Published online Feb 15, 2024. doi: 10.4239/wjd.v15.i2.186
Peer-review started: June 1, 2023
First decision: July 3, 2023
Revised: August 5, 2023
Accepted: December 27, 2023
Article in press: December 27, 2023
Published online: February 15, 2024
Processing time: 247 Days and 23.7 Hours
Diabetic kidney disease (DKD) is a prevalent complication of diabetes that often requires hemodialysis for treatment. In the field of nursing, there is a growing recognition of the importance of humanistic care, which focuses on the holistic needs of patients, including their emotional, psychological, and social well-being. However, the application of humanistic nursing in the context of hemodialysis for DKD patients remains relatively unexplored.
To explore the experience of humanistic nursing in hemodialysis nursing for DKD patients.
Ninety-six DKD patients treated with hemodialysis from March 2020 to June 2022 were included in the study and divided into the control cluster (48 cases) and the study cluster (48 cases) according to different nursing methods; the control cluster was given routine nursing and the study cluster was given humanized nursing. The variances of negative emotion mark, blood glucose, renal function, the incidence of complications, life mark and nursing satisfaction before and after nur-sing were contrasted between the two clusters.
No significant difference in negative emotion markers between the two clusters were observed before nursing (P > 0.05), and the negative emotion markers of the two clusters decreased after nursing. The Hamilton Anxiety Rating Scale and Hamilton Depression Rating Scale markers were lower in the study cluster than the control cluster. The healing rate of patients in the study cluster was significantly higher than the control cluster (97.92% vs 85.42%, P < 0.05). Blood glucose parameters were not significantly different between the groups prior to nursing (P > 0.05). However, after nursing, blood urea nitrogen and serum creatinine (SCr) levels in the study cluster were lower than those in the control cluster (P < 0.05). The incidence rate of complications was significantly lower in the study group compared to the control cluster (6.25% vs 20.83%, P < 0.05). There was no significant difference in the life markers between the two clusters before nursing. While the life markers increased after nursing for both groups, the 36-item health scale markers in the study cluster were higher than those within the control cluster (P < 0.05). Finally, the nursing satisfaction rate was 93.75% in the study cluster, compared to 75% in the control cluster (P < 0.05).
In hemodialysis for DKD patients, the implementation of humanistic nursing achieved ideal results, effectively reducing patients’ psychological negative emotion markers so that they can actively cooperate with the diagnosis and nursing, facilitate the control of blood glucose and the maintenance of residual renal function, reduce the occurrence of complications, and finally enhance the life quality and nursing satisfaction of patients. It is worthy of being widely popularized and applied.
Core Tip: The study aimed to explore the experience of humanistic nursing in hemodialysis for patients with diabetic kidney disease (DKD). The results showed that humanistic nursing effectively reduced patients’ negative emotions, improved healing, controlled blood glucose levels, and maintained renal function. It also reduced the incidence of complications and enhanced patients’ life quality and nursing satisfaction. These findings highlight the importance of humanistic nursing in improving the care and well-being of DKD patients undergoing hemodialysis. The implementation of humanistic nursing should be widely promoted and applied in clinical practice.
- Citation: Chai XY, Bao XY, Dai Y, Dai XX, Zhang Y, Yang YL. Experience of humanistic nursing in hemodialysis nursing for patients with diabetic kidney disease. World J Diabetes 2024; 15(2): 186-195
- URL: https://www.wjgnet.com/1948-9358/full/v15/i2/186.htm
- DOI: https://dx.doi.org/10.4239/wjd.v15.i2.186
Diabetic kidney disease (DKD) is a renal disease that occurs as a result of diabetic injury. Its incidence is increasing each year due to the rising prevalence of diabetes[1]. Hemodialysis is the primary treatment for DKD, as it effectively eliminates harmful substances from the bloodstream, thus improving the patients’ quality of life. However, it is important to note that DKD patients undergoing hemodialysis face unique challenges compared to other dialysis patients. Firstly, the underlying cause of their kidney disease is different, stemming from diabetic kidney injury. Secondly, the close association between DKD and the increasing prevalence of diabetes often leads to additional complications and comorbidities. Lastly, DKD patients may encounter specific challenges such as disease and program awareness, adhering to treatment regimens, and a higher likelihood of developing complications during hemodialysis[2]. These distinctions highlight the need for tailored interventions and care approaches for this particular patient population.
Hemodialysis is a treatment method for kidney disease caused by diabetes complications. Over time, uncontrolled diabetes can damage the blood vessels and filters in the kidneys, impairing their function. Hemodialysis involves the use of a machine called a dialyzer to filter the blood, removing waste products and excess fluids that damaged kidneys can no longer effectively eliminate. This treatment helps maintain fluid and electrolyte balance, control blood pressure, and remove accumulated waste products. It is important to note that hemodialysis is not a cure for DKD, but rather a supportive therapy to manage symptoms and maintain overall health. Other treatments, such as medication, lifestyle modifications, and kidney transplantation, may also be considered as part of the DKD management plan.
However, hemodialysis is an invasive procedure that can be time-consuming, which presents specific challenges and requirements. Additionally, many patients lack awareness about their disease and the hemodialysis program, leading to low compliance with diagnosis and care. This can further contribute to complications during hemodialysis and poor patient prognosis[3,4]. In response to these challenges, nursing measures are often employed to enhance patient care. One such approach is humanistic nursing, which has emerged because of evolving nursing models. Humanistic nursing focuses on treating patients holistically, considering their physical, emotional, and psychological needs. By incorporating this approach, healthcare professionals aim to provide individualized and compassionate care, fostering a positive patient experience during hemodialysis. To investigate the application of humanistic nursing in hemodialysis nursing for DKD patients, this paper aims to share our experiences and findings.
Ninety-six DKD patients who received hemodialysis from March 2020 to June 2022 were included in the study and divided into the control cluster (48 cases) and the study cluster (48 cases) according to different nursing methods. Among them, there were 25 males and 23 females within the control cluster, aged 38-77 years, with an average of (56.43 ± 6.84) years. In the study cluster, there were 26 males and 22 females, aged 39-78 years, with an average of (57.05 ± 7.11) years. Inclusion criteria were as follows: (1) DKD; (2) Receiving hemodialysis for the first time; and (3) Informed consent. Exclusion criteria were as follows: (1) Mental, consciousness and communication disorders; (2) Incomplete follow-up data; (3) Renal parenchymal injury caused by other causes; and (4) Combined with other serious diabetic complications such as myocardial infarction, cirrhosis of the liver and kidney failure. To implement random allocation, we used a random number generator or statistical software to randomly assign patients to different groups.
Control cluster: Routine nursing: (1) Inform relevant precautions, closely observe all vital signs of patients, and timely report to the doctor once abnormalities are found; (2) Give specific guidance in diet, life and exercise; (3) Regularly test blood glucose to prevent the occurrence of hypoglycemia; (4) Do an excellent job in daily ward environment nursing; (5) Prevent and symptomatically treat complications, including maintaining skin cleanliness, oral care, puncture site care,
Study clusters: Humanized nursing was implemented on the basis of the control cluster, and all nursing staff were trained before implementation to enhance their own perception of humanized nursing, and patient-centered nursing was always achieved in nursing. The measures included: (1) Health education: Active communication with patients, health education could be conducted in the form of health knowledge lectures, one-on-one education, and WeChat video push, including methods, processes, precautions, and effectiveness, and the advantages of humanized nursing were informed to patients, and similar cases of successful nursing were listed to enhance patient confidence; (2) Psychological counseling: Communication with patients with mild tone, understanding their genuine emotions, and guiding patients to actively name their concerns, and targeted counseling was given for negative emotional causes, including cognitive therapy, attention transfer method, music relaxation therapy, and emotional catharsis method; (3) Fresh green plants were placed indoors to relax the patient’s mood; (4) Diet and exercise individualized nursing: The patient’s condition, weight and self-metabolism were analyzed, the most appropriate daily food intake and exercise were calculated for the patient, and personalized guidance was made. Diet instructs patients to eat more foods containing calcium, protein-rich and fresh vegetables, low-sugar fruits, etc.; and (5) Obtain social support: Communicate with patients’ families, often stand at the patient’s point of view to understand their behavior and enhance the participation of family members in patient care, and strive to create a harmonious, warm, and relaxed family environment at home.
Negative emotion comparative: The Hamilton Anxiety Rating Scale (HAMA) and Hamilton Depression Rating Scale (HAMD) were used to assess the negative emotion[5]. HAMA is a standardized assessment tool used by healthcare professionals to quantify the severity of anxiety symptoms in individuals. It measures the presence and intensity of various anxiety-related symptoms, such as tension, apprehension, and insomnia. On the other hand, HAMD is a widely used instrument that evaluates the severity of depressive symptoms. It assesses factors like mood, guilt, sleep disturbances, and suicidal tendencies. Both scales provide valuable insights into the level of anxiety and depression experienced by individuals, aiding in diagnosis, treatment planning, and monitoring of progress over time.
Comparative of compliance rate: The compliance of patients is often judged based on the following criteria: (1) Complete compliance: The patient follows the doctor’s advice throughout and actively cooperates with nursing staff; (2) Partial compliance: The patient may not fully cooperate but can complete nursing activities under the guidance of nursing staff; and (3) Non-compliance: The patient completely refuses to cooperate with nursing staff. Patient compliance is determined by observing and evaluating their interaction with the healthcare team and their adherence to treatment and nursing plans. However, it is important to consider individual differences, patient education level, and social support when assessing patient compliance[6].
Comparative blood glucose parameters: A total of 4 mL of peripheral venous blood was drawn from the patients in a fasting state or 2 h after a meal, and the supernatant was collected after centrifugation[7].
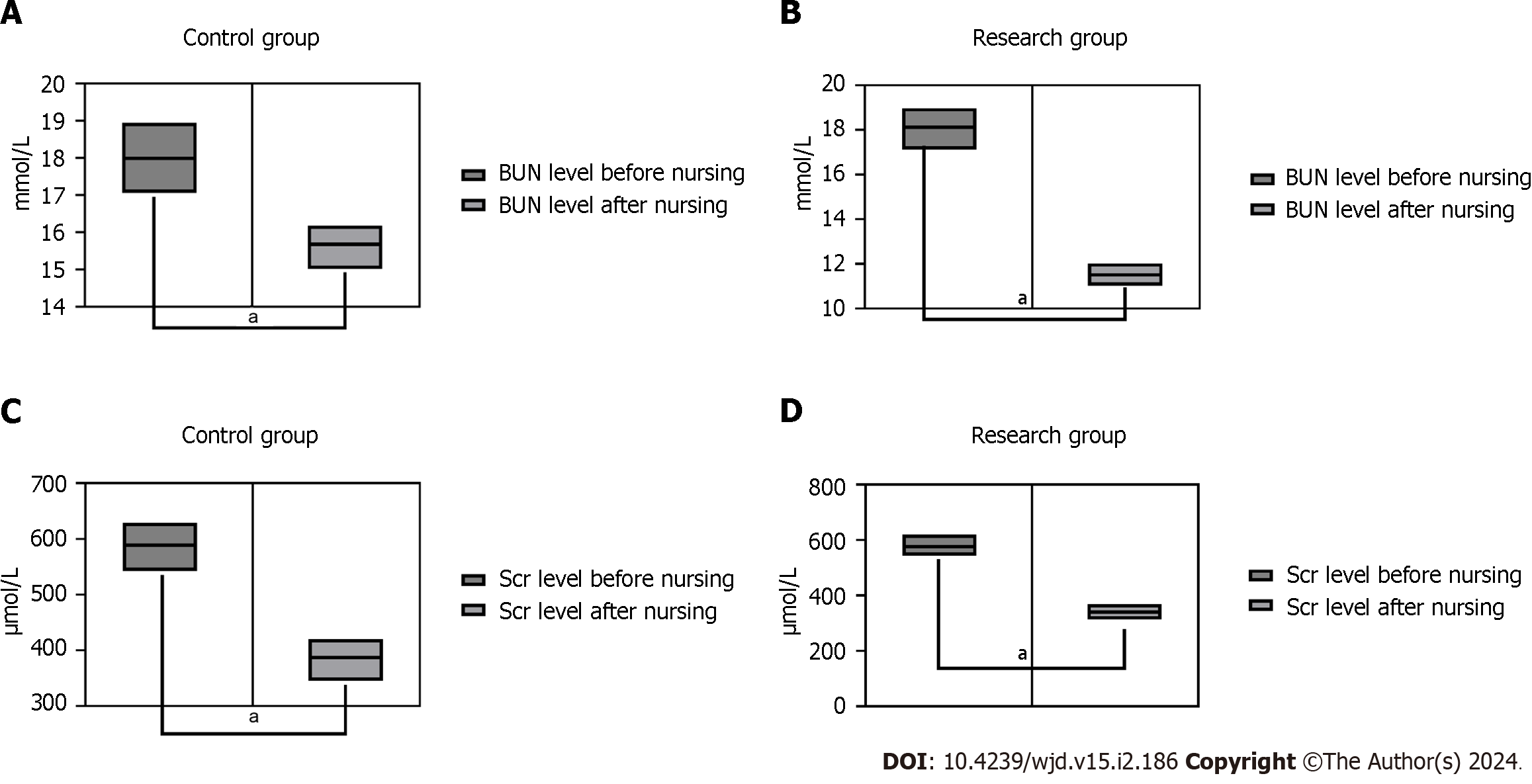
Comparative renal function indexes: A total of 4 mL of peripheral venous blood was drawn from the patients under a fasting state, and the supernatant was collected after centrifugation to detect blood urea nitrogen (BUN) and serum creatinine (SCr) by automatic biochemical analyzer[8].
Comparison of complications: Common complications in hemodialysis include infection, catheter dysfunction, hypoglycemia, hypotension, and heart failure. Intradialytic hypotension (IDH) is common after dialysis. IDH, which can be caused by aggressive ultrafiltration due to weight gain during dialysis, can lead to myocardial stunning and cardiac arrhythmias, which are associated with an increased risk of death[9]. Obviously, kidney failure has a major impact on heart function. Studies have shown that more than half of deaths in patients with end-stage renal disease (ESRD) are due to cardiovascular disease, with arrhythmias and cardiac arrest accounting for 38 percent of deaths[10]. The incidence of ESRD has nearly doubled in the past 20 years. Infection is the second leading cause of death in this patient population, and vascular access-associated infection is the most common identifiable source of infection in hemodialysis patients[11]. The quality of vascular access is the most important factor that determines dialysis treatment efficacy. Vascular lumen stenosis can lead to increased risk of thrombosis, catheter dysfunction and adverse effects on blood flow[12]. Case studies have shown that glucose is transferred from the dialysate into the blood during dialysis and reactive hypoglycemia occurs after the end of dialysis. Persistent hypoglycemia can lead to permanent brain damage[13]. Therefore, monitoring the above complications is of great significance for evaluating the efficacy of dialysis. All complications that occurred during hemodialysis were recorded for both clusters[14].
Quality-of-life comparison: Patient quality-of-life was assessed using the 36-item health scale (SF-36) with a total possible score of 100 points[15].
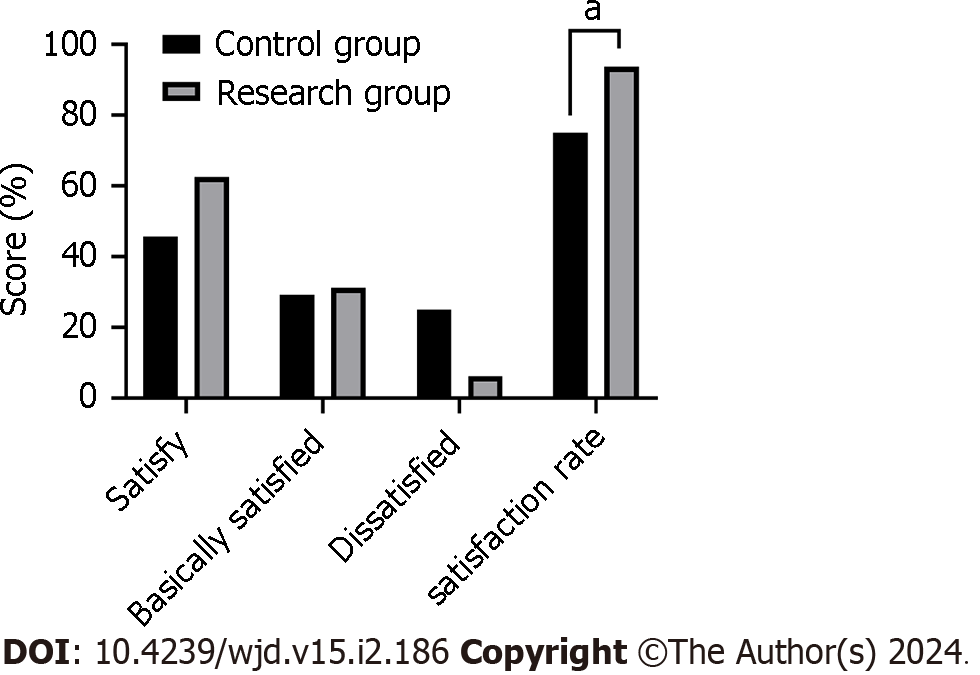
Comparison of nursing satisfaction rate: The self-generated satisfaction questionnaire was used to evaluate satisfaction with the nursing care received, out of a total of 100 points. The score ranges were as follows: Satisfaction: ≥ 80 points, essential satisfaction: 60-79 points, dissatisfaction: < 60 points; satisfaction rate = (satisfaction + essential satisfaction)/total × 100%[16].
Measurement data were expressed as (mean ± SD), and t-tests were used. Enumeration data were expressed as n (%), and a χ2 test was used. P < 0.05 was considered statistically significant and data were analyzed in GraphPad Prism 8 software.
There was no observable variance in negative emotion marks between the two clusters before nursing care (P > 0.05). After nursing, the negative emotion marks of the two clusters decreased, and the HAMA and HAMD marks of the study cluster were lower than those of the control cluster (P < 0.05) (Figure 1).
The compliance rate of patients in the control cluster was 85.42%, whereas it increased to 97.92% in the study cluster (P < 0.05) (Table 1).
| Cluster | Cases | Full compliance | Basic compliance | Non-compliance | Compliance rate |
| Control cluster | 48 | 16 | 25 | 7 | 41 (85.42) |
| Study cluster | 48 | 30 | 17 | 1 | 47 (97.92) |
| χ2 | / | / | / | / | 4.909 |
| P value | / | / | / | / | 0.027 |
There was no significant variance in blood glucose indices between the two clusters before nursing (P > 0.05). After nursing, blood glucose indices decreased in both clusters, and fasting plasma glucose (FPG), 2-hour plasma glucose (2hPG) and hemoglobin A1c (HbA1c) levels in the study cluster were lower than those within the control cluster (P < 0.05) (Figure 2).
There was no significant variance in renal function indices between the two clusters before nursing (P > 0.05). After nursing, the renal function indices decreased for both clusters, and BUN and SCr levels in the study cluster were lower than those within the control cluster (P < 0.05) (Figure 3).
The complication rate of the control cluster was 20.83%, compared to 6.25% in the study (P < 0.05) (Table 2). Complications included infection, catheter dysfunction, hypotension, hypoglycemia, and heart failure.
| Cluster | Cases | Infection | Catheter dysfunction | Hypotension | Hypoglycemia | Heart failure | Occurrence |
| Control cluster | 48 | 2 | 3 | 2 | 2 | 1 | 10 (20.83) |
| Study cluster | 48 | 1 | 1 | 1 | 1 | 0 | 3 (6.25) |
| χ2 | / | / | / | / | / | / | 4.360 |
| P value | / | / | / | / | / | / | 0.037 |
There were no significant differences in the quality-of-life marks between the two clusters before nursing (P > 0.05). The quality-of-life marks increased for both groups after nursing, but the SF-36 marks were higher in the study cluster than the control cluster (P < 0.05) (Table 3). The questionnaire covers eight domains: Physical functioning, role limitations due to physical health, bodily pain, general health perceptions, vitality, social functioning, role limitations due to emotional problems, and mental health.
| Cluster | Time | Social functioning | Physical function | Role function | Affective function | Cognitive function |
| Control cluster | Pre-nursing | 51.67 ± 4.47 | 56.27 ± 3.57 | 50.14 ± 4.27 | 62.11 ± 4.27 | 61.21 ± 4.72 |
| Post-carea | 58.57 ± 4.28 | 62.52 ± 3.74 | 58.16 ± 3.88 | 68.65 ± 5.08 | 69.66 ± 5.17 | |
| Study cluster | Pre-nursing | 51.59 ± 4.07 | 56.31 ± 4.07 | 50.09 ± 4.13 | 62.09 ± 4.31 | 61.26 ± 4.86 |
| Post carea,b | 65.25 ± 5.63 | 67.23 ± 4.24 | 67.15 ± 4.25 | 77.15 ± 5.52 | 78.65 ± 5.06 |
The nursing satisfaction rate was higher in the study cluster compared to the control cluster (93.75% vs 75%; P < 0.05) (Figure 4).
Compared to conventional hemodialysis patients with nephropathy, hemodialysis patients with DKD have a higher risk of discomfort and complications, resulting in a lower degree of nursing cooperation. Therefore, it is very important to strength the care of hemodialysis patients with DKD in the hemodialysis room[17,18]. In routine nursing, attention is focused on healing and attention to the patient’s psychology is neglected. This contributes to passivity and singularity, which leads to the high negative emotions of patients during healing and will hinder healing progress in serious cases. Overall, there is not a positive effect from nursing care; therefore, the exploration of a more effective nursing method is necessary[19].
With the continuous change of nursing model, humanistic nursing appears and is widely used in various fields. Humanistic nursing can be traced back to human nursing at the earliest. It requires nursing staff to have the cognition of human science, to implement humanistic nursing for patients, in order to make the patient’ psychology in a satisfactory and comfortable state to actively cooperate with nursing staff to complete the whole nursing, to achieve the best nursing[20]. With the continuous enhancement of humanistic nursing, its core refers to respecting the patient’s life value, personality dignity, privacy and face in nursing, without making them feel embarrassed and uncomfortable, which will greatly reduce the psychological discomfort caused by physical discomfort, so as to enhance the patient’s negative emotions[21,22]. Humanized nursing attaches importance to the psychological needs of patients, through effective communication to obtain the real ideas of patients’ thoughts, and through scientific and appropriate methods to guide them, in order to help patients establish the best rehabilitation state. Relevant studies have found that meeting the psychological needs of patients can enhance their own defense against stress response, facilitate the reconstruction of psychological balance, and is important for the enhancement of healing and body immunity[23].
Reasonable control of blood glucose is of great meaning for the enhancement of renal function in patients with DKD, and the purpose of nursing implementation is to help patients achieve the expected healing goals, so the detection of blood glucose and renal function indicators in patients can reflect the effect of nursing implementation to a certain extent. Among them, HbA1c has been officially included in the diagnostic criteria of diabetes, FPG and 2hPG are also the main diagnostic criteria, and they are used for the diagnosis of blood glucose levels in diabetic patients[24]. Diabetic nephropathy is a chronic kidney disease. Studies have shown that inflammation and depression have a two-way connection between people with chronic disease[25]. In chronic kidney disease, the increase in anxiety susceptibility may be associated with the inflammatory process of the toxin, the increase of oxidative stress, brain microvascular damage and the participation of the renin-angiotensin system[26]. So we can speculate that after nursing interventions, the patient’s anxiety and depression were relieved. This affects the function of inflammation and kidney function, which affects the level of blood creatinine.
SCr and BUN are the parameters usually used to estimate renal function of which SCr is a small molecule substance metabolized by muscle and BUN is a nitrogen-containing compound in plasma, and the excretion of both into the body is completed by glomerular filtration. Glomerular filtration is also decreased when kidney function is compromised, causing BUN and SCr to be incompletely eliminated from the body, thus resulting in increased serum levels of both[27]. This study found that the implementation of humanistic nursing can better control the blood glucose level of patients with DKD facilitating the maintenance of residual renal function. The study found that after the implementation of humanistic nursing, the healing, life and nursing satisfaction of patients were remarkably enhanced, and the complications and negative emotions were remarkably reduced, which suggests that humanistic nursing has a very high application value in hemodialysis.
In hemodialysis for patients with DKD, the implementation of humanistic nursing has achieved ideal results, which can effectively reduce the psychological negative emotion mark of patients, so that they can actively cooperate with the diagnosis and nursing, to facilitate the control of blood glucose and the enhancement of residual renal function, to reduce the occurrence of complications, and finally to enhance the life quality and nursing satisfaction of patients. It is worthy of being widely popularized and applied. However, the main limitations of our study are the small number of studied patients and the too short follow-up time. Our intention is to continue to study these aspects in future research with a more wide number of DKD patients.
Diabetic nephropathy is one of the common complications of diabetes, and as the disease progresses, patients may need to receive hemodialysis treatment. In the process of receiving hemodialysis, patients need long-term treatment, and the condition is changeable, so quality nursing services are needed to improve the treatment effect and the quality of life of patients. Humanistic nursing is a kind of patient-centered nursing concept, emphasizing respect for patients’ lives and personalities, paying attention to patients’ emotions and needs, and providing patients with comprehensive and personalized nursing services.
The traditional hemodialysis nursing model often only focuses on the physiological needs of patients, ignoring the psychological and social needs of patients, resulting in patients are prone to anxiety, depression and other adverse emotions in the treatment process, affecting the treatment effect. Therefore, the purpose of this study is to explore the application effect of anthropogenic nursing in hemodialysis nursing of diabetic nephropathy patients, to provide patients with more comprehensive and personalized nursing services.
The first is to discuss the application effect of humanistic nursing in hemodialysis nursing of diabetic nephropathy patients; the second is to evaluate the impact of humanistic nursing on patients’ quality of life, mental health and satisfaction.
A total of 96 diabetic kidney disease patients receiving hemodialysis treatment from March 2020 to June 2022 were selected as the study objects. The control group was given routine nursing, while the research group was given humanized nursing on this basis, including the following aspects: Nurses and patients fully communicate and exchange, understand the patient’s condition, family background, psychological state, etc., to provide personalized nursing services for patients; psychological support: Nurses provide psychological counseling and support to patients to help them relieve bad emotions and enhance treatment confidence; health education: Nurses provide comprehensive health education to patients, including diet guidance, exercise guidance, medication guidance, etc., to improve patients’ self-management ability; social support: Nurses provide family and social support to help patients deal with difficulties and problems in life. The control group received routine care. At the end of the trial, all patients were assessed for quality of life, mental health and satisfaction.
By comparing data from the experimental and control groups, we found that patients in the experimental group were better than those in the control group in terms of quality of life, mental health and satisfaction. After receiving humanistic care, anxiety, depression and other bad emotions were effectively alleviated, the treatment effect was improved, and the quality of life was improved. At the same time, the satisfaction of the experimental group was also higher than that of the control group.
Humanistic nursing has a remarkable effect on hemodialysis nursing of diabetic nephropathy patients. Through humanistic nursing, patients’ mental health and quality of life have been effectively improved, the treatment effect has been improved, and the satisfaction of patients has also been improved. Therefore, we suggest to promote and apply humanistic nursing concept in hemodialysis nursing of diabetic nephropathy patients.
From the perspective of patient needs, understand the physiological, psychological and social needs of patients. From the perspective of nursing practice, this paper explores the application method and effect of humanistic nursing concept in hemodialysis nursing practice. From the perspective of nursing staff, this paper discusses the requirements of humanistic nursing on the quality and working style of nursing staff, and the experience and feeling of nursing staff in the process of implementing humanistic nursing.
We thank all medical staff and technicians of dialysis centers who agreed to participate in this study.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Endocrinology and metabolism
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D, D
Grade E (Poor): 0
P-Reviewer: Freund O, Israel; Martinez-Castelaoa A, Spain S-Editor: Wang JJ L-Editor: Filipodia P-Editor: Chen YX
| 1. | Siegel KR, Ali MK, Zhou X, Ng BP, Jawanda S, Proia K, Zhang X, Gregg EW, Albright AL, Zhang P. Cost-effectiveness of Interventions to Manage Diabetes: Has the Evidence Changed Since 2008? Diabetes Care. 2020;43:1557-1592. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 111] [Article Influence: 22.2] [Reference Citation Analysis (0)] |
| 2. | Varghese RT, Jialal I, Doerr C. Diabetic Nephropathy (Nursing). 2023 Jul 24. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. [PubMed] |
| 3. | Scarton L, Hebert LE, Goins RT, Umans JG, Jiang L, Comiford A, Chen S, White A, Ritter T, Manson SM. Diabetes and health-related quality of life among American Indians: the role of psychosocial factors. Qual Life Res. 2021;30:2497-2507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Brown EA, Zhao J, McCullough K, Fuller DS, Figueiredo AE, Bieber B, Finkelstein FO, Shen J, Kanjanabuch T, Kawanishi H, Pisoni RL, Perl J; PDOPPS Patient Support Working Group. Burden of Kidney Disease, Health-Related Quality of Life, and Employment Among Patients Receiving Peritoneal Dialysis and In-Center Hemodialysis: Findings From the DOPPS Program. Am J Kidney Dis. 2021;78:489-500.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 82] [Article Influence: 20.5] [Reference Citation Analysis (0)] |
| 5. | Tamru K, Aga F, Berhanie E, Aynalem YA, Shiferaw WS. Incidence of diabetic nephropathy in patients with type 2 diabetes mellitus at a tertiary healthcare setting in Ethiopia. Diabetes Metab Syndr. 2020;14:1077-1083. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Yu L, Yang X, Hao J. Study on the effect of high quality nursing in patients with diabetic nephropathy. Panminerva Med. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Guo Y, Song Q, Cui Y, Wang C. Clinical Effects of Primary Nursing on Diabetic Nephropathy Patients Undergoing Hemodialysis and Its Impact on the Inflammatory Responses. Evid Based Complement Alternat Med. 2022;2022:1011415. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 8. | Guo F, Lin YL, Raji M, Leonard B, Chou LN, Kuo YF. Processes and outcomes of diabetes mellitus care by different types of team primary care models. PLoS One. 2020;15:e0241516. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 9. | Morfin JA, Fluck RJ, Weinhandl ED, Kansal S, McCullough PA, Komenda P. Intensive Hemodialysis and Treatment Complications and Tolerability. Am J Kidney Dis. 2016;68:S43-S50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 56] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 10. | Ahmadmehrabi S, Tang WHW. Hemodialysis-induced cardiovascular disease. Semin Dial. 2018;31:258-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 101] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 11. | Gupta V, Yassin MH. Infection and hemodialysis access: an updated review. Infect Disord Drug Targets. 2013;13:196-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 12. | Masud A, Costanzo EJ, Zuckerman R, Asif A. The Complications of Vascular Access in Hemodialysis. Semin Thromb Hemost. 2018;44:57-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 33] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 13. | Rigg GA, Bercu BA. Hypoglycemia--a complication of hemodialysis. N Engl J Med. 1967;277:1139-1140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | El Berri H, Gedik FG, Belkhadir J, Catton H, Hammerich A, Oweis A, Slama S. Tackling diabetes: how nurses can make the difference. East Mediterr Health J. 2020;26:1318-1319. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 15. | Liao K, Lin KC, Chiou SJ. Self-efficacy remains a vital factor in reducing the risk of dialysis in type 2 diabetes care. Medicine (Baltimore). 2021;100:e26644. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 16. | Chen HC, Lai MJ, Wu WC, Lee CY, Lin HJ, Lin CC, Chang CT, Wang CCN, Chou CY. Association of diabetes, education level, and care dependency with use of temporary vascular access in patients with chronic kidney disease. Semin Dial. 2021;34:130-136. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 17. | Li L, Chen H, Peng C, Yang L. Analysis on Value of Continuous Nursing Based on WeChat in Improving Healthy Quality of Life and Self-Management Behavior of Patients with Diabetic Nephropathy. Evid Based Complement Alternat Med. 2022;2022:5131830. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 18. | Beetham KS, Krishnasamy R, Stanton T, Sacre JW, Douglas B, Isbel NM, Coombes JS, Howden EJ. Effect of a 3-Year Lifestyle Intervention in Patients with Chronic Kidney Disease: A Randomized Clinical Trial. J Am Soc Nephrol. 2022;33:431-441. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 30] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 19. | Blanchfield D, O'Connor L. A participatory action research study to inform combined type 2 diabetes and chronic kidney disease care provided in the context of advanced practice nursing. J Adv Nurs. 2022;78:3427-3443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 20. | Mott AK. Diabetes Mellitus Self-Management to Decrease the Risk for Chronic Kidney Disease. Nephrol Nurs J. 2021;48:65-63. [PubMed] |
| 21. | Watanabe H, Anezaki H, Kazawa K, Tamaki Y, Hashimoto H, Moriyama M. Long-term effectiveness of a disease management program to prevent diabetic nephropathy: a propensity score matching analysis using administrative data in Japan. BMC Endocr Disord. 2022;22:135. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 22. | Lucena AF, Magro CZ, Proença MCDC, Pires AUB, Moraes VM, Aliti GB. Validation of the nursing interventions and activities for patients on hemodialytic therapy. Rev Gaucha Enferm. 2018;38:e66789. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 23. | Pérez-Alba A, Catalán Navarrete S, Renau Ortells E, García Peris B, Agustina Trilles A, Cerrillo García V, Calvo Gordo C. Nursing program to support home hemodialysis. Experience of a center. Nefrologia (Engl Ed). 2021;41:360-362. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (1)] |
| 24. | Yuan L, Yuan H, Feng Q, Zhao J. Effect of continuous nursing on quality of life of hemodialysis patients: A protocol for systematic review and meta-analysis. Medicine (Baltimore). 2021;100:e24942. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 25. | Katon WJ. Epidemiology and treatment of depression in patients with chronic medical illness. Dialogues Clin Neurosci. 2011;13:7-23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 412] [Cited by in RCA: 486] [Article Influence: 34.7] [Reference Citation Analysis (0)] |
| 26. | Huang CW, Wee PH, Low LL, Koong YLA, Htay H, Fan Q, Foo WYM, Seng JJB. Prevalence and risk factors for elevated anxiety symptoms and anxiety disorders in chronic kidney disease: A systematic review and meta-analysis. Gen Hosp Psychiatry. 2021;69:27-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 80] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 27. | Acharya DK, Nilmanat K, Boonyasopun U. Textual Organization of Hemodialysis Nursing Practice: An Institutional Ethnography. J Nepal Health Res Counc. 2022;20:180-185. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |