Published online Aug 15, 2023. doi: 10.4239/wjd.v14.i8.1194
Peer-review started: February 3, 2023
First decision: March 1, 2023
Revised: March 9, 2023
Accepted: June 21, 2023
Article in press: June 21, 2023
Published online: August 15, 2023
Processing time: 188 Days and 19.6 Hours
This review describes the prevalence, incidence, and demographics of children and young people (CYP) with type 1 diabetes in England and Wales using data from the United Kingdom National Paediatric Diabetes Audit (NPDA) and has almost 100% submission from all paediatric diabetes centres annually. It is a powerful benchmarking tool and is an essential part of a long-term quality improvement programme for CYP with diabetes. Clinical characteristics of this population by age, insulin regimen, complication rates, health inequalities, access to diabetes technology, socioeconomic deprivation and glycaemic outcomes over the past decade is described in the review. The NPDA for England and Wales is commissioned by the United Kingdom Healthcare Quality Improvement Partnership as part of the National Clinical Audit for the United Kingdom National Service Framework for Diabetes. The rising incidence of Type 1 diabetes is evidenced in the past decade. Reduction in national median glycated hemoglobin for CYP with diabetes is observed over the last 10 years and the improvement sustained by various initiatives and quality improvement pro-grammes implemented with universal health coverage.
Core Tip: This review describes the prevalence, incidence and demographics of children and young people (CYP) with type 1 diabetes in England and Wales using data from the United Kingdom National Paediatric Diabetes Audit. Reduction in national median glycated hemoglobin for CYP with diabetes is seen over the last 10 years and sustained by various initiatives and quality improvement programmes implemented with universal health coverage.
- Citation: Ng SM, Soni A. Ten-year review of trends in children with type 1 diabetes in England and Wales. World J Diabetes 2023; 14(8): 1194-1201
- URL: https://www.wjgnet.com/1948-9358/full/v14/i8/1194.htm
- DOI: https://dx.doi.org/10.4239/wjd.v14.i8.1194
Type 1 diabetes is a chronic condition and represent the most common type of diabetes in children and young people (CYP). International epidemiology reported that there has been a significant rise in the diagnosis of type 1 diabetes in CYP in the past decade with an estimated incidence of approximately 1 in every 1000 children[1]. Globally, diabetes is reported to affect 1.5 million deaths due to short and long term complications. However, there is currently no accurate epidemiological data on the prevalence or incidence of Type 1 diabetes in many countries worldwide, particularly lacking in low-middle-income countries[2]. The United Kingdom has one of the highest prevalence of CYP with type 1 diabetes in Western Europe and it has an estimated incidence rate of 193.8 per 100000[3].
In the United Kingdom, there are approximately 400000 people diagnosed with type 1 diabetes, with 30000 CYP from 0 to of 18 years living with Type 1 diabetes[1]. The International Diabetes Federation Diabetes Atlas 9th edition reported that an estimated 600000 CYP with Type 1 diabetes are under 15 years of age worldwide[4-6]. A recent paper based on the discrete-time cohort-level Markov illness–death model, estimates that worldwide prevalence of type 1 diabetes is substantial and is growing[2].
The United Kingdom National Paediatric Diabetes Audit (NPDA) 2020/2021 in England and Wales reported approximately 30000 CYP with Type 1 diabetes and 600 CYP with type 2 Diabetes[7]. The reported prevalence rate of Type 1 diabetes in England and Wales was 204.5 per 100000 population in the United Kingdom. The NPDA 2019/2020 audit reported an incidence of 2900 CYP diagnosed with Type 1 diabetes, of whom almost 3000 CYP (95.3%) were aged between 0 and 15 years. In 2020/2021, there was an increase in number of both girls and boys diagnosed with Type 1 diabetes (27.4% and 12.6% increase in boys and girls respectively). The seasonal pattern of new diagnoses of type 1 diabetes mellitus (T1DM) was also disrupted in 2020/2021. Previously there had been a consistent pattern of new diagnoses of Type 1 amongst CYP with a spike in new diagnoses during winter months and fall in the summer. This is a well-known phenomenon in other countries with high incidence of diabetes[8]. The reason for this is unclear but it has been suggested that this could be due to increase in viral illnesses during winter months[7]. This pattern of new diagnoses was disrupted in 2020/2021 and reason for this is not known. One could attribute this to coronavirus disease 2019 (COVID-19) pandemic. Efforts to control COVID-19 such as lockdowns, social isolation led to reduction in common childhood viral illnesses[9-11].
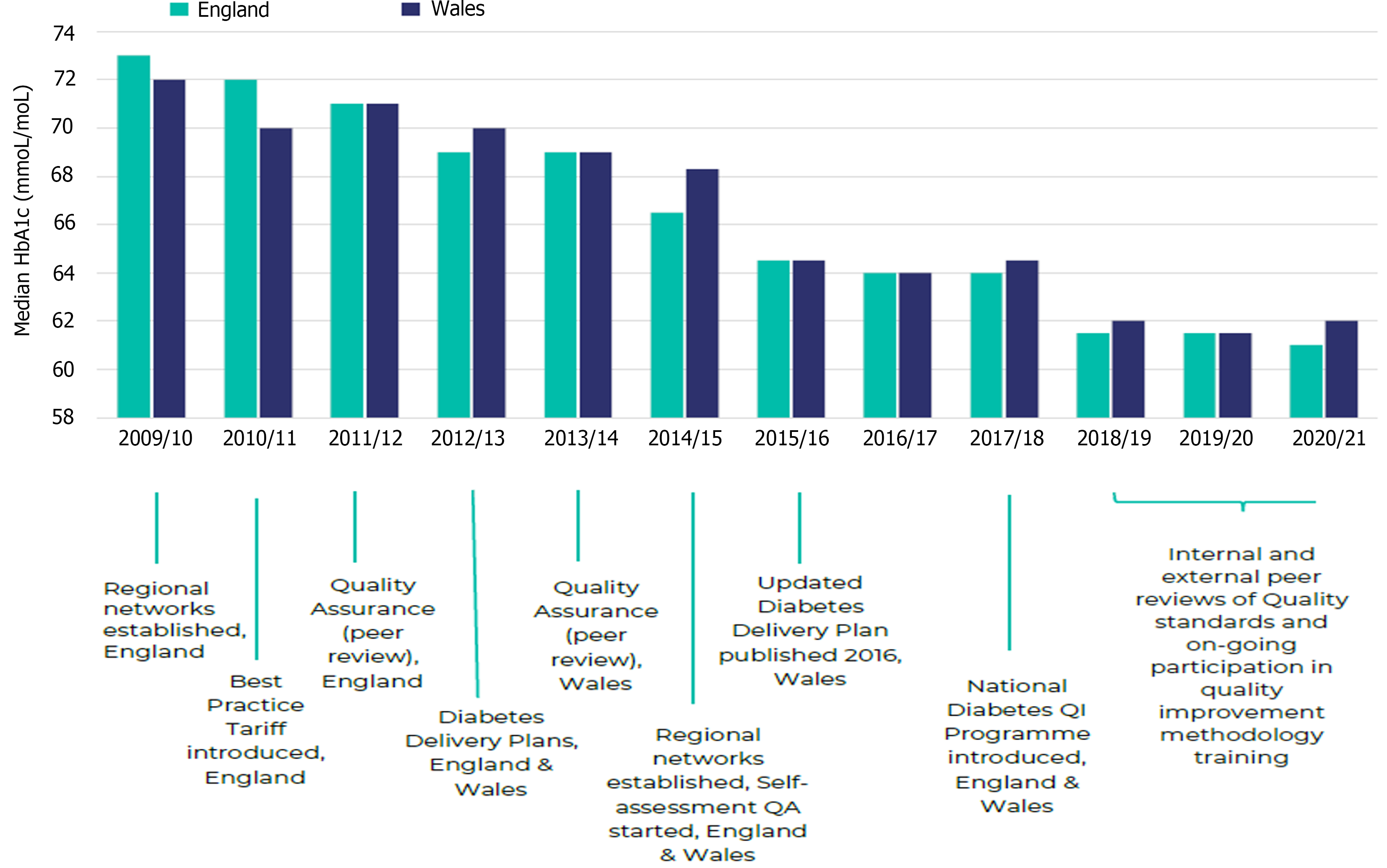
Glycated hemoglobin (HbA1c) is a marker for glycaemic control over preceding 2-3 mo. The Diabetes and Complications Trial (DCCT) trial has shown that intensive diabetes management and good glycaemic control lower the risk of developing microvascular complications and early mortality in the future[12]. Data from NPDA have shown consistent year on year improvements in HbA1c[5]. Median HbA1c in England has fallen from 73 mmol/mol in 2009/2010 to 61 mmol/mol 2020/2021. Similar trend has been noticed in Wales where HbA1c fell from 72 mmol/mol to 62 mmol/mol over the same period (Figure 1).
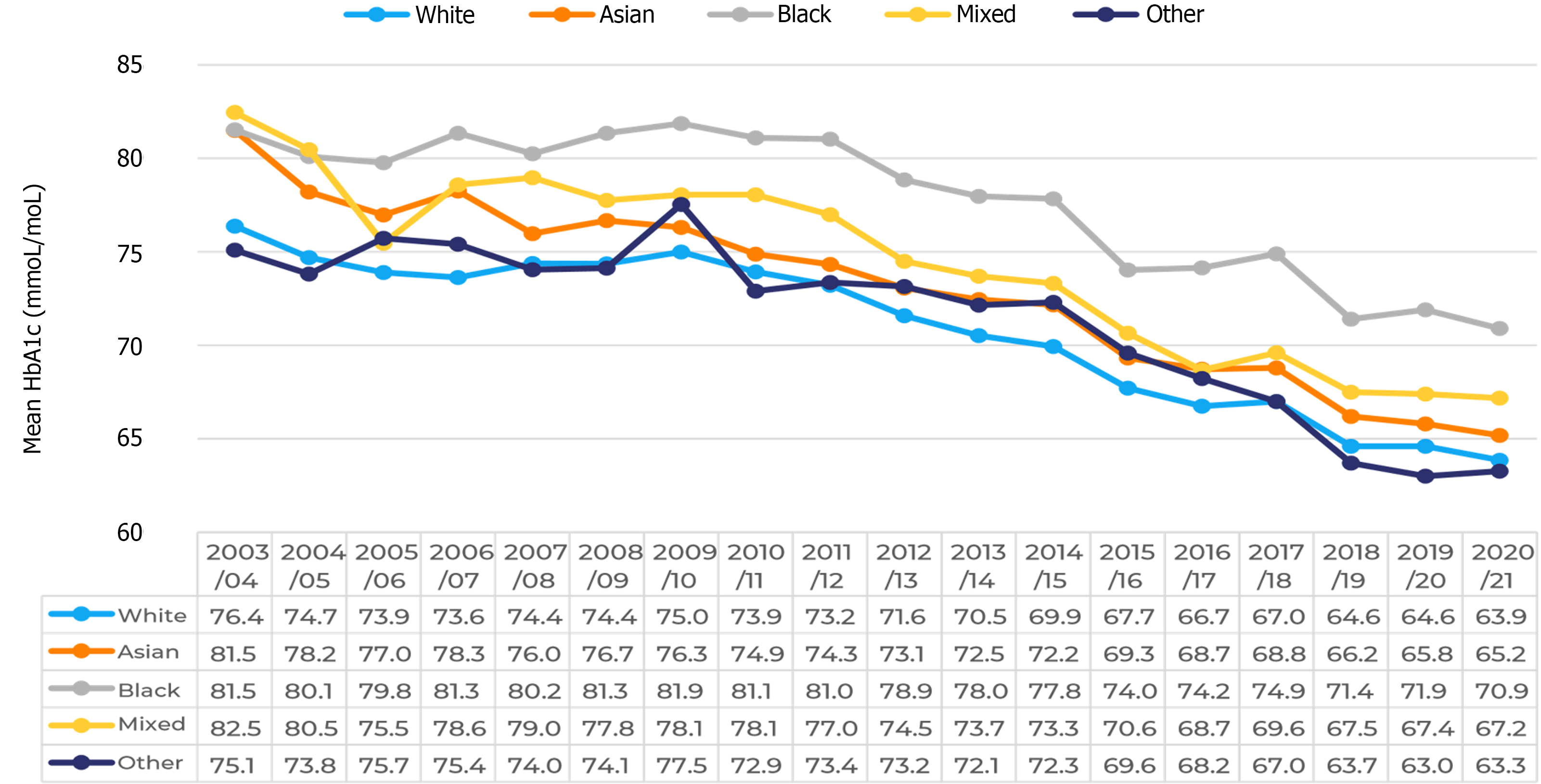
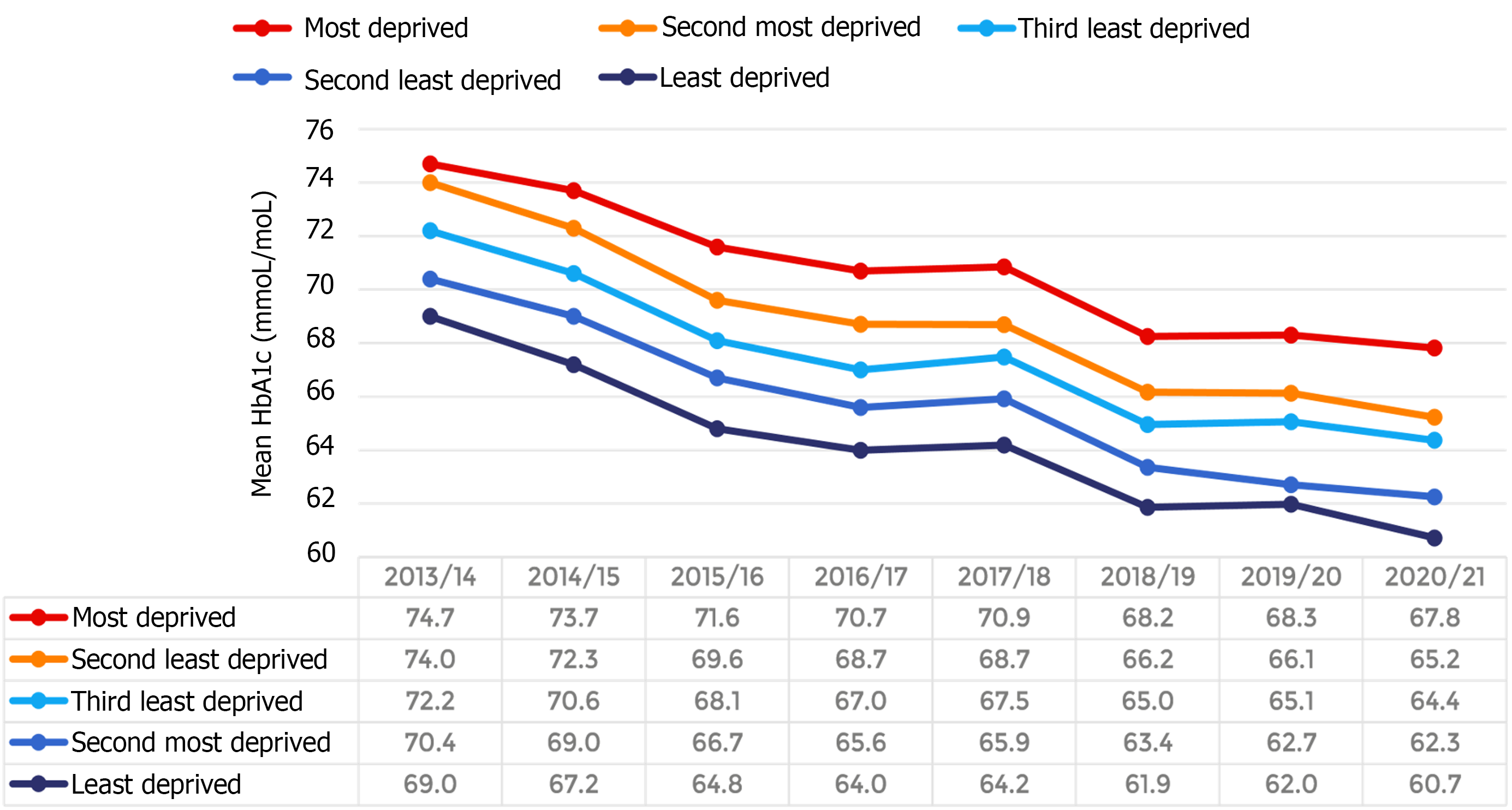
In 2015, the National Institute for Health and Care Excellence (NICE) recommended a target HbA1c of 48 mmol/mol or less to improve the diabetes management[13]. This led to updated diabetes delivery plan in Wales[14]. Prior to that best practice tariff (BPT) was introduced in England in 2012. Peer review (Quality assurance) was introduced at the back of BPT to support the paediatric diabetes units in fulfilling the criteria as set out in BPT. Other national initiatives such as the Royal College of Paediatrics and Child Health Quality improvement programme have been introduced to help achieve the target HbA1c[15. This QI collaborative supported diabetes teams with tools to identify and deliver their own initiatives that are relevant to the needs of the CYP and their families that they care for locally. Although the overall HbA1c trend has been downwards amongst the CYP with T1DM, there have been consistent differences in outcomes between different ethnic backgrounds. Those from white ethnicity achieve lower average HbA1c compared to those from black ethnicity and this trend is apparent year on year[7] (Figure 2). The NPDA showed a significant relationship between HbA1c and deprivation. Those living in deprived areas tend to have a higher HbA1c (Figure 3). However, this trend has not been noticed in CYP of black ethnicity. Average HbA1c for CYP from black ethnicity living in least deprived areas is similar to those from white ethnicity in the most deprived.
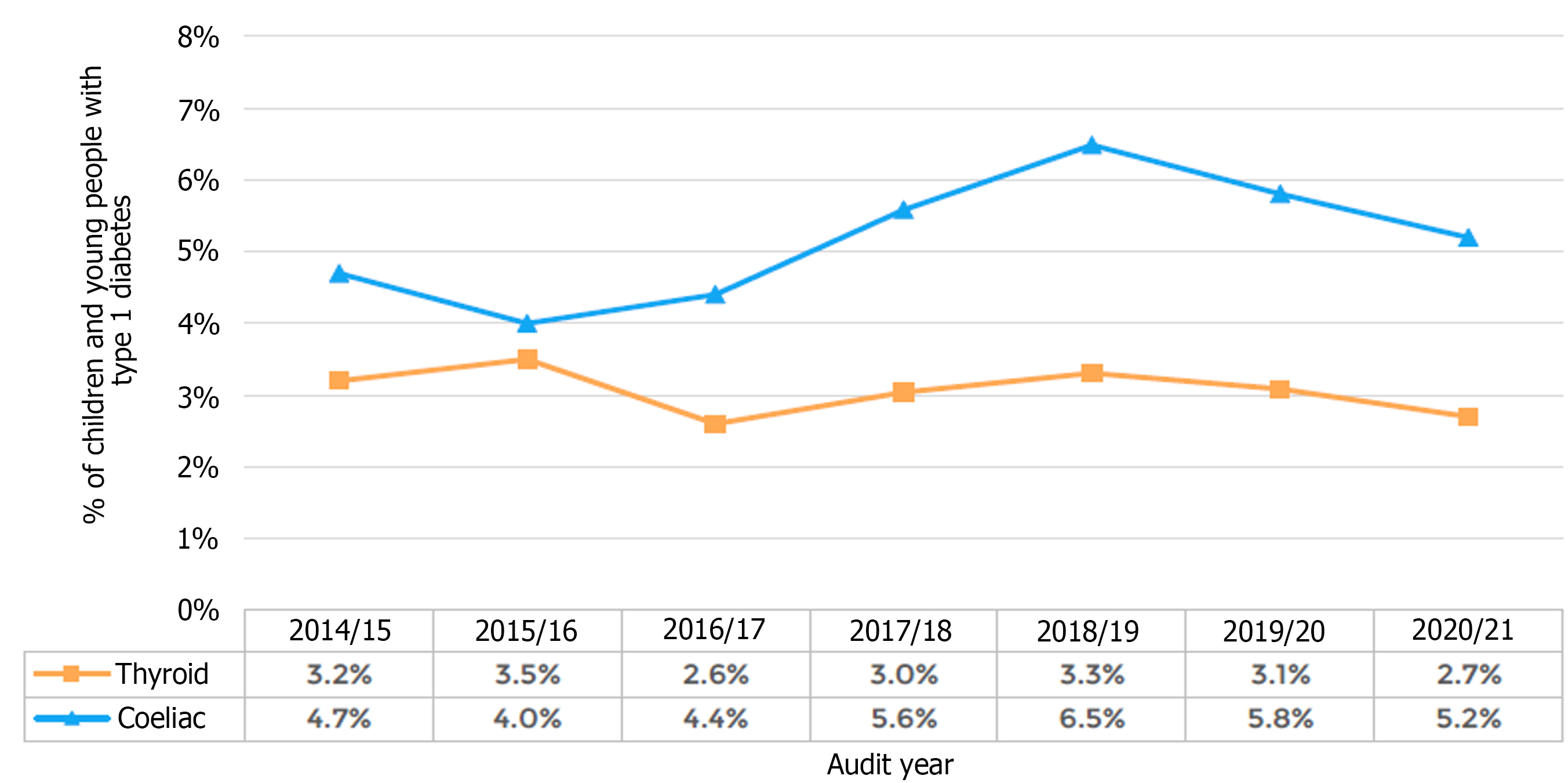
CYP with diabetes are at increased risk of diabetic nephropathy and retinopathy. All CYP with Type 1 diabetes are screened for albuminuria after 12 years of age since NICE made that recommendation in 2015[13]. 10.3% of CYP were recorded as having micro or macroalbuminuria. This number has been static since 2015/2016[7,14]. Across the audit year, there has been no significant changes in the presence of albuminuria associated with duration of diabetes. CYP above 12 years of age get retinopathy screening annually. But the interval for screening changed for many in 2020/2021. Many screening services were advised to screen biennially unless an abnormal result was identified previously. Almost 25% of CYP with T1DM who were eligible for eye screening were screened in 2020/2021 compared to 75% in 2019/2020. The NPDA records eye screening as abnormal or normal. It does not differentiate between the grade of retinopathy. In 2020/2021, 16.9% of those who were screened had an abnormal result, this number has varied between 12%-15% since 2015/2016. CYP with T1DM are more likely to develop other autoimmune conditions. They are annually screened for thyroid and coeliac disease. Two-point-seven percent of screened children had thyroid disease and 5.2% were positive for coeliac in 2020/2. Figure 4 shows the longitudinal trend of% of children with thyroid and coeliac disease from 2015/2016- 2020/2021.
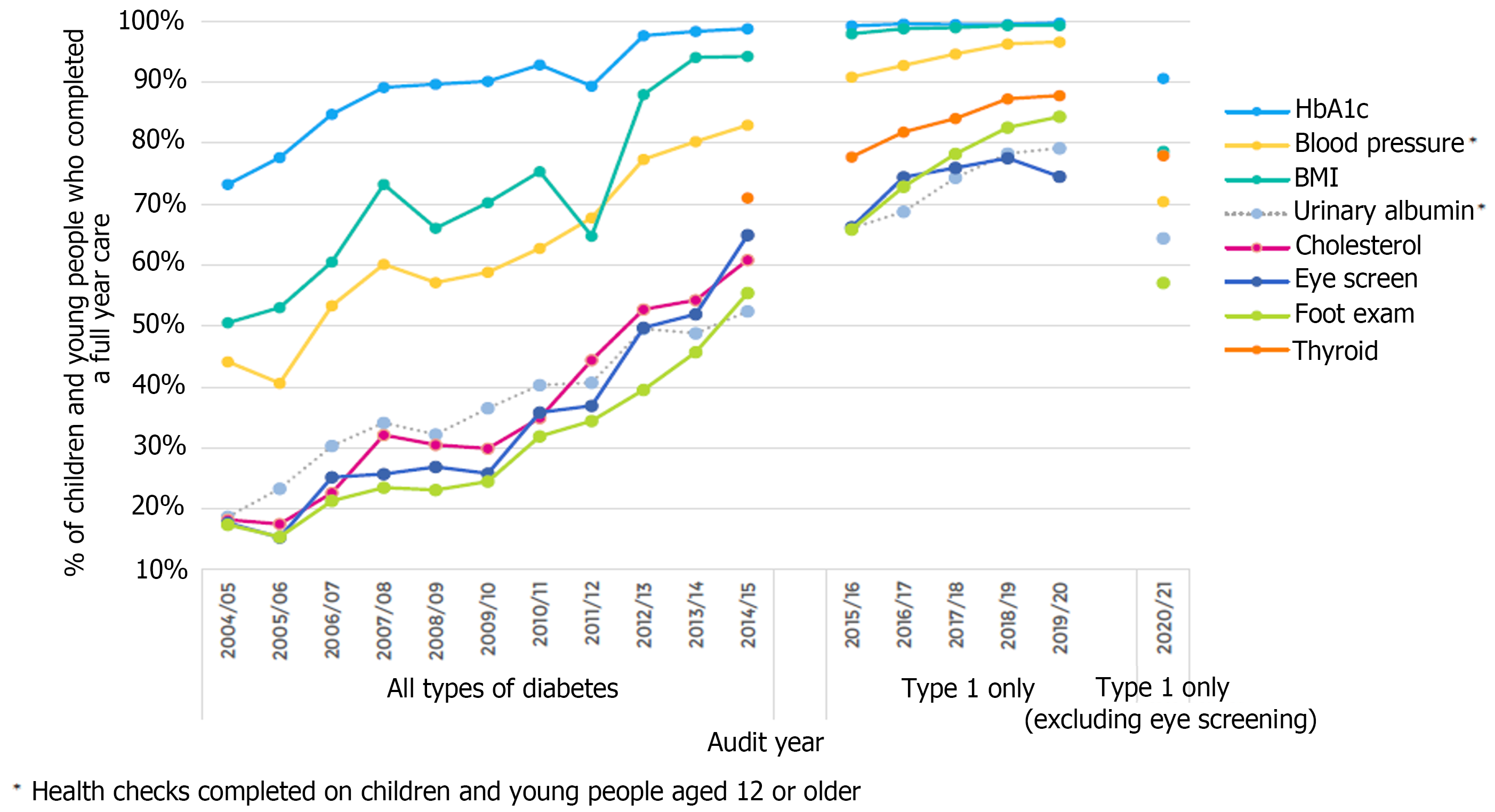
NICE recommends 7 key health check that should be performed annually[13]. HbA1c (4 readings a year), height and weight for all CYP with T1DM. Thyroid function tests to be undertaken every year for all CYP. After 12 years of age, CYP with T1DM should get urinary albumin, blood pressure, retinopathy screen and foot examination. However, there were disruptions to retinopathy screening in 2020/2021[7]. Retinopathy screening was reduced from annually to biennially unless there was a previous abnormal result. There have been an improvement in completion of key health checks over the last 10 years. The completion rates for 2020/2021 reduced due to cessation of face to face clinic due the COVID-19 pandemic. Figure 5 shows the trend improvement in completion of all key processes over the years. There was a large difference amongst various diabetes units’ ability in completing key health check in 2020/2021. Similar trends have been noticed in previous audit years.
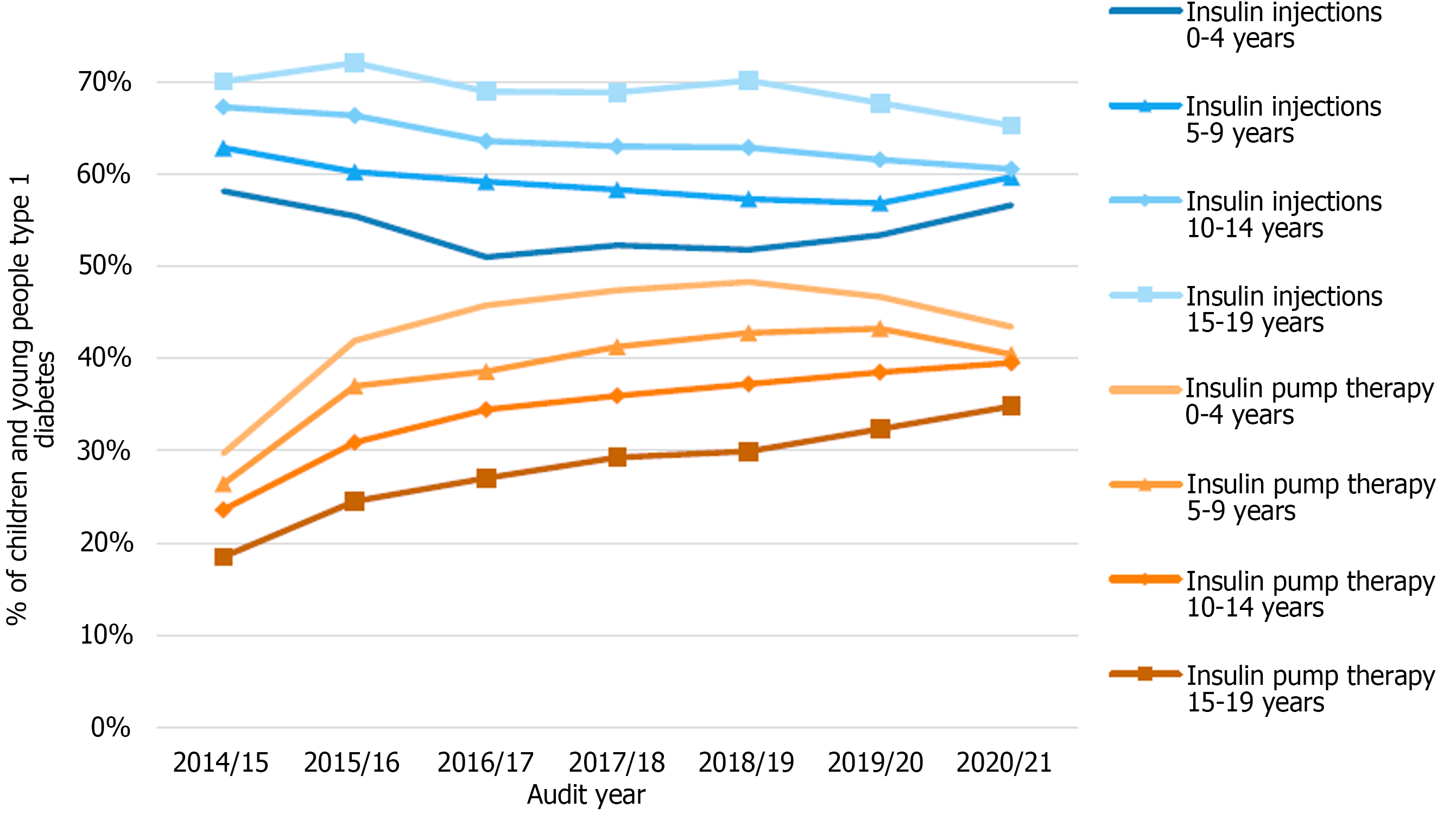
In 2020/2021, 38.5% of CYP with T1DM in England and Wales were using an insulin pump to manage their diabetes[7]. This has increased from 28.1% in 2015/2016. In 2020/2021, 59.1% were on multiple daily injection and only 2.4% were on one-three injections a day. The number of CYP using pump therapy have steadily increased over the years. But this trend has reversed amongst 0-9 years old since 2018/2019 (Figure 6). CYP are more likely to be on insulin injections in the first year of their diagnosis compared to those who were 5-9 years in to diagnosis in 2020/2021. The percentage of those using insulin pumps in 1st year of their diagnosis reduced in 2020/2021 to 13.9% from 4.8% in the previous year. It could be a reflection of changes in care provision due to pandemic as this number has been steadily increasing since 2016/2017. There remains a larger gap in insulin pump usage and insulin injections amongst those CYP living in most deprived areas. In 2020/2021 the gap in number of CYP on insulin pump therapy in those living in the most and least deprived areas was 32.5% compared to 44.0%, respectively (a difference of 11.5 percentage points), which had widened from 2014/2015, when it was 18.4% vs 26.3% (a difference of 7.9 percentage points).
Similar differences in the use of real time continuous glucose monitor (rtCGM) have been identified. Over last few years, increased use of rtCGM has been noticed but the gap in its usage for most and least deprived has widened with time. CYP from least deprived quintiles are more likely to use rtCGM. This is true across most ethnic groups but black CYP typically have lower use of rtCGM which was irrespective of their deprivation status[16]. NPDA data[7] has also reported that CYP who were using rtCGM technology were more likely to attain target HbA1c levels compared to those who were not on trCGM. Similarly, pump users were more likely to be using rtCGM compared to those on insulin injections.
In England and Wales, the existence of universal health coverage and national quality initiatives as well as the formation of 10 Diabetes Regional Networks geographically situated in former Strategic Regional Health Authorities has resulted in improved diabetes health outcomes and diabetes units’ increasing participation in the NPDA[7]. As a result, the NPDA has allowed a country-wide data monitoring and benchmarking of diabetes outcomes and its services within and between regions. The ultimate aim of such national quality initiatives is to improve diabetes care and quality, and to remove health inequalities of service provision within and between regions. The past decade have seen a move towards intensification of insulin therapy, and increasing use of diabetes technologies such as continuous subcutaneous insulin infusions and rtCGM. The BPT was introduced in England to increase the funding provisions per year of care for paediatric diabetes services, with the aim to enhance the quality of diabetes care and improve the health outcomes for CYP with diabetes[17]. Participation in the NPDA is one of the key requirements for obtaining the BPT and data for individual centres are further tracked and utilized as part of a ‘peer review’ quality assurance programme.
The NPDA report[7] has shown that while there is an increasing trend in insulin pump usage compared to injections in all areas of deprivation, the gap between insulin pump usage and rtCGM usage amongst CYP living in the most and least deprived areas, and between CYP of White ethnicity and Black ethnicity has further widened year-on-year over the past 6 years. Table 1 shows the graphs of CYP with Type 1 diabetes by deprivation areas which are derived by postcode-matching to the English (IMD, 2016) and Welsh (WIMD, 2015) indices of multiple deprivation data. The proportion of CYP with Type 1 diabetes living in the most deprived quintile was slightly higher, and this has been a trend across the years.
| Deprivation quintile | Total | % of cohort | % of total with known deprivation | % of children and young people aged 0-19 yr old (England and Wales) |
| Most deprived | 6786 | 22.70% | 22.70% | 23.70% |
| Second most deprived | 6069 | 20.30% | 20.30% | 20.70% |
| Third least deprived | 5659 | 18.90% | 19.00% | 19.00% |
| Second least deprived | 5682 | 19.00% | 19.00% | 18.10% |
| Least deprived | 5665 | 19.00% | 19.00% | 18.50% |
| Missing | 31 | 0.10% | - | - |
There remains a persistent difference in HbA1c health outcomes achieved by Paediatric Diabetes centres across England and Wales even after patient characteristics have been accounted for in the last decade. In addition, there is clear evidence that there are inequalities on access to use of diabetes technologies such as insulin pump and rtCGM which has been shown to have the potential to impact positively on of glycaemic control, fear of hypoglycemia and quality of life[16].
Research has shown that healthcare professionals can hold strong and sometimes incorrect views about the kinds of individuals who will be the ‘best candidates’ for, and make the best use of, diabetes technologies. Such views may influence who healthcare professionals offer technologies to and/or how they present the benefits/burdens of the technology. Studies have also shown that other factors, such as lack of availability of funding and staff with relevant clinical training, can also influence who does/does not get given opportunities to use new diabetes technologies[18,19].
Similar trends of health inequalities and racial-ethnic disparities in diabetes outcomes and management are reported from the United States Type 1 Diabetes Exchange National Registry which reported that ethnic minority young people had significantly worse diabetes health outcomes and were also prescribed less advanced diabetes technologies, while carers’ perceptions of cost and healthcare providers’ perception bias of family competence cited as reasons to such variations[20-22].
We thank Holly Robinson and the National Paediatric Diabetes United Kingdom NPDA, Royal College of Paediatrics and Child Health and Healthcare Quality Improvement Partnership for the reporting data and the figures.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Professor Sze May Ng, OBE is Chair of the UK Association of Children’s Diabetes Clinicians; Chair of the UK NIHR Clinical research Group and Diabetes Research Steering Group for Children and Young People; Officer for Research for the Royal College of Paediatrics; Chair of the European Society of Paediatric Endocrinology (ESPE) E-learning and on the International Society of Pediatric and Adolescent Diabetes (ISPAD) advisory council.
Specialty type: Endocrinology and metabolism
Country/Territory of origin: United Kingdom
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Belosludtseva NV, Russia; Islam MS, South Africa; Ng HY, China S-Editor: Li L L-Editor: A P-Editor: Cai YX
| 1. | Chan JCN, Lim LL, Wareham NJ, Shaw JE, Orchard TJ, Zhang P, Lau ESH, Eliasson B, Kong APS, Ezzati M, Aguilar-Salinas CA, McGill M, Levitt NS, Ning G, So WY, Adams J, Bracco P, Forouhi NG, Gregory GA, Guo J, Hua X, Klatman EL, Magliano DJ, Ng BP, Ogilvie D, Panter J, Pavkov M, Shao H, Unwin N, White M, Wou C, Ma RCW, Schmidt MI, Ramachandran A, Seino Y, Bennett PH, Oldenburg B, Gagliardino JJ, Luk AOY, Clarke PM, Ogle GD, Davies MJ, Holman RR, Gregg EW. The Lancet Commission on diabetes: using data to transform diabetes care and patient lives. Lancet. 2021;396:2019-2082. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 489] [Cited by in RCA: 427] [Article Influence: 106.8] [Reference Citation Analysis (0)] |
| 2. | Gregory GA, Robinson TIG, Linklater SE, Wang F, Colagiuri S, de Beaufort C, Donaghue KC; International Diabetes Federation Diabetes Atlas Type 1 Diabetes in Adults Special Interest Group, Magliano DJ, Maniam J, Orchard TJ, Rai P, Ogle GD. Global incidence, prevalence, and mortality of type 1 diabetes in 2021 with projection to 2040: a modelling study. Lancet Diabetes Endocrinol. 2022;10:741-760. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 498] [Article Influence: 166.0] [Reference Citation Analysis (0)] |
| 3. | Iacobucci G. UK has fifth highest rate of type 1 diabetes in children, new figures show. BMJ. 2013;346:f22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | International Diabetes Federation. International Diabetes Federation. [cited 23 May 2023]. Available from: https://idf.org/. |
| 5. | IDF Diabetes Atlas Group. Update of mortality attributable to diabetes for the IDF Diabetes Atlas: Estimates for the year 2013. Diabetes Res Clin Pract. 2015;109:461-465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 177] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 6. | IDF Diabetes Atlas. IDF Diabetes Atlas 10th Ed 2021. 2020. [cited 23 May 2023]. Available from: https://diabetesatlas.org/atlas/tenth-edition/. |
| 7. | Royal College of Paediatrics and Child Health. NPDA National report 2020/21: Care processes and outcomes Appendix 1: Full audit analysis. In: health RCoPac. 2022. [cited 23 May 2023]. Available from: https://www.rcpch.ac.uk/sites/default/files/2022-04/NPDA%20report%202020-21%20Appendix%201%20Full%20audit%20analysis_0.pdf. |
| 8. | Turtinen M, Härkönen T, Ilonen J, Parkkola A, Knip M; Finnish Pediatric Diabetes Register. Seasonality in the manifestation of type 1 diabetes varies according to age at diagnosis in Finnish children. Acta Paediatr. 2022;111:1061-1069. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 9. | Principi N, Berioli MG, Bianchini S, Esposito S. Type 1 diabetes and viral infections: What is the relationship? J Clin Virol. 2017;96:26-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 40] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 10. | Kruizinga MD, Peeters D, van Veen M, van Houten M, Wieringa J, Noordzij JG, Bekhof J, Tramper-Stranders G, Vet NJ, Driessen GJA. The impact of lockdown on pediatric ED visits and hospital admissions during the COVID19 pandemic: a multicenter analysis and review of the literature. Eur J Pediatr. 2021;180:2271-2279. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 149] [Cited by in RCA: 137] [Article Influence: 34.3] [Reference Citation Analysis (0)] |
| 11. | Kuitunen I, Artama M, Mäkelä L, Backman K, Heiskanen-Kosma T, Renko M. Effect of Social Distancing Due to the COVID-19 Pandemic on the Incidence of Viral Respiratory Tract Infections in Children in Finland During Early 2020. Pediatr Infect Dis J. 2020;39:e423-e427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 228] [Article Influence: 45.6] [Reference Citation Analysis (0)] |
| 12. | Nathan DM, Genuth S, Lachin J, Cleary P, Crofford O, Davis M, Rand L, Siebert C; Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329:977-986. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17510] [Cited by in RCA: 16273] [Article Influence: 508.5] [Reference Citation Analysis (3)] |
| 13. | National Collaborating Centre for Women's and Children's Health (UK). Diabetes (Type 1 and Type 2) in Children and Young People: Diagnosis and Management. London: National Institute for Health and Care Excellence (UK); 2015 Aug. [PubMed] |
| 14. | Llywodraeth Cymru Welsh Government. Diabetes Delivery Plan for Wales 2016-2020. Welsh: Government W. Dec 2016. [cited 23 May 2023]. Available from: https://www.gov.wales/sites/default/files/publications/2018-12/diabetes-delivery-plan-2016-to-2020.pdf. |
| 15. | National Diabetes Quality Programme. Secondary National Diabetes Quality Programme. [cited 23 May 2023]. Available from: https://www.rcpch.ac.uk/work-we-do/QI-patient-safety/diabetes-quality-programme. |
| 16. | Ng SM, Evans ML. Widening health inequalities related to type 1 diabetes care in children and young people in the UK: A time to act now. Diabet Med. 2021;38:e14620.. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 17. | Randell T. Developing a Best Practice Tariff in paediatric diabetes. Practical Diabetes. 2012;29:176-177a. [RCA] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 18. | Ng SM, Moore HS, Clemente MF, Pintus D, Soni A. Continuous Glucose Monitoring in Children with Type 1 Diabetes Improves Well-Being, Alleviates Worry and Fear of Hypoglycemia. Diabetes Technol Ther. 2019;21:133-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 31] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 19. | Lawton J, Kirkham J, Rankin D, White DA, Elliott J, Jaap A, Smithson WH, Heller S; REPOSE Group. Who gains clinical benefit from using insulin pump therapy? A qualitative study of the perceptions and views of health professionals involved in the Relative Effectiveness of Pumps over MDI and Structured Education (REPOSE) trial. Diabet Med. 2016;33:243-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 53] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 20. | Lawton J, Kimbell B, Rankin D, Ashcroft NL, Varghese L, Allen JM, Boughton CK, Campbell F, Randell T, Besser REJ, Trevelyan N, Hovorka R; CLOuD Consortium. Health professionals' views about who would benefit from using a closed-loop system: a qualitative study. Diabet Med. 2020;37:1030-1037. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 39] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 21. | Willi SM, Miller KM, DiMeglio LA, Klingensmith GJ, Simmons JH, Tamborlane WV, Nadeau KJ, Kittelsrud JM, Huckfeldt P, Beck RW, Lipman TH; T1D Exchange Clinic Network. Racial-ethnic disparities in management and outcomes among children with type 1 diabetes. Pediatrics. 2015;135:424-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 220] [Cited by in RCA: 294] [Article Influence: 29.4] [Reference Citation Analysis (0)] |
| 22. | Valenzuela JM, La Greca AM, Hsin O, Taylor C, Delamater AM. Prescribed regimen intensity in diverse youth with type 1 diabetes: role of family and provider perceptions. Pediatr Diabetes. 2011;12:696-703. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 43] [Article Influence: 3.1] [Reference Citation Analysis (0)] |