INTRODUCTION
Diabetic nephropathy is considered to be one of the major complications of diabetes mellitus and its prevalence is continuously progressing worldwide. Progression of this disease is further accelerated by the partial or complete contribution of various factors, such as hypertension, chewing tobacco, alcoholism and smoking. Predominantly, nicotine exposure via chronic cigarette smoking is an emerging cause that accelerates the microvascular complications in diabetes mellitus[1]. The pathophysiological mechanisms underlying the health effects of cigarette smoking in diabetes are complex. Diabetic smokers are usually associated with glomerular hypertrophy, glomerulosclerosis, tubulointerstitial fibrosis and mesangial cell expansion, followed by albuminuria and reduction in the glomerular filtration rate[2,3]. Thus, establishing the causes of smoking mediated progression of diabetic nephropathy remains the key step towards the prevention and amelioration of this disease.
In diabetic microvasculature, a high level of glucose probably synergizes with superimposed stresses such as oxidative stress and hyperlipidemia to continue the stress on vascular cells, which is further increased by smoking. The potential risk factors involved in the progression of diabetic nephropathy remain unclear, although smoking mediated hastening of oxidative stress and hyperlipidemia play partial but key roles in this. Chronic and uncontrolled diabetes mellitus is often coupled with oxidative stress, a risk factor for diabetic microvascular complications. Furthermore, nicotine (an active constituent of a cigarette) exposure is noted to promote excessive oxidative stress in diabetes[3]. Together, diabetes and smoking mediated increased oxidative stress subsequently leads to vascular endothelial cell dysfunction (VED), which is one of the earliest metabolic consequence of chronic hyperglycemia[3-5]. In addition to this, both hyperglycemia and smoking (nicotine) downregulates endothelial nitric oxide synthase (eNOS), an enzyme involved in the generation of NO, decreases endothelium dependent vasodilation and results in VED, which is subsequently involved in the pathogenesis of diabetic nephropathy[5-7]. Evidently, diabetes mediated oxidative stress upregulates the expression of transforming growth factor-β (TGF-β), a prosclerotic and profibrogenic cytokine, which again is implicated in the pathogenesis of nephropathy[8,9]. Similarly, nicotine has also been noted to upregulate the expression of TGF-β and is involved in the pathogenesis of diabetic nephropathy[8]. Thus, TGF-β is considered to be another common pathway for diabetes and smoking to worsen the nephropathy.
Hyperlipidemia is considered another major risk factor implicated in the progression of diabetic nephropathy[10]. Dyslipidemia is a condition associated with hypertriglyceridemia, elevated low density lipoprotein (LDL) levels and decreased high density lipoprotein (HDL) levels. Diabetes mediated hyperlipidemia is noted to be responsible for the progression of nephropathy in rats[5]. The astonishing fact is that nicotine causes an impairment of lipoprotein lipase (LPL), an enzyme involved in the hydrolysis and clearance of triglyceride (TG) from the circulation, and thus causes hyperlipidemia[11,12]. Furthermore, smokers have higher serum concentrations of TG and LDL and lower serum concentrations of HDL compared with non-smokers[13]. This indicates that smoking independently contributes to hyperlipidemia and/or dyslipidemia-like conditions. Although the precise mechanism involved in diabetes-associated dyslipidemia is not clear, the insulin resistance in type II diabetes mellitus could play a key role in elevating lipid levels[2,10]. In diabetic patients, high lipids could induce renal injury by stimulating TGF-β and thereby inducing the generation of reactive oxygen species (ROS) to damage the glomeruli, showing that diabetic hyperlipidemia accelerates reno-vascular complications[10]. Cigarette smoking associated hyperlipidemia has been identified as a progression factor in the development of diabetic reno-vascular complications[14]. A study illustrated that diabetes mellitus may mediate renal injury by increasing the renal expression of sterol regulatory element-binding protein-1 (SREBP-1), which is responsible for increasing the synthesis of TGs and cholesterol, that are further associated with upregulation of TGF-β and could play a pivotal role in the pathogenesis of glomerulosclerosis and tubulointerstitial fibrosis[15]. One potential explanation for supporting the intricate effects of nicotine is that smoking stimulates renal lipid accumulation by increasing expression of SREBP-1, which increases the synthesis of TGs and cholesterol[16]. In addition to this, diabetes mediated activation of Rho-kinase and advanced glycation end products (AGEs)-like factors also participate in the pathogenesis of nephropathy[17,18]. Taken together, it could be indubitably suggested that cigarette smoking could induce and worsen diabetic nephropathy. Therefore, initial interest focuses on strict glycemic control and subsequently smoking secession. Thus, identifying the major culprits and path of their involvement in the pathogenesis of diabetic nephropathy may open a vista in exploring novel therapeutic agents to ameliorate the induction and progression of this disease.
OPTIMISTIC CONTRIBUTION OF DIABETIC OXIDATIVE STRESS AND HYPERLIPIDEMIA IN THE DEVELOPMENT OF NEPHROPATHY
In diabetes, chronic hyperglycemia is the single most important factor in the generation of sustained oxidative stress. Under normal physiological conditions, a homeostatic balance exists between the formation of ROS and their removal by endogenous antioxidant compounds. However, oxidative stress occurs when this balance is disrupted by excessive production of ROS and decreasing endogenous antioxidants, probably due to chronic hyperglycemia[19,20]. ROS encompasses diverse chemical species, including superoxide or hydroxyl, are produced by oxygen metabolism and play a major part in cell signaling, aging and microvascular diseases[21]. ROS acts as intracellular messengers and integral glucose signaling molecules in the diabetic kidney. The metabolism of glucose through harmful alternate pathways, such as glycolysis, specific defects in the polyol pathway, nicotinamide adenine dinucleotide phosphate (NADPH) oxidase, advanced glycation and uncoupling of nitric oxide synthase, are mainly responsible to generate ROS[9]. In physiology, the unused glucose in the cytosol is diverted to the polyol pathway, where the aldose reductase reduces it to sorbitol by utilizing cofactor NADPH from the pentose phosphate pathway. In addition, chronic hyperglycemia causes excessive consumption of NADPH in the polyol pathway and the net effect is the generation of ROS[21].
Most estimates suggest that the excessive generation of ROS in diabetes precedes endothelial dysfunction by decreasing eNOS expression and decreasing NO production[5,19,22,23]. Thus, the impaired ability of endothelial cells to modulate the vascular tone is a result of low bioavailability of nitric oxide in the vascular lumen. Furthermore, in diabetes, low levels of nitric oxide in endothelial cells may potentially result in ineffective suppression of ROS and could indirectly lead to enhanced vasoconstriction. This contention was further confirmed in subsequent in vitro and in vivo studies, which explains the enhancement in superoxide generation that ultimately increases endothelin-I production in diabetic rat glomeruli[24]. These alterations of nitric oxide metabolism promote oxidative stress, particularly in the diabetic renal milieu (glomerular and tubulointerstitial cells)[25]. In support of these claims, oxidative stress coupled with chronic hyperglycemia may have an important role in the pathogenesis of glomerular and tubular functional and structural abnormalities [20].
Cavernous mechanism often pertains in the development of oxidative stress. In diabetes, intricate mechanisms are involved in the promotion of oxidative stress. NADPH oxidase is the major source for superoxide generation. NADPH oxidase is located in the plasma membrane of various cells, including renal endothelial cells, fibroblast mesangial cells, proximal tubular cells and vascular smooth muscle cells[26]. Furthermore, in the diabetic rat, the stimulation of expression of NADPH oxidase was noted to be increased in the kidney and NADPH oxidase dependent overproduction of ROS plays a key role in the induction of renal hypertrophy and nephropathy[23,27]. Intriguingly, activation of glomerular SREBP-1 increases NADPH oxidase-mediated ROS production, which further progresses diabetic nephropathy[28]. Thus, this evidence suggests a possible pathological role of NADPH in diabetic nephropathy. Enhanced oxidative stress has been shown to activate TGF-β, which regulates the extracellular matrix remodeling in the mesangial cells[29]. It is plausible that diabetes mediated oxidative stress activates TGF-β and could play a role in the development of the characters of diabetic nephropathy[20,30]. In the case of signaling kinases, protein kinase C (PKC) is considered to be the central culprit involved diversely to the pathogenesis of diabetic nephropathy[31]. Evidently, involvement of PKC is further confirmed by the treatment with ruboxistaurin, a specific PKC inhibitor, which prevented the development of diabetes-induced nephropathy by reducing the increased mRNA expression of TGF-β1 and fibronectin[32]. Therefore, in diabetes, NADPH oxidase acts as an engine for the generation of oxidative stress and oxidative stress mediated TGF-β initiates secondary microvascular complications.
Dyslipidemia is a condition associated with hypertriglyceridemia, elevated LDL levels and decreased HDL levels[10]. The association between hyperglycemia and lipid accumulation is a hall mark of diabetic nephropathy. Insulin resistance in diabetes is the initial step in the formation of dyslipidemia[33]. Furthermore, dyslipidemia has been suggested as an independent risk factor for the development and progression of diabetic nephropathy[34]. This indicates that insulin resistance/hyperinsulinemia is a primary cause of diabetic dyslipidemia. Thus, patients with diabetic nephropathy often have multiple lipoprotein abnormalities[35]. However, two key mechanisms explain the association between diabetes mellitus and hyperlipidemia. Firstly, insulin deficiency downregulates the LPL, an enzyme involved in the hydrolysis and clearance of TGs from the circulation[36]. Secondly, insulin has an inhibitory action on 3-hydroxy-3-methyl-glutaryl-Co-A (HMG-COA) reductase, a key rate limiting enzyme involved in the synthesis of cholesterol[37]. Jointly, it is possible that hypoinsulinemia during long term diabetes downregulates LPL and activates the HMG-COA reductase pathway and might play a role in excessive lipid accumulation during early stages of diabetic nephropathy. The strong correlation between diabetic-endothelial dysfunction and nephropathy has been demonstrated in various studies[5,38,39]. Worthy of note is that increased concentrations of free fatty acids impairs NO production by downregulating eNOS and decreases endothelial dependent vasodilation[40,41]. The diabetic hyperlipidemia-induced VED is characterized by reduced activation of eNOS, reduced generation and bioavailability of NO[5,39]. Moreover, the accumulation of renal lipid and generation of ROS is collectively involved in the pathogenesis of diabetic nephropathy[42]. Supporting this contention, Chen et al[43] observed that both native and oxidized LDL enhances superoxide generation in isolated diabetic rat glomeruli. Furthermore, a recent study certainly emphasized that, in diabetes, an excess amount of a variety of lipid progressively affects glomerular and tubular function[44]. Likewise, diabetic dyslipidemia is often associated with glomerular, mesangial and tubulointerstitial injury[43]. Additionally, it has been suggested that an increased expression of SREBP-1 in diabetic mice could play a central role in renal lipid accumulation, glomerulosclerosis and proteinuria[15]. Thus, growing evidence suggests that hyperlipidemia is considered a serious risk factor involved in the pathogenesis of diabetic renal diseases.
TGF-β PLAYS AN ABYSMAL ROLE IN PATHOGENESIS OF NEPHROPATHY: A PROFOUND LOOK
Although precise mechanisms involved in diabetes-associated renal complications are not clear, oxidative stress and dyslipidemia could play a key role in elevating renal complications. As many factors contribute to the induction and progression of diabetic nephropathy, the association between plasma levels of TGF-β (pro-sclerotic cytokine) and diabetes is considered an independent and major determinant of the progression of renal disease in patients with diabetes mellitus[8]. Various studies strongly suggested that high lipids could induce renal injury by stimulating TGF-β. This contention is supported by the fact that TGF-β is a fibrogenic cytokine and seems to promote extracellular matrix accumulation, a cardinal structural feature of the kidney in diabetic mice[45]. Furthermore, TGF-β appears to be an important mediator in oxidized LDL-induced mesangial matrix expansion, which changes the architecture of the kidney[46]. The strong correlation between hyperglycemia and TGF-β has been demonstrated as high-content glucose medium increases TGF-β mRNA expression glomeruli[47] and diabetic smokers are noted to have increased serum concentration of TGF-β[8,48]. Additionally, TGF-β stimulates the expression of connective tissue growth factor, which promotes glomerulosclerosis, renal deposition of extracellular matrix and hypertrophy of mesangial cells[49]. Furthermore, abnormal regulation of the renin angiotensin system is directly involved in the pathogenesis of diabetic nephropathy. It has been noted that angiotensin-II (Ang-II) increases the expression of TGF-β, which stimulates the synthesis of the mesangial matrix[50]. Thus, it may be concluded that long-term hyperglycemia elevates Ang-II, which increases the expression of TGF-β and plays a pathological role in the induction of diabetic nephropathy.
Ordinarily, in diabetes, AGEs are a heterogeneous compound formed non-enzymatically through an interaction of reducing sugar with an amino group of proteins and lipids[51]. Various studies have reported that the renal accumulation of AGEs is implicated in the pathogenesis of diabetic vascular complications[52]. As well, AGEs are noted to upregulate the expression of TGF-β and collagen, which accumulates particularly in glomerular and extracellular matrix, thus provoking glomerular hypertrophy in diabetes [53].
A further step towards the pathogenesis of diabetic nephropathy is involvement of Rho-kinase, a serine/threonine kinase noted to promote diabetic nephropathy[54]. This notation is further supported by the fact that the Rho-kinase plays a pivotal role in the pathogenesis of VED, which again complicates the condition of diabetic secondary complications[55]. Apparently, diabetes mediated activation of Rho-kinase contributes to the induction of glomerulosclerosis and upregulation of glomerular matrix deposition in rats[54,55]. This fact is further confirmed by treatment with fasudil, a selective Rho-kinase inhibitor, which markedly attenuated the development of diabetic nephropathy by inhibiting the renal upregulation of TGF-β, connective tissue growth factor and NADPH oxidase in rats[56]. Therefore, TGF-β is a marked contributor in the pathogenesis of diabetic nephropathy.
PARTICIPATION OF SMOKING MEDIATED OXIDATIVE STRESS IN THE DEVELOPMENT OF DIABETIC NEPHROPATHY
As there is no prior information about the role of nicotine as a powerful fierce molecule, many efforts entail a conceptual shift to understand the health hazards of nicotine. Smoking has been noted to develop large amount of free radicals and pro-oxidant molecules, exerting an adverse influence on endothelial cells through an inhibitory effect on components of the L-arginine-nitric oxide pathway[54,55]. Furthermore, nicotine plays a key role in the pathogenesis of endothelial dysfunction by decreasing the generation and bioavailability of NO and downregulating the expression of eNOS[7,56]. Thus, smoking mediated high oxidative stress and low availability of eNOS may engender VED, which is the initial step in the pathogenesis of glomerulosclerosis in diabetic nephropathy. In recent years, the increasing prevalence of smoking has been pinpointed as a progression factor for diabetic nephropathy. The chronic administration of nicotine is noted to increase lipid peroxidation products (cell membrane phospholipids) in serum and various tissues of rat. The concentration of these products was found to be inversely proportional to activity of endogenous antioxidants like catalase and superoxide dismutase[57]. Accordingly, breakdown of membrane phospholipids by lipid peroxidation is expected to play an important role in the vascular pathogenesis. Recently, David et al tested the hypothesis that exposure to tobacco smoke (nicotine) in db/db mice worsens the progression of diabetic nephropathy by increasing the severity of ECM deposition and increasing the expression of the profibrotic cytokine TGF-β. The knowledge about the involvement of ROS in the pathogenesis of vascular disease should facilitate the development of therapies that directly target ROS production to prevent microvascular complications.
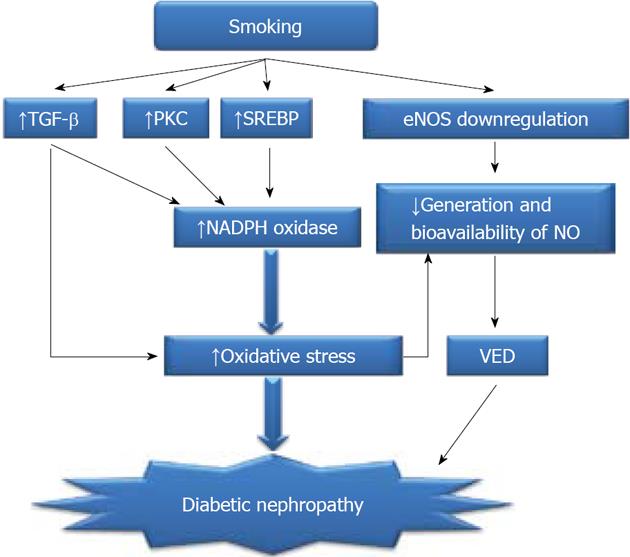
During smoking, nicotine is fiercely worked for the development of oxidative stress. Nicotine has been noted to increase generation of superoxide by activation of NADPH oxidase and PKC, which ultimately damages the kidney[23,31,58]. The destructive role of PKC is manifested as inhibition of PKC by calphostin C, a potent PKC inhibitor, which prevents nicotine-induced mesangial cell proliferation and fibronectin production. It suggests that nicotine-mediated growth promoting effects is through activation of NADPH oxidase and PKC, probably ROS as second messengers[3,59,60]. Thus, the inhibition of PKC halts the progression of nicotine-mediated renal damage and decreases NADPH oxidase mediated ROS generation. One unique mechanism explains that smoking stimulates lipid accumulation by increasing expression of SREBP-1, which is responsible for increasing the synthesis of TGs and cholesterol, which again sidewise contributes in the pathogenesis of nephropathy[16]. The possible mechanisms involved in smoking-induced oxidative stress mediated renal damage in diabetes have been depicted in Figure 1.
Figure 1 Possible mechanism involved in smoking-induced oxidative stress.
TGF-β: Transforming growth factor β; PKC: Protein kinase C; eNOS: Endothelial nitric oxide synthase; NO: Nitric oxide; SREBP: Sterol regulating element binding protein; VED: Vascular endothelial dysfunction.
PARTICIPATION OF SMOKING MEDIATED HYPERLIPIDEMIA IN DEVELOPMENT OF DIABETIC NEPHROPATHY
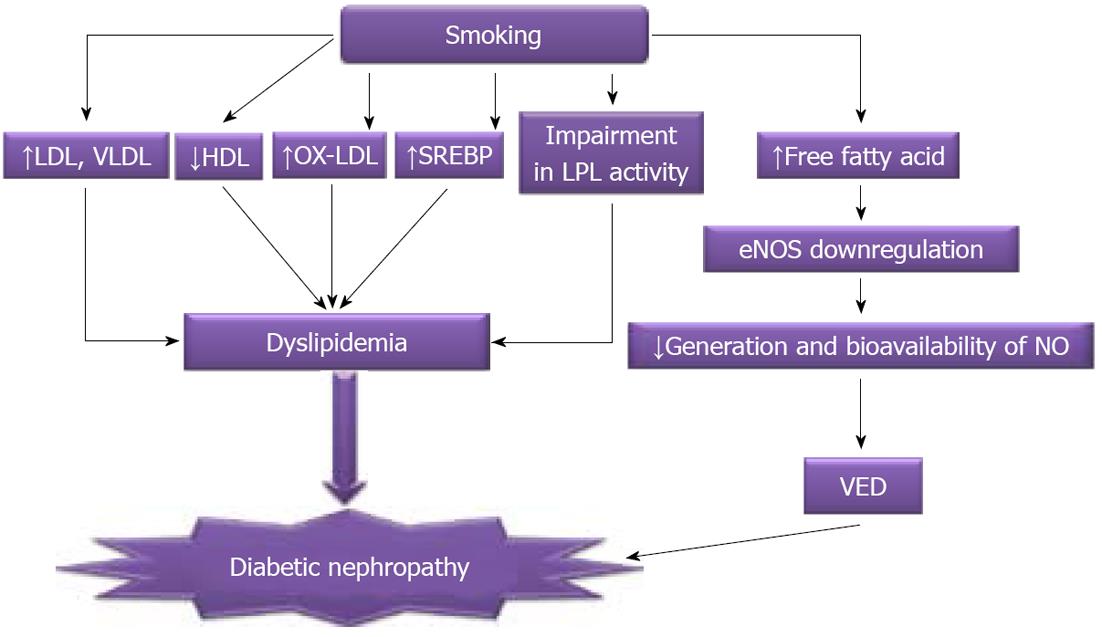
It is very difficult to understand smoking-mediated lipid wiggles because nicotine has intricate mechanisms; however, serial analysis may explore its role in the development of dyslipidemia in diabetes. Smoking has numerous atrocious effects, which initially pertain to the pathogenesis of microvascular and subsequently renal complications. Cigarette smoking is positively associated with higher serum concentrations of TGs and LDL and lower serum concentrations of HDL[13]. In fact, nicotine causes an impairment of LPL and increases plasma lipid concentration[11]. Elegant studies show that nicotine-mediated hyperlipidemia is considered to be an underlying mechanism involved in the nicotine-induced endothelial dysfunction[6,7]. Especially, nicotine plays a key role in induction of VED by decreasing the generation and bioavailability of NO and downregulating the expression of eNOS[7,34,59]. Nicotine is also noted to induce glomerulosclererosis and provokes reno-vascular pathogenesis[12]. Thus, smoking endorses dyslipidemia and worsens the severity of nephropathy in diabetes. After pondering over the above discussion, it can be said that the deleterious effect of cigarette smoking, such as renal damage, is through dyslipidemia. Taken together, through direct or indirect multiple mechanisms, smoking in diabetes has been regarded as a major risk factor in the induction and progression of oxidative stress and dyslipidemia mediated renal damage (Figure 2).
Figure 2 Possible mechanisms involved in smoking-induced dyslipidemia.
eNOS: Endothelial nitric oxide synthase; NO: Nitric oxide; SREBP: Sterol regulating element binding protein; VED: Vascular endothelial dysfunction; LDL: Low density lipoprotein; VLDL: Very low density lipoprotein; HDL: High density lipoprotein; LPL: Lipoprotein lipase.
COMRADESHIP BETWEEN SMOKING AND DIABETIC NEPHROPATHY: EXACERBATION OF NEPHROPATHY?
Various epidemiological studies have explored potential mechanisms that could be responsible for smoking-mediated progression diabetes nephropathy. The main clinical associations that frequently precede diabetic nephropathy are hypertension and poor glycemic control. A recent gender-specific, dose-response relationships study demonstrated that smoking is a significant risk factor for future kidney failure[61]. Clinical hallmarks of diabetic nephropathy include a progressive increase in urinary albumin excretion and a decline in glomerular filtration rate. Diabetes and smoking concurrently activated cellular pathways uncompromisingly and participate in step wise progression of nephropathy[21,57]. The frequent microalbuminuria is more commonly noted in diabetic smokers than non smokers with nephropathy[4,60]. Similarly, the rate of loss of measured creatinine clearance was noted to be higher in smokers compared to non-smoking diabetic patients[61]. Intriguingly, smoking also increases the risk of subjects to develop type II diabetes, possibly because it increases insulin resistance[62]. Furthermore, a growing body of evidence compared non-diabetic smokers and non-smokers and found that smokers were more insulin resistant and hyperinsulinemic[63]. Furthermore, smoking impaired insulin action, mainly due to a lowering of peripheral glucose uptake[64]; thus, smoking is a key risk factor for the subject to develop type II diabetes and secondary complications. Preclinical studies further support the fact that smoking accelerates diabetic nephropathy. It is worth mentioning that administration of nicotine develops glomerular hypertrophy and mesangial expansion and increases high glucose mediated ROS generation through activation of NADPH oxidase and aggravates nephropathy in diabetic mice[3]. In addition, exposure to tobacco smoke in db/db mice significantly increases urinary albumin excretion, mesangial expansion and extracellular matrix deposition and worsens diabetic nephropathy[65].
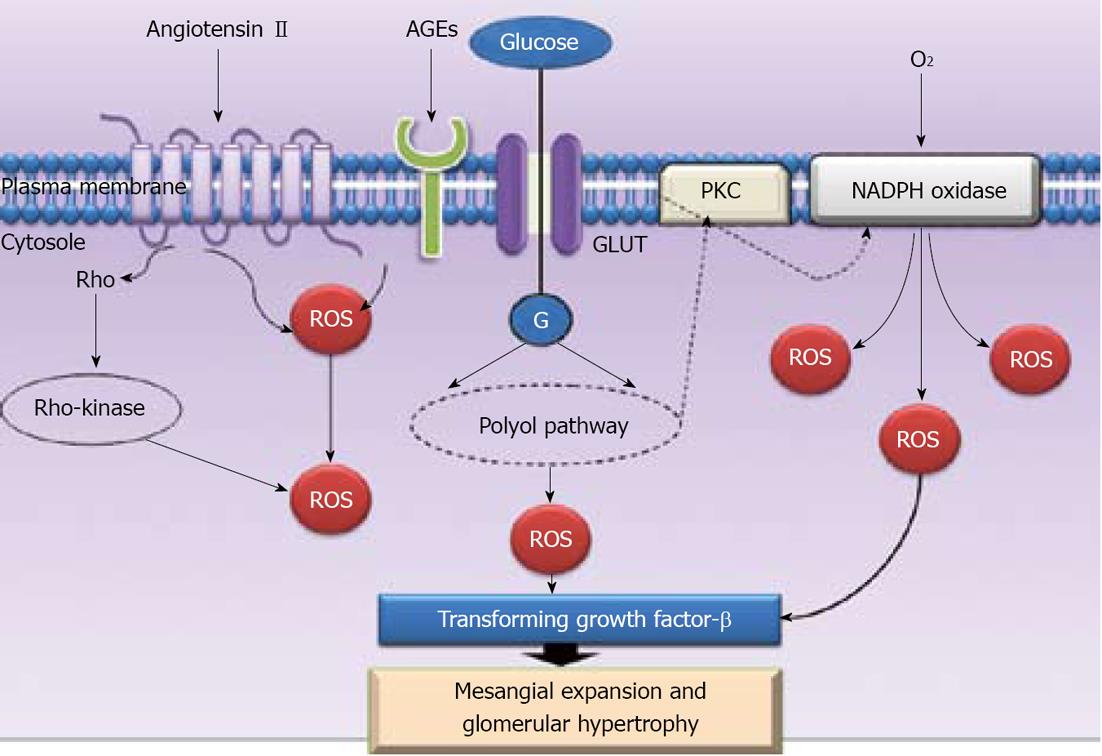
Despite this, various endogenous molecules may be associated with smoking and could partially contribute to the pathogenesis of microvascular complications in diabetes, which are yet poorly understood. Importantly, it has been noted that smoking increases serum concentration of Ang-II and TGF-β1 in diabetic patients[8]. Along with this, it has been noted that cessation of smoking downregulates TGF-β1 when compared with diabetic non-smokers[66]. Prominently, cigarette smoking enhances the accumulation of AGEs, which crosslink with collagen to promote vascular complications[67] and also increases production of TGF-β in aortic endothelial cells[48], indicating the strong relationship between smoking, AGEs and TGF-β in the pathogenesis of vascular complications. As described above, accumulation of AGEs by diabetes and smoking is directly proportional to expression of TGF-β, which is finally involved in reno-vascular complications. Taken together, available evidence indicates that accumulation of AGEs, either by diabetes or by smoking, promotes an appalling role for TGF-β in the progression of nephropathy. Furthermore, crucial involvement of Rho-kinase provides a suitable target system to understand the basic pathways of smoking-mediated reno-vascular disease. It is interesting to note that treatment with fasudil, a Rho-kinase inhibitor, significantly prevented the smoking-induced impairment in endothelium-dependent vasodilation[68], which suggests the detrimental involvement of Rho-kinase in nicotine-induced endothelial dysfunction. The broad utility of these approaches is to target these endogenous molecules to attenuate smoking-mediated reno-vascular damage. The availability of this comprehensive data allows accelerating development of active compounds and strategies for intervention at various stages in the development of diabetic nephropathy. Thus, smoking mediated insulin resistance, frequent microalbuminuria, mesangial expansion and glomerular hypertrophy indicate the detrimental effects of smoking in development and progression of diabetic nephropathy (Figure 3).
Figure 3 Various endogenous modulators contribute to renal complications.
AGEs: Advance glycation end products; ROS: Reactive oxygen species; GLUT: Glucose transporters; PKC: Protein kinase C; NADPH oxidase: Nicotinamide adenine dinucleotide phosphate-oxidase.
Therefore, from the above critical discussion and pondering over accumulating evidence, it may be understood that oxidative stress and hyperlipidemia are key players in the pathogenesis of diabetic nephropathy. Furthermore, smoking provokes oxidative stress and dyslipidemia upregulates TGF-β in diabetes, which worsens the severity of nephropathy. Simultaneously, Ang-II, AGEs and Rho/Rho-kinase upregulate TGF-β, which plays a pathogenic role in the induction of renal hypertrophy and progression of diabetic nephropathy. Thus, it may be concluded that chronic cigarette smoking may exacerbate diabetic nephropathy.
PHARMACOLOGICAL INTERVENTIONS TO TREAT DIABETIC SMOKERS WITH NEPHROPATHY
Over several decades, there have been extensive investigations concerning the development of novel target sites and thus numerous agents have been explored for therapeutic potential in treating diabetic nephropathy. Smoking is an additional factor directly involved in the progression of nephropathy. Thus, diabetic smokers are more complicated to treat than non smokers. Yet, a promising and effective therapy has not been deduced for these complicated diseases. Hyperglycemia and cigarette smoking mainly arouses oxidative stress and hyperlipidemia. Hence, strict glycemic control and smoking secession remains the cornerstone of the current standard therapeutic approaches and may help to ameliorate vascular complications.
The drugs currently used to treat diabetic nephropathy mainly target the hypertensive component, such as drugs that interrupt the renin-angiotensin system, angiotensin-converting enzyme (ACE) inhibitors and Ang-II receptor antagonists, and are currently considered first-line treatments for diabetic nephropathy. In particular, the use of a different class of drugs, such as ACE inhibitors captopril, lisinopril, fosinopril, benazapril and quinapril, and AT-I receptor blockers, such as losartan, olmesartan and irbesartan, have been observed in numerous experimental and clinical studies to have therapeutic potential in the treatment of diabetic nephropathy[69-77]. Captopril was the first drug approved by Food and Drug Administration in the nineties for the treatment of diabetic nephropathy[48].
Cigarette smoking is major fuel for the generation of oxidative stress. As mentioned in the preceding section, NADHP oxidase is a master enzyme involved in ROS formation. Therefore, a superior approach to ameliorate oxidative stress is to inhibit the culprit enzyme NADHP oxidase. This contention is further supported by the fact that apocynin restores renal function by decreasing the expression of collagen-1, mesangial expansion and albuminuria diabetic rats[78,79]. The evidence presented above provides a strong rationale for the use of pharmacological inhibitors of NADPH oxidase to combat oxidative stress and its associated vascular pathologies. The current research interest is to treat diabetic nephropathy by use of a fibrates class of interventions, such as fenofibrate, bezafibrate and gemfibrozil, well-known hypolipidemic agents[80-82]. Recently, in our laboratory we have shown that treatment with fenofibrate and concurrent administration of benfotiamine, a transketolase activator, prevented the development of diabetic nephropathy. This renoprotective effect of fenofibrate was associated with its actions on reducing the circulating lipids and oxidative stress[5]. Furthermore, fenofibrate was shown to ameliorate nicotine-induced endothelial dysfunction by reducing hyperlipidemia and oxidative stress in rats[7]. Thus, the available evidence says that the use of fenofibrate attenuates diabetes and nicotine-mediated hyperlipidemia and oxidative stress and ameliorates endothelial dysfunction and nephropathy. Therefore, use of fenofibrate is the most logical pharmacological intervention to treat smoking mediated progression of diabetic nephropathy, like killing two birds with one stone. From the above discussion, it may be concluded that fibrate really preserves kidney function in diabetes. On other hand, cyclohexenonic long-chain fatty alcohol (N-hexacosanol) was noted to reduce significantly TGF-β and concentrations of PKC, which ameliorate the diabetic-induced tubulointerstitial pathological changes[83]. Furthermore, N-hexacosanol was also noted to reduce diabetes-mediated alteration in eNOS, which attenuates glomerulosclerosis[84].
Taken together, these studies suggest that these drugs may provide supportive therapeutic advancement for treating diabetic smokers with nephropathy. However, further studies are needed to illuminate their therapeutic potential in treating diabetic smokers with vascular pathogenesis.
CONCLUSION
Smoking is ubiquitous in patients with diabetes mellitus. Smoking and hyperglycemia increase oxidative stress and lipid accumulation, which upregulates TGF-β, accumulates AGEs, decreases nitric oxide production, which leads to thickening of glomerular basement membrane and mesangial expansion, with progression in glomerulosclerosis and interstitial fibrosis, and results in nephropathy. It is emerging from above that smoking is a hitherto major fuel to aggravate diabetic nephropathy.
ACKNOWLEDGEMENT
I wish to express my gratitude to my father, Mr. Arvind S. Chakkarwar, for his praiseworthy enthusiastic support for writing this article. I also express my thankfulness to my wife, Vaishali V Chakkarwar, for her constant moral support.
Peer reviewers: Dr. Goji Hasegawa, Department of Endocrinology and Metabolism, Kyoto Prefectural University of Medicine Graduate School of Medical Science, 465 Kajii-cho, Hirokoji, Kawaramachi, Kamikyo-ku, Kyoto 602-8566, Japan; Dr. Motoaki Saito, Mol Pharmacology, Tottori University, 86 Nishimachi, Yonago 683-8503, Japan
S- Editor Wen LL L- Editor Roemmele A E- Editor Xiong L