Published online Sep 15, 2023. doi: 10.4239/wjd.v14.i9.1403
Peer-review started: June 6, 2023
First decision: June 21, 2023
Revised: June 30, 2023
Accepted: July 18, 2023
Article in press: July 18, 2023
Published online: September 15, 2023
Processing time: 99 Days and 1.6 Hours
Urinary sepsis is frequently seen in patients with diabetes mellitus (DM) complicated with upper urinary tract calculi (UUTCs). Currently, the known risk factors of urinary sepsis are not uniform.
To analyze the risk factors of concurrent urinary sepsis in patients with DM complicated with UUTCs by logistic regression.
We retrospectively analyzed 384 patients with DM complicated with UUTCs treated in People’s Hospital of Jincheng between February 2018 and May 2022. The patients were screened according to the inclusion and exclusion criteria, and 204 patients were enrolled. The patients were assigned to an occurrence group (n = 78) and a nonoccurrence group (n = 126). Logistic regression was adopted to analyze the risk factors for urinary sepsis, and a risk prediction model was established.
Gender, age, history of lumbago and abdominal pain, operation time, urine leukocytes (U-LEU) and urine glucose (U-GLU) were independent risk factors for patients with concurrent urinary sepsis (P < 0.05). Risk score = 0.794 × gender + 0.941 × age + 0.901 × history of lumbago and abdominal pain - 1.071 × operation time + 1.972 × U-LEU + 1.541 × U-GLU. The occurrence group had notably higher risk scores than the nonoccurrence group (P < 0.0001). The area under the curve of risk score for forecasting concurrent urinary sepsis in patients was 0.801, with specificity of 73.07%, sensitivity of 79.36% and Youden index of 52.44%.
Sex, age, history of lumbar and abdominal pain, operation time, ULEU and UGLU are independent risk factors for urogenic sepsis in diabetic patients with UUTC.
Core Tip: This study was to determine risk factors of concurrent urinary sepsis in patients with diabetes mellitus comorbid with upper urinary tract calculi and construct a risk prediction model. Gender, age, history of lumbago and abdominal pain, operation time, urinary leukocytes and urinary glucose were independent risk factors for concurrent urinary sepsis. It is helpful to identify high-risk patients at an early stage and implement active and effective intervention measures to reduce complications and improve the prognosis of patients.
- Citation: Gou JJ, Zhang C, Han HS, Wu HW. Risk factors of concurrent urinary sepsis in patients with diabetes mellitus comorbid with upper urinary tract calculi. World J Diabetes 2023; 14(9): 1403-1411
- URL: https://www.wjgnet.com/1948-9358/full/v14/i9/1403.htm
- DOI: https://dx.doi.org/10.4239/wjd.v14.i9.1403
With the improvement of living standards, the incidence of urinary calculi worldwide is increasing gradually. Its incidence in adults in China is 1%-5%, and upper urinary tract calculi (UUTCs) are a more frequently seen problem[1]. Calculi are caused by several factors, such as socioeconomic status, environmental factors and eating habits[2]. The incidence of calculi in northern and southern areas of China differs, with a high incidence in southern areas (5%-10%)[3]. Other factors such as gender and genetic susceptibility can also affect the occurrence of calculi, and the incidence rate among males is three times that among females[4]. In China, the annual incidence of urinary calculi is 150-200 cases per 100000 people, and approximately 25% of patients need hospitalization and surgical treatment. After treatment, the recurrence rate is high at approximately 50% within 10 years[5].
The urethra connects the urinary system with the outside world, providing a way for bacteria and other pathogens to invade the urinary system[6]. Usually, the flushing action during urination and urethral mucosa form a natural protective barrier to prevent bacteria from remaining, growing and reproducing[7]. However, various factors hinder the defensive function of the urinary system. For example, obstruction can result in stagnant water above the obstruction, making it easier for pathogenic bacteria to invade and colonize the urinary system, giving rise to infection[8]. Without timely intervention, the infection may develop into urinary sepsis or even septic shock, endangering the life of patients.
Sepsis is a serious disease and an acute physical reaction caused by infection, with associated physiological, pathological and biochemical abnormalities[9]. Sepsis is defined as organ dysfunction due to the host’s uncontrolled immune response to infection. Unfortunately, sepsis is a global health threat with high mortality[10]. Without timely treatment, sepsis may develop into septic shock and multiple organ dysfunctions and even cause death[11].
The incidence of diabetes mellitus (DM) is increasing. According to the latest statistics of the International Diabetes Federation, the global prevalence of DM has reached 9.3%. DM can give rise to systemic damage, leading to immune dysfunction and proneness to serious infection[12]. However, currently, the risk factors for concurrent urinary sepsis in patients with UUTCs and DM are still under investigation.
Accordingly, this study aimed to determine the risk factors for concurrent urinary sepsis in patients with DM comorbid with UUTCs to provide a reference for clinical therapy and prevention.
We retrospectively analyzed 384 patients with DM complicated with UUTCs treated in People’s Hospital of Jincheng between February 2018 and May 2022. Inclusion criteria were: (1) Imaging results, such as urinary ultrasound, intravenous urography or abdominal computed tomography, suggested the presence of UUTCs; (2) a clear history of DM that met the guidelines for the diagnosis and treatment of senile DM in China[13]; and (3) a complete medical history and laboratory and imaging data. Exclusion criteria were: (1) Age < 18 years; (2) pregnant women; (3) bilateral UUTCs; (4) hematological disease, immune system disease, or malignant tumors; (5) treated with immunomodulatory drugs; and (6) other primary infection, such as lung or abdominal infection. The 384 patients were screened according to the inclusion and exclusion criteria, and 204 patients were enrolled. According to Guidelines for Emergency Treatment of Sepsis/Septic Shock in China (2018)[14] and the diagnostic criteria for urinary sepsis[14], patients were assigned to an occurrence group (n = 78) and nonoccurrence group (n = 126).
The clinical data were collected through the medical record system of our hospital, including: (1) General information: Gender, age and body mass index; (2) medical history: Lumbago and abdominal pain, hematuria, symptoms of urinary tract irritation, hypertension, and DM; (3) urine examination data: Urinary leukocytes (U-LEU), urinary nitrite (U-NIT), urinary glucose (U-GLU), and urinary occult blood; and (4) imaging examination data: Lateral classification, location, maximum diameter and hydronephrosis of calculi.
We used R language 4.1.1 software (R Foundation for Statistical Computing, Vienna, Austria) for data cleaning and analysis, and constructed a model. Logistic regression was adopted for screening the risk factors, and receiver operating characteristic (ROC) curve was adopted for value verification. This study used Graph Pad Prism 8.0 for data visualization. P < 0.05 indicated a significant difference.
The occurrence and nonoccurrence groups did not differ significantly for hematuria and hypertension (P > 0.05) (Table 1), but they did differ significantly for gender, age, history of lumbago and abdominal pain, symptoms of urinary tract irritation and operation time (P < 0.05) (Table 1).
| Factors | Occurrence group (n = 78) | Nonoccurrence group (n = 126) | χ2 value | P value | |
| Gender | 9.219 | 0.002 | |||
| Male | 30 | 76 | |||
| Female | 48 | 50 | |||
| Age | 5.732 | 0.016 | |||
| ≥ 60 yr | 45 | 51 | |||
| < 60 yr | 33 | 75 | |||
| BMI | 0.292 | 0.588 | |||
| ≥ 25 kg/m2 | 28 | 50 | |||
| < 25 kg/m2 | 50 | 76 | |||
| History of lumbago and abdominal pain | 8.459 | 0.003 | |||
| Yes | 38 | 36 | |||
| No | 40 | 90 | |||
| Hematuria | 0.569 | 0.450 | |||
| Yes | 36 | 65 | |||
| No | 42 | 61 | |||
| Symptoms of urinary tract irritation | 4.036 | 0.044 | |||
| Yes | 60 | 80 | |||
| No | 18 | 46 | |||
| Hypertension | 0.533 | 0.465 | |||
| Yes | 30 | 55 | |||
| No | 48 | 71 | |||
| Operation time | 64.32 ± 15.35 | 59.94 ± 7.04 | 4.662 | 0.001 |
The occurrence and nonoccurrence groups did not differ significantly for urinary occult blood (P > 0.05) (Table 2), but they did differ significantly for U-LEU, U-NIT, and U-GLU (P < 0.01) (Table 2).
| Factors | Occurrence group (n = 78) | Nonoccurrence group (n = 126) | χ2 | P value | |
| Urine occult blood | 1.210 | 0.750 | |||
| - | 18 | 35 | |||
| 1+ | 22 | 28 | |||
| 2+ | 24 | 38 | |||
| 3+ | 14 | 25 | |||
| U-LEU | 15.330 | 0.002 | |||
| - | 4 | 30 | |||
| 1+ | 26 | 38 | |||
| 2+ | 20 | 37 | |||
| 3+ | 28 | 25 | |||
| U-NIT | 12.499 | 0.001 | |||
| - | 33 | 85 | |||
| + | 45 | 41 | |||
| U-GLU | 11.596 | 0.008 | |||
| - | 7 | 33 | |||
| 1+ | 17 | 31 | |||
| 2+ | 40 | 50 | |||
| 3+ | 14 | 12 |
The occurrence and nonoccurrence groups did not differ significantly for lateral classification of calculi, obstruction position, maximum calculi diameter and severity of hydronephrosis (P > 0.05) (Table 3).
| Factors | Occurrence group (n = 78) | Nonoccurrence group (n = 126) | χ2 | P value | |
| Lateral classification of calculi | 1.494 | 0.221 | |||
| Left | 48 | 88 | |||
| Right | 30 | 38 | |||
| Obstruction position | 2.938 | 0.086 | |||
| Ureter | 64 | 90 | |||
| Kidney | 14 | 36 | |||
| Maximum diameter of calculi | 0.048 | 0.825 | |||
| ≥ 20 mm | 39 | 65 | |||
| < 20 mm | 39 | 61 | |||
| Degree of hydronephrosis | 0.400 | 0.526 | |||
| Yes | 11 | 22 | |||
| No | 67 | 104 |
According to the above results, meaningful indicators were assigned (Table 4). The backward logistic regression method was used. Gender, age, history of lumbago and abdominal pain, operation time, U-LEU and U-GLU were independent risk factors for concurrent urinary sepsis (P < 0.05) (Table 5).
| Factors | Assignment |
| Gender | Male = 0, female = 1 |
| Age | ≥ 60 yr = 1, < 60 yr = 0 |
| History of lumbago and abdominal pain | Yes = 1, no = 0 |
| Symptoms of urinary tract irritation | Yes = 1, no = 0 |
| Operation time | ≥ 60 yr = 1, < 60 yr = 0 |
| U-LEU | - = 0, 1 + -3 + = 1 |
| U-NIT | - = 0, + = 1 |
| U-GLU | - = 0, 1 + -3 + = 1 |
| Occurrence | Occurrence group = 1, nonoccurrence group = 0 |
| Factors | β | Standard error | χ2 | P value | OR | 95%CI | |
| Lower limit | Upper limit | ||||||
| Gender | 0.794 | 0.335 | 5.603 | 0.018 | 2.212 | 1.146 | 4.268 |
| Age | 0.941 | 0.346 | 7.408 | 0.006 | 2.563 | 1.301 | 5.047 |
| History of lumbago and abdominal pain | 0.901 | 0.348 | 6.700 | 0.010 | 2.462 | 1.245 | 4.871 |
| Symptoms of urinary tract irritation | 0.628 | 0.379 | 2.753 | 0.097 | 1.875 | 0.892 | 3.939 |
| Operation time | -1.071 | 0.345 | 9.619 | 0.002 | 0.342 | 0.174 | 0.674 |
| U-LEU | 1.972 | 0.602 | 10.725 | 0.001 | 7.182 | 2.207 | 23.373 |
| U-NIT | 0.491 | 0.339 | 2.101 | 0.147 | 1.634 | 0.841 | 3.172 |
| U-GLU | 1.541 | 0.509 | 9.171 | 0.002 | 4.668 | 1.722 | 12.652 |
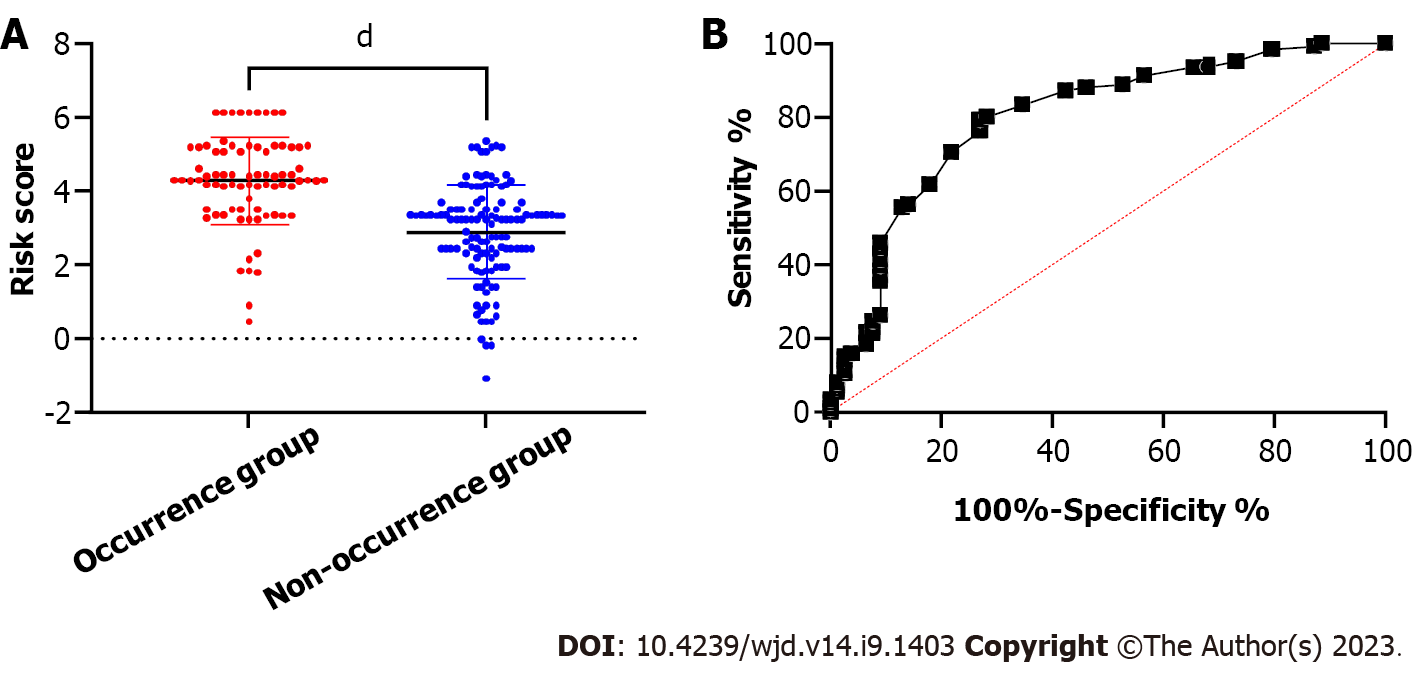
Based on the β coefficient of logistic regression, a risk score for predicting concurrent urinary sepsis was constructed. Risk score = 0.794 × gender + 0.941 × age + 0.901 × history of lumbago and abdominal pain - 1.071 × operation time + 1.972 × U-LEU + 1.541 × U-GLU. According to the comparison results, the occurrence group had notably higher risk scores than the nonoccurrence group (Figure 1A) (P < 0.0001). According to ROC curve analysis, the area under the curve (AUC) of risk score for forecasting concurrent urinary sepsis was 0.801, with specificity of 73.07%, sensitivity of 79.36% and Youden index of 52.44% (Figure 1B).
Urinary sepsis is a dangerous disease. Without timely diagnosis and treatment, its prognosis is unfavorable[15]. There are approximately 2.8 to 9.8 million new cases of urinary sepsis every year, with 1.6 million deaths[16]. Thus, it is important to quickly identify urinary sepsis and provide effective timely treatment. In the guidelines of the European Association of Urology (2017 edition), the definition of urinary sepsis has been updated, which emphasizes that the disease is more serious than uncomplicated infection and may cause organ dysfunction and become life-threatening[17]. Patients with UUTCs and DM are more likely to have urinary sepsis[18]. This is because calculi may trigger infection, and DM makes patients susceptible to various diseases[19]. Therefore, early identification of high-risk factors in these patients and effective intervention have become the focus of many hospitals, which has also been recognized by the World Health Organization.
Our study retrospectively analyzed the risk factors for concurrent urinary sepsis in patients with DM complicated with UUTCs. Gender, age, history of lumbago and abdominal pain, operation time, U-LEU and U-GLU were independent risk factors for concurrent urinary sepsis. The risk of urinary sepsis was about 2.212 times higher in women than in men. Prior research has revealed that women with ureteral calculi or who undergo endoscopic lithotripsy face an independently increased risk of urinary sepsis[20]. However, one other study has revealed no independent correlation between gender and incidence of urinary sepsis[21]. Kumar et al[22] have revealed that the reasons why older women are prone to urinary tract infection and progression to urinary sepsis may include poor perineal hygiene, postmenopausal estrogen deficiency, atrophic vaginitis, uterine and bladder prolapse and the use of vaginal supports.
With the increase of age, the functions of various organs or systems tend to decline, including liver and kidney dysfunction, cardiovascular system defects, and immune system defects[23]. Weakened compensatory ability of organs and systems in patients gives rise to a decline in overall physical function, and patients with DM are more susceptible to infection in such cases[24]. Urinary tract obstruction can easily give rise to secondary infection, systemic inflammatory reaction and even sepsis[25]. In this study, the risk of urinary sepsis in patients aged > 60 years was 2.563 times that in patients < 60 years old, which is in agreement with previous studies.
Similar to prior research, U-LEU was an independent risk factor for UUTCs complicated with urinary sepsis in our study[26]. Some researchers believe that positive urine bacterial culture can more accurately predict the occurrence of urinary sepsis[27]. However, our study did not include the results of urine bacterial culture as a predictor because of the lag time of urine bacterial culture. Usually, it takes 2-3 d or even longer to achieve the results of urine bacterial culture, which leads to a lag in forecasting ability. Therefore, we mainly adopted U-LEU as an indicator, which suggests purulent inflammation in the urinary tract, so it can be used to predict the risk of urinary sepsis.
In patients with DM, the reasons for positive U-GLU may include an increase in blood glucose and decrease in renal glucose threshold. Hyperglycemia causes failure of glucose absorption in the renal tubules, so that glucose is excreted in the urine[18]. Additionally, DM can decrease the ability of renal tubules to absorb glucose, and the glucose in urine cannot be completely reabsorbed[28]. Both of these conditions may lead to positive U-GLU. Positive U-GLU may indicate poor control of DM or diabetic nephropathy. Diabetic nephropathy can easily damage the genitourinary system, causing difficulty in controlling urinary tract infection or recurrence. High concentration of U-GLU provides heat for the growth and metabolism of pathogenic bacteria, which in turn leads to disorder of the body’s defense mechanisms.
In this study, a history of lumbago and abdominal pain had a strong correlation with concurrent urinary sepsis in patients with DM and UUTCs. Lumbago and abdominal pain are frequent symptoms of UUTCs, and one of the manifestations of many patients with urinary sepsis[29]. UUTCs can give rise to urinary retention, bacterial reproduction and infection, increasing the risk of urinary sepsis. DM complicated with UUTCs is a risk factor for urinary sepsis[30]. Patients with DM are often accompanied by various pathophysiological changes such as decreased immune function and metabolic disorder, which can lead to urinary tract infection. Therefore, patients with DM and UUTCs are at higher risk of urinary sepsis.
Long operation time increases the risk of infection. Long-term exposure of wound tissue increases the probability of infection by surrounding flora, and long operation time also increases bleeding and absorption of perfusion fluid, which increase the risk of infection. Urethral obstruction during surgery may also lead to urinary retention, creating favorable conditions for bacterial reproduction[24,31].
We constructed a risk prediction model based on the regression coefficient. A prediction model is a mathematical model that estimates the probability of a specific event or disease according to the combination of multiple risk factors. Through the analysis and assessment of risk factors, a data-based model can be established to help doctors and researchers better understand the risk factors of a disease and develop better prevention and treatment plans. In this study, the occurrence group had notably higher risk scores than the nonoccurrence group, and the AUC of risk score in forecasting urinary sepsis was > 0.8, indicating a high value of the risk model in predicting urinary sepsis.
We analyzed the risk factors for concurrent urinary sepsis in patients with DM complicated with UUTCs by logistic regression model, and successfully constructed a prediction model. However, our study had some limitations. First, there was no external verification of our results. This was because in such a single-center study, it was impossible to establish an effective verification set because of the small number of samples collected. Second, as a single-center research model, its universality needs further verification. Therefore, we hope to carry out prospective research and collect more samples in the future to improve the conclusions.
Gender, age, history of lumbago and abdominal pain, operation time, U-LEU and U-GLU were independent risk factors for concurrent urinary sepsis in patients with DM and UUTCs. It is helpful to identify high-risk patients at an early stage and implement effective intervention measures to reduce complications and improve prognosis.
In patients with diabetes mellitus (DM), long-term hyperglycemia can trigger increases in sugar, protein and other substances in urine, promoting formation of calculi. Urinary calculi can lead to urinary tract infection, renal insufficiency and other complications, and even become life-threatening in severe cases, causing a serious impact on the health of patients with DM. However, at present, the risk factors for urinary sepsis are not uniform. The purpose of this study was to analyze the risk factors for urinary sepsis in patients with DM complicated with upper urinary tract calculi (UUTCs) to provide potential indicators for clinical observation.
It is helpful to identify high-risk patients at an early stage and implement and effective intervention measures by constructing a prediction model, thus reducing complications and improving prognosis.
We successfully predicted high-risk patients by establishing a risk model, which was beneficial to clinical and targeted treatment and prevention.
We constructed a risk model of urinary sepsis by logistic regression model, which provided an observation model for the prediction of high-risk patients.
Although we successfully established a risk model, due to the small number of patients, it was impossible to carry out external verification, so more data are needed to verify whether the model is universal.
Gender, age, history of lumbago and abdominal pain, operation time, and urinary leukocytes and urinary glucose were independent risk factors for concurrent urinary sepsis in patients with DM and UUTCs, and we predicted high-risk patients using a risk model.
The universality of the model could be verified based on multicenter data, and then extended to clinical practice.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Endocrinology and metabolism
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Sachmechi I, United States; Selvin E, United States; Cai L, United States S-Editor: Chen YL L-Editor: A P-Editor: Chen YL
| 1. | Abedi G, Monga M. Flexible Ureteroscopy for Treatment of Upper Urinary Tract Calculus. J Endourol. 2021;35:S56-S61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 2. | Wang X, Zhang Y, Zhao F, Li J, Yian Y. Symptomatic recurrence rate of upper urinary tract calculi in children after endourological procedures. J Pediatr Urol. 2022;18:141.e1-141.e7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 3. | Lou B, Sun Y, Lin J, Yuan Z, He L, Long C, Lin X. Clinical Features of Endogenous Endophthalmitis Secondary to Minimally Invasive Upper Urinary Tract Calculus Removal. Ocul Immunol Inflamm. 2022;30:104-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Prasongwatana V, Bovornpadungkitti S, Chotikawanich E, Pachitrat K, Suwanatrai S, Sriboonlue P. Chemical components of urinary stones according to age and sex of adult patients. J Med Assoc Thai. 2008;91:1589-1594. [PubMed] |
| 5. | Lai L, Zhang W, Zheng F, Wang T, Bai P, Liu Z, Zheng J, Shao Z, Duan B, Wang H, Xing J, Chen H, Huang Y, Chen B. Comparison of the Efficacy of ShuoTong Ureteroscopy and Simple Flexible Ureteroscopy in the Treatment of Unilateral Upper Ureteral Calculi. Front Surg. 2021;8:707022. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 6. | Nicolle LE. Urinary tract infection. Crit Care Clin. 2013;29:699-715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 61] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 7. | Petrosillo N, Granata G, Boyle B, Doyle MM, Pinchera B, Taglietti F. Preventing sepsis development in complicated urinary tract infections. Expert Rev Anti Infect Ther. 2020;18:47-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (2)] |
| 8. | Tan N, Xu L, Wu J. Analysis of the Causes and Preventive Strategies of Urogenic Sepsis after Flexible Ureteroscopic Lithotripsy. Evid Based Complement Alternat Med. 2022;2022:5332101. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 9. | Purcarea A, Sovaila S. Sepsis, a 2020 review for the internist. Rom J Intern Med. 2020;58:129-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 10. | Salomão R, Ferreira BL, Salomão MC, Santos SS, Azevedo LCP, Brunialti MKC. Sepsis: evolving concepts and challenges. Braz J Med Biol Res. 2019;52:e8595. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 138] [Cited by in RCA: 208] [Article Influence: 34.7] [Reference Citation Analysis (0)] |
| 11. | Rello J, Valenzuela-Sánchez F, Ruiz-Rodriguez M, Moyano S. Sepsis: A Review of Advances in Management. Adv Ther. 2017;34:2393-2411. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 163] [Cited by in RCA: 282] [Article Influence: 35.3] [Reference Citation Analysis (0)] |
| 12. | The Prevention of Diabetes Mellitus. JAMA. 2021;325:190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 47] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 13. | Deng MQ, Pan Q, Xiao XH, Guo LX. [Interpretations of guideline for the management of diabetes mellitus in the elderly in China (2021 edition)]. Zhonghua Nei Ke Za Zhi. 2021;60:954-959. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 14. | Napolitano LM. Sepsis 2018: Definitions and Guideline Changes. Surg Infect (Larchmt). 2018;19:117-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 173] [Article Influence: 24.7] [Reference Citation Analysis (0)] |
| 15. | Porat A, Bhutta BS, Kesler S. Urosepsis. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing, 2023. |
| 16. | Guliciuc M, Maier AC, Maier IM, Kraft A, Cucuruzac RR, Marinescu M, Şerban C, Rebegea L, Constantin GB, Firescu D. The Urosepsis-A Literature Review. Medicina (Kaunas). 2021;57. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 17. | Cotterill N, Madersbacher H, Wyndaele JJ, Apostolidis A, Drake MJ, Gajewski J, Heesakkers J, Panicker J, Radziszewski P, Sakakibara R, Sievert KD, Hamid R, Kessler TM, Emmanuel A. Neurogenic bowel dysfunction: Clinical management recommendations of the Neurologic Incontinence Committee of the Fifth International Consultation on Incontinence 2013. Neurourol Urodyn. 2018;37:46-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 41] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 18. | Hong X, Liu G, Chi Z, Yang T, Zhang Y. Predictive model for urosepsis in patients with Upper Urinary Tract Calculi based on ultrasonography and urinalysis using artificial intelligence learning. Int Braz J Urol. 2023;49:221-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 19. | Sabih A, Leslie SW. Complicated Urinary Tract Infections. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing, 2023. |
| 20. | Liu J, Yang Q, Lan J, Hong Y, Huang X, Yang B. Risk factors and prediction model of urosepsis in patients with diabetes after percutaneous nephrolithotomy. BMC Urol. 2021;21:74. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 21. | Kino M, Hayashi T, Hino D, Nakada T, Kitoh H, Akakura K. Patients' poor performance status is an independent risk factor for urosepsis induced by kidney and ureteral stones. Urolithiasis. 2021;49:477-484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 22. | Kumar S, Bag S, Ganesamoni R, Mandal AK, Taneja N, Singh SK. Risk factors for urosepsis following percutaneous nephrolithotomy: role of 1 week of nitrofurantoin in reducing the risk of urosepsis. Urol Res. 2012;40:79-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 37] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 23. | Cao JD, Wang ZC, Wang YL, Li HC, Gu CM, Bai ZG, Chen ZQ, Wang SS, Xiang ST. Risk factors for progression of Urolith Associated with Obstructive Urosepsis to severe sepsis or septic shock. BMC Urol. 2022;22:46. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 24. | Bhojani N, Miller LE, Bhattacharyya S, Cutone B, Chew BH. Risk Factors for Urosepsis After Ureteroscopy for Stone Disease: A Systematic Review with Meta-Analysis. J Endourol. 2021;35:991-1000. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 74] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 25. | Chugh S, Pietropaolo A, Montanari E, Sarica K, Somani BK. Predictors of Urinary Infections and Urosepsis After Ureteroscopy for Stone Disease: a Systematic Review from EAU Section of Urolithiasis (EULIS). Curr Urol Rep. 2020;21:16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 81] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 26. | Amier Y, Zhang Y, Zhang J, Yao W, Wang S, Wei C, Yu X. Analysis of Preoperative Risk Factors for Postoperative Urosepsis After Mini-Percutaneous Nephrolithotomy in Patients with Large Kidney Stones. J Endourol. 2022;36:292-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 27. | Zhu Z, Cui Y, Zeng H, Li Y, Zeng F, Chen Z, Hequn C. The evaluation of early predictive factors for urosepsis in patients with negative preoperative urine culture following mini-percutaneous nephrolithotomy. World J Urol. 2020;38:2629-2636. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 28. | Sun L, Diao X, Gang X, Lv Y, Zhao X, Yang S, Gao Y, Wang G. Risk Factors for Cognitive Impairment in Patients with Type 2 Diabetes. J Diabetes Res. 2020;2020:4591938. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 46] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 29. | Wang S, Yuan P, Peng E, Xia D, Xu H, Wang S, Ye Z, Chen Z. Risk Factors for Urosepsis after Minimally Invasive Percutaneous Nephrolithotomy in Patients with Preoperative Urinary Tract Infection. Biomed Res Int. 2020;2020:1354672. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 30. | Liang X, Huang J, Xing M, He L, Zhu X, Weng Y, Guo Q, Zou W. Risk factors and outcomes of urosepsis in patients with calculous pyonephrosis receiving surgical intervention: a single-center retrospective study. BMC Anesthesiol. 2019;19:61. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 31. | Zhu H, Liu B, Karagöz MA, Yue G, Lei Y, Dou S, Xu Z, Liu Y. Reasons and risk factors for delayed discharge after day-surgery percutaneous nephrolithotomy. BMC Urol. 2022;22:209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |