Published online Feb 15, 2012. doi: 10.4239/wjd.v3.i2.29
Revised: January 6, 2012
Accepted: February 8, 2012
Published online: February 15, 2012
AIM: To compare mortality risks associated with known diabetic patients to hyperglycemic non-diabetic patients.
METHODS: PubMed data base was searched for patients with sepsis, bacteremia, mortality and diabetes. Articles that also identified new onset hyperglycemia (NOH) (fasting blood glucose > 125 mg/dL or random blood glucose > 199 mg/dL) were identified and reviewed. Nine studies were evaluated with regards to hyperglycemia and hospital mortality and five of the nine were summarized with regards to intensive care unit (ICU) mortality.
RESULTS: Historically hyperglycemia has been believed to be equally harmful in known diabetic patients and non-diabetics patients admitted to the hospital. Unexpectedly, having a history of diabetes when admitted to the hospital was associated with a reduced risk of hospital mortality. Approximately 17% of patients admitted to hospital have NOH and 24% have diabetes mellitus. Hospital mortality was significantly increased in all nine studies of patients with NOH as compared to known diabetic patients (26.7% ± 3.4% vs 12.5% ± 3.4%, P < 0.05; analysis of variance). Unadjusted ICU mortality was evaluated in five studies and was more than doubled for those patients with NOH as compared to known diabetic patients (25.3% ± 3.3% vs 12.8% ± 2.6%, P < 0.05) despite having similar blood glucose concentrations. Most importantly, having NOH was associated with an increased ICU and a 2.7-fold increase in hospital mortality when compared to hyperglycemic diabetic patients. The mortality benefit of being diabetic is unclear but may have to do with adaptation to hyperglycemia over time. Having a history of diabetes mellitus and prior episodes of hyperglycemia may provide time for the immune system to adapt to hyperglycemia and result in a reduced mortality risk. Understanding why diabetic patients have a lower than expected hospital mortality rate even with bacteremia or acute respiratory distress syndrome needs further study.
CONCLUSION: Having hyperglycemia without a history of previous diabetes mellitus is a major independent risk factor for ICU and hospital mortality.
- Citation: Tayek CJ, Tayek JA. Diabetes patients and non-diabetic patients intensive care unit and hospital mortality risks associated with sepsis. World J Diabetes 2012; 3(2): 29-34
- URL: https://www.wjgnet.com/1948-9358/full/v3/i2/29.htm
- DOI: https://dx.doi.org/10.4239/wjd.v3.i2.29
Small increases in fasting blood glucose concentrations (and A1c levels) have been associated with a significant risk for cardiovascular mortality and all cause mortality[1,2]. For example, a mean fasting blood glucose of 104.5 mg/dL was associated with a 1.19 odds ratio (OR) for all cause mortality (1.05-1.35, P < 0.05)[1]. The OR for mortality was 1.61 (1.35-2.25) when the fasting blood glucose was 113 mg/dL (equilivent to an A1c of 6.1%). Maybe patients at risk for diabetes mellitus have an elevated hospital mortality risk when ill with new onset hyperglycemia (NOH).
Somewhat unexpectedly, mortality in critically ill patients has been reported to be significantly higher in patients without a history of diabetes mellitus compared to patients with diabetes[3-5]. The greater the blood glucose concentration in non-diabetic patients, the greater the mortality[4]. Adults with NOH, defined as a fasting blood glucose > 125 mg/dL or a random blood glucose > 199 mg/dL in non-diabetic individuals was associated with a 3-fold intensive care unit (ICU) and 5-fold increased hospital mortality rate when compared to diabetic patients[6].
Unexpectedly, bacteremic diabetic patients have a lower hospital mortality rate when compared to nondiabetic patients (24.1% vs 44.0%, P < 0.05)[7]. In addition, known diabetic patients with bacteremia are less likely to develop septic shock than non-diabetics (4% vs 13%, P < 0.05), and less well to develop acute renal failure (7% vs 19%, P < 0.05)[7]. The adjusted OR for mortality was 0.47 (0.25-0.88, P < 0.05) for diabetic patients when compared to non-diabetic patients with bacteremia (21.6% vs 37.2%, P < 0.05)[8]. However, not all studies have demonstrated a reduced mortality in diabetics with bacteremia. For example, one study (n = 1112) demonstrated a slight reduction in hospital mortality rate (8.2% vs 7.2%, P = 0.39, non-diabetics vs diabetics)[9]. The similar or reduced mortality in bacteremic diabetic patients was unexpected and may be secondary to the patients previous exposure to hyperglycemia (recent exposure raising the mortality risk and more chronic exposure potentially blunting the acute deleterious effects of hyperglycemia on septic mortality). Other studies have seen dramatic differences in ICU mortality rates when groups have been identified as having NOH as compared to patients with established diabetics mellitus[6,10-17].
The reason for apparently reduced mortality in hospitalized patients with diabetes mellitus is unknown. Potentially, a sudden increase in blood glucose concentration with acute illness observed in the prediabetic patient (A1c 5.5% to 6.4%) may produce dysregulation of the immune system and serious consequences of infection prevail. An alternative explanation could be related to potential benefits of traditional medication given to the diabetics as an outpatient (Statins, ACE, Aspirin, etc.) which may help reduce inpatient mortality. The purpose of this study was to identify if having diabetes with previous hyperglycemia or having NOH alters ICU and hospital mortality risk.
All Pubmed references up to January 2012 were searched for all articles associated with key words of mortality and hyperglycemia. Manuscripts were excluded if they involved acute trauma, ACS, MI, CHF, CVA and pediatrics. Selection criteria required reporting three groups: (1) data meeting criteria for NOH; (2) normal glycemia; and (3) diabetes mellitus as separate groups. A few papers using the cutoff of 180 mg/dL were identified and excluded from the analysis.
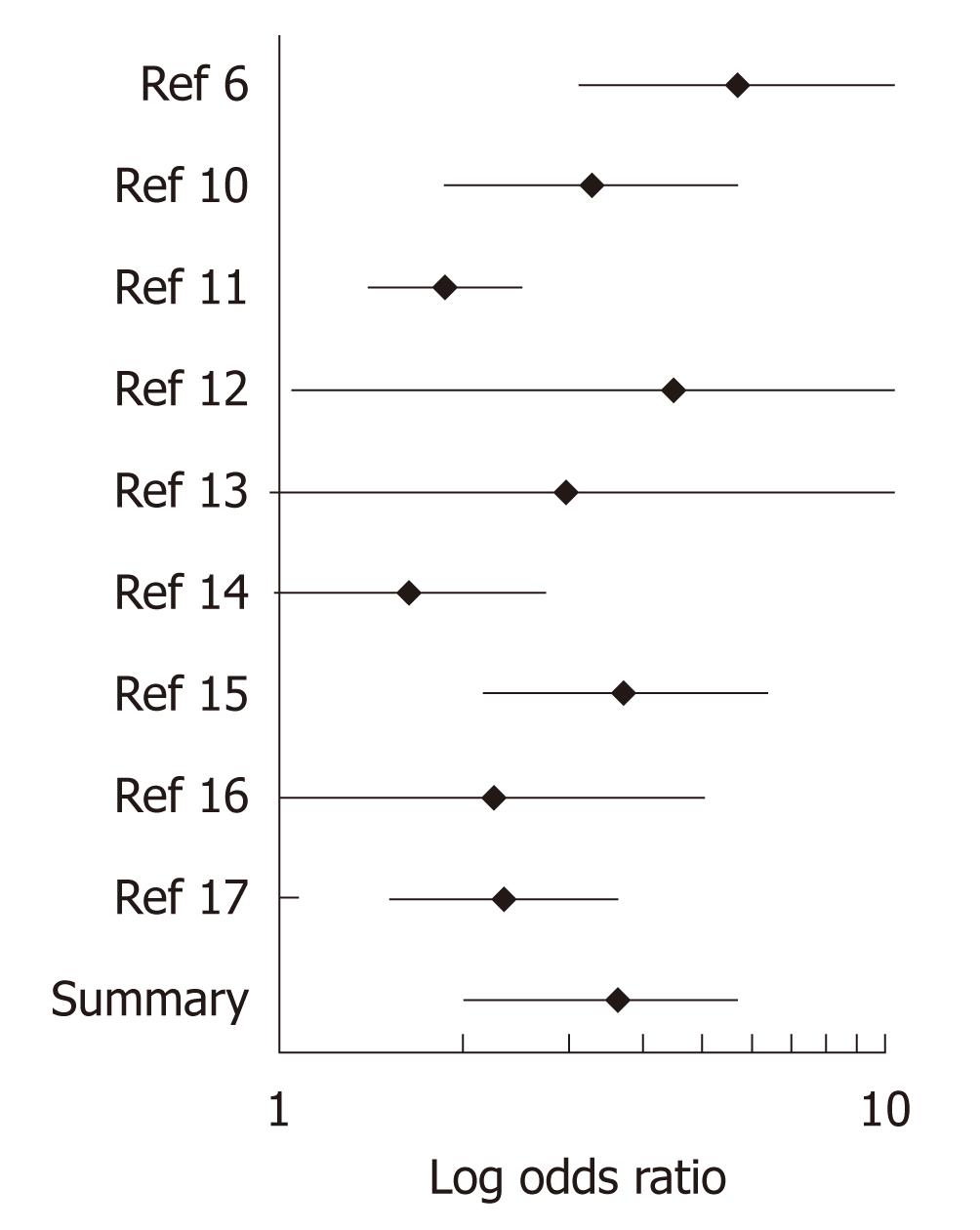
Eight research papers were identified that met inclusion criteria. A ninth research paper met inclusion criteria after personal communications with the author and the author’s permission to include the data provided (Person Communications March 2010)[10]. Primary endpoints were NOH (fasting blood glucose > 125 mg/dL or > 199 mg/dL twice; History of diabetes and normal glycemia. Unadjusted mortality data was obtained and compared between the three groups by analysis of variance (ANOVA). Meta analysis was obtained using the BioStat program. Figure 1 demonstrates a weighted summary log transformed statistics for the analysis of the nine studies. Data analysis was reported as mean ± SE. Significance was defined as a P < 0.05.
Nine studies of 20 966 patients demonstrated that NOH was seen in approximately 17% (range 2%-31%) of the patients admitted to the hospital. A history of diabetes was seen in 23.9% of patients admitted to the hospital. Therefore, approximately 59% of patients were admitted without NOH or history of diabetes.
ICU mortality was evaluated in five studies (Table 1). ICU mortality was more than doubled for those patients with NOH as compared to diabetic patients (25.3% ± 3.3% vs 12.8% ± 2.6%, P < 0.05). ICU mortality was similar between diabetics and normal glycemic non-diabetics (Table 1).
Hospital mortality is summarized in Table 2. Hospital mortality was significantly increased in all nine studies of patients with NOH as compared to known diabetic patients (26.7% ± 4.4% vs 12.5% ± 3.4%, P < 0.05; ANOVA). Mortality in patients with an admission history of diabetes was similar to those patients with normal glycemia (Table 2). Meta-analysis demonstrated an increased OR for mortality in patients with NOH (OR = 2.71, 95% CI: 2.03-3.61, P < 0.001). Figure 1 demonstrates a weighted summary statistics for the analysis of the nine studies. Using meta-analysis, a significant increase in mortality was seen for seven of the nine studies of patients with NOH compared to diabetic patients.
| NOH (%) | Known history of diabetes (%) | Hospitalized patients without NOH (%) | Sample size (n) | Patients diagnosis | Ref. |
| 16.0 | 3.0a | 1.7a | 2030 | Hospital | [6] |
| 15.2 | 5.2ac | 8.3a | 27131 | ICU | [10] |
| 10.0 | 5.6a | 5.2a | 7285 | ICU | [11] |
| 43.8 | 14.8ac | 5.3a | 62 | Hospital | [12] |
| 27.4 | 10.6a | 13.7a | 189 | ICU | [13] |
| 43.0 | 31.4a | 27.2a | 830 | ICU | [14] |
| 19.6 | 6.1a | 3.9a | 6367 | Hospital | [15] |
| 42.5 | 24.6a | 13.7a | 265 | Hospital | [16] |
| 23.2 | 11.4a | 11.2a | 1155 | Hospital | [17] |
| mean ± SE 26.7 ± 4.4 | 12.5 ± 3.4a | 10.0 ± 2.8a | 20 966 |
Having a history of diabetes prior to admission to the hospital, where the hyperglycemia is not new, may be a protective factor in that your immune system may have adapted to the hyperglycemia over time. In fact, in over 10 million patients, diabetic patients had a reduced hospital mortality when compared to non-diabetic patients OR of 0.87, 95% CI: 0.83-0.91, P < 0.001[5]. Unfortunately, blood glucose concentration was not reported in this study to identify if the greater mortality in the non-diabetic patients was due to some 20% of the patients with NOH and greater mortality risk.
Fortunately, a recent study has evaluated the role of hyperglycemia in non-diabetic patients. Hospital mortality was significantly increased at all mean blood glucose ranges (111-145, 146-199, 200-300 and > 300 mg/dL) in non-diabetic patients when compared to diabetic patients[4]. While these authors did not focus on admission blood glucose concentration, a similar relationship between admission blood glucose and mortality was seen by Cheung[15]. For example, OR adjusted mortality was doubled for non-diabetic patients compared to diabetic patients with an admission blood glucose between 144-179 mg/dL[15]. Unfortunately, blood glucose concentrations alone may not be a great marker of systemic injury in diabetic patients since diabetic patients have varying degrees of insulin deficiency in that a higher blood glucose observed in a diabetic patient may not reflect a greater injury but a longer duration of diabetes and less β cell function (for type 2 diabetes).
Dissecting the acuteness of hyperglycemia provides new identifiable risk factors with regards for diabetic status and NOH. The enclosed data demonstrates a protective role that hyperglycemic diabetics patients may have when they are hospitalized. Diabetic patients are less likely to develop acute respiratory distress syndrome (ARDS) than patients without diabetes[18]. Only 25% of diabetic patients with septic shock develop ARDS as compared to 47% in non-diabetic patients in septic shock. Even after adjustment of several risk factors for the development of ARDS, diabetic patient have an OR of 0.33 (90% CI: 0.12-0.90, P < 0.05) for the development of ARDS[18]. One explanation for this unexpected finding is that mortality may be increased in the non-diabetic group because approximately 1/5) of these patients will have NOH which may promote the inflammatory response (or prevent that anti-inflammatory response such as seen with glucocorticoid therapy).
The incidence of NOH is common in hospitalized patients and may develop from the common finding of prediabetes in the developed world population. NOH has been reported to occur in 12% of hospitalized patients[4,6] and approximately 27% of ICU patients[6,10]. We found in this review that NOH occurs in approximately 17% of all admissions. NOH was seen in those patients that had a mildly increased A1c concentration (5.7% ± 0.3%)[16] upon admission. Mortality is higher in a non-diabetic hyperglycemic patient with an A1c > 5.4%[1]. In addition, this association suggests that mild elevation in A1c measurement (similar to what is now being call pre-diabetes) might account for a large portion of patients admitted with NOH. Furthermore, the increasing incidence of abnormal A1c levels in the world will likely contribute to a greater number of hospital admissions of non-diabetic patients with NOH.
There are several other explanations as to why diabetic patients have a reduced mortality when compared to patients without a history of diabetes who develop hyperglycemia due to injury. Many diabetic patients admitted to the hospital have recently been taking cardioprotective medications. Guidelines suggest that diabetics routinely be provided medications that impact on survival (HMG CoA reductase inhibitors, ACE, ARB, asprin and calcium channel blockers). For example, mortality is significantly reduced in bacteremic patients who had previously been treated with HMG CoA reductase inhibitor therapy[19-22]. The attributable mortality was reduced from 20% to 3% in one study[19] and hospital mortality was reduced from 23.1% to 10.6% in a second study (OR 0.39, 95% CI: 0.17-0.91, P < 0.05)[20]. Furthermore, if HMG CoA reductase inhibitor therapy was continued during the hospital stay, the OR for mortality was greatly reduced (0.06; 95% CI: 0.01-0.44, P < 0.01)[20]. Even if prior HMG CoA reductase inhibitor therapy was stopped upon admission to the hospital, a mortality benefit persisted (0.37 risk adjusted OR, P < 0.05)[21].
Prior ACE therapy[19] or ARB therapy[22] appear to have similar mortality benefits in users as compared to non-users. Diabetic patients undergoing renal transplant have a reduced mortality if they had been given β-blocker and calcium channel blocker medications (mean survival of 72.5 mo vs 36.8 mo, P < 0.005)[23].
An additional possibility for the observed lower mortality rate in patients with diabetes may be due to the fact that they likely receive insulin administration sooner than those with NOH. An emergency room physician may be more inclined to administer insulin sooner to a patient with a history of diabetes than non-diabetic patients. Paradoxically, critically ill non-diabetic patients provided intravenous insulin demonstrated a mortality benefit over that seen in diabetic patients[24].
Potential risk factors are many that may be contributory for specific diagnosis that may explain why one observes an increase mortality risk in hospitalized patients with NOH. Acute hyperglycemia increases risk for mortality from pneumonia in non-diabetic patients with a 30-d average blood glucose concentration above 109 mg/dL[25]. For example, the OR for mortality was 1.43 with a 30-d mean blood glucose concentration between 110-198 mg/dL, 1.65 between 199-252 mg/dL and 1.91 for a concentration greater than 252 mg/dL (all P < 0.05). In contrast, diabetic patients failed to have a significant increase in mortality (OR of 0.96; NS) with a blood glucose between 110 mg/dL and 198 mg/dL. Consistent with the diabetic protective effect, the OR was also not significant for diabetic patients with regards to mortality risk even with a mean blood glucose concentration between 199 mg/dL and 252 mg/dL (OR of 1.24; NS). This appears counter-intuitive but acuteness of the hyperglycemia (within a few days or weeks) may play a pivotal role in septic mortality risk. Unfortunately the mechanism is not known.
In this group of community acquired pneumonia patients, mortality was only increased in diabetic patients with the highest blood glucose, an average blood glucose > 252 mg/dL (OR = 1.43, P < 0.05). The higher glucose threshold for an increase in mortality risk seen in established diabetic patients suggest that they their body’s immune system may adapt to hyperglycemia over time. Consistent with this is the fact that bacteremia and fungemia are much more common in patients with NOH. The OR was 4.2-fold increased (1.5-12, P < 0.05) for development of bacteremia or fungemia in chemotherapy patients who also had acute hyperglycemia[26]. While none of the bacteremia studies use the criteria for the diagnosis of NOH, mortality was increased 3-fold in patients with a blood glucose > 170 mg/dL compared to patients with a lower blood glucose concentration[27]. This suggests that acute elevations in blood glucose concentration below the 199 mg/dL cutoff for the criteria of NOH may also carry additional mortality risk.
Increased mortality may also be related to cardiac function during illness. For example, the electrical conduction pathway is altered by acute hyperglycemia that may not be seen in diabetic patients who have many hyperglycemic episodes. Acute hyperglycemia prolongs both QT interval and QTc dispersion in diabetic patients and in acute hyperglycemic patients. However, the prolonged QTc dispersion does not rapidly recover in acute hyperglycemia. QTc dispersion recovers normally in diabetic patients[28]. An alternative hypothesis worth testing is to see if an increased QTc dispersion may contribute to mortality risk seen in those patients with NOH due to illness (infection, sepsis, etc.).
Lastly, coronary artery plaque instability may be a reason for increased mortality risk. One earlier study showed that normal volunteers had acute hyperglycemia which blunted the optimal response to injury by reducing MMP-3 concentration and altering plaque stability[29]. Elevated blood glucose concentration may contribute to coronary and carotid plaque rupture. While cytokine levels (tumor necrosis factor-α, IL-6) are similar in both diabetic and non-diabetic septic patients, there is a significant reduction in anticoagulants seen in non-diabetic patients[14]. The lower concentrations of Protein S and Antithrombin may contribute to an alteration in the normal coagulation profile and promote coronary plaque unstability.
In summary, in someone who is hyperglycemic, having a history of diabetes mellitus appears to lower one’s risk for hospital and ICU mortality. The exact mechanism behind this is unknown but may likely be due to the body’s ability to adapt to hyperglycemia over an extended period of time. In comparison, developing NOH in adults increased the OR for mortality by 2.7-fold. Since recent clinical trials of intravenous insulin treatment have failed to confirm a mortality benefit in all ICU patients[24,30], and it may even show harm[30], studies to test the benefits in a more select group of patients seems warranted.
Recent recommendations have increased target blood glucose goals in hospitalized patients due to the lack of evidence associated with aggressive insulin treatment. Unfortunately, none of the earlier studies have evaluated the benefit of intravenous insulin treatment in patients with NOH)[30]. The median blood glucose for treated patients was 144 mg/dL)[30]. Since the mortality risk is increase 2.7-fold greater in patients with NOH as compared to diabetic patients it would seem rational to test the benefits of early aggressive insulin treatment in this select group of non-diabetic patients. Furthermore, it would seem equally important to identify risk factors for those who are at risk to develop NOH. Some of these risk factors include: family history of diabetes, metabolic syndrome, impaired fasting glucose or an A1c concentration consistent with the diagnosis of pre-diabetes (5.5%-6.4%). As of 2012, the ADA recomends an A1c measurement as part of the admission labs to hospital. Septic patients in the ER with NOH have recently been shown to have 2.1 fold OR for mortality as compared to known diabetics with similar blood glucose concentration[31]. Identifying NOH will identify patients with a high mortality risk.
Diabetes is known to increase the risk for multiple infections with serious infections a common reason for hospital admission. Some patients without diabetes when they become ill also have elevated blood glucose concentrations due to illness that are similar to the concentration seen in patients with diabetes. For example, a random blood glucose above 199 mg/dL is not uncommon in hospitalized patients with and without diabetes. The elevated blood glucose in the non-diabetic patient is likely due to the patient having prediabetes. Prediabetes is defined as someone having a fasting blood glucose between 100 mg/dL and 125 mg/dL. Approximately 20% of the US population is considered to have pre-diabetes. It is possible that a large proportion of pre-diabetic patients who are hospitalized develop an elevated blood glucose concentration above 199 mg/dL. The novel and acute elevated in blood concentration likely reduces the persons’ immune response to fight infection which would explain the 2.7-fold observed increase in mortality as compared to diabetic patients with a similar blood glucose concentration.
Understanding the immunological reason for the greater mortality in patients with new onset hyperglycemia (NOH) is paramount. While it is well known that neutorphill phagocytosis is reduced at elevated blood glucose concentrations other critical immune functions may be reduced with acute hyperglycemia. Research to identify those factors is needed.
The breakthrough has begun with the use of this knowledge to help identify seven additional studies that have demonstrated a higher mortality risk in patients with NOH as compared to patients with known diabetic mellitus. Using this information in the emergency room or after surgery may identify patients at very high mortality risk as compared to patients without an elevated blood glucose concentration.
This study established the criteria for the diagnosis of NOH which will become an important marker of hospital mortality risk. In addition, it will help direct new research into testing benefits of treatment of hyperglycemia in non-diabetic patients. An ICD9 code should be established for the diagnosis of NOH.
NOH is defined as two fasting blood glucose concentrations greater than 125 mg/dL or two non-fasting glucose concentrations above 199 mg/dL or one of each. This criteria, while used on an out patient bases for the diagnosis of diabetes mellitus, does not make the diagnosis of diabetes mellitus in the inpatients setting due to the fact that illness is known to increase blood glucose concentrations due to an increase in the stress hormones (cortisol, GH, Catacholamines, Glucagon). The reason why the blood glucose increases greater than 199 mg/dL with illness is likely due to the patient have pre-diabetes.
This is a good descriptive in which the authors analyze the association between blood glucose concentration and whether the patient has had a history of hyperglycemia in the past or NOH. Historically, blood glucose concentrations were perceived to be of equal risk when seen in a hospitalized patient. These authors support the hypothesis that NOH has a very high mortality risk as compared to hyperglycemia that may be more chronic as seen in many diabetic patients. The results of the study demonstrate that all the research trials have demonstrated a similar trend and that seven of the nine trials have a significant increase in hospital or intensive care unit mortality was observed in patients with NOH.
Peer reviewer: Semir Ozdemir, Associate Professor, Department of Biophysics, Faculty of Medicine, Akdeniz University, Antalya 07058, Turkey
S- Editor Wu X L- Editor A E- Editor Zheng XM
| 1. | Selvin E, Steffes MW, Zhu H, Matsushita K, Wagenknecht L, Pankow J, Coresh J, Brancati FL. Glycated hemoglobin, diabetes, and cardiovascular risk in nondiabetic adults. N Engl J Med. 2010;362:800-811. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1161] [Cited by in RCA: 1093] [Article Influence: 72.9] [Reference Citation Analysis (0)] |
| 2. | Barr EL, Boyko EJ, Zimmet PZ, Wolfe R, Tonkin AM, Shaw JE. Continuous relationships between non-diabetic hyperglycaemia and both cardiovascular disease and all-cause mortality: the Australian Diabetes, Obesity, and Lifestyle (AusDiab) study. Diabetologia. 2009;52:415-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 130] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 3. | Graham BB, Keniston A, Gajic O, Trillo Alvarez CA, Medvedev S, Douglas IS. Diabetes mellitus does not adversely affect outcomes from a critical illness. Crit Care Med. 2010;38:16-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 97] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 4. | Falciglia M, Freyberg RW, Almenoff PL, D'Alessio DA, Render ML. Hyperglycemia-related mortality in critically ill patients varies with admission diagnosis. Crit Care Med. 2009;37:3001-3009. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 442] [Cited by in RCA: 391] [Article Influence: 24.4] [Reference Citation Analysis (0)] |
| 5. | Martin GS, Mannino DM, Moss M. The effect of age on the development and outcome of adult sepsis. Crit Care Med. 2006;34:15-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 764] [Cited by in RCA: 665] [Article Influence: 35.0] [Reference Citation Analysis (0)] |
| 6. | Umpierrez GE, Isaacs SD, Bazargan N, You X, Thaler LM, Kitabchi AE. Hyperglycemia: an independent marker of in-hospital mortality in patients with undiagnosed diabetes. J Clin Endocrinol Metab. 2002;87:978-982. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 329] [Cited by in RCA: 233] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 7. | Akbar DH. Adult bacteremia. Comparative study between diabetic and non-diabetic patients. Saudi Med J. 2000;21:40-44. [PubMed] |
| 8. | Greenberg BM, Atmar RL, Stager CE, Greenberg SB. Bacteraemia in the elderly: predictors of outcome in an urban teaching hospital. J Infect. 2005;50:288-295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 32] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 9. | Peralta G, Sánchez MB, Roiz MP, Garrido JC, Teira R, Mateos F. Diabetes does not affect outcome in patients with Enterobacteriaceae bacteremia. BMC Infect Dis. 2009;9:94. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Whitcomb BW, Pradhan EK, Pittas AG, Roghmann MC, Perencevich EN. Impact of admission hyperglycemia on hospital mortality in various intensive care unit populations. Crit Care Med. 2005;33:2772-2777. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 158] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 11. | Rady MY, Johnson DJ, Patel BM, Larson JS, Helmers RA. Influence of individual characteristics on outcome of glycemic control in intensive care unit patients with or without diabetes mellitus. Mayo Clin Proc. 2005;80:1558-1567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 143] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 12. | Cheung NW, Napier B, Zaccaria C, Fletcher JP. Hyperglycemia is associated with adverse outcomes in patients receiving total parenteral nutrition. Diabetes Care. 2005;28:2367-2371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 151] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 13. | Wasmuth HE, Kunz D, Graf J, Stanzel S, Purucker EA, Koch A, Gartung C, Heintz B, Gressner AM, Matern S. Hyperglycemia at admission to the intensive care unit is associated with elevated serum concentrations of interleukin-6 and reduced ex vivo secretion of tumor necrosis factor-alpha. Crit Care Med. 2004;32:1109-1114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 49] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 14. | Stegenga ME, Vincent JL, Vail GM, Xie J, Haney DJ, Williams MD, Bernard GR, van der Poll T. Diabetes does not alter mortality or hemostatic and inflammatory responses in patients with severe sepsis. Crit Care Med. 2010;38:539-545. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 94] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 15. | Cheung NW, Li S, Ma G, Crampton R. The relationship between admission blood glucose levels and hospital mortality. Diabetologia. 2008;51:952-955. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 16. | Leonidou L, Michalaki M, Leonardou A, Polyzogopoulou E, Fouka K, Gerolymos M, Leonardos P, Psirogiannis A, Kyriazopoulou V, Gogos CA. Stress-induced hyperglycemia in patients with severe sepsis: a compromising factor for survival. Am J Med Sci. 2008;336:467-471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 47] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 17. | Sleiman I, Morandi A, Sabatini T, Ranhoff A, Ricci A, Rozzini R, Trabucchi M. Hyperglycemia as a predictor of in-hospital mortality in elderly patients without diabetes mellitus admitted to a sub-intensive care unit. J Am Geriatr Soc. 2008;56:1106-1110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 43] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 18. | Moss M, Guidot DM, Steinberg KP, Duhon GF, Treece P, Wolken R, Hudson LD, Parsons PE. Diabetic patients have a decreased incidence of acute respiratory distress syndrome. Crit Care Med. 2000;28:2187-2192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 176] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 19. | Liappis AP, Kan VL, Rochester CG, Simon GL. The effect of statins on mortality in patients with bacteremia. Clin Infect Dis. 2001;33:1352-1357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 251] [Cited by in RCA: 249] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 20. | Kruger P, Fitzsimmons K, Cook D, Jones M, Nimmo G. Statin therapy is associated with fewer deaths in patients with bacteraemia. Intensive Care Med. 2006;32:75-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 162] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 21. | Almog Y, Novack V, Eisinger M, Porath A, Novack L, Gilutz H. The effect of statin therapy on infection-related mortality in patients with atherosclerotic diseases. Crit Care Med. 2007;35:372-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 70] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 22. | Mortensen EM, Restrepo MI, Copeland LA, Pugh JA, Anzueto A, Cornell JE, Pugh MJ. Impact of previous statin and angiotensin II receptor blocker use on mortality in patients hospitalized with sepsis. Pharmacotherapy. 2007;27:1619-1626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 59] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 23. | Weinrauch LA, D'Elia JA, Gleason RE, Shaffer D, Monaco AP. Role of calcium channel blockers in diabetic renal transplant patients: preliminary observations on protection from sepsis. Clin Nephrol. 1995;44:185-192. [PubMed] |
| 24. | Krinsley JS. Glycemic control, diabetic status, and mortality in a heterogeneous population of critically ill patients before and during the era of intensive glycemic management: six and one-half years experience at a university-affiliated community hospital. Semin Thorac Cardiovasc Surg. 2006;18:317-325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 111] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 25. | Kornum JB, Thomsen RW, Riis A, Lervang HH, Schønheyder HC, Sørensen HT. Type 2 diabetes and pneumonia outcomes: a population-based cohort study. Diabetes Care. 2007;30:2251-2257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 175] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 26. | Sonabend RY, McKay SV, Okcu MF, Yan J, Haymond MW, Margolin JF. Hyperglycemia during induction therapy is associated with increased infectious complications in childhood acute lymphocytic leukemia. Pediatr Blood Cancer. 2008;51:387-392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 32] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 27. | Bader MS. Hyperglycemia and mortality in elderly patients with Staphylococcus aureus bacteremia. South Med J. 2007;100:252-256. [PubMed] |
| 28. | Gordin D, Forsblom C, Rönnback M, Groop PH. Acute hyperglycaemia disturbs cardiac repolarization in Type 1 diabetes. Diabet Med. 2008;25:101-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 37] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 29. | Death AK, Fisher EJ, McGrath KC, Yue DK. High glucose alters matrix metalloproteinase expression in two key vascular cells: potential impact on atherosclerosis in diabetes. Atherosclerosis. 2003;168:263-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 181] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 30. | Finfer S, Chittock DR, Su SY, Blair D, Foster D, Dhingra V, Bellomo R, Cook D, Dodek P, Henderson WR. Intensive versus conventional glucose control in critically ill patients. N Engl J Med. 2009;360:1283-1297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3409] [Cited by in RCA: 3186] [Article Influence: 199.1] [Reference Citation Analysis (0)] |
| 31. | Schuetz P, Jones AE, Howell MD, Trzeciak S, Ngo L, Younger JG, Aird W, Shapiro NI. Diabetes is not associated with increased mortality in emergency department patients with sepsis. Ann Emerg Med. 2011;58:438-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 36] [Article Influence: 2.6] [Reference Citation Analysis (0)] |