Published online Jan 15, 2024. doi: 10.4239/wjd.v15.i1.1
Peer-review started: October 21, 2023
First decision: December 6, 2023
Revised: December 10, 2023
Accepted: December 28, 2023
Article in press: December 28, 2023
Published online: January 15, 2024
Processing time: 83 Days and 6.7 Hours
Tai Chi, a practice that combines elements of both exercise and mindfulness, offers a wide range of health benefits. The body of evidence concerning the impact of Tai Chi on diabetes has recently been growing. This editorial aims to provide a concise summary of the current state of evidence for Tai Chi's effects on individuals with type 2 diabetes (T2D). The review includes 3 randomized controlled trials (RCTs) and 5 systematic reviews and meta-analyses, all of which investigate the effectiveness of Tai Chi on various health outcomes in individuals with T2D. Tai Chi demonstrates a significant effect to enhance glycemic control, lower blood pressure, improve serum lipid profiles, reduce insulin resistance, positively influence obesity-related indices, and improve overall quality of life in individuals with T2D. However, it is noteworthy that recent RCTs have reported inconsistent findings regarding the effects of Tai Chi on glycemic control and insulin resistance. The author also delves into potential mechanisms by which Tai Chi may exert its influence on the human body. Finally, the editorial highlights the critical issues that warrant further exploration in the future.
Core Tip: Exercise therapy plays a crucial role in the management of diabetes. Tai Chi offers a unique approach, serving not only as a moderate-intensity exercise but also as a mindfulness intervention that incorporates deep breathing and meditation. While prior systematic reviews have highlighted the favorable effects of Tai Chi on glycemic control and metabolic parameters in individuals with type 2 diabetes, recent randomized controlled trials have yielded inconsistent findings. This suggests that Tai Chi holds potential as an addition to diabetes management, yet there remains an insufficiency of scientific evidence, particularly in terms of elucidating its biological mechanisms of action.
- Citation: Hamasaki H. Effects of Tai Chi in diabetes patients: Insights from recent research. World J Diabetes 2024; 15(1): 1-10
- URL: https://www.wjgnet.com/1948-9358/full/v15/i1/1.htm
- DOI: https://dx.doi.org/10.4239/wjd.v15.i1.1
Tai Chi, a traditional Chinese martial art, provides various health benefits. In 2016, Huston and McFarlane[1] summarized the evidence regarding the effects of Tai Chi on health as follows:
Strong evidence supports the positive impact of Tai Chi exercise in managing depression, aiding in cardiac and stroke rehabilitation, and addressing dementia. There is also moderate evidence suggesting that Tai Chi exercise can improve the quality of life (QOL) for patients with cancer, fibromyalgia, hypertension, and osteoporosis. However, there is currently no clear evidence directly linking Tai Chi exercise to benefits for diabetes, rheumatoid arthritis, or chronic heart failure. Systematic reviews on overall health and fitness consistently demonstrate strong evidence for improving balance and aerobic capacity, particularly in individuals with low fitness levels. Furthermore, there is good evidence indicating that Tai Chi exercise can enhance lower limb strength, with moderate evidence suggesting improvements in overall well-being and sleep quality.
Tai Chi serves as a dual intervention, encompassing both exercise and mindfulness. Mindfulness-based interventions have demonstrated a positive impact on glycemic control, leading to an approximate 0.3% reduction in hemoglobin A1c (HbA1c) levels in individuals with type 2 diabetes (T2D)[2]. In addition, traditional martial arts, such as Tai Chi, incorporate breathing techniques aimed at harmonizing the human body. For instance, diaphragmatic breathing can effectively alleviate both physiological and psychological stress, potentially benefiting the brain and cardiovascular (CV) system by enhancing autonomic nervous system (ANS) function[3]. Notably, a recent systematic review has revealed that Tai Chi enhances heart rate variability, which is closely associated with ANS function, when compared to control groups[4].
Patients with diabetes frequently experience ANS dysfunction, and CV autonomic neuropathy plays a pivotal prognostic role in CV morbidity and mortality. Exercise holds the potential to rectify sympatho-vagal balance by elevating parasympathetic nervous system activity while reducing sympathetic nervous activity in individuals with T2D. This adjustment could be particularly valuable in the management of diabetes patients at risk of severe hypoglycemia unawareness[5]. Consequently, Tai Chi, which incorporates both exercise and mindfulness, may offer additional benefits to diabetes patients compared to conventional structured exercise.
The body of evidence regarding the effects of Tai Chi on diabetes has been steadily growing. A PubMed search utilizing the terms "Tai Chi" and "diabetes" yielded 168 articles as of September 30, 2023. Among these, 52 articles were randomized controlled trials (RCTs) and systematic reviews. In this paper, the author reviewed representative RCTs and systematic reviews published within the last five years, summarizing the current state of evidence on this topic.
The author identified three eligible RCTs published between 2018 and 2023.
In the study by Chan et al[6], the effects of Tai Chi on reducing CV risk factors were compared to brisk walking in adults with hypertension. Although the study participants were not necessarily patients with diabetes, 58.5% of them had diabetes, prompting the author's review. A total of 246 adults with hypertension were randomly assigned to three groups: Tai Chi (n = 82), brisk walking (n = 82), or a control group (n = 82). However, 52 participants dropped out at the 9-month follow-up point, resulting in a dropout rate of 21.1%. An intention-to-treat analysis was conducted accordingly. The adherence rate to the exercise intervention was 90% in the Tai Chi group and 88% in the brisk walking group during the 3-mo study period. In the Tai Chi group, participants performed a 24-form Yang style Tai Chi for 60 min, twice a week, for a duration of three months. All training sessions were led by the same qualified and experienced Tai Chi Master. Additionally, participants were encouraged to engage in daily Tai Chi practice at home for 30 min, on at least five days each week, both during and after the 3-mo study period. Adherence to the intervention was defined as successfully completing at least 80% of the recommended sessions.
In contrast, individuals in the brisk walking group were instructed to walk at a pace of 5 to 6 km/h for 30 min a day, on at least five days per week. Each participant was provided with a pulse oximeter to monitor their heart rate during brisk walking and was advised to aim for a personalized heart rate corresponding to a moderate-intensity exercise, determined based on their age. The primary outcome measured was the change in blood pressure. Secondary outcomes included fasting blood glucose and HbA1c levels.
At the 9-mo follow-up, Tai Chi demonstrated significant improvements in various CV risk factors compared to the control group. These improvements encompassed a substantial decrease in systolic blood pressure (−13.33 mmHg) and diastolic blood pressure (−6.45 mmHg), lower fasting blood glucose levels (−0.72 mmol/L), reduced HbA1c levels (−0.39%), decreased perceived stress, and improved mental health and self-efficacy in exercising. Notably, the Tai Chi group exhibited even more pronounced improvements compared to the brisk walking group. Specifically, the Tai Chi group experienced more substantial decreases in systolic blood pressure (−12.46 mmHg), diastolic blood pressure (−3.20 mmHg), and fasting glucose levels (−1.27 mmol/L), more significant drops in HbA1c levels (−0.56%), lower levels of perceived stress, and more substantial enhancements in perceived mental health and exercise self-efficacy in contrast to the brisk walking group. However, no significant differences emerged in body mass index (BMI), waist circumference, serum cholesterol levels, aerobic endurance, and perceived physical health among the groups at the 9-mo follow-up.
The authors concluded that Tai Chi displayed more favorable effects on CV risks compared to brisk walking. However, it is worth noting that they did not describe whether the participants in the brisk walking group were encouraged to continue brisk walking after the 3-mo intervention, whereas the participants in the Tai Chi group were encouraged to engage in daily Tai Chi practice at home for 30 min. This disparity in post-intervention activities may have introduced some bias. Indeed, at the 3-mo mark, no significant differences in glycemic control appeared to exist between the Tai Chi group and brisk walking group.
Li et al[7] conducted a study to examine the therapeutic effects of Tai Chi and Qigong exercises in middle-aged and older patients with T2D. Initially, 103 eligible patients were randomly allocated to the Tai Chi group, the Qigong group, and the control group. However, 16 participants dropped out, leaving 24 participants in the Tai Chi group, 34 participants in the Qigong group, and 29 participants in the control group who completed the study. Each group engaged in 60 min of exercise, five times a week, over a span of 12 wk.
For the Tai Chi intervention, the authors employed the classical Chen style (18 forms), and these Tai Chi classes were led by an experienced instructor. Each session adhered to a structured format, commencing with a 10-min warm-up and self-massage, followed by a 10-min review of principles and essential movements, 30 min of practice and skill-building, and concluding with a 10-min relaxation period.
In contrast, the Qigong exercise was specifically tailored based on the theory of meridians in traditional Chinese medicine, with a focus on the unique characteristics of diabetic patients. Each Qigong movement was designed to promote meridian circulation, emphasizing the benefits of clearing various meridians to prevent and treat diseases related to internal organs. Professional instructors from the Fitness Qigong Association of Jiaozuo led the fitness Qigong classes, and similar to the Tai Chi sessions, these classes followed a structured pattern. They started with a 10-min warm-up and self-massage, followed by a 10-min review of movement principles and breathing techniques, a 30-min practice session, and ended with a 10-min relaxation period. Throughout the intervention period, participants were encouraged to practice Qigong for approximately 60 min at home.
As for the control group, participants engaged in low-intensity stretching exercises. Each class session consisted of 40 min of activity, which included a 10-min warm-up and self-massage, followed by 30 min of supervised stretching exercises. These stretching exercises primarily focused on the upper body, trunk, and lower body, incorporating controlled breathing and relaxation techniques.
Fasting blood glucose levels increased in the control group, slightly decreased in the Qigong group, and remained unchanged in the Tai Chi group. However, there was no significant difference in the effects of the interventions between the groups. Although no significant difference was observed between the groups, HbA1c levels decreased in the control group and showed no change in the Qigong group. On the other hand, HbA1c levels increased in the Tai Chi group compared to those in the control group. This result is unexpected, as regular exercise typically leads to improvements in glycemic control. The author speculates that other factors, such as dietary intake and changes in medications, which were not mentioned in the paper, may have contributed to this outcome.
Furthermore, blood C-peptide levels significantly decreased in the Tai Chi group compared to both the Qigong group and the control group. The authors mentioned the possibility that Tai Chi exercise may lead to a decrease in insulin secretion in patients with T2D. However, given that Tai Chi involves moderate-intensity exercise and offers various health benefits, including insulin sensitivity[8], caution is needed in interpreting these results.
Most recently, Chen et al[9] assessed the effectiveness of Tai Chi exercise in improving cognitive function compared to fitness walking in patients with T2D who had mild cognitive impairment. A total of 328 patients were randomly assigned to three groups: The Tai Chi group (n = 107), the fitness walking group (n = 110), and the control group (n = 111). All participants were included in the intention-to-treat analysis, and 289 participants (88.1%) completed the study, with 282 participants (86.0%) evaluated at the 36-wk follow-up. The adherence rate for the intervention was 88.8% in the Tai Chi group and 90.0% in the fitness walking group.
The primary outcome measured was cognitive function, assessed using the Montreal Cognitive Assessment (MoCA) at 36 wk. Secondary outcomes included fasting blood glucose, insulin, homeostasis model assessment-insulin resistance (HOMA-IR), HbA1c, advanced glycation end products (AGEs), and soluble receptor of AGE (sRAGE) levels. All groups attended educational seminars focused on T2D management, with each seminar lasting 30 min. These seminars were held once every four weeks during the 24-wk study period.
Participants in the Tai Chi group underwent supervised 24-wk training in the 24-form Tai Chi, with 1-h training sessions three times a week. Additionally, participants were encouraged to continue exercising beyond the 24-wk supervised period, up until the 36-wk follow-up evaluation. Certified instructors guided the fitness walking and Tai Chi exercises. Participants in the control group did not receive any exercise intervention and maintained their usual lifestyle.
In comparison to fitness walking, Tai Chi exercise at 36 wk demonstrated a greater improvement in mean MoCA scores (24.67 ± 2.72 vs 23.84 ± 3.17; between-group mean difference (MD) of 0.84; 95%CI: 0.02 to 1.66). Furthermore, Tai Chi was more effective in enhancing other cognitive subdomain test results, fasting blood glucose levels (129.4 ± 25.9 mg/dL vs 139.5 ± 36.2 mg/dL; between-group MD of −10.3; 95%CI: −18.6 to −2.3), and the AGE/sRAGE ratio (0.05 ± 0.03 vs 0.07 ± 0.05; between-group MD of −0.02; 95%CI: −0.03 to −0.01). However, no significant differences were observed in HOMA-IR and HbA1c levels.
At 24 wk, Tai Chi did not exhibit a significantly greater improvement in MoCA scores compared to fitness walking. Nonetheless, Tai Chi was more effective in enhancing certain cognitive subdomain test results compared to fitness walking. Additionally, there were no differences between groups in fasting blood glucose and HbA1c levels, HOMA-IR, and the AGE/sRAGE ratio.
Compared with the control group, Tai Chi significantly improved mean MoCA scores at 24 wk (23.99 ± 3.10 vs 22.54 ± 3.29; between-group MD of 1.45; 95%CI: 0.59 to 2.32). However, no significant improvements were observed in fasting blood glucose and HbA1c levels, HOMA-IR, and the AGE/sRAGE ratio.
At 36 wk, the Tai Chi group exhibited a significant improvement in cognitive subdomain test results, fasting blood glucose levels (129.4 ± 25.9 mg/dL vs 140.0 ± 29.7 mg/dL; between-group MD of -10.6; 95%CI: −18.9 to −2.3), and the AGE/sRAGE ratio (0.05 ± 0.03 vs 0.07 ± 0.04; between-group MD of −0.02; 95%CI: −0.03 to −0.01). However, HbA1c levels and HOMA-IR did not differ significantly between groups.
Although one patient in the control group reported hospital admission and one patient in the Tai Chi group visited the emergency department, there was no significant difference in the number of adverse events among the three groups. These findings suggest that Tai Chi exercise has a beneficial effect on cognitive function and may offer protection to the vasculature. However, it may not significantly improve glycemic control in patients with T2D.
Table 1 summarizes RCTs investigating the effects of Tai Chi in patients with T2D.
| Ref. | Country | Study design | Study period (follow-up period) | Subjects (baseline characteristics) | Study outcomes | Intervention/Control | Results |
| Chan et al[6], 2018 | China | Three-arm, randomized, controlled, parallel-group trial | 12 wk (9 month) | 246 patients with T2D. Tai Chi group (32 men and 50 women): Age: 64.70 ± 7.59 years, BMI: 26, 38 ± 4.26 kg/m2, HbA1c: 6.66% ± 1.17% | Primary outcome: Blood pressure Secondary outcomes: BMI, waist circumference, aerobic endurance, fasting blood glucose, HbA1c, TC, TG, HDL-C, LDL-C, perceived stress, quality of life, exercise self-efficacy | Tai Chi/brisk walking/usual physical activity | Blood pressure↓1. Fasting blood glucose↓, HbA1c↓, perceived stress↓. Exercise self-efficacy↑2 |
| Walking group (42 men and 40 women): Age: 63.22 ± 11.11 years, BMI: 25.90 ± 4.39 kg/m2, HbA1c: 7.10% ± 1.61% | |||||||
| Control group (38 men and 44 women): Age: 65.13 ± 10.22 years, BMI: 25.72 ± 4.04 | |||||||
| Li et al[7], 2020 | China | Three-arm, randomized, controlled, parallel-group trial | 12 wk | 87 patients with T2D. Tai Chi group (12 men and 12 women): Age: 61.71 ± 6.91 years, BMI: 24.04 ± 2.98 kg/m2, HbA1c: 8.20% ± 2.46% | Primary outcome: Fasting blood glucose, HbA1c, C-peptide | Tai Chi/Qigong/stretching exercise | Fasting blood glucose→3, HbA1c↑, C-peptide↓ |
| Qigong group (21 men and 13 women): Age: 59.71 ± 6.67 years, BMI: 25.21 ± 2.71 kg/m2, HbA1c: 7.99% ± 1.66% | |||||||
| Control group (14 men and 15 women): Age: 58.66 ± 10.89 years, BMI: 25.69 ± 2.57 | |||||||
| Chen et al[9], 2023 | China | Three-arm, randomized, controlled, parallel-group trial | 24 wk (36 wk) | 328 patients with T2D. Tai Chi group (49 men and 58 women): Age: 67.56 ± 4.99 years, BMI: 24.32 ± 3.03 kg/m2, HbA1c: 7.04% ± 1.20% | Primary outcome: MoCA assessment at 36 wk. Secondary outcomes: MoCA assessment at 24 wk, cognitive subdomain tests, fasting blood glucose, HbA1c, AGE, sRAGE, HOMA-IR | AE + RT/usual care | MoCA score at 36 wk↑ vs fitness walking group: (at 24 wk). Fasting blood glucose→, HbA1c→, HOMA-IR→, AGE: sRAGE ratio→. (at 36 wk) Fasting blood glucose↓, HbA1c→, HOMA-IR→, AGE: sRAGE ratio↓ vs control group: (at 24 wk) Fasting blood glucose→, HbA1c→, HOMA-IR→, AGE: sRAGE ratio→. (at 36 wk) Fasting blood glucose↓, HbA1c→, HOMA-IR→, AGE: SRAGE ratio↓ |
| Fitness walking group (61 men and 49 women): Age: 67.46 ± 4.73 years, BMI: 23.86 ± 2.90 kg/m2, HbA1c: 6.84% ± 1.41% | |||||||
| Control group (51 men and 60 women): Age: 67.62 ± 5.35 years, BMI: 23.98 ± 3.40 kg/m2, HbA1c: 7.14% ± 1.48% |
The author identified a total of five systematic reviews and meta-analyses investigating the effects of Tai Chi on health outcomes in patients with T2D.
In a review by Zhou et al[10], 25 studies were assessed, focusing on the effects of Tai Chi on physiological parameters, balance function, and QOL in T2D patients. It's worth noting that all the included studies were RCTs; however, 17 out of 25 (68%) articles were of Chinese origin and were not listed in major English databases such as PubMed.
The review found that Tai Chi was effective in reducing fasting blood glucose levels [21 studies; standardized MD (SMD) = −0.67; 95%CI: −0.87 to −0.47], HbA1c levels (14 studies; MD = −0.88%; 95%CI: −1.45% to −0.31%), HOMA-IR (5 studies; MD = −0.41; 95%CI: −0.78 to −0.04), total cholesterol levels (10 studies; SMD = −0.59; 95%CI: −0.90 to −0.27), systolic blood pressure (5 studies; MD = −10.03 mmHg, 95%CI: −15.78 to −4.29 mmHg), diastolic blood pressure (5 studies; MD = −4.85 mmHg, 95%CI: −8.23 to −1.47 mmHg), and BMI (7 studies; MD = −0.82 kg/m2, 95%CI: −1.28 to −0.37 kg/m2). Moreover, Tai Chi improved QOL in terms of physical function, pain, and social function. However, Tai Chi exhibited no significant effect on fasting insulin levels and balance function. The quality of the included studies was assessed using the PEDro scale. Most of the studies received scores of 4 or 5, with only 3 studies scoring 6 to 10 (indicating high quality).
Xia et al[11] investigated the differences in the effectiveness of Tai Chi for glycemic control in T2D patients based on different durations and styles of interventions. The analysis included a total of 17 RCTs. Among these, 12 studies (70.6%) were conducted in China, while others were carried out in Taiwan, Australia, and Thailand. Various Tai Chi styles were utilized, including the simplified style (n = 4), Yang-style (n = 3), Lin-style (n = 1), Da Yuan Jiang Tang-style (n = 1), Chen-style (n = 2), Sun-style and Yang-style (n = 2), Tai Chi Ball (n = 2), and an unknown style (n = 2). The number of sessions per week and the duration of Tai Chi exercise also varied.
The findings revealed that Tai Chi significantly reduced fasting blood glucose levels (13 studies; SMD = −0.54; 95%CI: −0.91 to −0.16) and HbA1c levels (9 studies; SMD = −0.68; 95%CI: −1.17 to −0.19) in comparison to control groups. However, Yang-style Tai Chi and 24 movements (simplified style) did not show improvements in glycemic control, and other styles with a duration of ≤ 12 wk also had no significant effects on glycemic control. On the other hand, Tai Chi, excluding the simplified style and Yang-style Tai Chi with a duration of > 12 wk, led to reductions in fasting blood glucose (2 studies; SMD = −0.90; 95%CI: −1.28 to −0.52) and HbA1c levels (2 studies; SMD = −0.90; 95%CI: −1.28 to −0.52).
Furthermore, Tai Chi was effective in reducing total cholesterol (7 studies; SMD = −0.35; 95%CI: −0.54 to −0.16), triglycerides (8 studies; SMD = −0.19; 95%CI: −0.31 to −0.07), and BMI (6 studies; SMD = −0.61; 95%CI: −0.85 to −0.38). However, it is important to note that the methodological quality of the included studies was generally low due to potential biases, including the inability to blind participants to the intervention.
Palermi et al[12] examined the impact of Tai Chi programs on balance function in patients with T2D. This systematic review included only 3 RCTs and one before-after quasi-experimental study written in English. The findings revealed that Tai Chi effectively improved balance function, as measured by the single-leg stance test, tandem walk score, or Berg Balance Scale (SMD = 0.52; 95%CI: 0.20 to 0.84). The overall quality of the included RCTs, assessed using the Cochrane risk-of-bias tool, was categorized as "some concerns."
Qin et al[13] assessed the impact of Tai Chi on BMI, waist-to-hip ratio, and QOL in patients with T2D. The analysis included 15 RCTs and 3 quasi-experimental studies. Among these, 14 studies (77.8%) were conducted in China, while the others were carried out in Australia, South Korea, and Thailand. The results showed that compared with control groups, Tai Chi led to a reduction in BMI (11 studies; MD = −1.53 kg/m2; 95%CI −2.71 kg/m2 to −0.36 kg/m2). However, Tai Chi did not have a significant effect on BMI when compared to other types of exercise, such as aerobic exercise, walking, and dancing. In contrast, Tai Chi did not demonstrate a beneficial effect on the waist-to-hip ratio. Moreover, Tai Chi improved QOL, as measured by Medical Outcomes Study Short Form-36 (e.g., physical function: MD = 7.73; 95%CI: 1.76 to 13.71; body pain: MD = 8.49; 95%CI: 1.18 to 15.8; overall health: MD = 9.80; 95%CI: 5.77 to 13.82; social functioning: MD = 9.1; 95%CI: 4.75 to 13.45; mental health: MD = 5.62; 95%CI: 1.57), compared to control groups. The mean methodological quality score, as measured by the PEDro scale, was 5.3, indicating that the overall quality of the included studies was "fair".
Recently, Guo et al[14] reported that Tai Chi had a favorable impact on metabolic parameters in patients with T2D; however, its superior effects were observed only in relation to HbA1c and high-density lipoprotein cholesterol when compared to aerobic exercise. The analysis encompassed a total of 23 RCTs, with 19 studies (82.6%) conducted in China, 3 studies in Australia, and one study in South Korea.
Tai Chi was found to significantly reduce fasting blood glucose levels (15 studies; SMD = −1.04; 95%CI: −1.42 to −0.66) compared to conventional therapies; however, there was no significant difference in fasting blood glucose levels observed between the Tai Chi group and the aerobic exercise group. Furthermore, Tai Chi exhibited a positive effect on postprandial glucose levels (2 studies; MD = −1.58, units not specified but assumed to be mmol/L; 95%CI: −1.94 to −1.22) when compared to conventional therapies. The reduction in HbA1c levels was also more significant in the Tai Chi group (9 studies; MD = −1.28%; 95%CI: −2.06 to −0.51) compared to conventional therapies, and Tai Chi showed a trend towards statistical significance in decreasing HbA1c levels (5 studies; MD = −0.24%; 95%CI: −0.49 to 0.00, P = 0.05) compared to the aerobic exercise group.
Moreover, Tai Chi significantly reduced total cholesterol levels (11 studies; SMD = −0.50; 95%CI: −0.86 to −0.13), triglycerides (9 studies; SMD = −0.38; 95%CI: −0.65 to −0.10), and low-density lipoprotein cholesterol levels (9 studies; SMD = −0.38; 95%CI: −0.65 to −0.10) compared to conventional therapies. However, when compared to aerobic exercise, Tai Chi did not offer additional benefits in reducing total cholesterol, triglycerides, and low-density cholesterol levels.
On the other hand, Tai Chi significantly increased high-density cholesterol levels compared to both conventional therapies (9 studies, SMD = 0.13; 95%CI: 0.06 to 0.20) and aerobic exercise (5 studies, SMD = 0.07; 95%CI: 0.01 to 0.12). Moreover, Tai Chi was effective in decreasing BMI (5 studies; MD = −1.15 kg/m2; 95%CI: −1.79 kg/m2 to −0.51 kg/m2), fasting insulin levels (7 studies; MD = −2.63, units not specified but assumed to be μIU/mL; 95%CI: −4.51 to −0.76), HOMA-IR (3 studies; MD = −1.02; 95%CI: −1.39 to −0.64), systolic blood pressure (5 studies; MD = −11.86 mmHg; 95%CI: −14.47 to −9.25 mmHg), and diastolic blood pressure (5 studies; MD = −9.58 mmHg; 95%CI: −11.52 to −7.63 mmHg) compared to conventional therapies. These reductions in BMI and blood pressure were observed regardless of whether the study duration was < 12 wk or 12-24 wk. However, the quality of the included studies remained an issue to be addressed, as there were no studies with a low risk of bias.
Table 2 summarizes systematic reviews and meta-analyses reporting the effectiveness of Tai Chi on health outcomes in T2D patients.
| Ref. | Subjects | Interventions (Tai Chi style) | Comparators | Outcomes | Results |
| Zhou et al[10], 2019 | 1235 patients with T2D. Age: 35.6–69.5 years, sex: No description, BMI: No description, HbA1c: 6.9%–11.9% | Time: 15–120 min/session, Number of sessions: 2–14 sessions/wk, Duration of the intervention: 4–24 wk, (Simplified style, Chen style, Yang style, Sun and Yang style, Lin style, Da-yuan-jiang-tang style) | Usual care, usual exercise, or sham exercise | BMI, fasting blood glucose, HbA1c, insulin, HOMA-IR, TC, blood pressure, QoL (SF-36), balance (single-leg stance test) | BMI↓1, fasting blood glucose↓, HbA1c↓, HOMA-IR↓, insulin→3, TC↓, Systolic blood pressure↓, diastolic blood pressure↓, QOL↑2 |
| Xia et al[11], 2019 | 774 patients with T2D. Age: No description, sex: No description, BMI: No description, HbA1c: No description | Time: 30–60 min/session, Number of sessions: 2–14 sessions/wk, Duration of the intervention: 8–24 wk, (Simplified style, Chen style, Yang style, Sun and Yang style, Lin style, Da-yuan-jiang-tang style, Tai Chi Ball, Unknown style) | Usual care, wait list, dancing, walking or running, conventional exercise, sham exercise, no intervention | BMI, fasting blood glucose, HbA1c, TC, TG, HDL-C, LDL-C | BMI↓, fasting blood glucose↓, HbA1c↓, TC↓, TG↓, HDL-C→, LDL-C→ |
| Palermi et al[12], 2020 | 144 patients with T2D. Age: 62.73–66.05 years (mean), sex: No description, BMI: No description, HbA1c: No description | Time: 55–120 min/session Number of sessions: 2–3 sessions/wk, Duration of the intervention: 12–16 wk, (Yang and Sun style) | Usual care, sham exercise, no intervention | Balance function measured by single-leg stance test, tandem walk test, Balance Index, and Berg Balance Scale | Balance function↑ |
| Qin et al[13], 2020 | 1418 patients with T2D. Age: 47–70 years, sex: No description, BMI: No description, HbA1c: No description | Time: 30–120 min/session, Number of sessions: 1–7 sessions/wk, Duration of the intervention: 12–24 wk | Usual care, wait-list, walking, brisk walking, aerobic exercise, dancing, Baduanjin, sham exercise, no intervention | BMI, waist-to-hip ratio, QOL measured by SF-36 or DSQOL | BMI↓, QOL↑ |
| Guo et al[14], 2021 | 1549 patients with T2D, Age: 46.1–70.4 years (mean), sex: No description, BMI: No description, HbA1c: No description | Time: No description, Number of sessions: No description, Duration of the intervention: No description (Simplified style, Yang and Sun style, Yang style, Chen style) | Usual care, walking, brisk walking, dancing, aerobic exercise, sham exercise | BMI, fasting blood glucose, HbA1c, insulin, HOMA-IR, TC, TG, HDL-C, LDL-C, blood pressure | BMI↓, fasting blood glucose↓ (→ vs aerobic exercise), HbA1c↓, insulin↓, HOMA-IR↓, TC↓ (→ vs aerobic exercise), TG↓ (→ vs aerobic exercise), HDL-C↓, LDL-C↓ (→ vs aerobic exercise), blood pressure↓ |
Based on the findings of recent systematic reviews and meta-analyses, Tai Chi significantly reduces fasting blood glucose and HbA1c levels. Furthermore, Tai Chi improves blood pressure, serum lipid profiles, insulin resistance, obesity-related indices, and the QOL in patients with T2D. However, recent RCTs have shown inconsistent effects of Tai Chi on glycemic control and insulin resistance. This inconsistency may be attributed to variations in Tai Chi styles[11] and differences in control group interventions (e.g., usual care, sham exercise, aerobic exercise)[13,14].
Most systematic reviews, except Palermi et al[12], have reported significant heterogeneity among the included RCTs. Therefore, the effectiveness of Tai Chi on glycemic control may vary based on demographic characteristics of study subjects, physical fitness, medications, the severity of diabetes, and comorbidities, including diabetic complications and CV diseases. Furthermore, the majority of the studies have been conducted in China, which could introduce regional bias and limit the generalizability of the evidence. In addition, there is a lack of well-designed studies investigating the effects of Tai Chi in patients with type 1 diabetes, a condition characterized by depleted insulin secretion. Since the pathophysiology of type 1 diabetes differs significantly from that of T2D, further studies in patients with type 1 diabetes are warranted to understand the potential benefits of Tai Chi.
Tai Chi, considered a moderate-intensity exercise, reduces oxidative stress in obese patients with T2D[15]. Exercise is known to have an anti-inflammatory effect mediated by various myokines, such as interleukin (IL)-6, tumor necrosis factor-α, and IL-10[16,17], suggesting that Tai Chi may also reduce inflammation[18]. Yeh et al[19] revealed that Tai Chi exercise decreased HbA1c levels along with an increase in IL-12 Levels and the T-cell helper type 1 reaction in patients with T2D, indicating that Tai Chi benefits immune function. Moreover, a 12-wk Tai Chi exercise improves physical function, vascular function, reduces anxiety and mental fatigue when compared to baseline[20], indicating Tai Chi's potential to help prevent frailty in older adults.
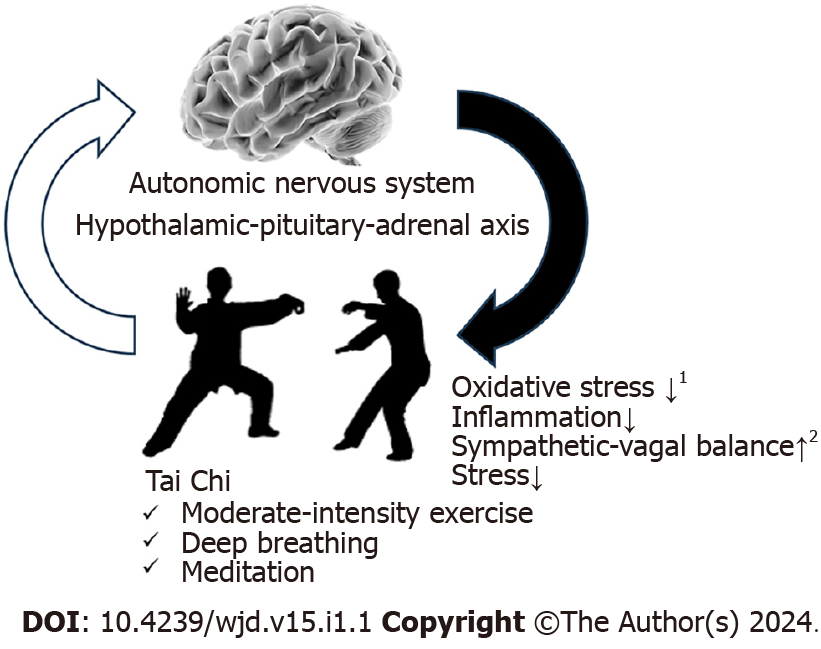
The molecular mechanisms underlying the effects of Tai Chi on noncommunicable diseases (NCDs) remain unclear. However, recent research provides valuable insights that helped elucidate the benefits of Tai Chi in patients with diabetes. Tai Chi exercise has reduced epicardial adipose tissue volume and heart rate by inactivating the mitogen-activated protein kinase/extracellular signal-regulated kinase pathway, along with an increase in serum miR-126 Levels in patients with coronary heart disease[21]. Additionally, Tai Chi influences specific gene expression involved in neutrophil activation, T-cell activation, and the Nod-like receptor signaling pathway in patients with Parkinson’s disease. The key candidate genes play a role in modulating peripheral immunity and inflammation[22]. A recent study revealed that Tai Chi intervention reduced the expressions of inflammatory factors, including Never in Mitosis A-related Kinase 7, nucleotide-binding domain, leucine-rich–containing family, pyrin domain–containing-3, reactive oxygen species, nuclear factor-kappa B, and IL-1β in individuals with prediabetes[23]. Further, Tai Chi exercises may induce beneficial epigenetic changes[24]. Furthermore, Tai Chi may modulate the ANS and the hypothalamus–pituitary–adrenal axis, providing potential therapeutic effects on depression, mood disorders, stress, and gut dysbiosis[25-29] (Figure 1).
However, the effect of gene–environment interactions is likely substantial, considering the etiology of complex diseases, such as diabetes, making the combined effects of environmental and lifestyle factor assessment essential along with Tai Chi on metabolic mechanisms[30]. The combination of a healthy diet, nonsmoking habits, and appropriate alcohol intake with Tai Chi practice demonstrated potential for improving health outcomes in patients with diabetes in terms of the exercise aspect of Tai Chi. No studies directly compare the effectiveness of Tai Chi with these lifestyle factors on a one-to-one basis, while holistic lifestyle interventions are crucial for addressing metabolic disturbances and improving the prognosis of patients with diabetes[31-33]. Moreover, abnormal bowel health, such as chronic diarrhea or constipation, is associated with an increased risk of cancer, CV diseases, and diabetes. Chronic constipation contributes to a higher risk of CV mortality (hazard ratio = 1.698; 95%CI: 1.144 to 2.520)[34]. Indeed, high-fiber diets have improved glycemic control and insulin sensitivity, thereby decreasing all-cause mortality (risk ratio = 0.55; 95%CI: 0.35 to 0.86) when comparing the highest with the lowest fiber intakes[35]. In summary, Tai Chi exercise should be integrated with various lifestyle modifications to improve the management of patients with diabetes.
Molecular pathological epidemiology (MPE) research, which investigates the combined effects of Tai Chi in association with molecular pathologies and clinical outcomes, demonstrates the potential for elucidating the biological mechanisms of Tai Chi in the human body. Traditional epidemiological studies may underestimate true associations between diet, physical activity, smoking, drinking habits, and other lifestyle-related factors concerning molecular markers of genetic pathways and NCD risk. In contrast, MPE studies can help determine the association of such factors with the risk of colorectal cancer[36] and the relationship of host and microbial tryptophan metabolites with T2D risk[37]. The MPE research paradigm not only provides future perspectives on the dynamics among the environment, NCDs, and hosts but also introduces new areas for investigation. Emerging advancements, including computational digital pathology, systems biology, big data analytics, and artificial intelligence, will continue to revolutionize the fields of pathology and MPE[38]. This approach offers a promising direction for fully investigating the effects of Tai Chi on patients with diabetes.
However, high-quality evidence related to the physiological, endocrinological, and biochemical mechanisms of Tai Chi intervention is still insufficient due to methodological limitations, such as the blinding of study participants and the number of well-designed studies, including large-scale RCTs with extended study periods, compared to structured exercise. A PubMed search using the term 'Tai Chi' yielded a limited number of articles (approximately 4000 articles), while a search using the term 'aerobic exercise' resulted in significantly more articles (540000 articles). This suggests that research on Tai Chi is still relatively sparse. Additionally, Tai Chi, unlike other structured exercise programs, is a martial art that typically requires several years to master the various skills, including breathing techniques, specific physical manipulations, and form. If study participants are beginners who engage in mere physical exercise, they may not fully realize Tai Chi's health benefits during the short study duration.
In conclusion, Tai Chi may be considered as an option for exercise therapy in the management of diabetes by clinicians who possess the requisite skills and knowledge of Tai Chi. However, future studies should further explore the differences between conventional exercise and Tai Chi, as well as the underlying biological mechanisms explaining Tai Chi's positive clinical effects in diabetes patients. More research into these areas is essential for building a stronger evidence base.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Endocrinology and metabolism
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): A, A
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Li SY, China; Ogino S, United States; Sanyal D, India S-Editor: Li L L-Editor: A P-Editor: Li L
| 1. | Huston P, McFarlane B. Health benefits of tai chi: What is the evidence? Can Fam Physician. 2016;62:881-890. [PubMed] |
| 2. | Hamasaki H. The Effects of Mindfulness on Glycemic Control in People with Diabetes: An Overview of Systematic Reviews and Meta-Analyses. Medicines (Basel). 2023;10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 3. | Laborde S, Allen MS, Borges U, Dosseville F, Hosang TJ, Iskra M, Mosley E, Salvotti C, Spolverato L, Zammit N, Javelle F. Effects of voluntary slow breathing on heart rate and heart rate variability: A systematic review and a meta-analysis. Neurosci Biobehav Rev. 2022;138:104711. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 96] [Article Influence: 32.0] [Reference Citation Analysis (0)] |
| 4. | Zhou Y, Wang Q, Larkey L, James D, Cui H. Tai Chi Effects on Heart Rate Variability: A Systematic Review and Meta-Analysis. J Integr Complement Med. 2023;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 5. | Hamasaki H. The Effect of Exercise on Cardiovascular Autonomic Nervous Function in Patients with Diabetes: A Systematic Review. Healthcare (Basel). 2023;11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 6. | Chan AWK, Chair SY, Lee DTF, Leung DYP, Sit JWH, Cheng HY, Taylor-Piliae RE. Tai Chi exercise is more effective than brisk walking in reducing cardiovascular disease risk factors among adults with hypertension: A randomised controlled trial. Int J Nurs Stud. 2018;88:44-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 65] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 7. | Li X, Si H, Chen Y, Li S, Yin N, Wang Z. Effects of fitness qigong and tai chi on middle-aged and elderly patients with type 2 diabetes mellitus. PLoS One. 2020;15:e0243989. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 8. | Zou L, Xiao T, Cao C, Smith L, Imm K, Grabovac I, Waldhoer T, Zhang Y, Yeung A, Demurtas J, Veronese N, Ekelund U, Park Y, Yang L. Tai Chi for Chronic Illness Management: Synthesizing Current Evidence from Meta-Analyses of Randomized Controlled Trials. Am J Med. 2021;134:194-205.e12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 22] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 9. | Chen Y, Qin J, Tao L, Liu Z, Huang J, Liu W, Xu Y, Tang Q, Liu Y, Chen Z, Chen S, Liang S, Chen C, Xie J, Liu J, Chen L, Tao J. Effects of Tai Chi Chuan on Cognitive Function in Adults 60 Years or Older With Type 2 Diabetes and Mild Cognitive Impairment in China: A Randomized Clinical Trial. JAMA Netw Open. 2023;6:e237004. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 41] [Article Influence: 20.5] [Reference Citation Analysis (0)] |
| 10. | Zhou Z, Zhou R, Li K, Zhu Y, Zhang Z, Luo Y, Luan R. Effects of tai chi on physiology, balance and quality of life in patients with type 2 diabetes: A systematic review and meta-analysis. J Rehabil Med. 2019;51:405-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 11. | Xia TW, Yang Y, Li WH, Tang ZH, Li ZR, Qiao LJ. Different training durations and styles of tai chi for glucose control in patients with type 2 diabetes: a systematic review and meta-analysis of controlled trials. BMC Complement Altern Med. 2019;19:63. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 12. | Palermi S, Sacco AM, Belviso I, Marino N, Gambardella F, Loiacono C, Sirico F. Effectiveness of Tai Chi on Balance Improvement in Type 2 Diabetes Patients: A Systematic Review and Meta-Analysis. J Aging Phys Act. 2020;28:787-797. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 13. | Qin J, Chen Y, Guo S, You Y, Xu Y, Wu J, Liu Z, Huang J, Chen L, Tao J. Effect of Tai Chi on Quality of Life, Body Mass Index, and Waist-Hip Ratio in Patients With Type 2 Diabetes Mellitus: A Systematic Review and Meta-Analysis. Front Endocrinol (Lausanne). 2020;11:543627. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 14. | Guo S, Xu Y, Qin J, Chen Y, You Y, Tao J, Liu Z, Huang J. Effect of tai chi on glycaemic control, lipid metabolism and body composition in adults with type 2 diabetes: A meta-analysis and systematic review. J Rehabil Med. 2021;53:jrm00165. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 15. | Chen SC, Ueng KC, Lee SH, Sun KT, Lee MC. Effect of t'ai chi exercise on biochemical profiles and oxidative stress indicators in obese patients with type 2 diabetes. J Altern Complement Med. 2010;16:1153-1159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 71] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 16. | Petersen AM, Pedersen BK. The anti-inflammatory effect of exercise. J Appl Physiol (1985). 2005;98:1154-1162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1723] [Cited by in RCA: 1900] [Article Influence: 95.0] [Reference Citation Analysis (0)] |
| 17. | Tan L, Yan W, Yang W, Kamionka A, Lipowski M, Zhao Z, Zhao G. Effect of exercise on inflammatory markers in postmenopausal women with overweight and obesity: A systematic review and meta-analysis. Exp Gerontol. 2023;183:112310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 18. | Shu C, Feng S, Cui Q, Cheng S, Wang Y. Impact of Tai Chi on CRP, TNF-alpha and IL-6 in inflammation: a systematic review and meta-analysis. Ann Palliat Med. 2021;10:7468-7478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 19. | Yeh SH, Chuang H, Lin LW, Hsiao CY, Wang PW, Liu RT, Yang KD. Regular Tai Chi Chuan exercise improves T cell helper function of patients with type 2 diabetes mellitus with an increase in T-bet transcription factor and IL-12 production. Br J Sports Med. 2009;43:845-850. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 55] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 20. | Kasim NF, Veldhuijzen van Zanten J, Aldred S. Tai Chi is an effective form of exercise to reduce markers of frailty in older age. Exp Gerontol. 2020;135:110925. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 28] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 21. | Zhang G, Wang S, Gu Y, Song L, Yu S, Feng X. Tai Chi Improves Coronary Heart Disease Risk by Inactivating MAPK/ERK Pathway through Serum miR-126. Evid Based Complement Alternat Med. 2020;2020:4565438. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 22. | Yang G, Dong Q, Yang H, Wang F, Chen L, Tang J, Huang G, Zhao Y. Changes Observed in Potential Key Candidate Genes of Peripheral Immunity Induced by Tai Chi among Patients with Parkinson's Disease. Genes (Basel). 2022;13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 23. | Hu S, Hu Y, Long P, Li P, Chen P, Wang X. The effect of tai chi intervention on NLRP3 and its related antiviral inflammatory factors in the serum of patients with pre-diabetes. Front Immunol. 2022;13:1026509. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 16] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 24. | Ren H, Collins V, Clarke SJ, Han JS, Lam P, Clay F, Williamson LM, Andy Choo KH. Epigenetic changes in response to tai chi practice: a pilot investigation of DNA methylation marks. Evid Based Complement Alternat Med. 2012;2012:841810. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 36] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 25. | Kong J, Wilson G, Park J, Pereira K, Walpole C, Yeung A. Treating Depression With Tai Chi: State of the Art and Future Perspectives. Front Psychiatry. 2019;10:237. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 43] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 26. | Cole AR, Wijarnpreecha K, Chattipakorn SC, Chattipakorn N. Effects of Tai Chi exercise on heart rate variability. Complement Ther Clin Pract. 2016;23:59-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 27. | Zou L, Sasaki JE, Wei GX, Huang T, Yeung AS, Neto OB, Chen KW, Hui SS. Effects of Mind⁻Body Exercises (Tai Chi/Yoga) on Heart Rate Variability Parameters and Perceived Stress: A Systematic Review with Meta-Analysis of Randomized Controlled Trials. J Clin Med. 2018;7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 160] [Cited by in RCA: 128] [Article Influence: 18.3] [Reference Citation Analysis (0)] |
| 28. | Yeung A, Chan JSM, Cheung JC, Zou L. Qigong and Tai-Chi for Mood Regulation. Focus (Am Psychiatr Publ). 2018;16:40-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 72] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 29. | Hamasaki H. Exercise and gut microbiota: clinical implications for the feasibility of Tai Chi. J Integr Med. 2017;15:270-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 28] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 30. | Virolainen SJ, VonHandorf A, Viel KCMF, Weirauch MT, Kottyan LC. Gene-environment interactions and their impact on human health. Genes Immun. 2023;24:1-11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 81] [Cited by in RCA: 103] [Article Influence: 51.5] [Reference Citation Analysis (0)] |
| 31. | Schellenberg ES, Dryden DM, Vandermeer B, Ha C, Korownyk C. Lifestyle interventions for patients with and at risk for type 2 diabetes: a systematic review and meta-analysis. Ann Intern Med. 2013;159:543-551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 328] [Cited by in RCA: 363] [Article Influence: 30.3] [Reference Citation Analysis (0)] |
| 32. | Zhang Y, Pan XF, Chen J, Xia L, Cao A, Zhang Y, Wang J, Li H, Yang K, Guo K, He M, Pan A. Combined lifestyle factors and risk of incident type 2 diabetes and prognosis among individuals with type 2 diabetes: a systematic review and meta-analysis of prospective cohort studies. Diabetologia. 2020;63:21-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 230] [Cited by in RCA: 211] [Article Influence: 42.2] [Reference Citation Analysis (0)] |
| 33. | Zucatti KP, Teixeira PP, Wayerbacher LF, Piccoli GF, Correia PE, Fonseca NKO, Moresco KS, Guerra BA, Maduré MG, Farenzena LP, Frankenberg AD, Brietzke E, Halpern B, Franco O, Colpani V, Gerchman F. Long-term Effect of Lifestyle Interventions on the Cardiovascular and All-Cause Mortality of Subjects With Prediabetes and Type 2 Diabetes: A Systematic Review and Meta-analysis. Diabetes Care. 2022;45:2787-2795. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 27] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 34. | Peng Y, Liu F, Qiao Y, Wang P, Ma B, Li L, Si C, Wang X, Zhang M, Song F. Association of abnormal bowel health with major chronic diseases and risk of mortality. Ann Epidemiol. 2022;75:39-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 23] [Reference Citation Analysis (0)] |
| 35. | Reynolds AN, Akerman AP, Mann J. Dietary fibre and whole grains in diabetes management: Systematic review and meta-analyses. PLoS Med. 2020;17:e1003053. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 256] [Cited by in RCA: 293] [Article Influence: 58.6] [Reference Citation Analysis (0)] |
| 36. | Hughes LAE, Simons CCJM, van den Brandt PA, van Engeland M, Weijenberg MP. Lifestyle, Diet, and Colorectal Cancer Risk According to (Epi)genetic Instability: Current Evidence and Future Directions of Molecular Pathological Epidemiology. Curr Colorectal Cancer Rep. 2017;13:455-469. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 76] [Cited by in RCA: 92] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 37. | Qi Q, Li J, Yu B, Moon JY, Chai JC, Merino J, Hu J, Ruiz-Canela M, Rebholz C, Wang Z, Usyk M, Chen GC, Porneala BC, Wang W, Nguyen NQ, Feofanova EV, Grove ML, Wang TJ, Gerszten RE, Dupuis J, Salas-Salvadó J, Bao W, Perkins DL, Daviglus ML, Thyagarajan B, Cai J, Wang T, Manson JE, Martínez-González MA, Selvin E, Rexrode KM, Clish CB, Hu FB, Meigs JB, Knight R, Burk RD, Boerwinkle E, Kaplan RC. Host and gut microbial tryptophan metabolism and type 2 diabetes: an integrative analysis of host genetics, diet, gut microbiome and circulating metabolites in cohort studies. Gut. 2022;71:1095-1105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 156] [Article Influence: 52.0] [Reference Citation Analysis (0)] |
| 38. | Ogino S, Nowak JA, Hamada T, Milner DA Jr, Nishihara R. Insights into Pathogenic Interactions Among Environment, Host, and Tumor at the Crossroads of Molecular Pathology and Epidemiology. Annu Rev Pathol. 2019;14:83-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 176] [Article Influence: 29.3] [Reference Citation Analysis (0)] |