. BMJ. 2001;323:620-624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 82] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 11. | Hayes RP, Ballard DJ. Review: feedback about practice patterns for measurable improvements in quality of care--a challenge for PROs under the Health Care Quality Improvement Program. Clin Perform Qual Health Care. 1995;3:15-22. [PubMed] |
| 12. | Panagiotakos DB, Pitsavos C, Chrysohoou C, Skoumas I, Stefanadis C. Prevalence and five-year incidence (2001-2006) of cardiovascular disease risk factors in a Greek sample: the ATTICA study. Hellenic J Cardiol. 2009;50:388-395. [PubMed] |
| 13. | Panagiotakos DB, Pitsavos C, Skoumas Y, Lentzas Y, Stefanadis C. Five-year incidence of type 2 diabetes mellitus among cardiovascular disease-free Greek adults: findings from the ATTICA study. Vasc Health Risk Manag. 2008;4:691-698. [PubMed] |
| 14. | Katsilambros N, Aliferis K, Darviri C, Tsapogas P, Alexiou Z, Tritos N, Arvanitis M. Evidence for an increase in the prevalence of known diabetes in a sample of an urban population in Greece. Diabet Med. 1993;10:87-90. [PubMed] |
| 15. | Gikas A, Sotiropoulos A, Panagiotakos D, Peppas T, Skliros E, Pappas S. Prevalence, and associated risk factors, of self-reported diabetes mellitus in a sample of adult urban population in Greece: MEDICAL Exit Poll Research in Salamis (MEDICAL EXPRESS 2002). BMC Public Health. 2004;4:2. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 39] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 16. | Pitsavos C, Panagiotakos DB, Chrysohoou C, Stefanadis C. Epidemiology of cardiovascular risk factors in Greece: aims, design and baseline characteristics of the ATTICA study. BMC Public Health. 2003;3:32. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 177] [Cited by in RCA: 237] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 17. | Gale EA, Gillespie KM. Diabetes and gender. Diabetologia. 2001;44:3-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 355] [Cited by in RCA: 355] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 18. | Rallidis LS, Zolindaki MG, Chatziioakimidis VK, Velissaridou AH, Konstantellou ES, Papasteriadis EG. High prevalence and suboptimal treatment of risk factors in Greek coronary patients. Acta Cardiol. 2001;56:7-15. [PubMed] |
| 19. | Athyros VG, Ganotakis ES, Bathianaki M, Monedas I, Goudevenos IA, Papageorgiou AA, Papathanasiou A, Kakafika AI, Mikhailidis DP, Elisaf M. Awareness, treatment and control of the metabolic syndrome and its components: a multicentre Greek study. Hellenic J Cardiol. 2005;46:380-386. [PubMed] |
| 20. | Gazi IF, Milionis HJ, Filippatos TD, Tsimihodimos V, Kostapanos MS, Doumas M, Tselepis AD, Elisaf M. Hypertriglyceridaemic waist phenotype criteria and prevalent metabolic triad in women. Diabetes Metab Res Rev. 2008;24:223-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 21. | Stergiou GS, Thomopoulou GC, Skeva II, Mountokalakis TD. Prevalence, awareness, treatment, and control of hypertension in Greece: the Didima study. Am J Hypertens. 1999;12:959-965. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 42] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 22. | EUROASPIRE II Study Group. Lifestyle and risk factor management and use of drug therapies in coronary patients from 15 countries; principal results from EUROASPIRE II Euro Heart Survey Programme. Eur Heart J. 2001;22:554-572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 635] [Cited by in RCA: 642] [Article Influence: 26.8] [Reference Citation Analysis (0)] |
| 23. | Diamantopoulos EJ, Athyros VG, Yfanti GK, Migdalis EN, Elisaf M, Vardas PE, Manolis AS, Karamitsos DT, Ganotakis ES, Hatseras D. The control of dyslipidemia in outpatient clinics in Greece (OLYMPIC) Study. Angiology. 2005;56:731-741. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |