Published online Jul 15, 2024. doi: 10.4239/wjd.v15.i7.1499
Revised: April 25, 2024
Accepted: May 21, 2024
Published online: July 15, 2024
Processing time: 137 Days and 22.9 Hours
The diabetic foot is a common cause of disability and death, and comorbid foot infections usually lead to prolonged hospitalization, high healthcare costs, and a significant increase in amputation rates. And most diabetic foot trauma is com
To establish the efficacy and safety of endovascular revascularization (ER) com
Clinical data were collected from 40 patients with diabetic foot admitted to the Second Affiliated Hospital of Soochow University from April 2018 to April 2022. Diabetic foot lesions were graded according to Wagner’s classification, and blood flow to the lower extremity was evaluated using the ankle-brachial index test and computerized tomography angiography of the lower extremity arteries. Conti
Of the 35 cases treated with lower limb revascularization, 34 were successful with a revascularization success rate of 97%. Of these, 6 cases underwent stenting after BA of the superficial femoral artery, and 1 received popliteal artery stent im
ER in combination with VAC is a safe and effective treatment for diabetic foot that can significantly improve limb salvage rates. The use of VAC after ER simplifies and facilitates wound repair.
Core Tip: Diabetic foot trauma complicating lower-extremity arteriopathy is an independent risk factor for major amputation in patients with diabetic foot. Revascularization and wound repair are the two fundamental interventions in the treatment of diabetic foot. This study demonstrated that endovascular revascularization combined with vacuum-assisted closure is safe and effective treatment and can significantly improve limb salvage rates.
- Citation: Lei FR, Shen XF, Zhang C, Li XQ, Zhuang H, Sang HF. Clinical efficacy of endovascular revascularization combined with vacuum-assisted closure for the treatment of diabetic foot. World J Diabetes 2024; 15(7): 1499-1508
- URL: https://www.wjgnet.com/1948-9358/full/v15/i7/1499.htm
- DOI: https://dx.doi.org/10.4239/wjd.v15.i7.1499
Diabetic foot is a common cause of disability and death and a major cause of hospitalization in patients with diabetes. Comorbid foot infections often lead to prolonged hospital stays, high medical costs, and a significant increase in the limb amputation rate. Lower-extremity ischemia is a high-risk factor for the occurrence of diabetic foot and, consequently, difficult healing of diabetic foot wounds. Approximately 47.5% of diabetic foot wounds are complicated by lower-extremity arterial lesions, which is an independent risk factor for major amputations in patients with diabetic foot. Moreover, the complicated wound care of diabetic foot exacerbates treatment difficulty. This study summarizes the cases of diabetic foot treated by endovascular revascularization (ER) combined with vacuum-assisted closure (VAC) at our hospital in the last 4 years.
The data on 40 patients with diabetic foot admitted to the Department of Vascular Surgery of the Second Affiliated Hospital of Soochow University from April 2018 to April 2022 were retrospectively analyzed. The research participants had a male-to-female ratio of 28:12, an average age of 72.36 ± 8.57 years (range: 52-90 years), and a mean length of hospital stay of 21.6 ± 3.7 d. Lesions of the superficial femoral (SFA), popliteal (POA), and infrapopliteal arteries (IPA) were found in 12, 9, and 26 cases, respectively. Twenty-seven cases were complicated with hypertension, 10 with hyperlipidemia, 4 with coronary heart disease, 6 with renal insufficiency, 3 with uremia, 3 with cerebral infarction, and 1 with toe amputation. Four cases were categorized as Wagner’s classification grade 1, 7 cases as grade 2, 16 cases as grade 3, and 13 cases as grade 4 (Tables 1 and 2).
| Parameters | n = 40 |
| Age (yr) | 72.36 ± 8.57 |
| Male | 28 |
| Risk factor | |
| Smoking | 23 |
| Diabetes | 40 |
| Hypertension | 27 |
| Hyperlipidemia | 10 |
| Renal insufficiency | 6 |
| Coronary heart disease | 4 |
| History of cerebrovascular disease | 3 |
| History of dialysis | 3 |
| Target vessel for revascularization | |
| Balloon angioplasty of femoral and popliteal arteries | 15 |
| Superficial femoral artery stenting | 6 |
| Popliteal artery stenting | 1 |
| Reconstruction of anterior tibial artery | 11 |
| Reconstruction of posterior tibial artery | 15 |
| Reconstruction of peroneal artery | 13 |
| Wound treatment | |
| Number of cases of VAC | 32 |
| Number of cases of simple skin grafting | 24 |
| Number of cases of skin flap transplantation | 2 |
| Stage | 0 | 1 | 2 | 3 |
| A: No ischemia/infection | 0 | 0 | 0 | 0 |
| B: Infection | 0 | 0 | 5 | 0 |
| C: Ischemia | 0 | 2 | 0 | 0 |
| D: Ischemia + infection | 0 | 5 | 18 | 10 |
Infection assessment: First, patients were scored using the Wagner’s grading system and evaluated for foot infections. In the case of infection, empirical antimicrobial administration was given as first-line treatment (secretion culture was performed simultaneously). For patients with abscess, timely incision and drainage were performed, either at the bedside or in the operating room according to the patient’s general situation. Bedside debridement using the nibbling debri
Glycemic control and conventional medications: The member endocrinologist of the diabetic foot multidisciplinary team (MDT) evaluated the glycemic control of patients and implemented continuous subcutaneous insulin infusion pumps to control blood sugar. Blood pressure was controlled by oral administration of antiplatelet drugs (aspirin 100 mg/d or clopidogrel 75 mg/d) and lipid-lowering drugs. Cardiac and renal functions were also evaluated.
Assessment of lower limb blood transport: Ankle-brachial index (ABI) tests were performed to assess the degree of lower limb ischemia. If the ABI was less than 0.7, computerized tomography angiography (CTA) was performed to evaluate lower limb arterial lesions and tailor the revascularization program. Hydration was performed before and after CTA for patients with renal dysfunction.
Revascularization: Endovascular angioplasty was performed to revascularize the lower extremity. Anterograde or retrograde puncture using crosses sheath technology was performed, depending on the target lesion. If the guidewire revealed a true-lumen stenosis or occlusion segment, balloon angioplasty (BA) was performed to expand the lesion segment. If the post-BA angiography showed a well-defined lumen of the diseased segment, drug-coated BA (DCBA) was performed for dilation. For patients with severe SFA calcification or long-segment occlusion, a retrograde puncture was made to unblock the distant and proximal end convergences of the distal good blood vessels, and, if the guidewire entered the subintimal artery, to establish a guidewire track that facilitated BA or stenting. For POA lesions, true-lumen wire passage was preferred over stent placement. For IPA lesions, attempts were made to establish true-lumen wire passage, and BA was performed to open at least one complete outflow tract (anterior tibial, posterior tibial, or peroneal artery). The common femoral artery was evaluated by preoperative computerized tomography to determine whether to perform puncture site stapler suture or compression to stop bleeding.
Wound repair: For patients with abscess with good blood supply, incision and drainage were performed, after which necrotic tissue was removed daily by bedside nibbling debridement. When the infection had been mostly controlled, thorough debridement and VAC aspiration were performed simultaneously in the operating room to promote gra-nulation tissue formation on the wound surface. Skin grafting or flap repair was performed after sufficient growth of the granulation tissue. The wound was then transplanted with autologous split-thickness skin grafts, with holes distributed throughout the middle of the skin graft to promote drainage and intermittent sutures created around the wound. Following skin grafting, the wound was treated with topical VAC for 1 wk. The VAC was subsequently removed to check the survival of the skin graft. Necrotomy of the local toe was indicated for patients with dry gangrene 1 wk after revascularization.
Follow-up: Patients were followed up through outpatient visits at 2 wk and 1, 2, 3, and 6 months after discharge, and then every 3 months by outpatient visit or telephone consultation. Lower-extremity artery ultrasound, ABI, CTA, and other examinations were performed to monitor the relevant endpoint events, including target vessel primary patency rate, ulcer healing rate, and claudication distance.
SPSS 25.0 statistical software was used for analysis and processing. Measurement data were statistically described as mean ± SD. Kaplan-Meier survival analysis was performed to determine the target vessel primary patency rate. A P-value < 0.05 denoted statistical significance.
Thirty-five cases underwent revascularization of the affected limb, one of which failed, with an ER success rate of 97%. Of these, 25 cases were treated by antegrade puncture and 10 by retrograde puncture of the contralateral femoral artery using crosses sheath technology, with 2 cases developing puncture site hematoma. In total, 6 cases of SFA stent implantation, 1 case of stent POA (P1 and P2 segments) implantation, and 7 cases of distal retrograde puncture were performed. In 25 cases of IPA lesions, 39 arteries were dilated by BA, 7 of which were treated by DCBA and the remaining 32 by plain old balloon angioplasty (POBA). One case underwent tibiofibular artery dissection, but with no blood flow nor flow obstruction. No IPAs were stented. One patient suffered a myocardial infarction postoperatively, which was treated conservatively. Patients with renal insufficiency were hydrated before and after surgery, and no postoperative contrast nephropathy was observed. The endocrinology MDT team successfully controlled all patients’ blood glucose within the ideal range through the insulin pumps.
The dressings of infected abscess were changed daily, and the abscess was debrided and drained. VAC was used to treat the wound in 32 cases. Twenty-four cases underwent skin grafting, and all skin grafts survived successfully. Two flap grafts were performed, one for heel necrosis, with a free-style perforator flap, and the other for a medial malleolus ulcer using an anterolateral thigh flap. In total, 17 minor amputations and 2 major amputations (below-knee amputation) were performed, and the success rate of foot preservation was 95%. The wound healing rate was 100%, and the mean length of hospital stay was 21.6 ± 7.5 d.
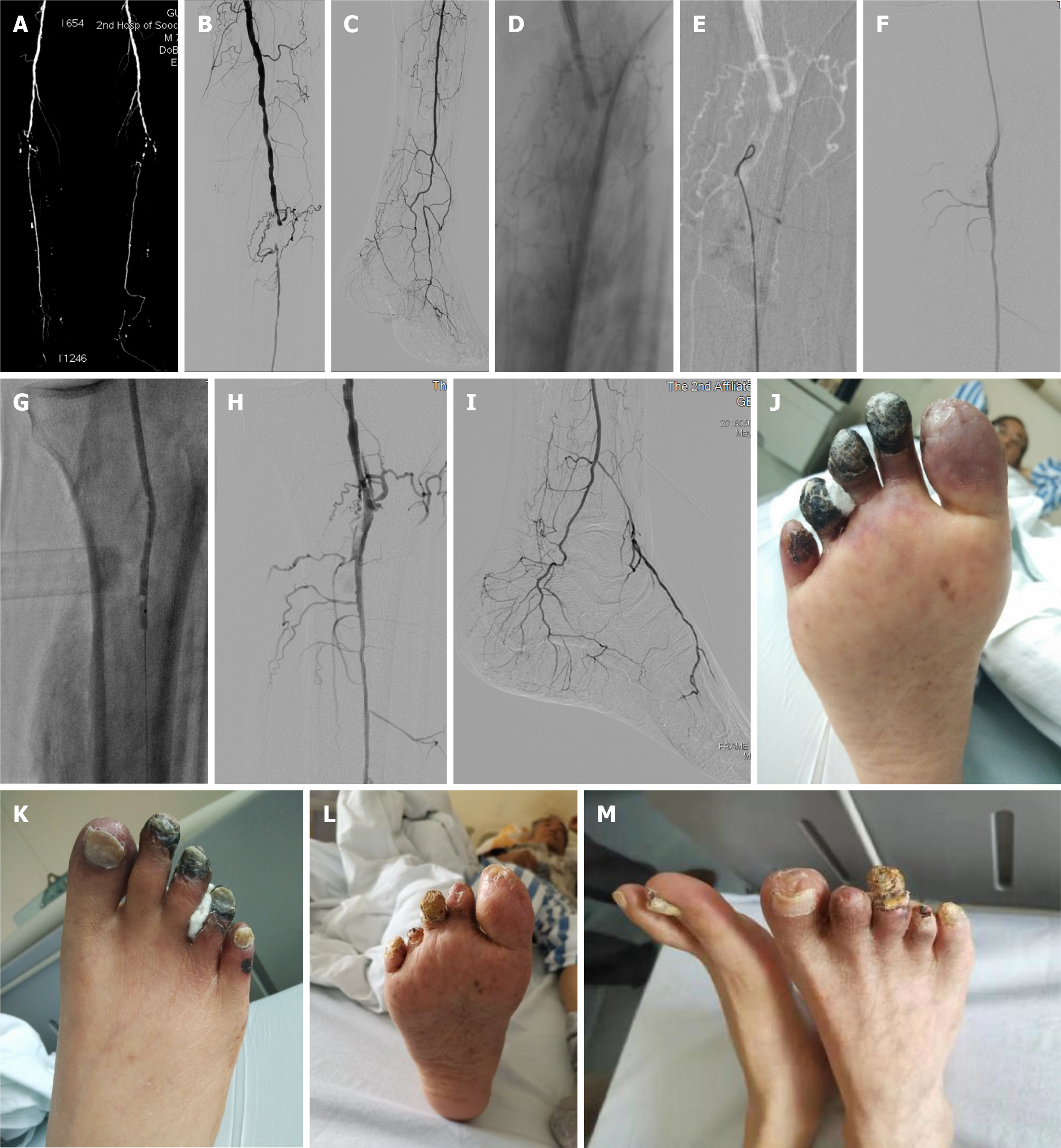
All 40 cases were followed up successfully, with a maximum follow-up of 36 months (mean: 26.7 ± 7.6 months). Two patients experienced cerebral infarction at the 1-year follow-up, with one dying 1 year later and the other maintaining limb function after active treatment. One case of renal insufficiency was found at 2 years’ follow-up. One patient died a year later from a sudden myocardial infarction. Two patients experienced in-stent SFA restenosis with intermittent claudication at 1 year postoperatively and underwent BA again. One patient was diagnosed with lung cancer 3 years later and died 3 months later. Three patients experienced recurrent toe ulceration 1 year postoperatively, which was assessed to be caused by shoe friction. The ulcers healed after local dressing changes without revascularization. The primary patency rate in patients who underwent revascularization was 78.74% in June and 67.78% in December (Figures 1-4).
Since the diabetic foot was first described by OAKLEY and COHEN[1] in 1955, it has become one of the most serious and costly chronic complications and a major cause of amputation in patients with diabetes. Diabetic foot accounts for 40%-60% of all nontraumatic lower-extremity amputations. Peripheral artery disease and infection are the leading causes of lower-leg amputations in patients with diabetes. Adverse clinical outcomes in patients with diabetic ischemic foot ulcers are associated with several factors, including infection, neuropathy, heart failure, and renal failure. Revascularization techniques for lower-extremity arteries, especially IPA, are important measures for limb salvage. Improving tissue perfusion to promote wound healing and preserve limbs through revascularization is an important component and therapeutic goal in the multidisciplinary treatment of diabetic foot. However, revascularization modalities remain highly controversial. The long-term patency rate of autogenous great saphenous vein bypass grafting is higher than that of stenting. However, in most diabetes cases, which are often complicated by multiple medical conditions, a great saphe
BA, the most basic modality of lower limb arterial revascularization, is also currently the most commonly used. Since most of the lower-extremity vascular lesions involve the IPA and SFA, anterograde femoral artery puncture is performed as comprehensively as possible. This is because anterograde puncture can establish a shorter path, provide better guidewire manipulation for the opening of the IPA, and allow preoperative evaluation of the common femoral artery by color ultrasound or CTA. As far as SFA lesions are concerned, true-lumen tracking using the guidewire should be performed as much as possible. If the guidewire enters into the subintimal space, it should not be forced forward to break through to avoid causing a more extensive flow-limiting dissection; a distal retrograde puncture should be considered instead. In our case series, 5 patients underwent retrograde puncture (2 cases in the POA P3 segment, 2 cases in the peroneal artery, and 1 case in the posterior tibial artery). The POA P3 segment, tibiofibular trunk, peroneal artery, posterior tibial artery, or anterior tibial artery can be selected for retrograde puncture, which can be performed by dynamic angiography or along the route. A growing body of evidence shows that good vascular preparation, true-lumen access, DCBA, and a low stent implantation rate can improve the primary patency rate and reduce the long-term re-intervention rate for femoral and POA lesions. This study included 5 cases of SFA stent implantation, 2 of which developed intermittent claudication at 6 and 11 months postoperatively and underwent BA again. However, 7 patients who underwent DCBA did not undergo another ischemic intervention during the 3-year follow-up period. Simple infrapopliteal lesions are a common type of ischemic diabetic foot. POBA and drug-coated balloon (DCB) are still performed for the treatment of IPA lesions because conventional stent implantation is generally not recommended for IPA. The results of a meta-analysis[5] revealed that, compared with POBA, DCB had no statistically significant differences in the incidence of major adverse events, all-cause mortality, major amputation, and target lesion revascularization at 12 months after surgery. The present study included 16 cases of IPA lesions, of which only 3 were treated with DCBA because of financial reasons, whereas the remaining 13 were treated with POBA. Nevertheless, all cases achieved good limb preservation.
Dilaver et al[6] conducted a systematic evaluation and meta-analysis involving 22 studies (4146 limbs) to compare the therapeutic effects of direct and indirect revascularization of IPA. They found that, compared with indirect revascularization, direct revascularization of IPA increased wound healing and limb salvage rates without affecting mortality or re-intervention rates. Alexandrescu et al[7] found through an 8-year prospective bi-center study that wound healing in patients with diabetes could be more significantly accelerated through direct revascularization. However, no significant benefit was found in terms of major limb adverse events and limb preservation. We believe that as long as IPA is opened with a good outflow tract, the blood supply to the affected foot can be sufficiently improved. However, outcomes may depend on whether the patient has a good plantar arch. Jung et al[8] and Nakama et al[9] demonstrated that pedal artery angioplasty facilitated wound healing in patients with CLI. Rashid et al[10] and Troisi et al[11] evaluated arch quality in patients with surgical revascularization and ER, respectively, and found a correlation with clinical outcomes. In the present study, the arch of the foot was opened only in three cases, while the rest of the affected foot presented good collateral compensation in the chronic course.
A complicated abscess infection also increases the difficulty of treatment of diabetic foot and is a major reason for prolonged hospitalization of patients with diabetic foot. Diabetic foot is complicated by the combination of complex infection and wound; thus, the assessment of foot infection is prioritized after admission. For cases complicated with abscess and wet gangrene, incision and drainage should be performed as soon as possible and sufficiently to ensure smooth drainage. Daily bedside dressing changes are required, and nibbling debridement in stages and batches should be performed. The section of foot with definite necrosis should be debrided promptly. For sections with unclear boundaries that present difficulty in determining complete necrosis, they should be temporarily retained. Subcutaneous tissue, adipose tissue, fascia, and muscle that have lost vitality should be removed. The necrotic tendon should be retained to the maximum extent to preserve limb function. Necrotic bone fragments can be gradually removed in patients with severe bone destruction and osteomyelitis caused by infection. For suspected anaerobic bacteria infection or deep wound sinuses with purulent secretion and odor, hydrogen peroxide can be used for cleaning, and the sinus tract can be excised in time if necessary. We believe that the importance of incision and drainage is much higher than the use of antibiotics. For ischemic dry gangrene without serious infection, appropriate disinfection can be performed to avoid the expansion of necrosis caused by early debridement as much as possible. After gradual debridement, granulation tissue gradually forms. Revascularization can be performed in patients with ischemia when inflammatory markers are reduced and local infection is effectively controlled. The growth of the wound surface will be significantly accelerated after revascularization, and optional thorough debridement can be performed in the operating room. We use femoral nerve block anesthesia or local anesthesia as most patients with diabetes have concurrent medical diseases and a poor general condition. In our case series, a patient with a cardiac ejection fraction of only 35% successfully underwent debridement, and VAC aspiration was performed subsequently. We believe that because patients with diabetic foot often have many comorbidities and are complicated with medical conditions (e.g., cardiac insufficiency, old myocardial infarction, renal insufficiency, chronic obstructive pulmonary disease, and hypoproteinemia), wound repair should be as simple as possible. For those with small wounds, two VAC aspiration procedures may achieve satisfactory results. For patients with large wounds and good general condition, autologous split-thickness skin grafting can be performed. Because of good postoperative blood supply, all cases with split-thickness skin grafts successfully gained patency 1 wk after revascularization. One patient in this study underwent extensive skin grafting because most of the patient’s dorsum and plantar skin had been removed by debridement when the patient was referred to our hospital, with some active tissues found on the outside of the plantar. The skin on the inner thighs of both legs was trimmed into split-thickness skin grafts to cover the wound, and the foot was successfully preserved (Figure 2). A patient with thrombocytopenia on long-term oral hormones received several negative pressure treatments, but little granulation tissue formed on the wound surface. Therefore, the wound was repaired with a free anterolateral thigh perforator flap (end-to-side anastomosis with the posterior tibial artery). A case of infected heel with gangrene was repaired by free-style perforator flap combined with plastic surgery. The rest of the patients underwent autologous split-thickness skin grafting after VAC, which was simple and feasible, with a survival rate of 100%. Vacuum sealing drainage (VSD) and VAC are the two key modalities of negative pressure wound therapy. However, we believe that VAC is superior to VSD in the following aspects: (1) The negative pressure value is accurate and controllable, which is more advantageous for diabetic foot with ischemia, and low negative pressure is more likely to promote granulation tissue formation; (2) VAC can be modified to intermittent vacuum drainage, which is more suitable for wound granulation tissue growth; and (3) because of the long wound repair time of some patients, the use of VAC enables patients to get out of bed and even be discharged while avoiding the incidence of deep vein thrombosis.
Although revascularization and wound repair are the two most important interventions in the treatment of diabetic foot, a comprehensive medical diagnosis and treatment scheme must be developed to cover the protection and hydration of renal function before endovascular treatment, the evaluation of cardiac function (evaluated if necessary), digestive function, nutritional status, and the application of oral drugs[12] because most patients with diabetic foot have multiple concurrent diseases. Establishing a good follow-up program after discharge is also critical, as most patients with diabetic foot have low overall education level and low compliance. Good outpatient follow-up can greatly reduce the recurrence rate of ulcers and improve the long-term foot preservation rate. This study is limited by the retrospective design, which does not allow randomization of patients. Therefore, to further confirm our findings, a well-designed randomized controlled trial with prospective data collection and sample size calculation should be performed. The data obtained would help develop an optimal management approach for patients with diabetic foot.
| 1. | OAKLEY W, COHEN SM. Diabetic gangrene. Trans Med Soc Lond. 1955;71:90-107. [PubMed] |
| 2. | Adam DJ, Beard JD, Cleveland T, Bell J, Bradbury AW, Forbes JF, Fowkes FG, Gillepsie I, Ruckley CV, Raab G, Storkey H; BASIL trial participants. Bypass versus angioplasty in severe ischaemia of the leg (BASIL): multicentre, randomised controlled trial. Lancet. 2005;366:1925-1934. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1636] [Cited by in RCA: 1390] [Article Influence: 69.5] [Reference Citation Analysis (0)] |
| 3. | Farber A, Menard MT, Conte MS, Kaufman JA, Powell RJ, Choudhry NK, Hamza TH, Assmann SF, Creager MA, Cziraky MJ, Dake MD, Jaff MR, Reid D, Siami FS, Sopko G, White CJ, van Over M, Strong MB, Villarreal MF, McKean M, Azene E, Azarbal A, Barleben A, Chew DK, Clavijo LC, Douville Y, Findeiss L, Garg N, Gasper W, Giles KA, Goodney PP, Hawkins BM, Herman CR, Kalish JA, Koopmann MC, Laskowski IA, Mena-Hurtado C, Motaganahalli R, Rowe VL, Schanzer A, Schneider PA, Siracuse JJ, Venermo M, Rosenfield K; BEST-CLI Investigators. Surgery or Endovascular Therapy for Chronic Limb-Threatening Ischemia. N Engl J Med. 2022;387:2305-2316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 510] [Cited by in RCA: 486] [Article Influence: 162.0] [Reference Citation Analysis (0)] |
| 4. | Faglia E, Dalla Paola L, Clerici G, Clerissi J, Graziani L, Fusaro M, Gabrielli L, Losa S, Stella A, Gargiulo M, Mantero M, Caminiti M, Ninkovic S, Curci V, Morabito A. Peripheral angioplasty as the first-choice revascularization procedure in diabetic patients with critical limb ischemia: prospective study of 993 consecutive patients hospitalized and followed between 1999 and 2003. Eur J Vasc Endovasc Surg. 2005;29:620-627. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 295] [Cited by in RCA: 260] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 5. | Cai H, Dong J, Ye Y, Song Q, Lu S. Safety and Efficacy of Drug-Coated Balloon in the Treatment of Below-the-Knee Artery: A Meta-analysis. J Surg Res. 2022;278:303-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 6. | Dilaver N, Twine CP, Bosanquet DC. Editor's Choice - Direct vs. Indirect Angiosomal Revascularisation of Infrapopliteal Arteries, an Updated Systematic Review and Meta-analysis. Eur J Vasc Endovasc Surg. 2018;56:834-848. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 31] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 7. | Alexandrescu VA, Brochier S, Limgba A, Balthazar S, Khelifa H, De Vreese P, Azdad K, Nodit M, Pottier M, Van Espen D, Sinatra T. Healing of Diabetic Neuroischemic Foot Wounds With vs Without Wound-Targeted Revascularization: Preliminary Observations From an 8-Year Prospective Dual-Center Registry. J Endovasc Ther. 2020;27:20-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 27] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 8. | Jung HW, Ko YG, Hong SJ, Ahn CM, Kim JS, Kim BK, Choi D, Hong MK, Jang Y. Editor's Choice - Impact of Endovascular Pedal Artery Revascularisation on Wound Healing in Patients With Critical Limb Ischaemia. Eur J Vasc Endovasc Surg. 2019;58:854-863. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 30] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 9. | Nakama T, Watanabe N, Haraguchi T, Sakamoto H, Kamoi D, Tsubakimoto Y, Ogata K, Satoh K, Urasawa K, Andoh H, Fujita H, Shibata Y. Clinical Outcomes of Pedal Artery Angioplasty for Patients With Ischemic Wounds: Results From the Multicenter RENDEZVOUS Registry. JACC Cardiovasc Interv. 2017;10:79-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 82] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 10. | Rashid H, Slim H, Zayed H, Huang DY, Wilkins CJ, Evans DR, Sidhu PS, Edmonds M. The impact of arterial pedal arch quality and angiosome revascularization on foot tissue loss healing and infrapopliteal bypass outcome. J Vasc Surg. 2013;57:1219-1226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 115] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 11. | Troisi N, Turini F, Chisci E, Ercolini L, Frosini P, Lombardi R, Falciani F, Baggiore C, Anichini R, Michelagnoli S. Impact of Pedal Arch Patency on Tissue Loss and Time to Healing in Diabetic Patients with Foot Wounds Undergoing Infrainguinal Endovascular Revascularization. Korean J Radiol. 2018;19:47-53. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 31] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 12. | Wang AH, Xu ZR. Drug treatment of diabetes complicated with arterial occlusive disease of lower limbs. Zhonghua Yixue Zazhi. 2012;92:219-220. [DOI] [Full Text] |