Published online Aug 15, 2025. doi: 10.4239/wjd.v16.i8.110088
Revised: June 18, 2025
Accepted: July 18, 2025
Published online: August 15, 2025
Processing time: 77 Days and 21.6 Hours
Diabetic ketoacidosis (DKA) remains a serious and potentially preventable com
To examine psychological predictors of DKA in children with T1DM using the health belief model, and to assess the role of caregiver-perceived understanding in influencing adherence and DKA occurrence.
A case-control study was conducted at Prince Sultan Military Medical City in Riyadh, Saudi Arabia, involving 191 caregivers of children with T1DM (96 cases with a history of DKA and 95 controls without). Validated questionnaires mea
Perceived understanding was the strongest predictor of adherence (β = 1.03, P < 0.001) and was inversely associated with DKA occurrence (P < 0.001). Children without a DKA history had significantly higher levels of perceived understanding and adherence. Perceived severity had a moderate positive association with ad
Caregiver-perceived understanding plays a critical role in adherence and DKA prevention. These findings support expanding the health belief model to include perceived understanding as a distinct construct and highlight the importance of integrating comprehension-focused strategies into pediatric diabetes education.
Core Tip: This study explores the psychological factors that contribute to diabetic ketoacidosis in children with type 1 diabetes mellitus, focusing on a population in Saudi Arabia. Using the health belief model, the research examines perceived severity and susceptibility, while introducing perceived understanding of diabetes management as a novel cognitive factor. The findings reveal that a caregiver’s understanding of diabetes management plays a more significant role in preventing diabetic ketoacidosis than risk perception alone. These insights suggest that enhancing comprehension through targeted education could improve adherence and reduce complications, offering a more patient-centered approach to pediatric diabetes care.
- Citation: Alissa N, Al Zahrani S. Psychological predictors of diabetic ketoacidosis in children: Health belief model-based case-control study. World J Diabetes 2025; 16(8): 110088
- URL: https://www.wjgnet.com/1948-9358/full/v16/i8/110088.htm
- DOI: https://dx.doi.org/10.4239/wjd.v16.i8.110088
Diabetic ketoacidosis (DKA) is a life-threatening complication of type 1 diabetes mellitus (T1DM), characterized by hyperglycemia, ketosis, and metabolic acidosis due to absolute insulin deficiency. In the absence of sufficient insulin, fat metabolism leads to ketone body accumulation, which causes systemic acidosis[1]. Clinically, DKA presents with symptoms such as polyuria, polydipsia, nausea, vomiting, abdominal pain, and a characteristic fruity breath odor. If left untreated, it can rapidly progress to cerebral edema, coma, and death[2,3]. DKA is among the most significant causes of mortality and hospitalization in children and adolescents with T1DM. Over half of all diabetes related deaths in this population are linked to DKA[4], and the condition is further associated with severe neurocognitive and economic burdens, with hospital admissions averaging over 26000 United States dollars per episode[5].
Despite substantial advances in diabetes care, the incidence of DKA remains unacceptably high worldwide, particularly in pediatric populations. Studies report that approximately 25% to 30% of children with T1DM present with DKA at diagnosis[2]. In the Gulf region, especially Saudi Arabia, the problem is more pronounced. Reports indicate that up to 77 percent of children with newly diagnosed T1DM present with DKA, reflecting delayed diagnosis, poor symptom recognition, and inadequate awareness among patients and caregivers[6-8]. These challenges highlight systemic gaps in early detection and diabetes education. Additional contributing factors include improper insulin dosing, infections, psychological distress, and socioeconomic barriers, which all increase the risk of acute decompensation[9-11].
Several studies have emphasized that poor compliance with diabetes management, particularly insulin therapy, glucose monitoring, and meal planning, is a critical driver of DKA episodes[12-14]. Infections, such as urinary or respiratory tract infections, often increase insulin requirements, and failure to adjust treatment appropriately can precipitate DKA[15]. Moreover, non-biological influences such as emotional stress, family conflict, and lack of social support may disrupt routine self-care behaviors, especially among children and adolescents[6]. In many cases, these psychosocial and behavioral determinants are more predictive of DKA risk than clinical factors alone.
The health belief model (HBM) provides a robust theoretical framework for understanding treatment adherence in chronic conditions. According to the HBM, individuals’ engagement in preventive health behaviors is shaped by their perceptions of illness severity, susceptibility to complications, perceived benefits of action, and perceived barriers to adherence[2]. In the context of T1DM, this model has been used to assess how psychological factors influence the consistency of self-care behaviors. Research suggests that children and caregivers who perceive DKA as a severe threat and understand their vulnerability are more likely to adhere to prescribed insulin regimens and monitoring protocols[16,17]. In Saudi Arabia, where health literacy on diabetes management is often limited, enhancing awareness of DKA through HBM informed education has shown promise in reducing complication rates[7,18].
However, while perceived severity and susceptibility have been extensively explored in previous studies, perceived understanding, defined as the patient or caregiver’s grasp of DKA mechanisms and management, has received comparatively little attention. Existing literature has largely focused on clinical predictors of DKA or general educational interventions without assessing how cognitive understanding influences treatment adherence. Several studies have documented that inadequate understanding of insulin adjustment, symptom monitoring, and emergency responses contributes to poor outcomes[19-21]. Furthermore, although research grounded in the HBM has demonstrated its utility in predicting health behaviors, its application in the Saudi pediatric population with T1DM remains limited.
Given the continued high burden of DKA among children with T1DM in Saudi Arabia, particularly at diagnosis, it is essential to explore not only the clinical and behavioural factors but also the psychological variables that influence adherence. Accordingly, this study aimed to investigate the psychological factors associated with adherence behaviors and the risk of DKA among children with T1DM in Saudi Arabia, using the HBM as a theoretical framework. Specifically, it examined how perceived severity, perceived susceptibility, and perceived understanding influence diabetes management practices. The study addressed the following research questions: (1) Is there a significant difference between children with and without a history of DKA in terms of perceived severity, susceptibility, understanding, and adherence? (2) What is the relationship between these psychological constructs and adherence behaviors? and (3) Which of these factors most strongly predicts adherence among pediatric patients with T1DM?
This study employed a case control design to examine psychological factors influencing adherence behaviors and the risk of DKA among children with T1DM in Saudi Arabia. The approach allowed for comparisons between children who had experienced at least one episode of DKA (cases) and those who had not (controls). By contrasting exposure to psychological perceptions between the two groups, the study aimed to identify key predictors of treatment adherence and DKA occurrence.
The research was conducted at Prince Sultan Military Medical City, a leading tertiary care hospital located in Riyadh, Saudi Arabia. Operated by the Ministry of Defense, Prince Sultan Military Medical City is one of the largest and most specialized medical institutions in the country, providing comprehensive healthcare services to military personnel and their families[22]. The hospital includes a well-established pediatric department with dedicated inpatient and outpatient services for children with T1DM. It serves as a regional referral center for complex pediatric endocrine cases and offers multidisciplinary diabetes management and structured patient education. Data collection took place between January and December 2024 and included pediatric patients either hospitalized for T1DM management or attending regular follow-up visits in the diabetes clinics.
The study targeted pediatric patients aged 2 years to 14 years with a confirmed diagnosis of T1DM. Participants were divided into two groups: Those with a documented DKA episode in the past year (cases) and those without any prior history of DKA since diagnosis (controls).
Inclusion criteria required the presence of a primary caregiver able to complete the survey, confirmation of a T1DM diagnosis, and clinical stability at the time of data collection. Patients were excluded if they had secondary diabetes, cognitive impairments that affected their understanding of treatment, or declined participation.
Sample size calculation was performed using standard epidemiological formulas for unmatched case–control studies, with assumptions based on prior literature. The calculation was conducted using OpenEpi, Version 3.01[23]. The total sample included 191 participants, comprising 96 cases and 95 controls. A non-probability sequential sampling method was employed.
Data was collected using a structured, self-administered computerized questionnaire completed by the patients’ primary caregivers. The questionnaire assessed psychological perceptions, treatment adherence behaviors, and demographic and clinical characteristics. Clinical information, including DKA episodes, was cross validated with patient medical records. A pilot study was conducted with 20 participants to evaluate the tool's clarity, feasibility, and reliability.
A validated structured questionnaire with five components was used, and each was evaluated by two experts to confirm its content validity and cultural suitability.
Demographic and clinical information: This section collected participant age, sex, Hemoglobin A1c (HbA1c) levels, pH values, history of hospitalization, presence of ketonuria, and gastrointestinal symptoms. Items were based on the Diabetes Care Profile (DCP), a validated tool for assessing social and psychological dimensions of diabetes care[24].
Perceived disease severity: A 5-item scale was adapted from the Risk Perception Survey for Developing Diabetes (RPS DD), a tool designed to assess perceived risk across various health conditions[25]. The items were modified to specifically reflect the perceived severity of diabetes related complications relevant to T1DM. An example item includes: “Do you consider DKA a serious complication of diabetes?” with response options ranging from 1 (strongly disagree) to 5 (strongly agree). The scale demonstrated good internal consistency, with a Cronbach’s alpha of 0.78, indicating sa
Perceived susceptibility: A 5-item scale assessing perceived susceptibility to T1DM related complications was developed using items adapted from the RPS DD. The items followed a Likert scale format consistent with the original RPS DD, measuring caregivers’ perceptions of risk. The scale demonstrated acceptable internal consistency, with a Cronbach’s alpha of 0.68. A sample item includes: “Are you constantly worried that your child’s ketoacidosis may recur?” with response options ranging from 1 (strongly disagree) to 5 (strongly agree).
Perceived understanding of T1DM management: This section assessed caregivers’ understanding of type 1 diabetes management using six items adapted from the Diabetes Attitude Scale and the DCP[26]. Responses were recorded on a 5-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree). The scale exhibited excellent internal consistency, with a Cronbach’s alpha of 0.94. An example item is: “I know how to use your diabetes test results to make decisions”.
Behavioral adherence practices: This section included 12 items across three domains: Blood glucose monitoring (4 items), treatment attitudes (3 items), and dietary behaviors (5 items). Items were adapted from the DCP, Diabetes Attitude Scale, and the Perceived Dietary Adherence Questionnaire[27].
Statistical analysis was performed using Stata version 18. Independent t tests and χ2 tests were used to compare perceived psychological variables and adherence practices between the case and control groups. Pearson correlation coefficients were calculated to explore relationships among perceived severity, susceptibility, understanding, and adherence. Multiple regression analysis identified significant psychological predictors of adherence behavior. Statistical significance was set at P < 0.05. Internal consistency of the scales was evaluated using Cronbach’s alpha, which ranged from 0.68 to 0.94.
A pilot test was conducted with 20 participants at Prince Sultan Military Medical City in Riyadh to assess the dependability of the instruments and the practicality of the data collection procedures. The electronic survey link was shared with participants, and feedback was used to revise unclear items. Reliability testing with SPSS yielded a Cronbach’s alpha of 0.90. Univariate analysis and logistic regression were performed to explore odds ratios for key predictors. The analysis included control variables such as age, sex, and health status.
The study protocol received ethical approval from the Institutional Review Board at Prince Sultan Military Medical City, approval No. IRB 1211. All participants were informed about the study’s purpose, procedures, and their right to withdraw at any time. Parental consent was obtained electronically and verbally prior to survey administration. Confidentiality was strictly maintained throughout the study, and all procedures followed established ethical guidelines for research involving human subjects.
All measurement tools demonstrated acceptable to excellent reliability. Table 1 summarizes the internal consistency coefficients for each scale used in the study.
| Scale | Cronbach’s alpha |
| Perceived severity | 0.78 |
| Perceived susceptibility | 0.68 |
| Perceived understanding | 0.94 |
| Behavioral adherence practices | - |
| Dietary adherence | 0.94 |
| Glucose testing adherence | 0.91 |
| Treatment adherence | 0.93 |
A total of 191 participants completed the online questionnaire. Although the survey was initially distributed to 200 individuals (100 cases and 100 controls), complete responses were obtained from 96 participants in the case group (with a history of DKA) and 95 in the control group (without a history of DKA).
There was a statistically significant difference in sex distribution between the groups (P = 0.036), with a higher proportion of females in the case group and more males in the control group. No significant difference in age was observed. Children in the case group had significantly higher mean HbA1c levels (9.82% vs 8.80%, P < 0.001) and lower mean pH values (7.21 vs 7.42, P < 0.001). A significantly greater proportion of patients in the case group had poor glycemic control (HbA1c ≥ 10%) (P = 0.004). Additionally, ketonuria, pediatric intensive care unit admissions, and gastrointestinal symptoms were significantly more common among cases (all P < 0.001) (Table 2).
| Variable | Cases (n = 96) | Controls (n = 95) | P value |
| Age (years), mean ± SD | 9.74 ± 2.21 | 9.90 ± 2.40 | 0.626 |
| Sex - male | 41.8% | 57.0% | - |
| Sex - female | 58.2% | 43.0% | - |
| HbA1c (%), mean ± SD | 9.82 ± 1.80 | 8.80 ± 1.59 | < 0.001 |
| HbA1c category - good control (< 7.5%) | 9.9% | 20.2% | - |
| HbA1c category - moderate (7.5%-9.9%) | 29.7% | 48.9% | - |
| HbA1c category - poor (≥ 10%) | 60.4% | 30.9% | 0.004 |
| pH, mean ± SD | 7.21 ± 0.17 | 7.42 ± 0.08 | < 0.001 |
| Ketonuria | 100% | 0% | < 0.001 |
| PICU admission | 73.2% | 0% | < 0.001 |
| GI symptoms | 59.8% | 9.6% | < 0.001 |
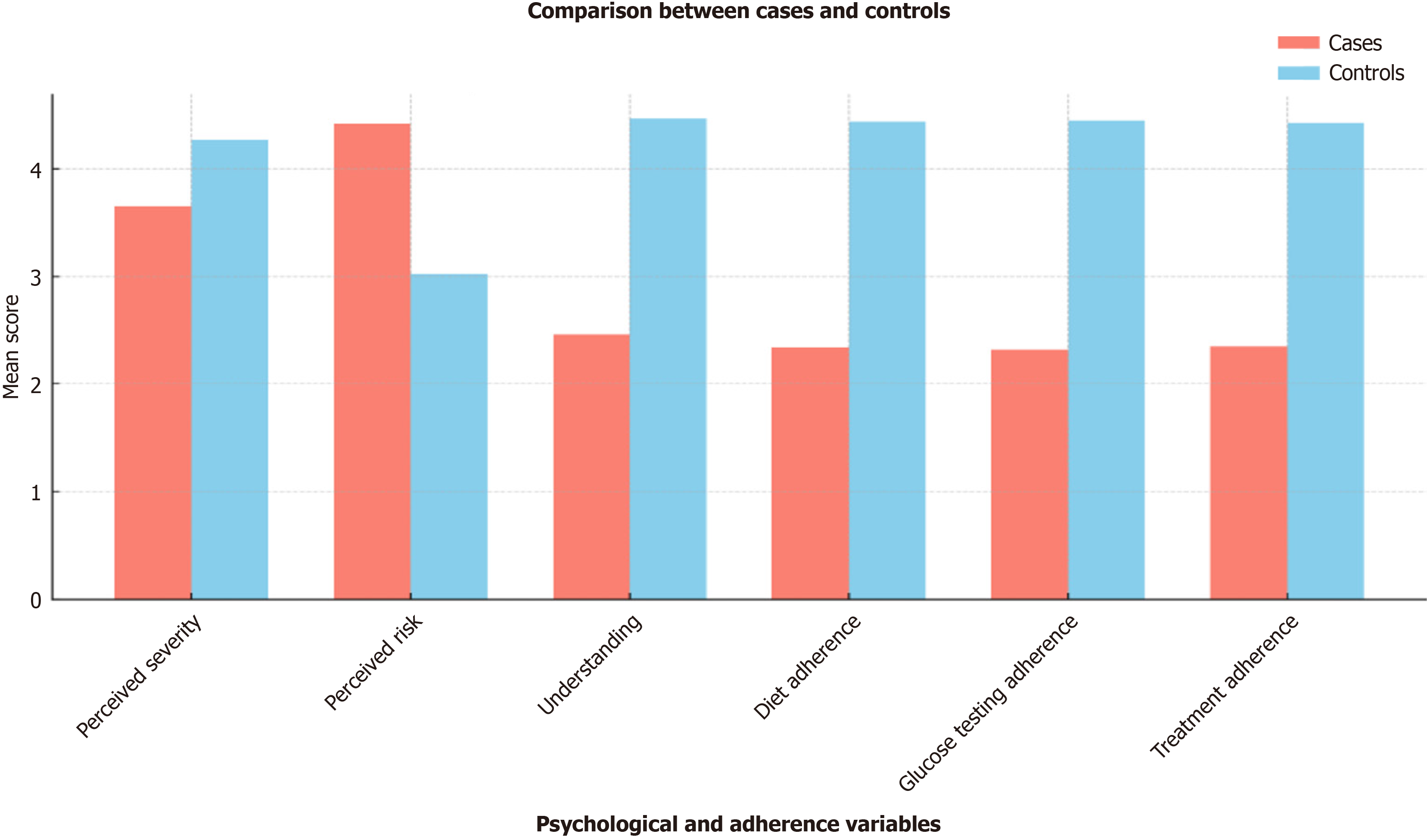
The mean perceived severity score was 3.65 ± 0.82, while the mean perceived susceptibility score was 4.42 ± 0.55. The average perceived understanding of T1DM management was 2.46 ± 0.99. Mean scores for adherence to diet, glucose testing, and treatment were 2.34 ± 0.94, 2.32 ± 0.96, and 2.35 ± 0.95, respectively. Comparisons between case and control groups revealed statistically significant differences across all psychological and behavioral measures, with the control group consistently demonstrating higher adherence and understanding, and lower perceived susceptibility (Table 3 and Figure 1).
| Variable | Case group | Control group | P value |
| Perceived severity | 3.65 ± 0.82 | 4.27 ± 0.74 | < 0.001 |
| Perceived susceptibility | 4.42 ± 0.55 | 3.02 ± 0.94 | < 0.001 |
| Perceived understanding | 2.46 ± 0.99 | 4.47 ± 0.55 | < 0.001 |
| Dietary adherence | 2.34 ± 0.94 | 4.44 ± 0.54 | < 0.001 |
| Glucose testing adherence | 2.32 ± 0.96 | 4.45 ± 0.56 | < 0.001 |
| Treatment adherence | 2.35 ± 0.95 | 4.42 ± 0.54 | < 0.001 |
Correlation analyses (Table 4) revealed moderate positive relationships between perceived severity and all adherence behaviors, including dietary adherence (r = 0.38), glucose testing adherence (r = 0.36), and treatment adherence (r = 0.37). This suggests that parents who recognized the seriousness of diabetes complications were more likely to ensure con
| Variable | Dietary adherence (r) | Glucose testing adherence (r) | Treatment adherence (r) |
| Perceived severity | 0.38 | 0.36 | 0.37 |
| Perceived susceptibility | -0.24 | -0.23 | -0.23 |
| Perceived understanding | 0.95 | 0.93 | 0.94 |
Perceived understanding of diabetes management emerged as the strongest predictor of adherence across all domains. It had a significant positive effect on overall adherence [β = 1.03, 95% confidence interval (CI): 0.97-1.09, P < 0.001], glucose testing (β = 0.91, 95%CI: 0.85-0.97, P < 0.001), and treatment adherence (β = 1.14, 95%CI: 1.06-1.22, P < 0.001). These findings suggest that a higher level of understanding substantially improves adherence outcomes.
Sex was also a significant predictor of overall adherence (β = 0.15, 95%CI: 0.05-0.25, P < 0.01) and treatment adherence (β = 0.20, 95%CI: 0.06-0.34, P < 0.01), suggesting that female caregivers may be more likely to support consistent adherence behaviors in children with T1DM. However, perceived severity and susceptibility were not significant predictors after controlling for understanding. This indicates that cognitive understanding of diabetes care, rather than emotional perceptions of risk or seriousness, is more influential in promoting adherence behaviors (Table 5).
| Predictor | Adherence behavior | β | 95%CI |
| Understanding | Overall adherence | 1.03b | 0.97-1.09 |
| Understanding | Glucose testing adherence | 0.91b | 0.85-0.97 |
| Understanding | Treatment adherence | 1.14b | 1.06-1.22 |
| Gender | Overall adherence | 0.15a | 0.05-0.25 |
| Gender | Glucose testing adherence | 0.09 | -0.01-0.19 |
| Gender | Treatment adherence | 0.20a | 0.06-0.34 |
| Perceived severity | All | Not significant | CI includes 0 |
| Perceived susceptibility | All | Not significant | CI includes 0 |
A statistically significant negative correlation was found between perceived understanding and perceived susceptibility (r = -0.239, P = 0.001), suggesting that greater understanding of T1DM management is associated with lower perceived susceptibility to complications.
Research question 1: Is there a significant difference between children with and without a history of DKA in terms of perceived severity, susceptibility, understanding, and adherence? As shown in Table 3, significant differences were observed between groups across all variables (P < 0.001). Compared to the control group, patients with DKA reported lower perceived severity, understanding, and adherence, but higher perceived susceptibility.
Research question 2: What is the relationship between these psychological constructs and adherence behaviors? As shown in Table 4, perceived understanding demonstrated the strongest positive correlation with adherence (r = 0.93 to 0.95), followed by perceived severity (moderate correlations), while perceived susceptibility showed weak negative associations.
Research question 3: Which of these factors most strongly predicts adherence among pediatric patients with T1DM? Table 5 indicates that perceived understanding was the only significant psychological predictor of adherence behaviors (β = 0.91 to 1.14, P < 0.001). Perceived severity and susceptibility were not significant predictors after controlling for understanding.
This study explored psychological factors influencing adherence behaviors among pediatric patients with T1DM in Saudi Arabia, guided by the HBM. Specifically, the study examined the roles of perceived severity, perceived susceptibility, and perceived understanding of diabetes management. Additionally, sex was investigated as a potential demographic predictor[28,29].
The results demonstrated that perceived understanding was the most influential psychological factor in predicting adherence behaviors. Strong, positive correlations were found between perceived understanding and all adherence domains, including dietary adherence, glucose testing, and treatment adherence (r = 0.93-0.95). Regression analysis confirmed that perceived understanding significantly predicted adherence (β = 0.91-1.14, P < 0.001), highlighting the critical role of caregiver comprehension in facilitating effective diabetes self-management. This finding is supported by previous studies conducted by Batwa and colleagues and Charron-Prochownik and colleagues[7,17], which emphasized that improved knowledge and understanding among caregivers contribute to better adherence and lower incidence of DKA.
Perceived severity showed moderate positive correlations with adherence (r = 0.36-0.38), suggesting that caregivers who recognized the seriousness of DKA were somewhat more likely to promote consistent diabetes care. However, in the adjusted regression model, perceived severity did not significantly predict adherence. This supports previous findings by Vitale et al[16] and Eltom et al[30], who reported that perceptions of severity, although important, must be accompanied by practical knowledge and motivation to influence health behavior.
Interestingly, perceived susceptibility demonstrated weak negative correlations with adherence behaviors (r = -0.23 to -0.24) and was not a significant predictor in the multivariate model. This contrasts with the classical assumptions of HBM, which posits that higher perceived risk leads to preventive action[2]. One explanation may be that perceived vulnerability, when not coupled with understanding or efficacy, can lead to avoidance or disengagement, as echoed in the psychological findings reported by Skinner et al[31]. A significant negative correlation between perceived understanding and perceived susceptibility (r = -0.239, P = 0.001) was observed, suggesting that caregivers who better understand diabetes management may feel less vulnerable or overwhelmed. This dynamic supports the conceptual model proposed by Zainal et al[32], where knowledge functions as a buffer against anxiety-driven risk perceptions.
Sex also emerged as a significant predictor of adherence. Female caregivers were more likely to support overall adherence (β = 0.15, 95%CI: 0.05-0.25, P < 0.01) and treatment adherence (β = 0.20, 95%CI: 0.06-0.34, P < 0.01). These results are consistent with findings reported by Al Hayek et al[33] and Alotaibi et al[34], who found that maternal figures often play a more proactive role in pediatric diabetes management, potentially due to greater caregiving responsibilities and health awareness.
Overall, these findings indicate that while the HBM remains a valuable framework, it may benefit from the inclusion of perceived understanding as an independent construct. The traditional domains of the model, including perceived severity, susceptibility, benefits, barriers, cues to action, and self-efficacy, may not fully capture the influence of cognitive understanding on health behavior. In the context of chronic illnesses such as T1DM, a strong understanding of disease management appears to be essential for converting risk perception into consistent adherence. This perspective aligns with the conclusions of Benouda et al[20], who emphasized the importance of integrating patient education and comprehension assessments into diabetes care practices.
Educational interventions for pediatric diabetes should therefore prioritize enhancing caregivers’ understanding of disease management. Structured health literacy assessments and comprehension-focused training modules should be integrated into diabetes education curricula. Furthermore, future research should examine perceived understanding across other chronic disease models and diverse cultural contexts to validate its role as a predictive factor in health behavior change.
This study has several limitations that should be acknowledged. First, the research was carried out at a single tertiary care hospital in Riyadh, which may limit how well the findings apply to other regions or healthcare systems. We recognize that different settings may have unique challenges and dynamics, so future studies would benefit from including participants across multiple centers and more diverse backgrounds to improve generalizability.
Second, the data were obtained from caregivers rather than directly from pediatric patients. While appropriate for the age group studied, this method may introduce bias due to differences in perception, recall, or interpretation. In
Third, the study focused on two key concepts from the HBM, specifically perceived severity and perceived susceptibility, while also introducing perceived understanding as an added cognitive factor. This focused approach was intended to highlight the most immediate psychological influences on adherence and risk of DKA. However, we recognize the value of including other elements of the model, such as perceived benefits, barriers, cues to action, and self-efficacy. Future research could take a more comprehensive approach or explore other psychological models to deepen our understanding of what drives effective diabetes management.
Finally, although the instruments used were adapted from validated tools and demonstrated acceptable internal consistency, the use of modified scales may limit comparability with other studies. Future work should include fully validated instruments or formally validate any adapted tools used.
Clinically, these findings underscore the importance of targeting perceived understanding as a modifiable factor to improve adherence in children with T1DM. Tailored educational programs should be developed to assess and address gaps in caregiver knowledge, ensuring that families are equipped to manage diabetes effectively. Future research should further investigate the integration of perceived understanding into behavioral health models and test its effectiveness in improving diabetes outcomes across settings.
This study provides important insights into the psychological determinants of adherence behaviours among pediatric patients with T1DM in Saudi Arabia. While grounded in the HBM, the study extends the framework by evaluating perceived understanding as an additional cognitive construct. The findings revealed that perceived understanding was the strongest predictor of adherence to dietary, glucose testing, and treatment practices, underscoring its potential role in supporting effective self-management.
Although perceived severity and susceptibility contributed to awareness of disease risks, they did not significantly predict adherence after accounting for perceived understanding. Moreover, sex was identified as a significant factor, with female caregivers more likely to facilitate consistent adherence, reflecting possible differences in caregiving dynamics or health engagement.
These results suggest that enhancing caregivers’ cognitive understanding of diabetes management may improve adherence and reduce the incidence of DKA. Future research should consider expanding behavioural models like the HBM to include perceived understanding and explore its applicability across diverse clinical and cultural settings. Broader investigations incorporating additional psychosocial variables and multi center designs are recommended to strengthen the generalizability and impact of these findings.
| 1. | Kitabchi AE, Umpierrez GE, Miles JM, Fisher JN. Hyperglycemic crises in adult patients with diabetes. Diabetes Care. 2009;32:1335-1343. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1090] [Cited by in RCA: 1186] [Article Influence: 74.1] [Reference Citation Analysis (3)] |
| 2. | Ehrmann D, Kulzer B, Roos T, Haak T, Al-Khatib M, Hermanns N. Risk factors and prevention strategies for diabetic ketoacidosis in people with established type 1 diabetes. Lancet Diabetes Endocrinol. 2020;8:436-446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 73] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 3. | Dayo AR, Wassan SM, Shahid QUA, Soomro AH, Ahmed N, Humaira M. Assessment of the Factors That Can Predict the Occurrence of Diabetic Ketoacidosis in Type 1 Diabetic Patients. PJMHS. 2023;17:749-751. [DOI] [Full Text] |
| 4. | Jefferies CA, Nakhla M, Derraik JG, Gunn AJ, Daneman D, Cutfield WS. Preventing Diabetic Ketoacidosis. Pediatr Clin North Am. 2015;62:857-871. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 46] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 5. | Wysham C, Bindal A, Levrat-Guillen F, Kostadinova D, Poon Y. A systematic literature review on the burden of diabetic ketoacidosis in type 2 diabetes mellitus. Diabetes Obes Metab. 2025;27:2750-2767. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 6. | Szypowska A, Skórka A. The risk factors of ketoacidosis in children with newly diagnosed type 1 diabetes mellitus. Pediatr Diabetes. 2011;12:302-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 52] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 7. | Batwa M, Alharthi L, Ghazal R, Alsulami M, Slaghour R, Aljuhani R, Bakhsh A. Diabetic Ketoacidosis at the Onset of Type 1 Diabetes Mellitus Among Children and Adolescents in Jeddah, Saudi Arabia: A Study From the Emergency Department. Cureus. 2022;14:e24456. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Alsolaimani N, Kattan M, Algabbani Z, Awlia G, Alhamdani Y, AlAgha A. Comparison of pediatric diabetic ketoacidosis in newly diagnosed versus known patients with type 1 diabetes mellitus: A single-center study. Saudi Med J. 2024;45:1326-1333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 9. | Alquwez N, Cruz JP, Almazan JU, Alamri MS, Mesde JJ. The Arabic version of the Kogan Attitudes toward Older People Scale among Saudi nursing students: a psychometric analysis. Ann Saudi Med. 2018;38:399-407. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 10. | Foti Randazzese S, La Rocca M, Bombaci B, Di Pisa A, Giliberto E, Inturri T, Militi D, Lombardo F, Gitto E, Salzano G, Passanisi S. Severe Diabetic Ketoacidosis in Children with Type 1 Diabetes: Ongoing Challenges in Care. Children (Basel). 2025;12:110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 11. | Lucier J, Mathias PM. Type 1 Diabetes. 2024 Oct 5. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. [PubMed] |
| 12. | Al Shaikh A, Farahat F, Saeedi M, Bakar A, Al Gahtani A, Al-Zahrani N, Jaha L, Aseeri MA, Al-Jifree HM, Al Zahrani A. Incidence of diabetic ketoacidosis in newly diagnosed type 1 diabetes children in western Saudi Arabia: 11-year experience. J Pediatr Endocrinol Metab. 2019;32:857-862. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 13. | Ahola AJ, Harjutsalo V, Thomas MC, Forsblom C, Groop PH. Dietary intake and hospitalisation due to diabetic ketoacidosis and hypoglycaemia in individuals with type 1 diabetes. Sci Rep. 2021;11:1638. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Ranjan A, Schmidt S, Damm-Frydenberg C, Holst JJ, Madsbad S, Nørgaard K. Short-term effects of a low carbohydrate diet on glycaemic variables and cardiovascular risk markers in patients with type 1 diabetes: A randomized open-label crossover trial. Diabetes Obes Metab. 2017;19:1479-1484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 60] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 15. | Wolfsdorf JI, Glaser N, Agus M, Fritsch M, Hanas R, Rewers A, Sperling MA, Codner E. ISPAD Clinical Practice Consensus Guidelines 2018: Diabetic ketoacidosis and the hyperglycemic hyperosmolar state. Pediatr Diabetes. 2018;19 Suppl 27:155-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 339] [Cited by in RCA: 404] [Article Influence: 57.7] [Reference Citation Analysis (0)] |
| 16. | Vitale RJ, Card CE, Lichtman JH, Weyman K, Michaud C, Sikes K, Tamborlane WV, Weinzimer SA. An Effective Diabetic Ketoacidosis Prevention Intervention in Children With Type 1 Diabetes. SAGE Open Nurs. 2018;4:2377960818804742. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 17. | Charron-Prochownik D, Moore KR, Stotz S, Akers A, Beirne S, Brega AG, Chalmers L, Fischl A, Garrow H, Gonzales K, Nadeau KJ, O'Banion N, Powell J, Seely E, Powell B, Abujaradeh H, Sereika SM. Comparing American Indian/Alaska Native Adolescent Daughters' and Their Mothers' Awareness, Knowledge, Attitudes, and Behaviors Regarding Risk for Gestational Diabetes: Implications for Mother-Daughter Communication on Reproductive Health. Sci Diabetes Self Manag Care. 2023;49:267-280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 18. | Shah VN, Wu M, Polsky S, Snell-Bergeon JK, Sherr JL, Cengiz E, DiMeglio LA, Pop-Busui R, Mizokami-Stout K, Foster NC, Beck RW; for T1D Exchange Clinic Registry. Gender differences in diabetes self-care in adults with type 1 diabetes: Findings from the T1D Exchange clinic registry. J Diabetes Complications. 2018;32:961-965. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 42] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 19. | Alqarni AM, Alrahbeni T, Qarni AA, Qarni HMA. Adherence to diabetes medication among diabetic patients in the Bisha governorate of Saudi Arabia - a cross-sectional survey. Patient Prefer Adherence. 2019;13:63-71. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 44] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 20. | Benouda S, Ziani I, Assarrar I, Rouf S, Latrech H. Predictive factors of diabetic ketoacidosis in patients with newly onset type 1 diabetes: A single center study. Diabetes Epidemiol Manag. 2024;16:100231. [DOI] [Full Text] |
| 21. | Aljulifi MZ, Mahzari M, Fatani HA, Ardah HI. A Retrospective Study of The Prevalence of Diabetic Ketoacidosis in Saudi Adolescents and Adults with Type 1 Diabetes. J Pioneer Med Sci. 2024;13:4-12. [DOI] [Full Text] |
| 22. | Nasser HA. Assessment of telemedicine by physicians at Prince Sultan Military Medical City. J Nutr Hum Health. 2017;1:1-10. [DOI] [Full Text] |
| 23. | Sullivan KM, Dean A, Soe MM. OpenEpi: a web-based epidemiologic and statistical calculator for public health. Public Health Rep. 2009;124:471-474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 252] [Cited by in RCA: 399] [Article Influence: 24.9] [Reference Citation Analysis (0)] |
| 24. | Fitzgerald JT, Davis WK, Connell CM, Hess GE, Funnell MM, Hiss RG. Development and validation of the Diabetes Care Profile. Eval Health Prof. 1996;19:208-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 220] [Cited by in RCA: 257] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 25. | Walker EA, Mertz CK, Kalten MR, Flynn J. Risk perception for developing diabetes: comparative risk judgments of physicians. Diabetes Care. 2003;26:2543-2548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 93] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 26. | Anderson RM, Fitzgerald JT, Funnell MM, Gruppen LD. The third version of the Diabetes Attitude Scale. Diabetes Care. 1998;21:1403-1407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 111] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 27. | Asaad G, Sadegian M, Lau R, Xu Y, Soria-Contreras DC, Bell RC, Chan CB. The Reliability and Validity of the Perceived Dietary Adherence Questionnaire for People with Type 2 Diabetes. Nutrients. 2015;7:5484-5496. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 44] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 28. | Berg KM, Demas PA, Howard AA, Schoenbaum EE, Gourevitch MN, Arnsten JH. Gender differences in factors associated with adherence to antiretroviral therapy. J Gen Intern Med. 2004;19:1111-1117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 157] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 29. | Choi IH, Kim MS, Hwang PH, Lee D. Clinical and Laboratory Characteristics of Pediatric Diabetic Ketoacidosis: A Single-Center Study. J Korean Diabetes. 2017;18:193. [DOI] [Full Text] |
| 30. | Eltom EH, Alali AOA, Alanazi RKM, Alanazi AAM, Albalawi MAA, Alanazi SAN, Alanazi MSG, Badawy AA, Mokhtar N, Fawzy MS. Exploring Awareness Levels of Diabetic Ketoacidosis Risk Among Patients with Diabetes: A Cross-Sectional Study. Clin Pract. 2024;14:2681-2692. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 31. | Skinner TC, John M, Hampson SE. Social support and personal models of diabetes as predictors of self-care and well-being: a longitudinal study of adolescents with diabetes. J Pediatr Psychol. 2000;25:257-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 133] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 32. | Zainal N, Holloway S, Edney SM. Health belief theories and their influence on adherence behaviours in individuals with diabetic foot ulceration: A literature review. J Wound Manag. 2021;22. [DOI] [Full Text] |
| 33. | Al Hayek AA, Robert AA, Al-Shaikh R, Alhojele M, Aloufi S, Sabri D, Alenazi M, Hassan AH, Al Dawish M. Factors associated with the presence of diabetic ketoacidosis: A retrospective analysis of patients with type 1 diabetes in Saudi Arabia. Diabetes Metab Syndr. 2020;14:2117-2122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 34. | Alotaibi R, Alsulami M, Hijji S, Alghamdi S, Alnahdi Y, Alnahdi H, Samargandy SA. Diabetic ketoacidosis in Saudi Arabia: factors precipitating initial admission and readmission. Ann Saudi Med. 2022;42:119-126. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |