Published online Mar 15, 2024. doi: 10.4239/wjd.v15.i3.440
Peer-review started: November 8, 2023
First decision: December 26, 2023
Revised: January 3, 2024
Accepted: February 18, 2024
Article in press: February 18, 2024
Published online: March 15, 2024
Processing time: 128 Days and 4.1 Hours
Patients with diabetes mellitus (DM) are predisposed to an increased risk of infection signifying the importance of vaccination to protect against its potentially severe complications. The Centers for Disease Control and Prevention/Advisory Committee on Immunization Practices (CDC/ACIP) issued immunization re-commendations to protect this patient population.
To assess the adherence of patients with DM to the CDC/ACIP immunization recommendations in Saudi Arabia and to identify the factors associated with the vaccine adherence rate.
An observational retrospective study conducted in 2023 was used to collect data on the vaccination records from 13 diabetes care centers in Saudi Arabia with 1000 eligible patients in phase I with data collected through chart review and 709 patients in phase II through online survey.
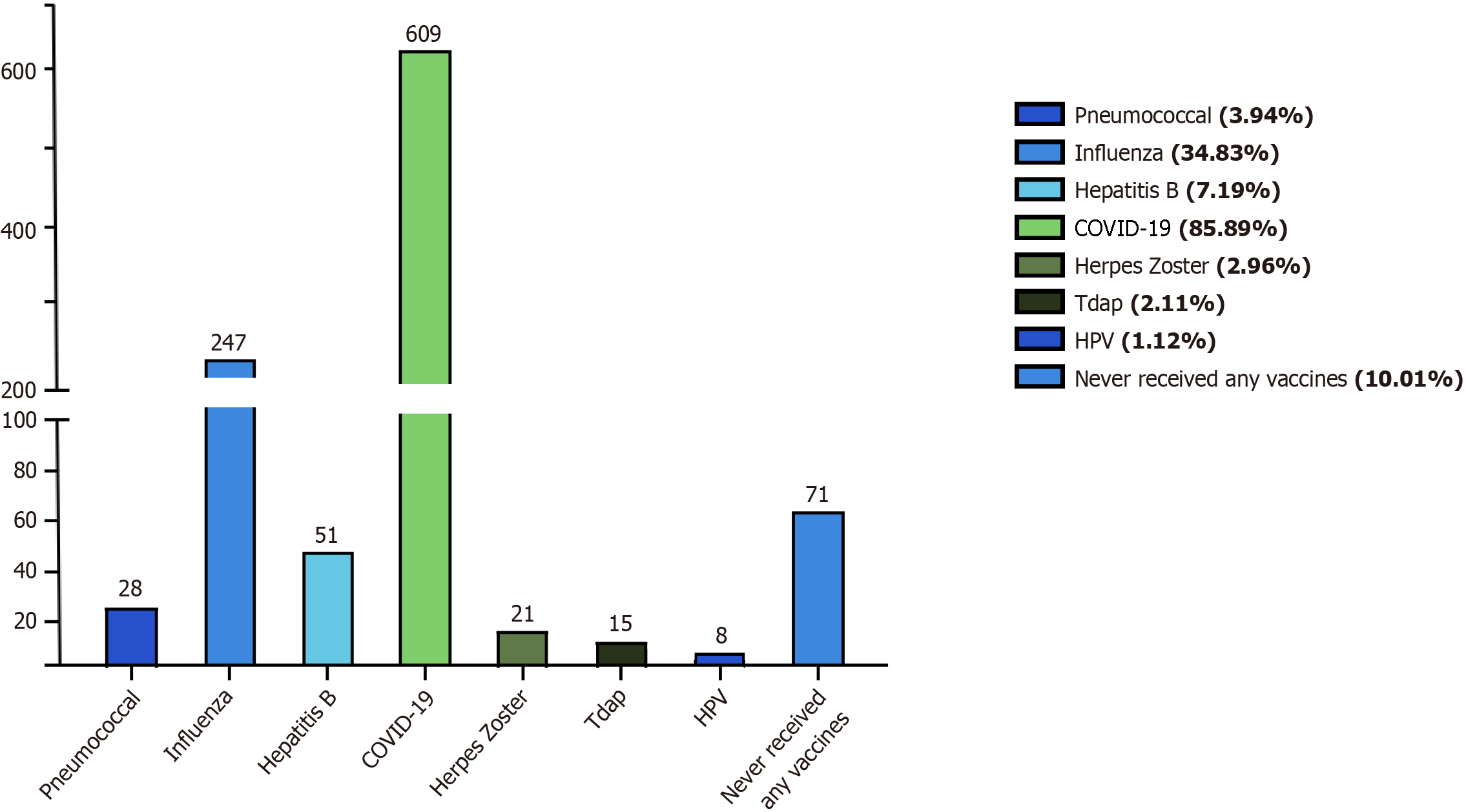
Among participants, 10.01% (n = 71) had never received any vaccine, while 85.89% (n = 609) received at least one dose of the coronavirus disease 2019 (COVID-19) vaccine, and 34.83% (n = 247) had received the annual influenza vaccine. Only 2.96% (n = 21), 2.11% (n = 15), and 1.12% (n = 8) received herpes zoster, tetanus, diphtheria, and pertussis (Tdap), and human papillomavirus (HPV) vaccines, respectively. For patients with DM in Saudi Arabia, the rate of vaccination for annual influenza and COVID-19 vaccines was higher compared to other vaccinations such as herpes zoster, Tdap, pneumococcal, and HPV. Factors such as vaccine recommendations provided by family physicians or specialists, site of care, income level, DM-related hospitalization history, residency site, hemoglobin A1c (HbA1c) level, and health sector type can significantly influence the vaccination rate in patients with DM. Among non-vaccinated patients with DM, the most reported barriers were lack of knowledge and fear of side effects. This signifies the need for large-scale research in this area to identify additional factors that might facilitate adherence to CDC/ACIP vaccine recommendations in patients with DM.
In Saudi Arabia, patients with DM showed higher vaccination rates for annual influenza and COVID-19 vaccines compared to other vaccinations such as herpes zoster, Tdap, pneumococcal, and HPV. Factors such as vaccine recommendations provided by family physicians or specialists, the site of care, income level, DM-related hospitalization history, residency site, HbA1c level, and health sector type can significantly influence the vaccination rate in patients with DM.
Core Tip: Given the increasing prevalence of diabetes in Saudi Arabia, this national study sheds light on vaccine practices for patients with diabetes mellitus in Saudi Arabia with regard to the Advisory Committee on Immunization Practices vaccine recommendations. The findings of this protocol will aid decision-makers in improving preventative vaccine care for patients with diabetes.
- Citation: Alqifari SF, Esmail AK, Alarifi DM, Alsuliman GY, Alhati MM, Mutlaq MR, Aldhaeefi M, Alshuaibi SA, Amirthalingam P, Abdallah A, Wasel AS, Hamad HR, Alamin S, Atia TH, Alqahtani T. Adherence to Advisory Committee on Immunization Practices in diabetes mellitus patients in Saudi Arabia: A multicenter retrospective study. World J Diabetes 2024; 15(3): 440-454
- URL: https://www.wjgnet.com/1948-9358/full/v15/i3/440.htm
- DOI: https://dx.doi.org/10.4239/wjd.v15.i3.440
Diabetes mellitus (DM) is a complex metabolic disorder characterized by long-term elevated blood sugar levels due to insufficient insulin production, insulin resistance, or both[1]. Globally, data from the International Diabetes Federation reveals that in 2021, approximately 537 million adults worldwide were affected by DM. Projections suggest that this number is expected to increase to 643 million by 2030 and further escalate to 783 million by 2045[2]. In Saudi Arabia, DM impacts roughly 20% of the adult population, with projections indicating that by 2030, the number of cases will more than double[3].
Worldwide, the burden of DM has led to approximate health expenses of 966 billion United States dollars. These expenses are projected to surpass 1.054 trillion United States dollars by 2045[4]. In Saudi Arabia, the escalating prevalence of DM is emerging as a significant contributor to medical complications and fatalities, imposing an economic burden measured at 17 billion Saudi riyals in 2018[5].
Vaccinations play a crucial role in preventing infectious diseases and promoting immunity, particularly for individuals with DM. This significance is evident in the 2011-2020 Global Vaccine Action Plan, built on the ideal that “The benefits of immunization to be equitably extended to all people”[6]. This includes high-risk groups vulnerable to vaccine-preventable diseases, such as patients with chronic and immune-compromising diseases[7]. Factors like impaired immunity, a prolonged course of the disease, poor diabetes control, hyperglycemia, and comorbidities make patients with DM more susceptible to infections and serious complications[8].
According to the World Health Organization, the mortality rate in cases of pneumococcal infection is estimated to be approximately 10%-20%, with rates exceeding 50% in high-risk populations. It is assumed that patients with DM who develop pneumonia-related complications face a nearly threefold higher risk of mortality in comparison to the general population[9]. Annually, influenza is responsible for approximately 10000 to 30000 fatalities, and individuals with DM have a sixfold increased likelihood of hospitalization during an outbreak compared to those without DM[8]. Through extensive efforts to promote vaccination within this vulnerable population, which have shown promising results, a study indicated that the influenza vaccine effectively reduced rates of hospitalization and mortality, with a number needed to treat of 60, 319, and 250 for all-cause hospitalizations, specific hospitalization, and all-cause mortality, respectively[10]. Another study demonstrated a decline in the risk of invasive pneumococcal disease (adjusted odds ratio = 0.86, 95% confidence interval: 0.78-0.94) among vaccinated patients compared to unvaccinated patients, along with a shorter length of stay at the hospital (-1.27 ± 0.19 d, P = 0.0012)[11]. This reinforces the importance of implementing vaccine recom-mendations and strictly encouraging adherence to these vaccinations.
Similar to other adults and as recommended by the Centers for Disease Control and Prevention (CDC) Advisory Committee on Immunization Practices (ACIP), patients with DM should receive vaccinations against coronavirus disease 2019 (COVID-19), influenza, tetanus, diphtheria, and pertussis (Tdap), as well as tetanus and diphtheria boosters. Additionally, individuals with DM must also receive the pneumococcal vaccine, hepatitis B vaccine, human papillomavirus (HPV) vaccine, herpes zoster (Shingles) vaccine, measles, mumps, and rubella (MMR) vaccine, and chickenpox vaccine. The CDC/ACIP recommendations are summarized in Table 1[12].
| Vaccine | Recommendation |
| IIV (IIV4 or RIV4 or LAIV) | Received every year |
| Tdap and Td vaccine | Tdap is received once followed by a Td booster dose every ten years |
| PCV (PCV151 or PCV20) | Given once to previously unimmunized diabetic adults who are 19-64 years old or unimmunized adults ≥ 65 |
| Hepatitis B vaccine | All previously unimmunized adults 19-59 years old. Diabetic adults ≥ 60 years old |
| HPV vaccine | Given in two or three doses as early as 9 years old and up to 26 years old and in some cases up to 47 years old |
| Herpes zoster vaccine | All adults ≥ 50 |
| Chickenpox (varicella) vaccine | Two doses with 4-8 wk interval to all previously unimmunized ≥ 13 adolescents and adult |
| MMR vaccine | One or two doses with 28 d interval for unimmunized adults |
Worldwide, adherence to these vaccinations among adult patients with DM has been investigated in a few single-center studies. A cross-sectional study conducted at Kent Hospital in the United Kingdom, involving 100 patients, revealed a notably low adherence rate to the ACIP recommendations for hepatitis B, pneumococcal, and influenza vaccines among patients with DM. Specifically, for the hepatitis B vaccine, 39% of vaccine-eligible patients reported non-compliance[13]. Additionally, a recent meta-analysis study noted that 27.8% of patients expressed reluctance to receive the COVID-19 vaccination[14].
To date, only three studies have been conducted in Saudi Arabia to assess vaccination adherence among patients with DM. These studies were either single-centered or focused on only one to three vaccines. A study conducted in Taif City among 336 patients found that only 43.5% of patients with DM received the influenza vaccine, contradicting the 61% expected adherence rate reported in 2017[15]. Another study at King Abdulaziz University Hospital in Jeddah showed a very low uptake rate of influenza, pneumococcal, and hepatitis B vaccines among admitted patients with DM, with only 1.17% of the 832 participants receiving all three vaccines[16].
This study was conducted over two phases. Phase I included an observational retrospective chart review from 13 diabetes care centers in Saudi Arabia. Subsequently, in phase II, we administered an online survey with electronic consent to patients with DM who have established care at those 13 diabetes care centers, aiming to gather additional information on socioeconomic, educational, and living status.
Participants’ vaccine records were reviewed by two independent teams of physicians and assessed for adherence to the latest vaccine recommendations announced in 2023 by ACIP and the CDC. Demographic data were collected from each participant, including gender, age, education, monthly household income, and living status, which was divided into two categories: City (a large human settlement with a significant population and extensive facilities) and village (a smaller settlement situated in a rural area with a small population ranging from hundreds to thousands), as well as body weight. Additionally, we collected data on hemoglobin A1c (HbA1c) levels, pre-existing conditions, DM duration, healthcare sector (either governmental sector - a public sector that provides free health-related services for Saudi citizens - or private sector - centers that deliver health services for all residents of the country and are funded by self-pay or insurance), preference for diabetic care (whether primary health care centers - centers provided by the Ministry of Health to offer primary health care to the regions it serves through applying a comprehensive care strategy for family medicine - or diabetes care centers - a center with a specialized diabetologist or endocrinologist; or none), frequency of diabetes provider visits (monthly, quarterly, annually, or none), diabetes regimen (oral medications, insulin, insulin and oral medications, no medications), frequency of total daily medications, and previous hospitalization due to diabetes complications. Finally, data about the reasons for non-adherence to vaccinations among non-vaccinated patients with DM were collected, with patients choosing one of several reasons: “I do not know the importance of these vaccines for diabetes”, “fear of side effects”, “the vaccines were not suggested by the doctor”, “I think the vaccine is not important”, “not educated about the importance of vaccines by the doctor”, “lack of vaccine”, or “reason not disclosed”.
We expressed categorical variables as frequencies and percentages, while continuous variables were presented as means and standard deviations or as medians and minimum-maximum ranges. To compare continuous variables between two groups, we utilized an independent Student’s t-test, while a one-way ANOVA was employed for the comparison of more than two groups. Additionally, we utilized the Tukey test for multiple comparisons of the subgroups. A predetermined significance level of P < 0.05 was used to detect differences between study groups. The statistical analysis was conducted using the SPSS version 26.0. Bar diagrams were generated using GraphPad Prism version 9.0. The study protocol (607-43-6007) received IRB approval from the Regional Research Ethics Committee, Ministry of Health, Saudi Arabia.
Out of 1000 eligible patients whose charts were reviewed in phase I, a total of 709 adult patients with DM consented and participated in phase II, being included in this study. Among the 709 adults with DM surveyed, the majority were between 46 and 55 years old, with 55.7% of participants being female. Most patients were educated, with 55.9% having a bachelor’s degree. The majority of participants in our study had a long-standing disease of more than 10 years (42.5%). Baseline characteristics are depicted in Table 2.
| Overall (n = 709) | |
| Age (yr) | |
| 18-25 | 172 (24.3%) |
| 26-35 | 82 (11.6%) |
| 36-45 | 115 (16.2%) |
| 46-55 | 177 (25.0%) |
| 56-65 | 123 (17.3%) |
| Above 65 | 40 (5.6%) |
| Gender | |
| Male | 314 (44.3%) |
| Female | 395 (55.7%) |
| HbA1C | |
| Less than 7% | 202 (28.5%) |
| From 7%-8% | 226 (31.9%) |
| From 8%-10% | 200 (28.2%) |
| More than 10 | 81 (11.4%) |
| Weight, mean ± SD | 76.72 ± 19.5 |
| Pre-existing conditions | |
| Heart disease | 101 (14.24%) |
| Hypertension | 271 (38.22%) |
| Dyslipidemia | 241 (33.99%) |
| Thyroid disease | 82 (11.56%) |
| None | 233 (32.9%) |
| Education level | |
| Below primary school | 36 (5.1%) |
| School (public education) | 225 (31.73%) |
| Bachelor’s degree | 396 (55.9%) |
| Post graduate degree | 52 (7.3%) |
| Living status | |
| City | 594 (83.8%) |
| Village | 115 (16.2%) |
| Monthly household income | |
| < 4500 SAR | 46 (6.5%) |
| 4500-5999 SAR | 186 (26.23%) |
| 6000-9000 SAR | 67 (9.44%) |
| > 9000 SAR | 145 (20.45%) |
| Not disclosed | 265 (37.37%) |
| Diabetes duration (yr) | |
| < 1 | 89 (12.6%) |
| 1-5 | 185 (26.1%) |
| 6-10 | 134 (18.9%) |
| > 10 | 301 (42.5%) |
| Health care sector | |
| Government | 547 (77.2%) |
| Private | 162 (22.8%) |
| Preference for diabetes care | |
| Primary care centers | 256 (36.1%) |
| Diabetes care centers | 296 (41.7%) |
| None | 157 (22.1%) |
| Frequency of diabetes provider visits | |
| Monthly | 263 (37.1%) |
| Quarterly | 230 (32.4%) |
| Annually | 207 (29.2%) |
| None | 9 (1.3%) |
| Diabetes regimen | |
| Oral mediations | 246 (34.7%) |
| Insulin | 299 (42.17%) |
| Insulin and oral medications | 91 (12.8%) |
| No medications | 73 (10.29%) |
| Number of total daily medications | |
| 0-2 medications | 333 (47%) |
| 3-4 medications | 235 (33.1%) |
| 5-9 medications | 129 (18.2%) |
| 10 medications | 12 (1.7%) |
| Previous hospitalization due to diabetes complication | |
| Heart attack | 20 (2.82%) |
| Diabetic foot | 27 (3.8%) |
| Pneumonia | 74 (10.43%) |
| Numbness in the limbs | 288 (40.62%) |
| Kidney disease | 26 (3.66%) |
| Stroke | 24 (3.38%) |
| Diabetes related vision problems | 116 (16.36%) |
| Hepatitis | 10 (1.41%) |
| Shingles | 7 (0.98%) |
| Erectile dysfunction | 20 (2.82%) |
| Previous depression diagnosis | 138 (19.46%) |
Figure 1 illustrates the varied vaccination rates among the study participants. It is notable that a small minority, 10.01% (n = 71), have never been administered any form of vaccine. Conversely, a substantial majority, 85.89% (n = 609), have received at least one dose of the COVID-19 vaccine. Additionally, 34.83% (n = 247) of participants had been administered the annual influenza vaccine. However, the reception for other vaccines was notably lower, with only 2.96% (n = 21) having received the herpes zoster vaccine, 2.11% (n = 15) the Tdap vaccine, and a mere 1.12% (n = 8) being administered the HPV vaccine.
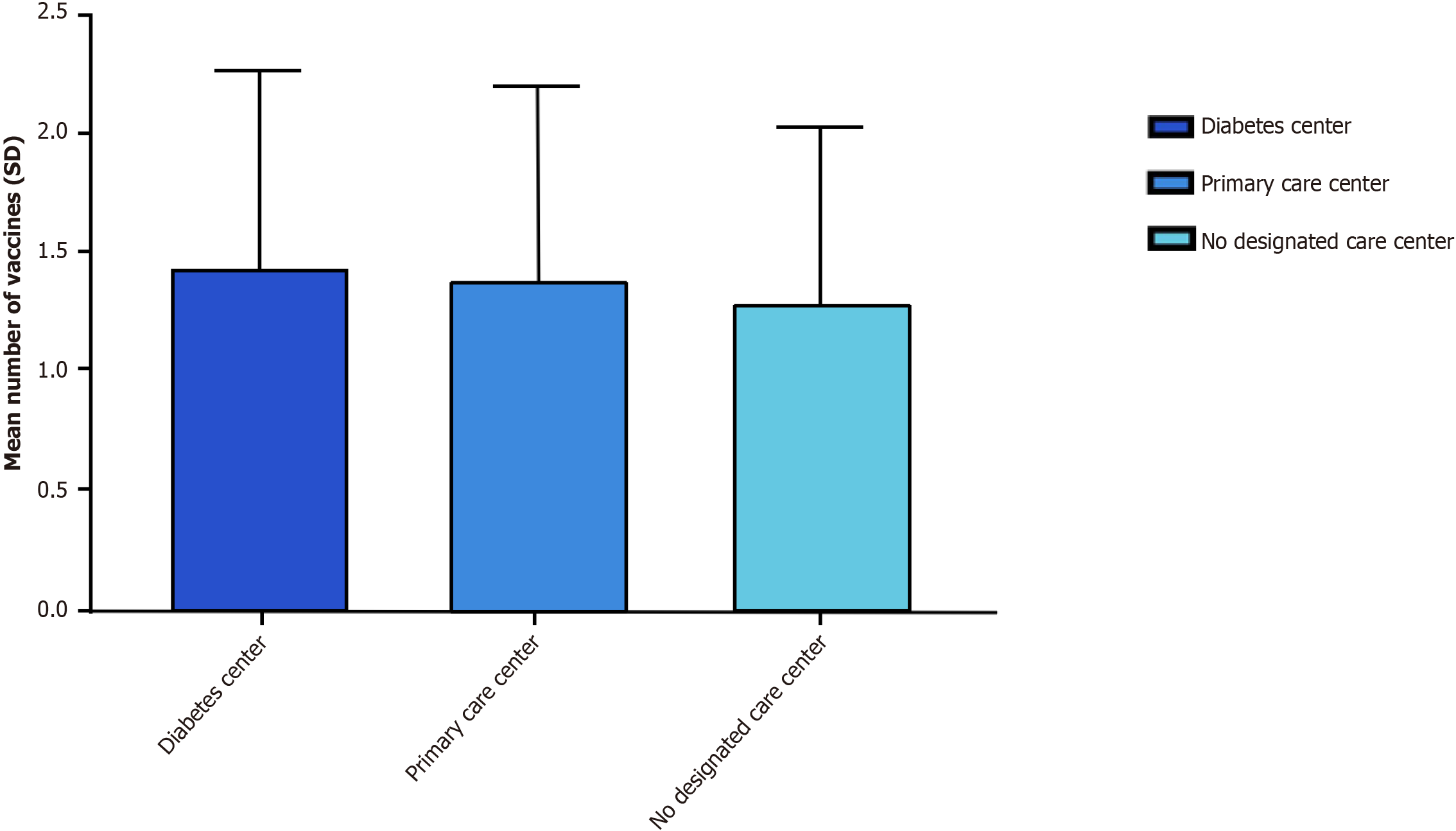
A one-way ANOVA was conducted to determine if there is a relationship between the site of care and the frequency of vaccines received by patients. Patients were classified into three groups according to their care site: Primary care center, provided by the Ministry of Health to offer primary health care to the region it serves, applying a comprehensive care strategy for family medicine (n = 256), diabetes center (n = 296), and no designated center of care (n = 157). One-way ANOVA indicated the presence of a statistically significant difference between sites of care. Post-hoc Tukey HSD test revealed that when compared to the patients who receive care from the diabetes center, the patients who have no designated center for DM care had a significantly lower mean frequency of vaccines received (mean different = 0.23, P = 0.015). In addition, no significant difference was found between the other groups (Figure 2).
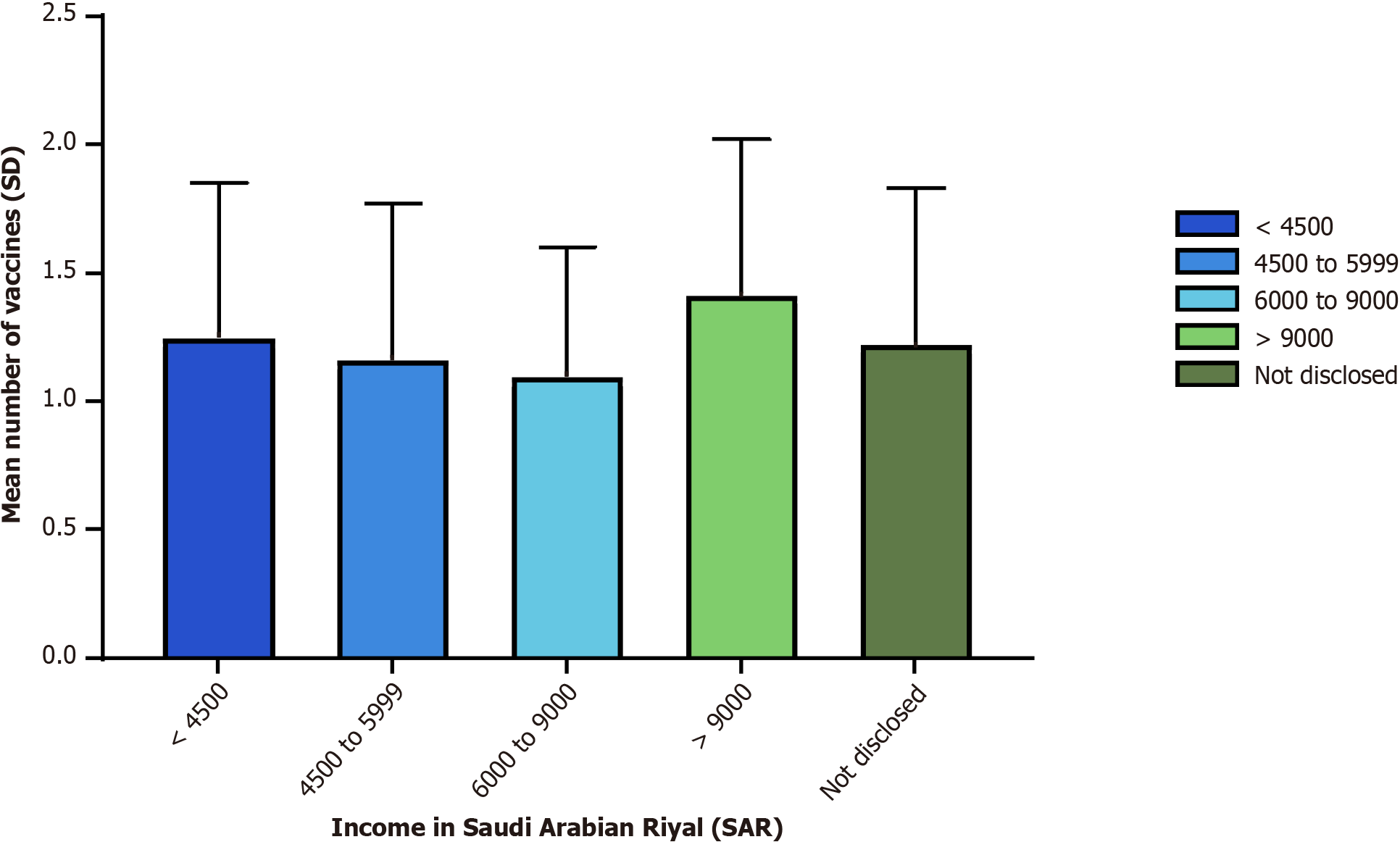
A one-way ANOVA was conducted to determine if there is a relationship between the frequency of vaccines received and different income levels. Patients were classified into five groups according to their income level: Not disclosed (n = 265), > 9000 Saudi Arabian Riyal (SAR) (n = 145), 6000-9000 SAR (n = 67), 4500-5999 SAR (n = 186), < 4500 SAR (n = 46). One-way ANOVA indicated the presence of a statistically significant difference between the income groups. Post-hoc Tukey HSD test revealed that, when compared to the > 9000 SAR income group, the 4500-5999 SAR and the 6000-9000 SAR income groups had a significantly lower mean frequency of vaccines received (mean different = 0.25, P = 0.042, and mean different = 0.38, P = 0.014) respectively. In addition, no significant difference was found between the other groups (Figure 3).
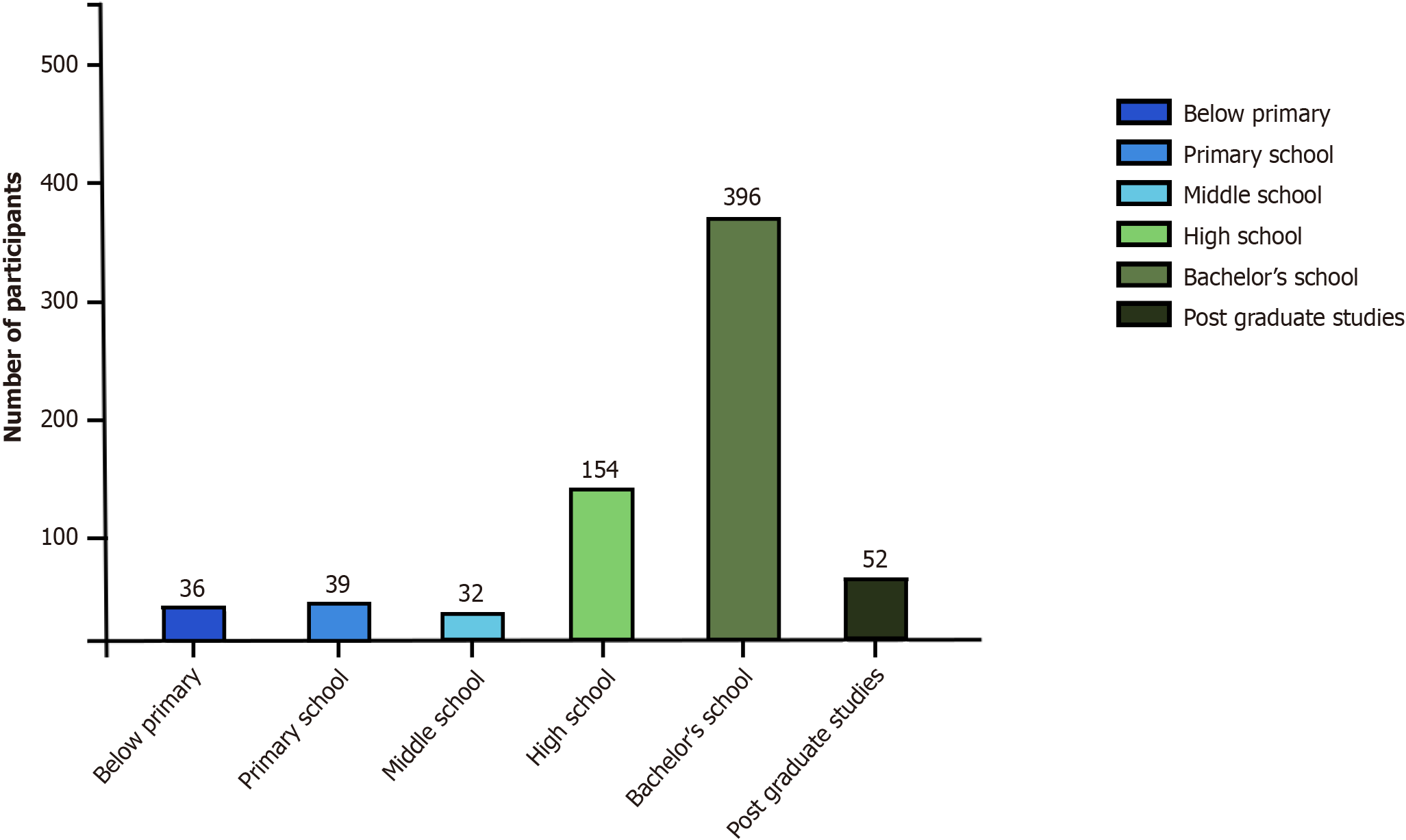
A one-way ANOVA was conducted to determine if there is a relationship between the frequency of vaccines received and the educational level of the patients. Patients were classified into four groups according to their education level: Less than primary school (n = 36), school (n = 225), graduate (n = 396), and postgraduate (n = 52). One-way ANOVA indicated a non-significant difference between the different education groups with a P-value of 0.233 (Figure 4).
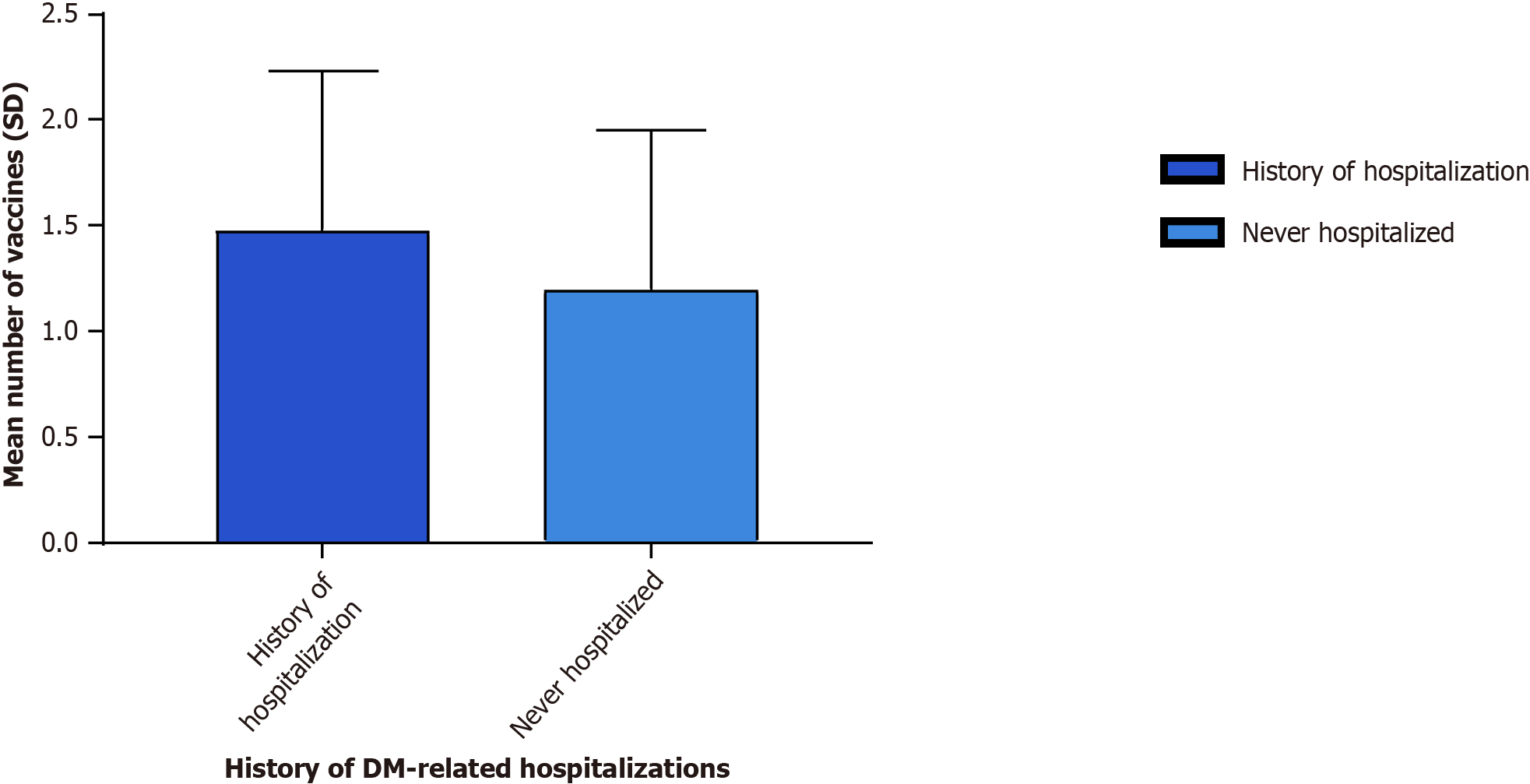
An independent t-test was performed to compare the frequency of vaccines received by diabetic patients with a history of hospitalization to those without. As seen in Figure 5, the analysis concluded that the group with a hospitalization history (mean = 1.42, SD = 0.83) received a significantly higher frequency of vaccinations [t(707) = 3.10, P = 0.002] compared to the non-hospitalized group (mean = 1.20, SD = 0.78).
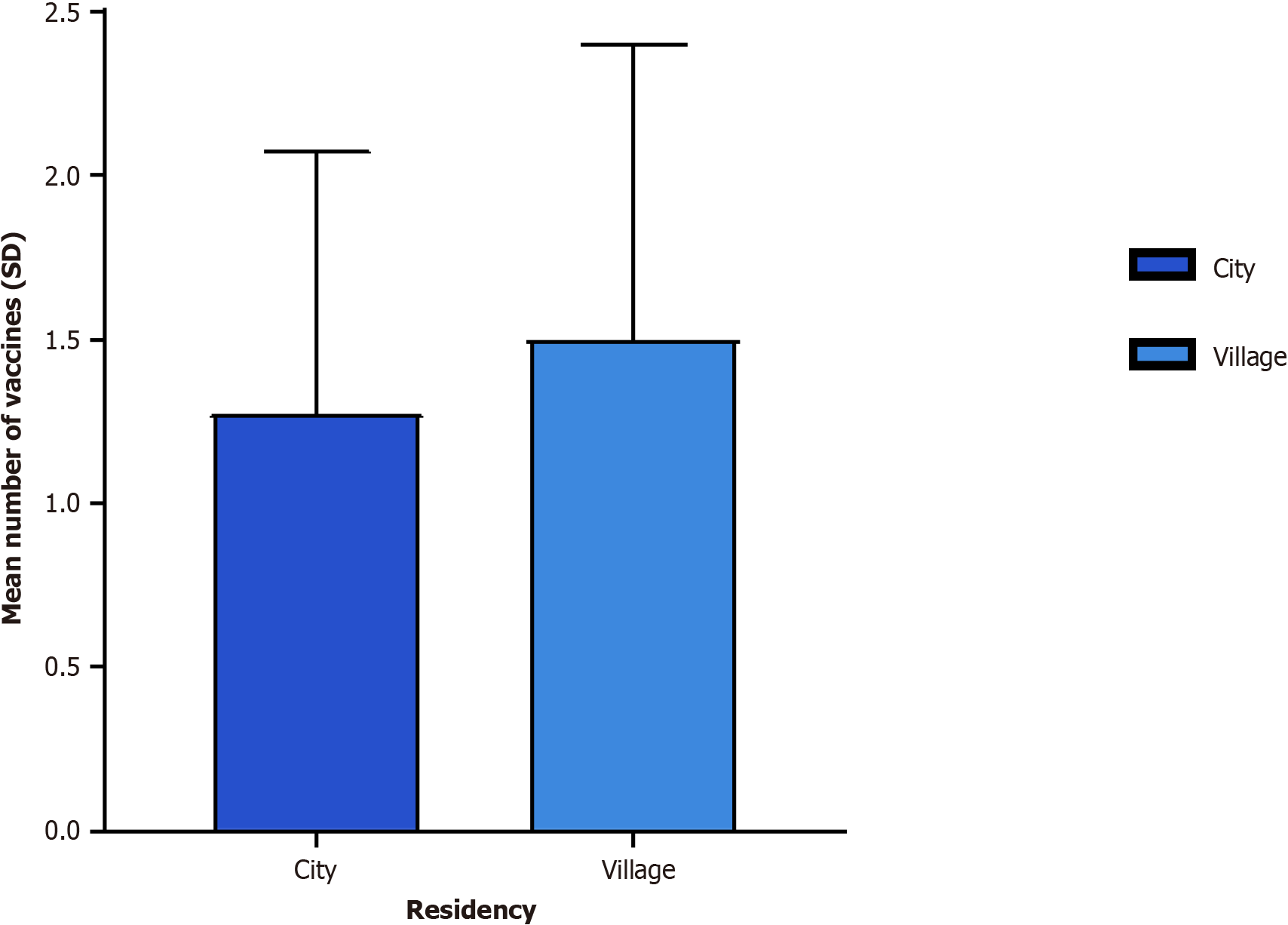
We performed an independent t-test to compare the frequency of vaccines received between city residents and village residents. The test concluded that village residents (mean = 1.53, SD = 0.93) had received a significantly higher frequency of vaccinations [t(707) = 2.33, P = 0.02] than city residents (mean = 1.33, SD = 0.79) (Figure 6).
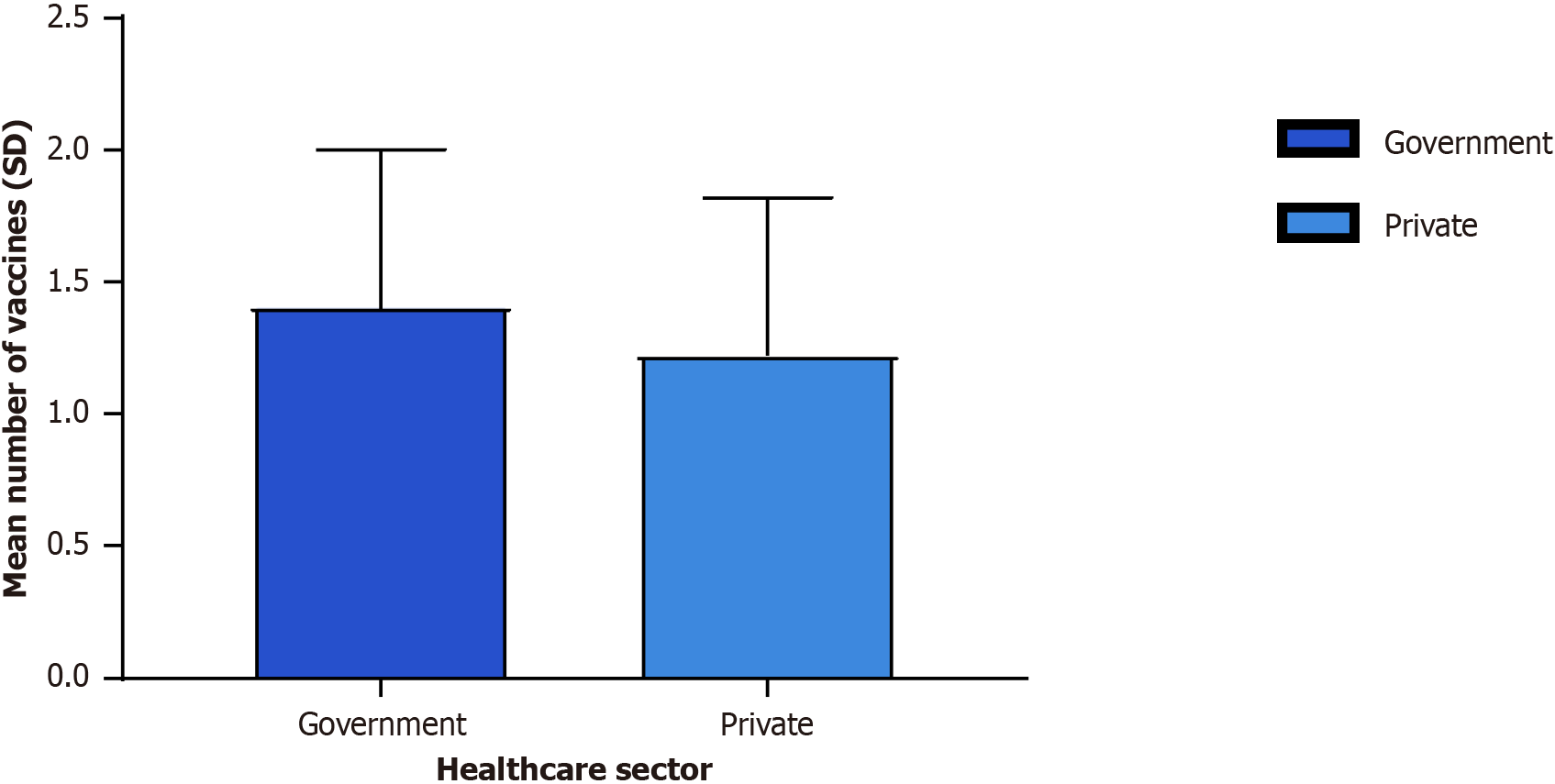
We performed an independent t-test to compare the frequency of vaccines received between the patients receiving care from government hospitals and the patients receiving care from private hospitals (Figure 7). The results concluded that patients in government sectors (mean = 1.40, SD = 0.82) had significantly higher adherence to vaccinations [t(707) = 2.22, P = 0.02] than patients in private sectors (mean = 1.24, SD = 0.80).
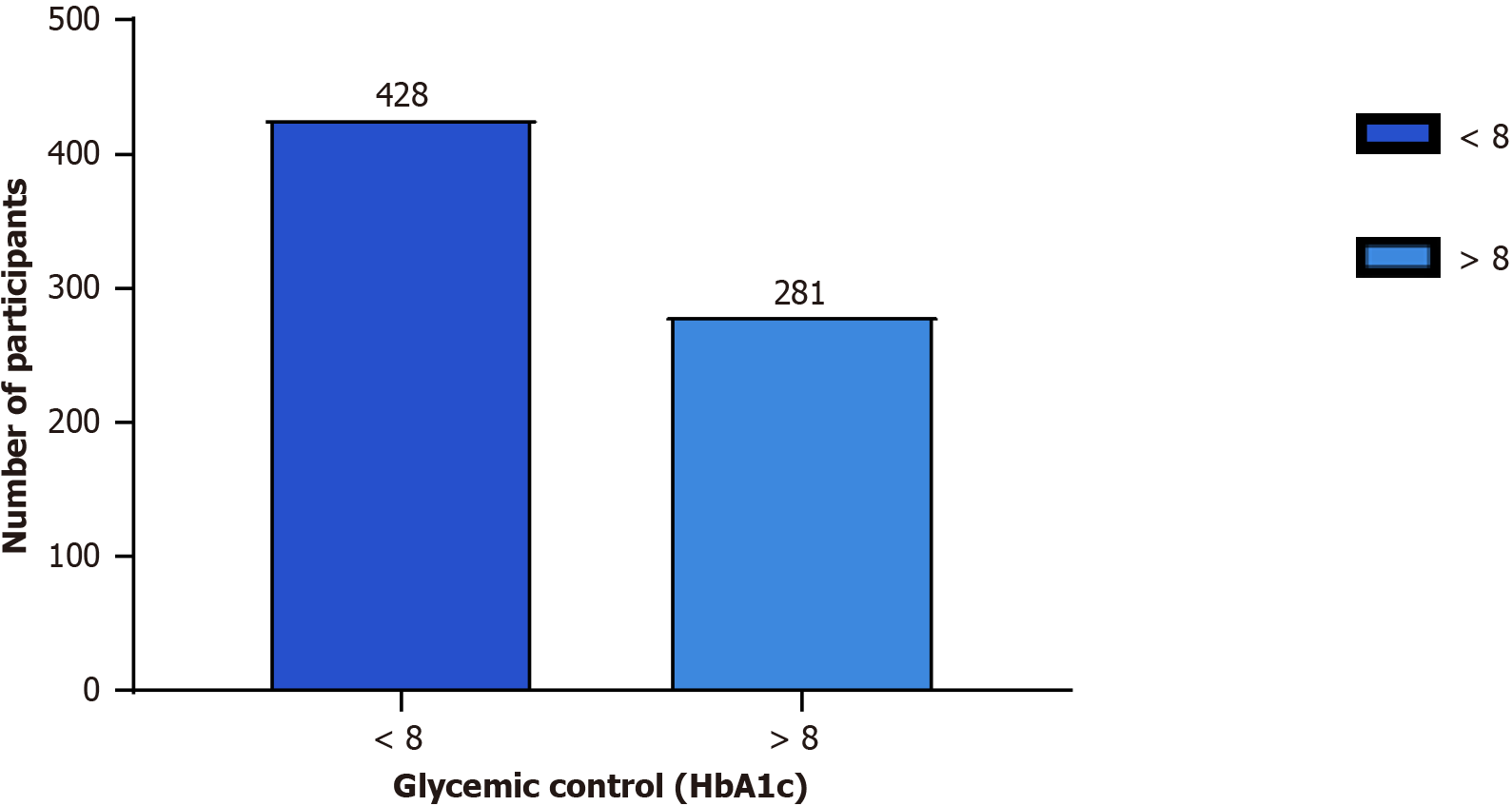
We performed an independent t-test to compare the frequency of vaccines received between those with HbA1c < 8% and those with HbA1c > 8% (Figure 8). The results concluded that patients with HbA1c > 8% (mean = 1.41, SD = 0.86) had received a significantly higher frequency of vaccinations [t(707) = 2.14, P = 0.03] than patients with HbA1c < 8% (mean = 1.26, SD = 0.71).
Our survey has shown that 71 out of 709 participants did not receive any vaccine. Table 3 demonstrates the most commonly reported barriers to receiving vaccination by patients with DM. The most prevalent reasons were lack of knowledge about the vaccines’ importance and fear of side effects, reported by 29.57% (n = 21) and 28.16% (n = 20), respectively. On the other hand, lack of vaccines was the least commonly disclosed barrier, reported by only 2.81% (n = 2).
| Barrier | Participants, n (%) |
| I do not know the importance of these vaccines for diabetes | 21 (29.57) |
| Fear of side effects | 20 (28.16) |
| The vaccines were not suggested by the doctor | 11 (15.49) |
| I think the vaccine is not important | 10 (14.08) |
| Not educated about the importance of vaccines by the doctor | 6 (8.45) |
| Lack of vaccine | 2 (2.81) |
| Reason not disclosed | 4 (5.63) |
The findings from 709 patients with DM in Saudi Arabia showed that 34.83% of participants received the annual influenza vaccine, and 85.89% received at least one dose of the COVID-19 vaccination. However, there is generally a low rate of other vaccinations, including herpes zoster, Tdap, pneumococcal, and HPV vaccines. In Saudi Arabia, MMR and varicella (chickenpox) vaccinations are included in the Saudi national vaccine schedule and are required for enrollment in the public education system[17].
Vaccine recommendations delivered to patients, either from their family physicians or specialists, can have an impact on vaccination acceptance by the patient[18]. In our study, we showed that participants without a designated care center exhibited significantly lower mean frequency of vaccination rates when compared to those who received care from a diabetes center. This finding is consistent with another study that showed higher vaccination coverage among patients reporting frequent physician visits[19]. Interestingly, the vaccination rates when comparing primary health care centers and specialized diabetic centers were not significantly different in our report. This contrasts with another report that considered visits to specialists as an independent factor in pneumococcal vaccination compared to family doctors[20]. Additionally, another study reported that patients with DM expressed more trust and willingness to take vaccines when advised by their diabetologist compared to family physicians, at rates of 80.9% and 50.9%, respectively[21].
The impact of socioeconomic status on vaccination rates has been investigated in previous studies. Research conducted in the United States, Thailand, and South Korea has shown that socioeconomic factors are related to unvaccinated status, especially among vulnerable groups such as young adults, individuals without insurance, low-income families, and those lacking access to medical care[22-24]. Our findings align with these studies, highlighting a significantly positive correlation between income levels and vaccination status. In our study, higher income emerged as an important factor associated with the likelihood of being vaccinated.
Regarding education level, findings from previous studies have been conflicting, particularly in relation to the association between education level and vaccination status. A study conducted in South Korea reported that individuals with higher education levels had lower vaccination rates[23]. In our study, we observed a non-statistically significant difference in vaccination status among individuals with varying educational levels, ranging from those below primary school to postgraduates. On the contrary, multiple previous studies have reported a significant positive correlation between higher educational levels and increased vaccination rates. For instance, a study conducted in Turkey aimed at determining vaccine awareness among patients with DM found a significant positive correlation between influenza vaccine acceptance and education level, suggesting that a higher education level increases the likelihood of accepting the vaccine[25]. Similarly, a study in Turkey also determined that receiving pneumococcal and influenza vaccinations is associated with higher education levels in patients with DM[26]. Additionally, previous studies in Austria, the United States, and Poland reported that individuals with high educational levels show an increase in vaccination coverage[24,27,28]. However, other studies conducted in Italy, China, and Spain reported that low vaccination rates were correlated with high educational levels[24,29,30].
In our current analysis, one of our interests was to investigate whether a previous history of hospitalization could affect the decision of DM patients to receive the CDC/ACIP-recommended vaccines. Our data indicated a significantly higher uptake of vaccines among patients with DM who have a history of hospitalization compared to those who have never been hospitalized due to DM complications. The results presented in a study by Lohan et al[31] provide a possible explanation for this finding. The study found an increase in vaccine coverage for influenza, Tdap, and pneumococcal vaccines in patients with DM after being admitted to an endocrinology department. Adherence to vaccines was especially noted in the department units that had an inpatient clinical pharmacist involved. This could be attributed to the fact that clinical pharmacists are more attentive to the patient’s medication report and possess skills in educating patients about the importance of vaccinations, thereby facilitating higher vaccine compliance[31]. This privilege of direct access to physicians, clinical pharmacists, and nurses who can provide information about the vaccines and address the patient’s concerns may explain the increased rate of vaccination in patients with a history of DM-related hospitalizations. Additionally, our study’s findings align with the results of the study of Hung et al[32], which demonstrated an increase in influenza vaccine uptake in patients with DM who reported being hospitalized during the preceding year.
One might assume that patients residing in urban areas, such as cities, would be more likely to get vaccinated for several reasons, including high accessibility to healthcare services, the abundance of vaccine promotion campaigns, increased awareness about infection risks, and the perceived effectiveness of vaccines. However, studies examining the relationship between residency (urban vs rural areas) and vaccine adherence have reported inconsistent findings. A cross-sectional study conducted in China investigated the rate of COVID-19 vaccination among hospitalized patients with DM and found that individuals living in rural areas were significantly less likely to be vaccinated with the COVID-19 vaccine[33]. Another study, which included two million patients with chronic diseases, including DM, documented that patients living in rural areas had significantly higher pneumococcal vaccination rates but lower influenza vaccination rates[34]. Conversely, our results showed a significantly higher adherence rate to vaccinations among village residents compared toxicity residents. This could be explained by the Ministry of Health’s efforts in rural areas and the periodic vaccination campaigns sent to villages. Additionally, the close connection among people living in village communities could facilitate the spread of vaccination awareness among them. Our results align with findings from a study that evaluated the uptake rate of the pneumococcal vaccine in the United Kingdom among two million at-risk patients, showing higher vaccination rates in patients living in rural areas[35]. An additional large-scale study in China found a higher hesitancy rate for COVID-19 vaccination in residents of rural areas[36].
The impact of governmental and private healthcare sectors on vaccine coverage among patients with DM is an interesting area to investigate due to the lack of research in this domain. Our results revealed that patients with DM who were followed up in governmental centers received more vaccines compared to those seeking healthcare in private centers. This difference might be explained by financial reasons, as vaccines are provided for free in governmental centers, whereas the cost of vaccines is either covered by patients’ own funds or through insurance claims in private centers.
Poor glycemic control increases the likelihood of infection-related morbidity and mortality in patients with DM; thus, vaccination is critical for this population. In our study, patients with poor glycemic control unexpectedly had higher vaccination rates compared to patients with better glycemic control. This could be because healthcare providers may prioritize vaccination for patients with poor glycemic control. Conversely, another study conducted in South Korea revealed that better glycemic control, evidenced by lower HbA1c levels, was associated with higher vaccine coverage. This was rationalized as poor glycemic control correlating with less adherence to medical advice and, therefore, lower vaccine coverage[23].
The adherence of patients diagnosed with DM to the recommended vaccinations is influenced by their attitudes and perceptions, which are shaped by personal beliefs and guidance from healthcare providers. In our analysis, we identified knowledge insufficiency and concerns regarding the potential side effects of vaccinations as the most prevalent barriers among non-vaccinated patients with DM. This observation aligns with findings from a study conducted in Spain, where fear of adverse events was reported as the most prevalent cause of non-adherence to the influenza vaccine among females with DM[37]. Additional reported barriers include misconceptions about the vaccines’ efficacy in preventing infectious diseases and their complications, needle aversion, concerns about vaccination costs, and issues related to vaccine availability[38,39]. In our current study, only 2.81% of the participants justified missing their vaccine due to the shortage of vaccine supply at the centers.
The crucial role of healthcare providers, including physicians, nurses, and pharmacists, in shaping the vaccination attitudes and perceptions of patients with DM is notable. This was evident in the study by Lewis-Parmar and McCann[40], which highlighted a pronounced fourteen-fold increase in the vaccination uptake rate among patients with DM following the delivery of vaccination recommendations by a healthcare provider[40]. Barriers hindering the effectiveness of healthcare providers’ role in motivating the adherence of patients with DM to recommended vaccinations include inadequate knowledge about these vaccines and limited participation by diabetologists and endocrinologists in guiding patient attitudes toward vaccines[41].
This calls for several key recommendations, including the utilization of various communication mediums such as social media and awareness campaigns to effectively correct any misconceptions. Furthermore, integrating a reminder system into electronic medical records can aid healthcare providers in educating and encouraging patients with DM to take their recommended vaccinations. Additionally, implementing the Standing Order Protocol, which allows non-physician medical providers to assess the patient’s eligibility for vaccines and administer them without a physician’s order, can be an effective strategy.
In Saudi Arabia, patients with DM showed higher vaccination rates for annual influenza and COVID-19 vaccines compared to other vaccinations such as herpes zoster, Tdap, pneumococcal, and HPV. Factors such as vaccine reco
Diabetes constitutes a major risk factor for all types of infection due to deficiency in immune system. Those infections are not only frequent, but also have more risk of progression into severe presentation and poorer response to treatment. Enhancing immunity through vaccinations helps protect against potentially severe complications of such infections. The Centers for Disease Control and Prevention/Advisory Committee on Immunization Practices (CDC/ACIP) issued immunization recommendations to protect this patient population.
Data on adherence to immunization recommendations in patients with diabetes mellitus (DM) in Saudi Arabia is scarce. Shedding some light on immunization practices in this patient group should aid healthcare providers and decision-makers in optimizing DM preventative care in Saudi Arabia.
This retrospective multicenter study objectives include assessing the adherence of patients with DM to the CDC/ACIP immunization recommendations in Saudi Arabia and identifying the factors associated with the vaccine adherence rate.
This is a retrospective study conducted in two phases to collect data regarding immunization rate of diabetic patients in Saudi Arabia. Data from 1000 eligible patient were gathered in phase I through chart review from 13 diabetes care centers. In phase II of the study, 709 out of the 1000 patients were enrolled through answering an online survey.
After data analysis, 10.01% (n = 71) of participants had never received any vaccine. The number of vaccinated diabetic patient with coronavirus disease 2019 (COVID-19) vaccine was 85.89% (n = 609), and annual influenza, 34.83% (n = 247), which is higher compared to other vaccinations. Multiple factors were significantly related to the rate of vaccinations among patients with diabetes including site of care, income level, DM-related hospitalization history, residency site, hemoglobin A1c (HbA1c) level, and health sector type. Lacking enough knowledge regarding the importance of immunizations and concerns regarding vaccine side effects were major barriers for receiving vaccines. This highlights the importance of conducting larger studies to explore other risk factors that may encourage adherence to CDC/ACIP vaccine recommendations.
Although patients with diabetes are more prone to developing all types of infections, their overall vaccination rate is still suboptimal. Adults with diabetes in Saudi Arabia have higher rate of COVID-19 and annual influenza vaccines compared to other vaccines recommended by CDC/ACIP. Among patients with diabetes, factors significantly influence the decision of vaccination include recommendations provided by family physicians or specialists, the site of care, income level, DM-related hospitalization history, residency site, HbA1c level, and health sector where care is being provided.
This signifies the need for large-scale research to identify additional factors that might facilitate adherence to CDC/ACIP vaccine recommendations in patients with DM.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Endocrinology and metabolism
Country/Territory of origin: Saudi Arabia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Odhar HA, Iraq; Yan LJ, United States S-Editor: Wang JJ L-Editor: A P-Editor: Zhao YQ
| 1. | Banday MZ, Sameer AS, Nissar S. Pathophysiology of diabetes: An overview. Avicenna J Med. 2020;10:174-188. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 266] [Article Influence: 53.2] [Reference Citation Analysis (1)] |
| 2. | Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB, Stein C, Basit A, Chan JCN, Mbanya JC, Pavkov ME, Ramachandaran A, Wild SH, James S, Herman WH, Zhang P, Bommer C, Kuo S, Boyko EJ, Magliano DJ. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. 2022;183:109119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3033] [Cited by in RCA: 4762] [Article Influence: 1587.3] [Reference Citation Analysis (36)] |
| 3. | Robert AA, Al Awad AD, Al Dawish MA. Current Status of Knowledge and Awareness of Diabetes Mellitus in Saudi Arabia. Curr Diabetes Rev. 2021;17:e101220186818. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 4. | GBD 2021 Diabetes Collaborators. Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: a systematic analysis for the Global Burden of Disease Study 2021. Lancet. 2023;402:203-234. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1683] [Cited by in RCA: 1744] [Article Influence: 872.0] [Reference Citation Analysis (18)] |
| 6. | World Health Organization. Global vaccine action plan 2011-2020. [cited 15 August 2023]. Available from: https://www.who.int/publications/i/item/global-vaccine-action-plan-2011-2020. |
| 7. | Doherty M, Schmidt-Ott R, Santos JI, Stanberry LR, Hofstetter AM, Rosenthal SL, Cunningham AL. Vaccination of special populations: Protecting the vulnerable. Vaccine. 2016;34:6681-6690. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 135] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 8. | Kesavadev J, Misra A, Das AK, Saboo B, Basu D, Thomas N, Joshi SR, Unnikrishnan AG, Shankar A, Krishnan G, Unnikrishnan R, Mohan V. Suggested use of vaccines in diabetes. Indian J Endocrinol Metab. 2012;16:886-893. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 24] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | Akbar DH. Bacterial pneumonia: comparison between diabetics and non-diabetics. Acta Diabetol. 2001;38:77-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 43] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 10. | Dicembrini I, Silverii GA, Clerico A, Fornengo R, Gabutti G, Sordi V, Tafuri S, Peruzzi O, Mannucci E. Influenza: Diabetes as a risk factor for severe related-outcomes and the effectiveness of vaccination in diabetic population. A meta-analysis of observational studies. Nutr Metab Cardiovasc Dis. 2023;33:1099-1110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 19] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 11. | Kuo CS, Lu CW, Chang YK, Yang KC, Hung SH, Yang MC, Chang HH, Huang CT, Hsu CC, Huang KC. Effectiveness of 23-valent pneumococcal polysaccharide vaccine on diabetic elderly. Medicine (Baltimore). 2016;95:e4064. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 12. | Centers for Disease Control and Prevention. What Vaccines are Recommended for You. [cited 15 August 2023]. Available from: https://www.cdc.gov/vaccines/adults/rec-vac/index.html. |
| 13. | Alcusky MJ, Pawasauskas J. Adherence to Guidelines for Hepatitis B, Pneumococcal, and Influenza Vaccination in Patients With Diabetes. Clin Diabetes. 2015;33:116-122. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 14. | Bianchi FP, Stefanizzi P, Martinelli A, Brescia N, Tafuri S. COVID-19 vaccination hesitancy in people affected by diabetes and strategies to increase vaccine compliance: A systematic narrative review and meta-analysis. Vaccine. 2023;41:1303-1309. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 14] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 15. | Alsufyani SA. Acceptance Rate of Influenza Vaccination Among Patients with Type II Diabetes. J Family Med Prim Care. 2022;11:44-52. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 16. | Alkhateeb S, Bahafzalla R, Bamanie H, Farag N, Alharbi R, Alfares MA. Influenza, Pneumococcal, and Hepatitis B Vaccination coverage and its determinants among diabetic patients at KAUH: A Single Center Cross-Sectional Study. Inter J Med Develop Countries. 2021;. [DOI] [Full Text] |
| 17. | Ministry of Health. National immunization schedule. [cited 20 August 2023]. Available from: https://www.moh.gov.sa/en/HealthAwareness/EducationalContent/HealthTips/Documents/Immunization-Schedule.pdf. |
| 18. | Fisher KA, Nguyen N, Fouayzi H, Singh S, Crawford S, Mazor KM. Impact of a physician recommendation on COVID-19 vaccination intent among vaccine hesitant individuals. Patient Educ Couns. 2023;106:107-112. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 25] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 19. | Williams WW, Lu PJ, O'Halloran A, Kim DK, Grohskopf LA, Pilishvili T, Skoff TH, Nelson NP, Harpaz R, Markowitz LE, Rodriguez-Lainz A, Fiebelkorn AP. Surveillance of Vaccination Coverage among Adult Populations - United States, 2015. MMWR Surveill Summ. 2017;66:1-28. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 297] [Cited by in RCA: 312] [Article Influence: 39.0] [Reference Citation Analysis (0)] |
| 20. | Gilani F, Majumdar SR, Johnson JA, Simpson SH; ABCD Cohort Investigators. Factors associated with pneumococcal vaccination in 2040 people with type 2 diabetes: A cross-sectional study. Diabetes Metab. 2020;46:137-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 21. | Dallagiacoma G, Allora A, Salvati S, Cocciolo G, Capraro M, Lamberti A, Senatore S, Gentile L, Gianfredi V, Laurenzi A, Molinari C, Caretto A, Faccini M, Signorelli C, Scavini M, Odone A. Type 1 Diabetes Patients' Practice, Knowledge and Attitudes towards Influenza Immunization. Vaccines (Basel). 2021;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 22. | Bhugra P, Mszar R, Valero-Elizondo J, Grandhi GR, Virani SS, Cainzos-Achirica M, Vahidy FS, Omer S, Nasir K. Prevalence of and Sociodemographic Disparities in Influenza Vaccination Among Adults With Diabetes in the United States. J Endocr Soc. 2020;4:bvaa139. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 23. | Lee DH, Yang B, Gu S, Kim EG, Kim Y, Kang HK, Choe YH, Jeon HJ, Park S, Lee H. Influenza vaccination trend and related factors among patients with diabetes in Korea: Analysis using a nationwide database. Front Endocrinol (Lausanne). 2023;14:1077846. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 24. | Ko YM, Ko SH, Han K, Park YM, Choi JY, Kim SY, Song SH, Kim CH, Kim SK. Importance of Awareness and Treatment for Diabetes in Influenza Vaccination Coverage of Diabetic Patients under 65 Years: A Population-Based Study. Diabetes Metab J. 2021;45:55-66. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 25. | Karagun B, Evran M, Odabas F, Akkus G, Kurtaran B, Sert M, Tetiker T. Awareness of Vaccination against Respiratory Tract Diseases, Including Pneumonia, Influenza, and COVID-19 in Patients with Diabetes Mellitus. Int J Clin Pract. 2022;2022:1389137. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 26. | Demirci I, Haymana C, Salman S, Tasci I, Corapcioglu D, Kirik A, Yetkin İ, Altay M, Sabuncu T, Bayram F, Satman I, Sonmez A; TEMD Study Group. Rates and associates of influenza and pneumococcus vaccination in diabetes mellitus: A nationwide cross-sectional study (TEMD vaccination study). World J Diabetes. 2021;12:2107-2118. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 27. | Takayama M, Wetmore CM, Mokdad AH. Characteristics associated with the uptake of influenza vaccination among adults in the United States. Prev Med. 2012;54:358-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 95] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 28. | de Perio MA, Wiegand DM, Evans SM. Low influenza vaccination rates among child care workers in the United States: assessing knowledge, attitudes, and behaviors. J Community Health. 2012;37:272-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 29. | Rodríguez-Rieiro C, Domínguez-Berjón MF, Esteban-Vasallodomínguez-Berjón MD, Cuadrado AR, Carrasco-Garrido P, Jiménez-García R. Coverage and predictors of influenza vaccine uptake among adults aged 16 to 59 years suffering from a chronic condition in Madrid, Spain. Hum Vaccin. 2011;7:557-562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 30. | Wu S, Yang P, Li H, Ma C, Zhang Y, Wang Q. Influenza vaccination coverage rates among adults before and after the 2009 influenza pandemic and the reasons for non-vaccination in Beijing, China: a cross-sectional study. BMC Public Health. 2013;13:636. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 52] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 31. | Lohan L, Cool C, Viault L, Cestac P, Renard E, Galtier F, Villiet M, Avignon A, Sultan A, Breuker C. Impact of Hospitalization in an Endocrinology Department on Vaccination Coverage in People Living with Diabetes: A Real-Life Study. Medicina (Kaunas). 2022;58. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 32. | Hung MC, Lu PJ, Srivastav A, Cheng YJ, Williams WW. Influenza vaccination coverage among adults with diabetes, United States, 2007-08 through 2017-18 seasons. Vaccine. 2020;38:6545-6552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 33. | Duan L, Wang Y, Dong H, Song C, Zheng J, Li J, Li M, Wang J, Yang J, Xu J. The COVID-19 Vaccination Behavior and Correlates in Diabetic Patients: A Health Belief Model Theory-Based Cross-Sectional Study in China, 2021. Vaccines (Basel). 2022;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 34. | Wang Y, Cheng M, Wang S, Wu F, Yan Q, Yang Q, Li Y, Guo X, Fu C, Shi Y, Wagner AL, Boulton ML. Vaccination coverage with the pneumococcal and influenza vaccine among persons with chronic diseases in Shanghai, China, 2017. BMC Public Health. 2020;20:359. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 33] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 35. | Pebody RG, Hippisley-Cox J, Harcourt S, Pringle M, Painter M, Smith G. Uptake of pneumococcal polysaccharide vaccine in at-risk populations in England and Wales 1999-2005. Epidemiol Infect. 2008;136:360-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 53] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 36. | Wu J, Shen Z, Li Q, Tarimo CS, Wang M, Gu J, Wei W, Zhang X, Huang Y, Ma M, Xu D, Ojangba T, Miao Y. How urban versus rural residency relates to COVID-19 vaccine hesitancy: A large-scale national Chinese study. Soc Sci Med. 2023;320:115695. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 19] [Reference Citation Analysis (0)] |
| 37. | Jiménez-Garcia R, Lopez-de-Andres A, Hernandez-Barrera V, Gómez-Campelo P, San Andrés-Rebollo FJ, de Burgos-Lunar C, Cárdenas-Valladolid J, Abánades-Herranz JC, Salinero-Fort MA. Influenza vaccination in people with type 2 diabetes, coverage, predictors of uptake, and perceptions. Result of the MADIABETES cohort a 7years follow up study. Vaccine. 2017;35:101-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 40] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 38. | Tan EK, Lim LH, Teoh YL, Ong G, Bock HL. Influenza and seasonal influenza vaccination among diabetics in Singapore: knowledge, attitudes and practices. Singapore Med J. 2010;51:623-630. [PubMed] |
| 39. | Olatunbosun OD, Esterhuizen TM, Wiysonge CS. A cross sectional survey to evaluate knowledge, attitudes and practices regarding seasonal influenza and influenza vaccination among diabetics in Pretoria, South Africa. Vaccine. 2017;35:6375-6386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 40. | Lewis-Parmar H, McCann R. Achieving national influenza vaccine targets--an investigation of the factors affecting influenza vaccine uptake in older people and people with diabetes. Commun Dis Public Health. 2002;5:119-126. [PubMed] |