Published online Sep 15, 2022. doi: 10.4239/wjd.v13.i9.696
Peer-review started: May 1, 2022
First decision: May 29, 2022
Revised: June 12, 2022
Accepted: August 15, 2022
Article in press: August 15, 2022
Published online: September 15, 2022
Processing time: 131 Days and 9.2 Hours
Diabetes mellitus is a chronic metabolic disorder resulting in an increased blood glucose level and prolonged hyperglycemia, causes long term health conse-quences. Chronic wound is frequently occurring in diabetes patients due to compromised wound healing capability. Management of wounds in diabetic patients remains a clinical challenge despite many advancements in the field of science and technology. Increasing evidence indicates that alteration of the biochemical milieu resulting from alteration in inflammatory cytokines and matrix metalloproteinase, decrease in fibroblast and keratinocyte functioning, neuropathy, altered leukocyte functioning, infection, etc., plays a significant role in impaired wound healing in diabetic people. Apart from the current pharmacotherapy, different other approaches like the use of conventional drugs, antidiabetic medication, antibiotics, debridement, offloading, platelet-rich plasma, growth factor, oxygen therapy, negative pressure wound therapy, low-level laser, extracorporeal shock wave bioengineered substitute can be considered in the management of diabetic wounds. Drugs/therapeutic strategy that induce angiogenesis and collagen synthesis, inhibition of MMPs, reduction of oxidative stress, controlling hyperglycemia, increase growth factors, regulate inflammatory cytokines, cause NO induction, induce fibroblast and keratinocyte proliferation, control microbial infections are considered important in controlling diabetic wound. Further, medicinal plants and/or phytoconstituents also offer a viable alternative in the treatment of diabetic wound. The focus of the present review is to highlight the molecular and cellular mechanisms, and discuss the drug targets and treatment strategies involved in the diabetic wound.
Core Tip: This paper reviewed molecular pathways and epigenetic mechanisms involved in the pathogenesis of diabetic wounds. The role of microbiota, oxidative stress, inflammatory cytokines, and alteration in the factors involved in normal wound healing process was highlighted. Molecular targets of therapeutic agents, the role of phytochemicals was discussed. The efficacy of several pharmacotherapy, treatment strategies, and recent clinical trials aiming to improve the outcome of diabetic foot ulcers was reviewed.
- Citation: Chakraborty R, Borah P, Dutta PP, Sen S. Evolving spectrum of diabetic wound: Mechanistic insights and therapeutic targets. World J Diabetes 2022; 13(9): 696-716
- URL: https://www.wjgnet.com/1948-9358/full/v13/i9/696.htm
- DOI: https://dx.doi.org/10.4239/wjd.v13.i9.696
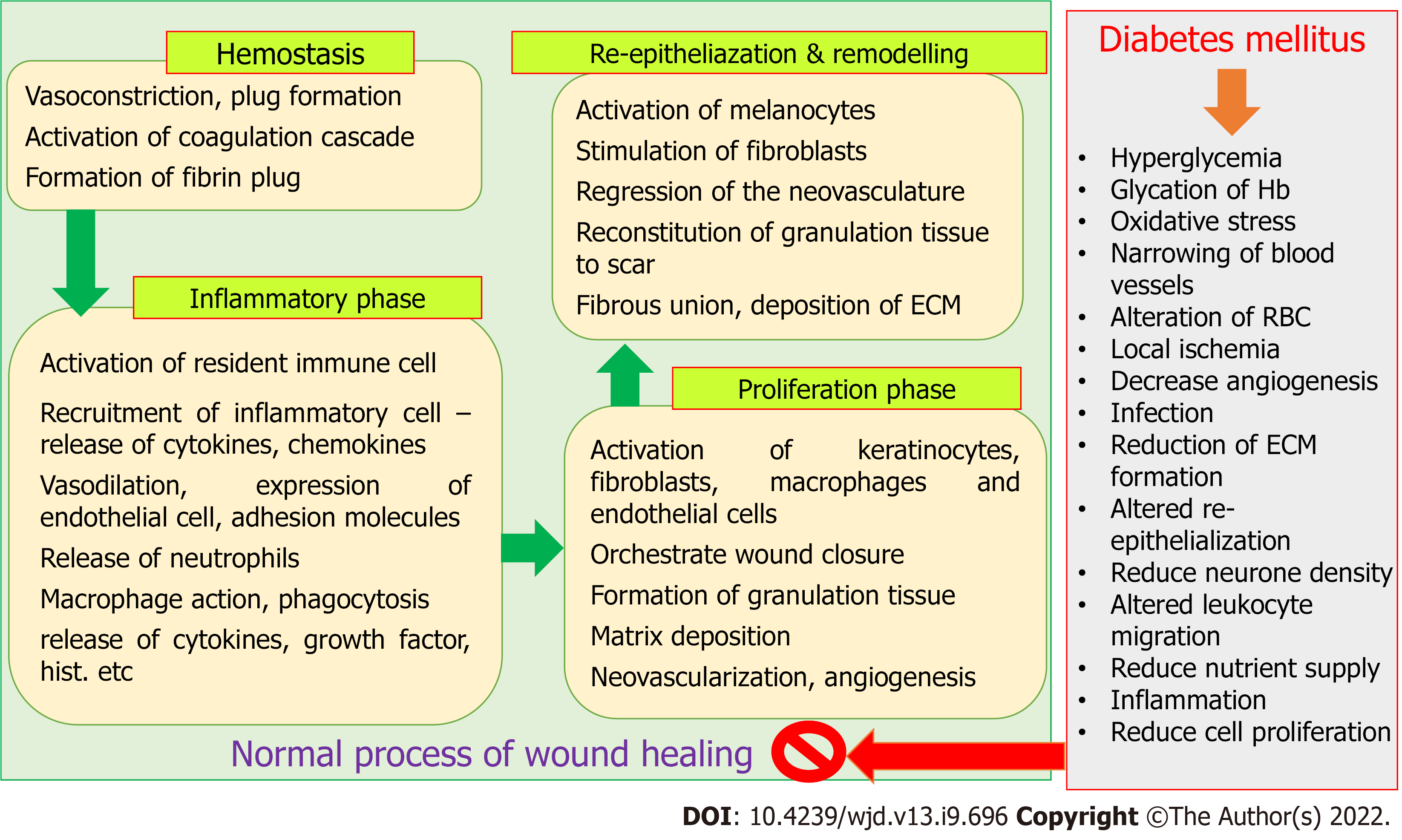
The process of wound healing is complex and requires spatial as well as temporal synchronization between different types of cells with specific functions. Hemostasis, inflammatory phase, proliferative phase, re-epithelialization, and remodelling phase are the four major phases of wound healing process, which result in the restoration of functional integrity of tissues[1-3]. Alteration in the microenvironment due to diabetes mellitus (DM) results in a change in the level of oxygen, chemokines, synthesis of growth factors, extracellular matrix, oxidative stress that in turn alter normal cellular recruitment and activation, and induce impaired or delayed wound healing[1,3]. Ageing, genetic disorders, obesity, and metabolic disorders including DM, are responsible for the abnormal wound healing process, that enhances the risk of developing chronic wound[1,3,4]. It was estimated that chronic wounds directly affect the quality of life of about 2.5% population of the United States, and the medicare cost for management of all wounds and the related situation was projected between $28.1 to $96.8 billion[5]. Management of wounds in the diabetic individual is a major clinical and social concern. The hyperglycaemic environment in diabetic people causes impaired and delayed wound healing[4], making the situation more perilous as the number of diabetic people is increasing day by day. It was also found that treatment and management of diabetic ulcers and surgical wounds were the most expensive[5]. The IDF Diabetes Atlas estimated that the prevalence of DM in 2021 was 10.5% (536.6 million people in the 20-79 year age group), which will increase to 12.2% (783.2 million in the 20-79 year age group) by 2045. Global health expenditures related to the management of DM and its complications are expected to reach $966 billion in 2021[6]. It was also predicted that almost half of the adult population (44.7%; 239.7 million of 20-79 years old) were unaware of their diabetic condition. People may develop micro and macrovascular complications during an asymptomatic diabetic state[7]. Impaired or delayed wound healing affects about 25% of diabetic people. A study suggested that 1 in 3 to 1 in 5 diabetic individuals are at risk of chronic non-healing wounds, including diabetic foot (with a very high recurrence rate) in their lifetime[8]. Zhang et al[9] estimated that the global prevalence of diabetic foot is 6.3%, which usually affects type 2 diabetic people, older people, and people with a longer duration of DM.
Both the extrinsic and intrinsic factors are responsible for delay in the wound healing process in diabetic patients. Repeated trauma or mechanical stress in the diabetic foot can lead to neuropathy and ischemic situation. Glucose-rich environment results in increased generation of advanced glycation end-products (AGEs) and elevated levels of inflammatory cytokines [i.e., interleukin (IL)-1β and tumor necrosis factor α (TNF-α)] for a persistent period that hinders the normal process of wound healing[10,11]. In turn, hyperglycemia reduces collagen synthesis, growth factor production, macrophage function, angiogenic response, migration and proliferation of fibroblast and keratinocyte, epidermal nerve count, and the balance between extracellular matrix (ECM) component accumulation and matrix metalloproteinase (MMP) induced remodelling [4,12]. The normal wound healing process and effect of the hyperglycemic condition are depicted in Figure 1.
Despite the presence of protocols to standardize care in the diabetic wounds, as well as numerous advancements in scientific research and in clinical fronts, DM remains a problematic situation for wound healing. This paper is an attempt to highlight the mechanistic insights, plausible therapeutic targets, and pharmacotherapeutic approaches, particularly the role of phytochemicals in the management of diabetic wounds, in light of recent shreds of evidence.
Wound healing, being an evolutionary conservation process, restores impaired epithelial barriers through a cascade of events including inflammatory responses, proliferation, cellular migration, angiogenesis, and remodeling of tissues[13]. DM interferes with the normal healing process to provoke non-healing wound, and leads to complications including walking difficulty and infections like septicemia, abscess, cellulitis, osteomyelitis, and gangrene[4]. Acute diabetic wounds with an impaired healing process of unknown aetiology are the first signs of chronic diabetic wounds. Hyperglycemia, hypoxia, chronic inflammation, neuropathy, circulatory dysfunctions, alteration in neuropeptide signalling, and infections impede the diabetic wound healing process. Importantly, due to the heterogeneous nature of the diabetic wound, there exist no clear implications from the pathogenic vantage. The following subsections discuss the potential factors underlying the pathogenesis of diabetic wound.
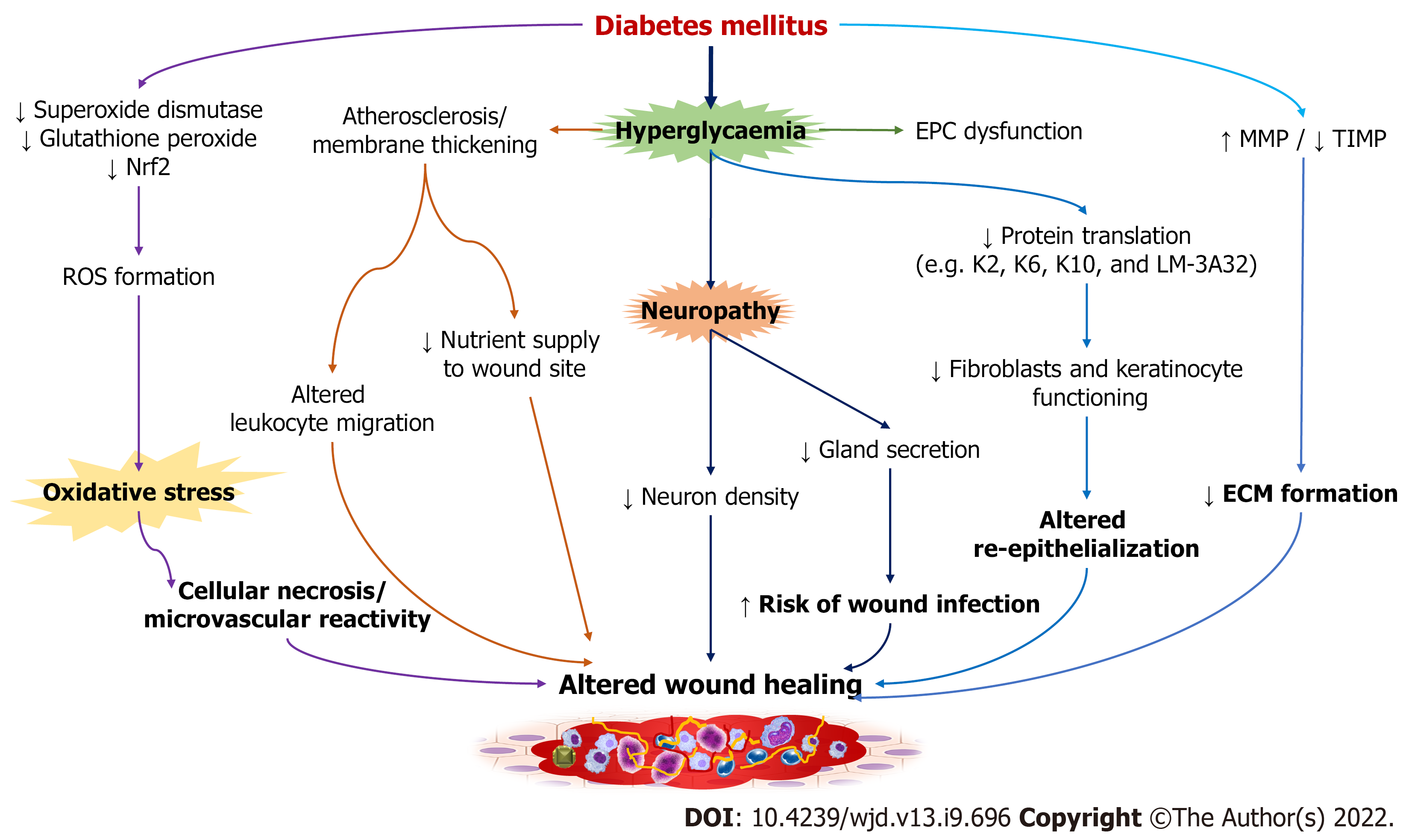
Impaired wound healing associated with diabetes remains inconclusive. However, the alterations in cellular factors and biochemical mediators have been believed to be involved in the development and progression of diabetic wound (Figure 2). Factors like hyperglycemia and oxidative stress in diabetic patients result in dysregulated macrophage polarization through modulation of epigenetic codes to delay the process of wound healing[14,15]. Hyperglycemia is implicated in impaired wound closure in diabetic foot ulcers (DFUs), with reduced skin cell function and the formation of atherosclerosis and neuropathy as possible contributors[8]. The development of atherosclerosis leads to alteration in the physiology of endothelial cells along with deprivation of nutrients in the wound site, critically affecting the healing process. Patients with type 1 DM are more prone to macrovascular diseases, especially affecting femoral and metatarsal arteries[16,17]. DM associated early microvascular deficiencies include decreased capillary size, basement membrane thickening, and arteriolar hyalinosis. Thickening of the membrane disrupts the physiological exchanges and causes altered leucocyte migration, and thereby increasing the risk of microbial infections[18,19]. Hyperglycemia disrupts protein translation as well as the migration and proliferation of fibroblasts and keratinocytes involved in the process of re-epithelialization[20-22]. For instance, altered expression of proteins like cytoskeletal keratin proteins (K2/K6/K10) associated with keratinocyte differentiation, and LM-3A32, a laminin-5 α3 chain precursor protein that regulates epithelial cell binding to the basement membrane, was reported in subjects with DFUs[23]. As LM-3A32 is required for the survival and differentiation of keratinocytes, reduction in this protein affects the re-epithelialization process[24]. Interestingly, the expression of mRNA and microRNA was found to be non-significant in diabetic and non-diabetic foot skin fibroblasts[25]. However, fibroblasts from DFUs were reported to exhibit altered morphology, growth factor unresponsiveness, ECM deposition, and reduced proliferation and migration[26-29]. Impaired vasculogenesis and angiogenesis due to deregulation of the growth factors and receptors leads to impaired wound healing. Dysfunctional endothelial progenitor cells (EPC) or reduction in their numbers and transition to proinflammatory EPC phenotypes have been implicated in DM[30,31]. Notably, EPC dysfunction and altered recruitment are contributed by hyperglycemia, chronic inflammation, oxidative stress, and activation of NADPH oxidase associated with diabetes pathogenesis[32]. Prolonged IL-1β production and reduced expression of peroxisome proliferator-activated receptor-γ are also involved in the impairment of wound healing in DM[33]. Higher expression of MMPs including MMP-1, 2, 8, 9, 14, and 26, and lower expression of their tissue inhibitors were also reported in diabetes[34,35]. In patients with DFUs, it was reported that there is an increase in MMPs and a decrease in tissue inhibitor of metalloproteinase (TIMP)-2, which supports the fact that in a proteolytic environment, diabetic wound fails to heal due to reduction in ECM formation[36]. An increase in MMPs also contributes to matrix degradation, delayed cell migration, and inhibition of collagen deposition[36]. Oxidative stress resulting due to decrease action of enzymes like superoxide dismutase and glutathione peroxidase augment diabetic wound. Overproduction of reactive oxygen species (ROS) from hexosamine, polyol, and AGE pathways affects the later stages of diabetic wound healing, particularly by damaging the peripheral nerves. Consequently, the detrimental effect on the structure, supply, and metabolism of peripheral nerves (neuropathy) increases the risk of DFU development[37]. Hyperglycemia not only contributes to impaired healing but also makes skin prone to injury. Decrease in nuclear factor erythroid factor 2-related factor 2 (Nrf2) in diabetic patients increases the oxidized proteins and ROS generation[38,39]. In Nrf2 knockout mice, delayed wound healing was reported when compared to a Nrf2+/+ mice, possibly due to oxidative DNA damage, elevated MMP-9 expression, and lower level of transforming growth factor-beta 1 (TGF-β1) expression[40]. Hyperglycemia also leads to an increase in neutrophil extracellular traps release, which has been implicated in delayed wound healing in both murine and human models[13,41].
The formation of a diabetic wound is also linked to several forms of neuropathy, including sensory, motor, and autonomic. Sensory deficits, for example, cause a loss of protective symptoms, whereas motor neuropathy causes anatomical deformities and ischemic death in the plantar region of the foot[42], and autonomic neuropathy reduces sweat secretion from the glands, making skin dry and increasing the risk of infection and pruritus[43]. Furthermore, neuropathy causes a decrease in neuron density, causing impairment in wound healing. Primarily, diabetic neuropathy occurs in nerves that are dependent on nerve growth factor[8]. Impaired microvascular processes along with autonomic neuropathy and denervation of sympathetic nerves disrupt the blood flow. Cellular necrosis and microvascular reactivity are also triggered by Poly (ADP-ribose) polymerase enzyme via oxidative DNA damage[16,44]. In diabetic neuropathy, impairment of C-fibre dependent neurovascular responses leads to abnormality in the release of histamine, substance P, and calcitonin related peptide, thus exhibiting altered vasodilatation in case of stress like pressure or trauma[44]. However, the direct link between neuropathic abnormalities and glucose control is yet to be proven.
Despite the fact that epigenetic pathways have a role in a variety of diabetic complications, evidence of epigenetics in diabetic wound or impaired wound healing is still emerging. The role of microRNA in diabetic wound was first highlighted by a study that revealed up-regulation of miR-503 in plasma obtained from DFUs and in human umbilical vein endothelial cells (HUVEC). In vitro experiment suggested the detrimental effect of forced miR-503 expression on function of HUVEC cells resulting due to impaired migration, proliferation, and formation of blood vessels[45]. Blockage of miR-503 expression showed improvement in angiogenesis in diabetic animals with limb ischemia[45,46]. Another study demonstrated that diabetic mice had a distinct microRNA signature, with differential expression of fourteen microRNAs[47]. Of these, expression of miR-146b was found to be up-regulated by 30 fold. Though miR-21 was up-regulated in diabetic skin, it was reduced in diabetic wound healing. This study suggested the necessity of miR-21 expression for fibroblast migration and miR-21 knock-down results in altered cellular migration. Similarly, another study showed the stabilisation of hypoxia-inducible factor α leads to miR210 expression, which silences the expression of E2F3, an important element of wound healing[46]. This implies the fact that epigenetic changes in miR-210 lead to impaired wound re-epithelialization and reduced proliferation. The involvement of DNA methylation in impaired diabetic wound healing is being studied in many experiments. A study reported inhibition of DNA methyltransferase 1 (DNMT1), an enzyme that transfers a methyl group to the cytosine ring to produce 5-methylcytosine associated with transcriptional repression, suppresses inflammatory signals in bone marrow derived macrophages and also promotes M2-like macrophage formation[48]. This finding was supported by DNMT1 knockdown in db/db mice showing improvement in wound healing[49]. In contrast to that, demethylation of MMP-9 promoter in keratinocytes was reported to be involved in the induction of diabetic wound[50,51]. Apart from the role of DNA methylation in wound healing, it is also associated with metabolic memory, insulin resistance, and other diabetic complications[52,53]. Unlike DNA methylation, histone methylation does not always lead to transcriptional repression. Instead, it silences or promotes transcription based on the target residue and methyl groups. Methylation of histone H3K4 is regulated by SET domain containing protein family, particularly MLL1 that promotes inflammatory gene expression in nuclear factor kappa B-dependent manner[54-56]. A study reported the role of mixed-lineage leukemia-1 (MLL1) is to catalyze H3K4me3 deposition in macrophages during the process of wound healing[57]. Delayed wound healing and reduced pro-inflammatory cytokine generation were reported in a myeloid-specific MLL1 deletion in mice. Monocytes isolated from patients with type-2 DM demonstrated higher MLL1 expression, indicating dynamic regulation of MLL1 expression during diabetic wound healing. In diet-induced obesity model of diabetes, increased expression of histone demethylase (i.e., lysine-specific demethylase 6B or JMJD3) that targets H3K27me3 was seen in wound macrophages[58,59]. Epigenetic regulation of IL-6 expression in neutrophils was believed to be impacted by toll-like receptor (TLR) activation associated with increased H3K27ac, H3K4me3, and acetylated histone H4[60]. Re-epithelialization is also promoted by JMJD3 expression, which induces keratinocyte migration to the wound site[61]. Similar report suggests upregulation of JMJD3 expression on the wound site is necessary for early onset of the wound healing process, which is absent in diabetic wound[62]. However, it will be too oversimplified interpolation as most of these findings are limited to normal wounds; thus, further studies are warranted. Other histone modifications including histone acetylation or deacetylation, histone phosphorylation, histone-arginine demethylation or methylation, and ATP-dependent chromatin remodelling are also being studied for their potential role in diabetic wound healing[62].
Certainly, pathogenic infections are not directly associated with the pathophysiology of diabetic wounds but are critical from the vantage of impaired wound healing, hospitalization, morbidity, and amputation. However, the role in the initiation of diabetic wound in case of trauma remains unclear. The rapid spreading of infections and high microbial burden exhibit detrimental effect on the wound healing process. Injury to the superficial skin layer allows polymicrobial contamination and colonization, affecting diabetic wound. Particularly, infections like cellulitis, osteomyelitis, and abscesses are of major concern[16]. The advent of high-throughput sequencing technologies like microarray, 16S rRNA sequencing, and whole-genome sequencing have enabled the expansion of diabetic wound microbiome. Diabetic wound has demonstrated higher colonization of Staphylococcus aureus and S. epidermidis[63]. Another study reported Staphylococcus, Enterobacteriaceae, and Pseudomonas to be the most common colonizers in DFUs[64]. Stratification of DFUs as per infection severity revealed higher bacterial diversity in severely infected DFUs, while Staphylococcus and Streptococcus were found to be the most abundant in mild-to-moderate DFUs[65]. It was similar to a previous finding that found diverse microbiota (with higher incidence of anaerobic and Proteobacteria infection) in deep chronic ulcers, while Staphylococcus was found to be abundant in acute and superficial ulcers[66]. However, contrary to these reports, another study reported Staphylococcus spp. to be the primary culture detected in the microbiome in diabetic foot osteomyelitis[67]. A higher prevalence of S. aureus colonization in DFUs and intact diabetic skin lead to systemic infection and osteomyelitis[63]. Indeed, in a Nigerian observational multi-center study, it was reported that the presence of osteomyelitis is an important predictor of wound healing in hospitalized patients with DFUs[68]. The expression of proteolytic factors by Streptococcus and Staphylococcus are believed to be the disruptor of skin barrier. For example, SpeB released by Streptococcus leads to cleavage of desmoglein 1 and 3 that causes epidermal barrier damage[69]. The alkaline environment of DFUs contributes to the formation of bacterial biofilm, leading to complex host–microbiome interaction[70]. The formation of bacterial biofilm along with alkaline pH affects drug action and is responsible for antibiotic resistance[71]. One should appreciate various other factors influencing this intricate microbiome network and its potential correlation with clinical significance. Keeping all this evidence in sight, more longitudinal studies are anticipated for an adequate understanding of the probable relevance of the microbiome to clinical outcomes.
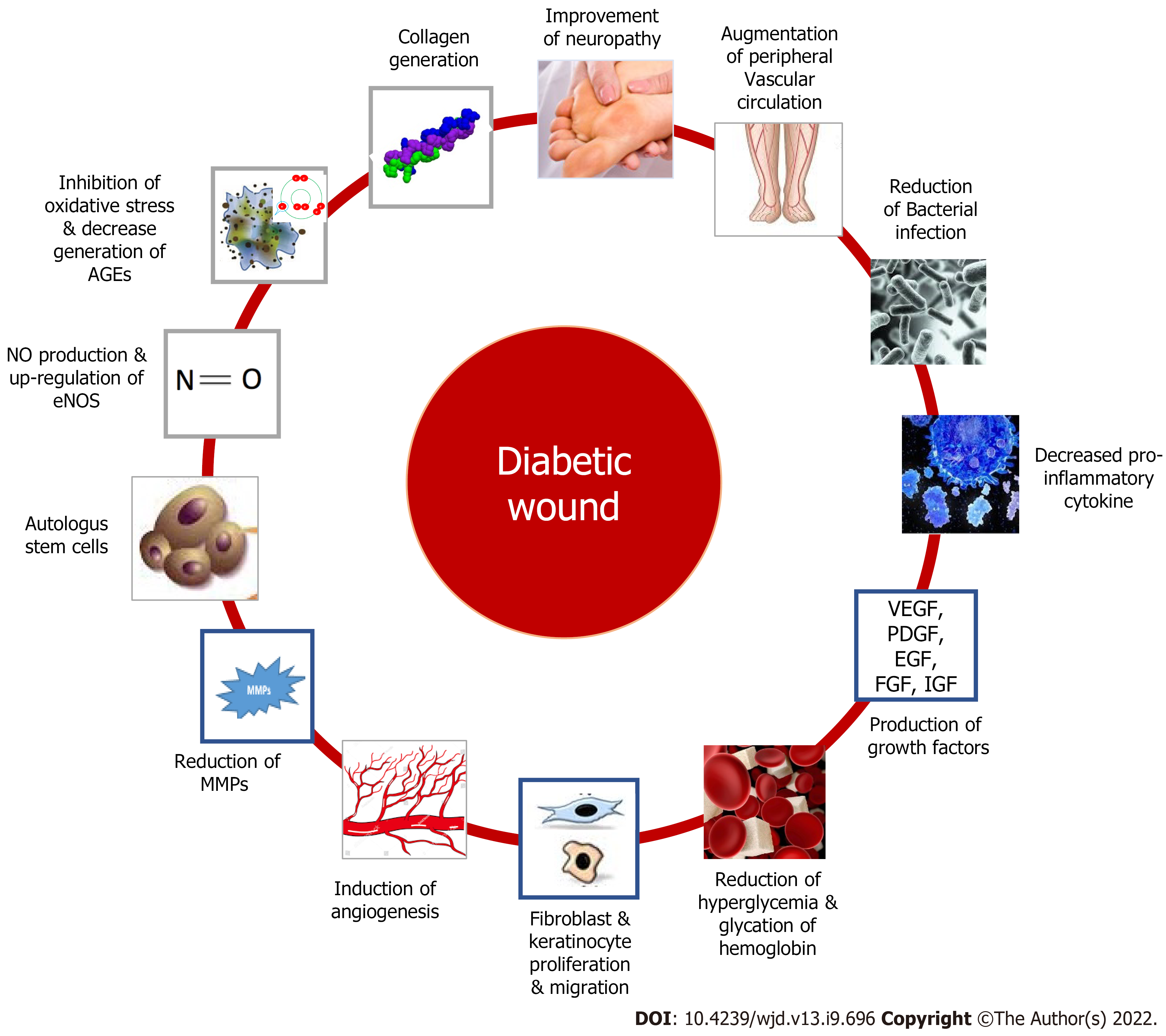
In recent studies, neuropathy, peripheral vascular disease, and impaired wound healing have all been identified as key contributors to diabetic wounds and have all become critical targets in improving wound healing in diabetic patients. But despite of this well-established knowledge, comparatively fewer treatment options are being implemented in routine practice. The expression of cellular components of participating cells, as well as cytokines, growth factors, and other molecular factors required for coordinating the normal healing process, is impaired in diabetic wounds, and as a result, they are unable to progress in synchrony and are primarily checked in the inflammatory phase. Therapeutic strategy targeting such cellular and molecular pathway could be useful for effective management of diabetic wound.
As a result of elevated blood sugar levels in diabetic conditions, damage to nerve fiber occurs, leading to diabetic neuropathy, which can be sensory, motor or autonomic[72]. Sensory neuropathy can result in one of two outcomes: a painful foot or a foot that is devoid of sensation[12]. Motor neuropathy is accompanied by muscle weakening, atrophy, and paresis. The inability of an intrinsic muscle to keep the foot in its normal state resulting because of weakening of inter-osseous muscles in the foot, which contributes to foot deformity. When the foot deforms, the pressure distribution throughout the foot changes, and aberrant pressure develops at various locations on the foot[73]. Keratosis and callus development occur as a result of repeated pressure, which leads to damage to callused areas and induces ulcer formation beneath the callus that further causes cracks on the foot[74-77]. Malfunctioning of the sympathetic nerves supplying the sweat glands in the foot reduces the sweat and moisture in the feet, which leads to the development of cracks[78]. Inflammation, necrosis, and ulceration result when an unnoticed injury is combined[16,79]. Currently, duloxetine, anticonvulsant pregabalin and opioid tapentadol are being prescribed for diabetic peripheral neuropathy. Besides these, a substance like α-lipoic acid has shown effectiveness in delaying or reversing peripheral diabetic neuropathy through its multiple antioxidant properties[80]. Neuropeptides such as substance-P and neuropeptide-Y are also been found to be effective in diabetic neuropathy and associated wound[81,82].
Peripheral vascular dysfunction is another major cause of diabetic wound in a majority of diabetic patients. The wound healing process in the diabetic condition is hampered by the altered physiological response due to glycation of hemoglobin, alteration of the red blood cell membrane and narrowing of blood vessels which cause the decreased supply of nutrients and oxygen to tissues[12]. The development of atherosclerotic plaque in diabetic patients also leads to the development of non-healing wound. Therefore, pharmacotherapeutic agents like antioxidant phytochemicals that can avert oxidative stress and formation of AGEs could be useful in treating diabetic wound.
Bacterial infection is one of the most common causes of wounds, and diabetic individuals are more vulnerable to it because of delayed wound healing and immunosuppression[83,84]. The biofilms created by microorganisms protect them from antimicrobial agents and the immune system while also interfering with the healing process, which is one of the most prevalent reasons for amputation of lower limbs in diabetic wounds[14]. Therefore, empiric therapy should include broad-spectrum antibiotics. In recent times, drug resistance is a bigger problem and several drugs are in use in the treatment of DFU.
Neutrophils, monocytes, macrophages, keratinocytes, fibroblasts, T cells, B cells, mast cells, and endothelial cells are all involved in wound healing and are responsible for the formation and modulation of pro-inflammatory cytokines and growth factors such IL-1, TNF-α, IL-6, vascular endothelial growth factor (VEGF), insulin-like growth factor 1 (IGF-1), and TGF-β. Hyperglycemia and oxidative stress lead to dis-regulation of these cells, resulting in delayed wound healing[85-87]. Increased amounts of pro-inflammatory cytokines cause an inflammatory cascade to be disrupted, resulting in hyper-inflammation and insulin resistance. These also lead to reduced angiogenesis and microvascular issues, impaired macrophage and neutrophil function, impaired keratinocyte and fibroblast migration and proliferation, and impaired growth factor generation[15,88-90]. Many of these cells play a vital role in the immune response, which is also important for wound healing. Various chemokines whose expression can regulate the function of immune cells have the potential to enhance wound healing. Mast cells with close coordination with macrophages, endothelial cells, and fibroblasts, play a key role in matrix remodeling and disrupt the balance of pro- and anti-angiogenic molecules in wound tissues, affecting angiogenesis and vascular regression in the proliferative and remodeling phases, respectively[91-93]. As a result, mast cell degranulation inhibitors such as disodium cromoglycate, quercetin, and luteolin may be promising options for improving diabetic wound healing[92]. Heat shock proteins (HSPs) aid wound healing by attracting dermal fibroblasts, stimulating cell proliferation and keratinocyte differentiation, reducing oxidative stress, ameliorating actin microfilaments, aiding endothelial cell migration, and enhancing pro-collagen synthesis and protein homeostasis[94,95]. Reduced levels of HSPs and their downstream components TLR4 and p38-MAPK (mitogen-activated protein kinases) in diabetic patients are responsible for the slowed healing process[96]. Therefore, targeting this as a therapeutic target could be useful in diabetic wound conditions.
Growth factors are biologically active polypeptides that play an important role in the onset and maintenance of wound healing[97]. In diabetics, any change, i.e., down-regulation of growth factor receptors and rapid degradation of growth factors, causes wound healing to be delayed. Factors such as VEGF, IGF, TGF-β, KGF24, platelet-derived growth factor (PDGF), epidermal growth factor (EGF), basic fibroblast growth factor (bFGF), TNF-α, and IL-6 are significantly reduced in diabetes patients, and several of them have been demonstrated to significantly enhance wound healing in many studies. Growth factors that cause a molecular alteration in the wound micro-environment may help patients with non-responsive wounds. PDGF is a major serum mitogen that promotes fibroblast proliferation, matrix formation, and connective tissue maturation[98]. They attract fibroblasts and inflammatory cells and aid in the production of glycosaminoglycans, proteoglycans, and collagen. During the healing process, it is a critical mediator in fibroblast migration and proliferation, the formation of granulation tissue proteins and provisional extracellular matrix, and angiogenesis[99]. The expression of PDGF and its receptors is reduced in diabetic wounds, and many clinical studies employing PDGF have shown improved healing time[100,101]. It is indicated for the treatment of infections that have spread to deeper subcutaneous tissues or beyond areas with a sufficient blood supply[102]. Another growth factor, bFGF, has a stimulatory effect on fibroblast growth and differentiation, as well as the proliferation of vascular smooth muscle cells, endothelial cells, ECM metabolism, growth, and movement of mesodermally derived cells, all of which speed up the formation of granulation tissue and promote wound healing[103]. Angiogenesis, cell proliferation, migration, differentiation, neo-vascularization, re-epithelialization, and collagen disposition were all stimulated by the clinical application of bFGF, all of which contribute to wound healing[104]. It promotes mesodermal cell chemotaxis and extracellular matrix growth and expedites both acute and chronic wound healing, which gives a scar-free cure[105]. VEGF is a potent angiogenic cytokine that has a substantial impact on healing and promotes rate-limiting processes in vasculogenesis and angiogenesis[106]. Low VEGF levels cause impaired wound healing and aberrant VEGF receptor patterns in diabetics. Decreased VEGF mRNA levels, increased VEGF receptor (VEGFR)-1 Levels, and decreased VEGFR-2 Level are some of the key causes of wound non-healing[107]. In diabetic wounds, VEGF leads to an increase in capillary density, which enhances blood perfusion and metabolism in the wounded tissue[108]. VEGF causes an increase in capillary density, which improves blood perfusion and metabolism in the wounded tissue. This leads to the facilitation of the supply of oxygen and nutrients to assist the growth and function of reparative cells. It is the primary regulator of wound revascularization and permeability and participates in the formation of granulation tissue. On binding with the EGF receptors, EGF causes an increase in epidermal cell, cell motility, cellular migration, mesenchymal regeneration, angiogenesis and cell proliferation[109]. Application of EGF into the wound site results in a greater pharmacodynamic response in terms of granulation tissue growth and wound closure. IGF-1 promotes wound healing by assisting in cell granulation and re-epithelisation, promoting endothelial cell chemotaxis and keratinocyte and fibroblast proliferation, while lower levels of both IGF-1 and TGF-β in wound tissue cause wound healing to be delayed[110,111]. TGF-β attracts and stimulates inflammatory cells such as neutrophils, macrophages, lymphocytes, keratinocytes, and fibroblasts, as well as the synthesis of growth factors, which speed up vascularisation, angiogenesis, and ECM synthesis while slowing down ECM degradation[112]. Therapeutic agents or strategy, which can ameliorate this positively, are useful in diabetic wound condition. Several drugs and phytoconstituents have shown their positive effect in diabetic wounds targeting these biomolecules. The use of platelet-rich plasma (PRP), EGF, PDGF, and FGF has shown promising effects in the treatment of diabetic wound in a better way.
MMPs are a class of endopeptidase that play a key part in wound debridement, as well as angiogenesis, epithelialization, and extracellular matrix remodeling[113]. Matrix proteins such as collagens, basement membrane collagens, proteoglycans, elastin, and fibronectin are digested by the MMPs. TIMPs form a complex with MMPs, limiting interaction with the active site. A balance between MMPs and TIMPs is required for wound healing, which is impaired in diabetes patients[114]. Increased protease activity caused by high MMP levels in diabetic wounds causes tissue damage and slows down normal repair processes[115]. This is due to altered MMP expression and decreased TIMP expression in diabetic conditions, which results in high levels of pro-inflammatory and pro-fibrotic cytokines due to increased inflammatory cell activation and invasion, and indirectly affects MMPs through the formation of advanced glycation products which leads to the loss of growth factors, receptors, and matrix proteins essential for wound healing[111,114]. Drugs, therapy that is useful in diabetic wounds are found to act by enhancing collagen synthesis, decreasing inflammatory cytokines, AGEs etc. Further, identifying the therapeutic agents that can inhibit MMPs, i.e., MMP-1, MMP-8, and MMP-9 could be important in the management of diabetic wounds.
Autologous stem cells capable of self-renewal and multi-lineage differentiation have been used in diabetic wound. Clinically, bone marrow-derived mononuclear cells and mesenchymal stem cells are the most successful stem cell therapies[116,117]. Besides these, several other targets to promote diabetic wound healing include stimulation of nitric oxide production and up-regulation of endothelial NO synthase and nitric oxide (NO) expression[118-120], a decrease of AGE receptors[121], collagen generation and epitheliazation etc[122-124]. Figure 3 represents plausible drug targets for diabetic wound.
Hyperglycemic environments worsen the wound situation and delay the wound healing process, thus controlling blood sugar levels is important for the wound healing process. Several antidiabetic medications [i.e., insulin, metformin, sulfonylureas, dipeptidyl peptidase-4 (DPP-4) inhibitors, thiazolidinediones] found effective in controlling not only blood sugar levels but also promoting the healing of a wound. Metformin was found to be effective in wound healing, which may act by improving epidermis and deposition of collagen, and increasing TGF-β production that may link with angiogenesis process, inflammatory reaction, re-epithelization, and remodeling process. DPP-4 inhibitors may act by increasing the generation of SDF1α, which is crucial for wound repair process[11,125]. Drugs like simvastatin (enhance VEGF and NO content at wound site) and phenytoin (enhance VEGF and FGF in wound area) have also shown some positive effects in wound healing[11,125].
Infection caused by microbes is a major problem in DFU. Antimicrobial therapy targeting Gram -ve, Gram +ve, anaerobic bacteria, and certain fungi, contributing to the pathophysiology of DFU, is also a key approach. Povidone iodine solution (10%), chlorhexidine, acetic acid (5%), and silver compounds can be used to treat the mild wound. Antibiotics like amoxicillin + clavulanate, ampicillin, dicloxacilline, cephalosporin (i.e., cephalexin, cefoxitin, ceftriaxone, and ceftazidime), quinolones (i.e., ciprofloxacin, levofloxacin), metronidazole, and clindamycin used to cure moderate DFU[126]. Drugs like piperacillin/tazobactam + clindamycin, meropenem, imipenem, ertapenem, ampicillin + sulbactam are used to cure severe infections caused by different Gram +ve and Gram -ve bacteria, anaerobes, MRSA, P. aeruginosa, while vancomycin, linezolid, and daptomycin can cure MRSA[11]. Cefepime, ceftazidime, meropenem, and piperacillin/tazobactam are recommended to use against P. aeruginosa; Metronidazole and clindamycin are used to manage infection caused by anaerobes, while osteomyelitis can be managed with quinolones and linezolid. Further, the effectiveness of different drugs like penicillin, cephalosporin (ceftazidime, ceftriaxone, and cefuroxime), dicloxacillin, vancomycin aztreonam, cefalotin, clindamycin, cefoxitin, gentamicin, imipenem, piperacillin/tazobactam, imipenem, metronidazole, amikacin, levofloxacin, and cefalotin against microbes contributing in DFU infection also established[126]. Dressings with hydrogels, acrylics, hydrofibers, films, hydrocolloids, calcium alginates, polyurethane foam and ciprofloxacin-loaded calcium alginate wafer are also used to control the infection[126,127].
Debridement (elimination of bacterial biofilm and necrotic tissue from wound site), offloading (complete/partial removal of pressure), PRP, EGF, PDGF, FGF, oxygen therapy, negative pressure wound therapy (NPWT), low-level laser therapy (LLLT), extracorporeal shock wave therapy (ESWT), bio-engineered skin substitutes/ soft tissue substitutes (amniotic membrane, autologous stem cell therapy, bi-layered bio-engineered skin substitute, human fibroblast-derived dermis, porcine small intestine submucosa), and maggot therapy are also used successfully to cure DFU[127-129].
In clinical practice, control of blood glucose level, periodical foot screening, patient education, use of therapeutic footware by susceptible people, prophylactic arterial revascularization are important in prevention of DFU[130]. Off-loading in different grades of DFUs (grade 1B, 1C), and diagnosis of diabetic foot osteomyelitis are recommended in grade 1B, 1C, 2C DFU using different screening methods by Society of Vascular Surgery[130]. Surgical debridement to remove necrotic and devitalized tissue, use of proper dressing to create and maintain moist environment, reducing plantar pressure and shear stress (off-loading), vascular assessment in patient with peripheral arterial disease are the vital part of wound care in diabetic people[130,131]. Microbial infection is a major concern in DFU, and in such cases, use of antimicrobial agents is advised conserving extent of infection[131]. A number of adjuvant therapy as discussed in previous section are also used for effective wound healing. Further, adequate glycemic control is important also in acceleratd healing of DFU’s[130,131].
Several treatments /medicines have been successfully investigated clinically for their beneficial effects on the diabetic wound, especially in DFUs which was tabulated in Table 1[132-159].
| Ref. | Type | Drug/ product /approach investigated | Type and number of participants | Type of wound | Observation |
| [132] | Homeopathic medicine | Silicea, Sulphur, Lycopodium, Arsenic album, Phosphorus | Observational study, 156 patients | DFU | Ulcer assessment score reduced significantly (P < 0.05) after treatment. Silicea, sulphur (n = 11), lycopodium, arsenic album, phosphorus were found more effective. Although, the effect of homeopathic therapy alone is difficult to establish |
| [133] | Silicea | Observational study, 22 patients | DFU | Positive and encouraging result of silicea in ulcer healing was reported. DFU assessment score was measured, and mean symptom scores at the end of the treatment were found to reduce significantly (P < 0.05) | |
| [134] | Herbal Products | ON101 cream (contain extract of Plectranthus amboinicus and Centella asiatica) | Phase 3 RCT, 236 participants | DFU | Incidence of complete healing in ON101 and comparator group was 60.7% and 35.1% respectively. Although, the number of adverse events in the ON101 group was 7 vs 5 in the comparator group. ON101 produced a better healing effect compared to absorbent dressing alone |
| [135] | Intravenous Semelil (a naive herbal extract) | RCT, 25 participants | DFU | Mean foot ulcer surface area reduced significantly in semelil (i.v. route) group and the average wound closure in semelil group was significantly more than control group (64% vs 25%, P = 0.015). Semelil in combination with conventional therapy showed better effect than conventional therapy | |
| [136] | Olive oil | Double blind RCT, 34 participants | DFU | Degree of ulcer, color, surrounding tissues, the status of ulcer and ulcer drainages were evaluated after topical application of olive oil. Complete ulcer healing in the treatment group was significantly better than the control group (73.3% vs 13.3%, P = 0.003). Olive oil treatment significantly reduced ulcer area and ulcer depth. Olive oil in combination with routine care was better than routine care alone | |
| [137] | Polyherbal formulation (contain G. glabra, M. paradisiaca, C. longa, P. odaratissimus, A.e vera, C. nucifera oil) | Open label, phase III, comparative study, 40 participants | DFU | Polyherbal formulation was found effective similar to that of standard silver sulphadiazine cream | |
| [138] | Semelil (ANGIPARS™, contain Melilotus officinalis) | Clinical study, 10 participants | DFU | ANGIPARS™ was found effective in reduction of wound size by at least 50% during 8 wk period | |
| [139] | PRP | PRP gel | Single-arm clinical trial, 100 participants | DFU | PRP therapy (2 mL/cm2 of ulcers) was found highly effective in the treatment and healing of non-healing chronic DFUs |
| [140] | PRP | Prospective RCT, 20 participants | DFU | Wound healing time was estimated as 8 wk which is superior to the control group. People treated with PRP it found more effective in wound healing | |
| [141] | Human EGF (hEGF) | Recombinant hEGF | Prospective, open-label trial, crossover study, 89 participants | DFU | Wound healing was noted within an average of 46 d in patients who were treated with 0.005% EGF twice a day. Topical application of hEGF combined with hydrocolloid dressing showed promoting healing effect in chronic DFU |
| [142] | Regen-D 150 (hEGF gel-based product) | RCT, 50 participants | DFU | Complete ulcer healing was detected in 78% population against 52% population in the placebo group. Collagen and fibroblasts were significantly developed in the treated group. The application of hEGF can be helpful to promote wound healing and in preventing leg amputations | |
| [143] | PDGF | rhPDGF | RCT, 50 participants | DFU | Wounds contracted more in rhPDGF-treated group compared to the control group (38.55% vs 12.79%; P ≤ 0.001). Dressing with rhPDGF was found more effective and promoted safe wound healing |
| [144] | PDGF gel | RCT, 29 participants | Diabetic lower extremity ulcer | 100% of ulcers were healed in subjects who received PDGF compared to 76.4% of wound healing in placebo group. The study confirms the effectiveness of PDGF gel | |
| [145] | FGF | bFGF | Double-blind RCT, 150 participants | Non-ischaemic diabetic ulcer | Wound cure rate in 0.001% bFGF, 0.01% bFGF and control group was 57.4%, 66.7% and 46.8%. The area of the ulcer was also significantly decreased in bFGF treated groups. bFGF accelerates wound healing in diabetic people |
| [146] | Oxygen therapy | Topical oxygen therapy | RCT, 145 participants | DFU | A significant decrease in wound area was reported in the topical oxygen therapy + standard care group (70%) compare to the standard care group (40%) Addition of topical oxygen therapy with standard care facilitates wound closure in a better way |
| [147] | Hyperbaric oxygen therapy | RCT, 75 participants | Chronic DFU | Complete healing of ulcer index was reported in 52% of participants who received hyperbaric oxygen therapy after 1 year, which was 29% in the placebo. Adjunctive treatment with hyperbaric oxygen therapy may facilitate the healing of foot ulcers | |
| [148] | NPWT | NPWT | Prospective randomized study, 55 participants | DFU | Granulation tissue formation (91.14% vs 52.61%, P < 0.001) and a decrease in the size of ulcer size (40.78% vs 21.18%, P = 0.008) were reported in the NPWT group after 14 d. Duration of hospital and time for complete coverage of the wound with granulation tissue was significantly less in the NPWT group. NPWT led to an early decrease in the size of the ulcer, formation of more granulation tissue, and wound healing |
| [149] | NPWT | RCT, 55 participants | DFU | The rate of ulcer healing was found higher in the NPWT group (P-value 0.01). NPWT leads to a higher rate of healing, and causes a significant decrease in ulcer surface area, size, and depth of the wound, reducing the risk of amputations | |
| [150] | Phototherapy | LLLT | RCT, 23 participants | DFU | Ulcers size reduced significantly in 4th week in LLLT group (P = 0.04). More patients healed completely in LLLT group compared to the placebo group. Meantime of complete healing in patients treated with LLLT was 11 wk vs 14 wk in placebo patients. LLLT promotes the healing process of chronic DFU, and reduces the time required for wound healing |
| [151] | LLLT | RCT, 56 participants | DFU | Increment in total hemoglobin was more using the highest intensity configuration compare to the lower intensity setup in patients with DFU. A decrease in the very-low frequency/low frequency ratio, slightly more than the highest intensity in DFU people was observed. LLLT was found to increase blood flow and regulation of the autonomic nervous system in patients with DFU | |
| [152] | ESWT | ESWT | Single-blinded RCT, 38 participants | DFU | Patients received shock wave therapy 2/week for a total of 8 treatments. Average healing time was lower in ESWT-group when compared with the control group (64.5 vs 81.17 d, P < 0.05). AT 20 wk, 54% of ulcer healed completely in ESWT-groups compared to 28.5% in the control group |
| [153] | ESWT | Prospective RCT, 23 participants | DFU | At 7 wk, the mean reduction in ulcer area was 34.5% (CI, 0.7-68.3) in the ESWT group and 5.6% (CI, -42.1-53.3) in the control group. ESWT also enhances tissue oxygenation | |
| [154] | Stem cell therapy | Topical application of MSC | Clinical case study of three patients | Neuropathic DFU | MSCs at low doses enhance the re-epithelialization of DFU. MSCs may start early to reduce overall wound closure time |
| [155] | HUCMSCs | RCT, 56 participants | DFU | Patients in HUCMSCs (endovascular infusion and injection around the foot ulcer) experienced greater and betterment in skin temperature, transcutaneous oxygen tension, ankle-brachial pressure index, and claudication distance. Three months after treatment significant enhancement in neovessels, and complete or gradual ulcer healing was observed in the experimental group | |
| [156] | NO generating approach | EDX110 (nitric oxide generating medical device) | RCT, 135 participants | DFU | At 12 wk, EDX110 use resulted in 88.6% reduction in median wound area compared to 46.9% for the control group (P = 0.016). EDX110 was found to improve foot wound healing in diabetic people significantly by reducing the ulcer area |
| [157] | Other Approaches | Bemiparin (low MW heparin) | RCT, 70 participants | DFU | In bemiparin group, the ulcer improvement rate was 70.3% compared to 45.5% in the placebo group. Though, complete healing rates found similar in both groups at 3 mo were, as were the number of adverse events. Bemiparin is better than a placebo in the management of DFU and has few side effects |
| [158] | Honey dressing | RCT, 348 participants | DFU | In 75.97% of cases wound healed completely after honey dressing in comparision to 57.39% of case in the saline dressing group. The homey dressing also reduced the median wound healing time (18.00 d) compare to the control group (29.00 d). Honey is an effective dressing substance compared to conventional dressings | |
| [159] | Omega-3–rich fish skin grafts | RCT, 49 participants | DFU | At 12 wk, 67% of foot wounds were completely closed compared with 32% in the standard care group. Study findings indicated that fish skin graft is useful in the treatment of chronic DFUs that do not heal with standard treatment |
PRP is an important treatment approach investigated in DFU. A systematic review with meta-analyses of 10 studies reported that PRP promotes chronic diabetic wound healing (RR = 1.32; 95%CI: 1.11-1.57, I2 = 15%) by reducing the volume and time of wound healing[160]. PRP may act via promoting the proliferation of wound cells, upregulation of cyclin A and cyclin-dependent kinase 4 proteins, modification of macrophage phenotype, reduction of TNF-α, enhancement of TGF-β and VEGF, increased secretion of fibroblast of collagen type I and III[161].
A systematic review of 26 randomized controlled trials (RCTs) examined the usefulness of different recombinant proteins and growth factors in the treatment of DFU. EGF can be used as intralesional injection, topical cream, or gel. This meta-analysis reported that EGF significantly improves wound healing and the study failed to find a significant effect of EGF in reducing the risk of amputation[162]. Decreasing the level of circulating C-reactive protein, decreasing NFκB1, TNF-α, and IL-1a expression, and increasing the wound expression of platelet-derived growth factors (PDGF)-B, cyclin-dependent kinase 4, P21, TP53, angiopoietin 1, collagen 1A1, MMP-2, and TIMP-2 after the treatment with hEGF may be linked to its beneficial effect[161]. Recombinant human PDGF (rhPDGF) also exhibits their beneficial effect in several clinical studies[143,144], but few clinical studies also failed to find statistically significant effects of rhPDGF compared to the control group[163,164] when used to cure DFU. The effectiveness of PDGF may be related to the promotion of fibroblast and leukocyte migration, and synthesis of extracellular matrix[161]. FGF, a family of cell signaling proteins, is found to stimulate angiogenesis, induce fibroblasts proliferation, and promote wound healing. About 23 subtypes of FGF from 7 subfamilies were identified[165]. Some clinical studies have reported the beneficial effect of FGF in diabetic wound[145], some studies failed to report the advantageous effect of FGF over the placebo group[166], while clinical studies reported the beneficial effect of combined use of human EGF and acidic FGF on wound healing in the later stage[167]. Very few clinical studies evaluated the effectiveness of granulocyte-colony-stimulating factor, topical telbermin, epoetin-β, talactoferrin, TGF-β2 in the diabetic wound. But the results are inconsistent[162].
Oxygen therapy is found to improve cell metabolism and energy, decrease proinflammatory cytokines and ROS, and promote the synthesis of matrix and wound repair[161]. Few clinical studies confirmed the beneficial effect of hyperbaric as well as topic oxygen therapy in promoting diabetic wound[146,147]. A systematic review and meta-analysis of 20 RCTs and 1263 trials analysed that hyperbaric oxygen therapy confer benefits in DFU treatment by increasing the healing of ulcers (relative risk, 1.901; 95%CI: 1.484-2.435, P < 0.0001), reducing healing time, and also decrease the risk of major amputation[148].
It was evaluated that NPWT results in macro- and micro-deformation that stimulate different wound healing cascade like promotion of tissue granulation, epithelialization, proliferation of vessel, neo-angiogenesis, pro-angiogenic condition, removal of surplus extracellular fluid, anti-inflammatory effect, increase expression of VEGF, FGF2, modification of circulating micro-RNAs, alteration of DNA methylation of genes linked with wound repair[161,168]. Liu et al[169] in their study (meta-analysis of 11 RCTs) concluded that NPWT is a safe, cost-effective and effective strategy in the treatment of DFU, while Liu also evaluated 11 RCTs and found that compared with wound dressings NPWT may enhance the proportion of wounds healed, decrease the time of postoperative foot wound healing[170].
LLLT was found to increase blood flow and regulation of the autonomic nervous system in patients suffering from DFU[151]. Reduce wound inflammation, enhance fibroblasts and angiogenesis[161], which may play an important role in diabetic wound healing. A metanalysis of 13 RCTs that included 413 patients concluded that LLLT significantly enhanced complete healing rate (RR = 2.10, 95%CI: 1.56-2.83, P < 0.00001), decreased wound ulcer area, and reduce mean healing time of wound healing in patients suffering from DFU[171].
Huang et al[172] performed a meta-analysis of 8 RCTs and concluded that ESWT treatment reduced wound surface area in greater proportion, enhances re-epithelialization and can reduce treatment inefficiency. ESWT is useful as an adjuvant strategy in the management of DFUs, which can improve the complete wound cure rate and reduce the healing period of DFUs. ESWT may enhance the angiogenesis process, decrease macrophage number, and enhance the production of macrophage of growth factors from macrophages that help in the healing of wound[161].
In light of current evidence, it can be suggested that stem cell-based therapy (delivery through both local and systemic route is effective to heal DFU and considered a promising regenerative medicine, and mechanisms of stem cell therapy include improved angiogenesis, decrease inflammation, ameliorating neuroischemia, improved collagen deposition, etc.[173].
Wound healing in diabetic people can be promoted by providing endogenous or exogenous NO. Products (i.e., patches/ matrices) that release NO are used to treat diabetic wounds by different mechanisms like enhancement of angiogenic activity, endothelial cell proliferation, conferring antimicrobial substances, and promoting cell migration to the injured site[174]. Only a few clinical studies have reported the beneficial effects of NO-releasing devices, and several products are in the clinical trial.
Homeopathic medicines (like silicea, sulphur, lycopodium, and arsenic) were also investigated in the clinical trial and concluded that homeopathic medicine may be useful in the management of diabetic wounds[132,133]. Several other products, like honey, fish skin grafts, etc., were also clinically investigated for their beneficial effects against DFU[158,159]. Further, several herbal products were also successfully investigated in the treatment of diabetic wound[134,135,136-138].
Medicinal plants and phytoconstituents always represent an important, effective and alternative treatment strategy to cure diseases. Phytochemicals have showed their effectiveness in different diabetes complications. Anti-inflammatory mechanism of phytochemicals is considered important in the management of diabetes wound. Epigallocatechin gallate in pre-clinical investigation was found to reduce reduced levels of IL-1β, TNF-α and IL-6, producing inhibition of Notch signaling and accumulation of macrophage at a wound site. Kaempferol, is an important dietary flavonoid found to exert different pharmacological activities, including antioxidant, anti-inflammatory and cardioprotective activity. An ointment containing Kaempferol was found effective in diabetic excisional and non-diabetic incisional wounds in experimental animals[175]. Flavonoids an important class of phytoconstituents, exerted anti-inflammatory and antioxidant effect, and also enhances angiogenesis and re-epithelialization. Preclinical trials found the effectiveness of isoliquiritin, isoflavonoid, naringenin, dihydromyricetin, dihydroquercetin, quercetin, hesperidin, kaempferol, proanthocyanidins, icariin, puerarin, rutin, genistein, luteolin, rutoside, silymarin, daidzein, genistein, and epigallocatechin gallate to cure wound[174]. Flavonoids positively regulate MMP-2, MMP-8, MMP-9, MMP-13, Ras/Raf/ MEK/ERK, PI3K/Akt, and NO pathways. Phytochemicals are found to reduce oxidative stress, expression/release of proinflammatory/inflammatory cytokines, i.e., TNF-α, IL-1β, IL-6, NF-κB and upregulate IL-10 and antioxidant enzymes. Flavonoids also act on macrophages, fibroblasts and endothelial cells by facilitating expression/release of TGF-β1, VEGF, angiopoietin, tyrosine kinase with immunoglobulin and epidermal growth factor homology domains, and small mothers against decapentaplegic 2 and 3[176]. Oguntibeju[177] in his paper highlighted different medicinal plants like Rosmarinus officinalis, Carica papaya, Radix rehmanniae, Annona squamosa, Catharanthus roseus, Centella asiatica, Acalypha langiana, Hylocereus undatus, Punica granatum, Aloe vera, and Martynia annua that has been investigated in the treatment of diabetic wound. Benefits of the plants may link to different mechanisms like an increase in fibroblast cell, fibroplasia, increase in collagen formation, enhancement of tissue regeneration, angiogenesis, antimicrobial, anti-inflammatory and antioxidant effect. A recent clinical study established the effectiveness and safety of nano-hydrogel embedded with quercetin and oleic acid when used in the management of lower limb skin wound in diabetic patients. The formulation effectively treated the wound and reduce the wound healing time compared to the control group[178]. Infections caused by different microbes like Staphylococcus aureus, Streptococcus β-hemolytic, Pseudomonas aeruginosa, Peptostreptococcus spp., Proteus spp., Prevotella spp., Bacteroides spp., Clostridium spp. and anaerobes are posing a serious situation in diabetic people[126]. Medicinal plants and phytochemicals with antimicrobial activity may also play an important role in the management of diabetic wound. Several plants have shown their potential against the microbial strain responsible for infection in the diabetic wound[126]. Formulation designed with Momordica charantia, Actinidia deliciosa, Aloe vera, citrus fruits, Sida cordifolia, Nigella sativa, Curcuma longa, and Azadirachta indica has shown their potential in the treatment of diabetic wound[126]. Isoflavones isolated from plant sources were also found to be effective against DFU bacteria[179] Phytofabricated silver nanoparticles (Aerva lanata reduced silver nanoparticles) at 20 μg/mL were found highly effective against multi antibiotic-resistant DFU isolates like E. coli, P. aeruginosa, S. aureus, S. subtilis. Identified phytochemicals of A. lanata include rutin, quercetin, kaempferol, gallic acid and ellagic acid[180]. The use of phytoextracts/active compounds may be considered as an important strategy for addressing the wound problem associated with DM in a better way.
Diabetes adversely acts on the phases of normal wound healing phases, i.e., hemostasis, inflammatory phase, proliferative phase, re-epithelialization and remodeling phase, and poses a big burden on the quality of life of a diabetic individual. Hyperglycemia can trigger oxidative stress, increase inflammatory cytokines, interrupt angiogenesis, decrease the functioning of fibroblast and keratinocyte, induce neuropathy associated events, increase MMPs, and reduce TIMPs that is responsible for impaired states of wound healing. An understanding sequence of the molecular and cellular cascade, epigenetic mechanisms, microbial perspective, complexity and plasticity of impaired wound healing in diabetic conditions is required for targeted research focusing on treatment of diabetic wound. Pharmacotherapy/strategy involving angiogenesis stimulation, growth factors, cytokines modulators, MMP inhibitors, ECM stimulators, anti-inflammatory drugs, antidiabetic agents, antimicrobial drugs, debridement, offloading, PRP, oxygen therapy, NPWT, LLLT, ESWT, stem cells, bio-engineered substitutes, and various natural-based products have shown their benefit. There has been a lack of quality-based evidence of efficacy of different adjuvant therapies tested through different clinical trials, thus more structured and quality studies are required. Indeed, the utilisation of medicinal plants/products in diabetic wound care holds prodigious potential in the future, and the development of innovative pharmaceutical formulations for advanced wound care is equally critical. Effective diabetic wound management necessitates a combination of techniques, including medication and non-pharmacological intervention. Hence, the treatment strategy of the future can only succeed if research concentrated on plausible drug targets after comprehending the inherent pathological complexities, evaluating non-pharmacological approaches through well-designed clinical trials, and targeting natural sources for new drug development.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, Research and Experimental
Country/Territory of origin: India
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Samadi N, Iran; Wu QN, China S-Editor: Chang KL L-Editor: A P-Editor: Chang KL
| 1. | Rodrigues M, Kosaric N, Bonham CA, Gurtner GC. Wound Healing: A Cellular Perspective. Physiol Rev. 2019;99:665-706. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1040] [Cited by in RCA: 1638] [Article Influence: 273.0] [Reference Citation Analysis (0)] |
| 2. | Shah A, Amini-Nik S. The Role of Phytochemicals in the Inflammatory Phase of Wound Healing. Int J Mol Sci. 2017;18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 61] [Cited by in RCA: 85] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 3. | Wilkinson HN, Hardman MJ. Wound healing: cellular mechanisms and pathological outcomes. Open Biol. 2020;10:200223. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 142] [Cited by in RCA: 840] [Article Influence: 168.0] [Reference Citation Analysis (0)] |
| 4. | Patel S, Srivastava S, Singh MR, Singh D. Mechanistic insight into diabetic wounds: Pathogenesis, molecular targets and treatment strategies to pace wound healing. Biomed Pharmacother. 2019;112:108615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 244] [Cited by in RCA: 571] [Article Influence: 95.2] [Reference Citation Analysis (0)] |
| 5. | Sen CK. Human Wound and Its Burden: Updated 2020 Compendium of Estimates. Adv Wound Care (New Rochelle). 2021;10:281-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 581] [Cited by in RCA: 516] [Article Influence: 129.0] [Reference Citation Analysis (0)] |
| 6. | Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB, Stein C, Basit A, Chan JCN, Mbanya JC, Pavkov ME, Ramachandaran A, Wild SH, James S, Herman WH, Zhang P, Bommer C, Kuo S, Boyko EJ, Magliano DJ. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. 2022;183:109119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3033] [Cited by in RCA: 4762] [Article Influence: 1587.3] [Reference Citation Analysis (36)] |
| 7. | Ogurtsova K, Guariguata L, Barengo NC, Ruiz PL, Sacre JW, Karuranga S, Sun H, Boyko EJ, Magliano DJ. IDF diabetes Atlas: Global estimates of undiagnosed diabetes in adults for 2021. Diabetes Res Clin Pract. 2022;183:109118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 436] [Article Influence: 145.3] [Reference Citation Analysis (0)] |
| 8. | Burgess JL, Wyant WA, Abdo Abujamra B, Kirsner RS, Jozic I. Diabetic Wound-Healing Science. Medicina (Kaunas). 2021;57. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 226] [Cited by in RCA: 334] [Article Influence: 83.5] [Reference Citation Analysis (1)] |
| 9. | Zhang P, Lu J, Jing Y, Tang S, Zhu D, Bi Y. Global epidemiology of diabetic foot ulceration: a systematic review and meta-analysis †. Ann Med. 2017;49:106-116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 666] [Cited by in RCA: 980] [Article Influence: 122.5] [Reference Citation Analysis (4)] |
| 10. | Tsourdi E, Barthel A, Rietzsch H, Reichel A, Bornstein SR. Current aspects in the pathophysiology and treatment of chronic wounds in diabetes mellitus. Biomed Res Int. 2013;2013:385641. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 114] [Cited by in RCA: 130] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 11. | Spampinato SF, Caruso GI, De Pasquale R, Sortino MA, Merlo S. The Treatment of Impaired Wound Healing in Diabetes: Looking among Old Drugs. Pharmaceuticals (Basel). 2020;13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 226] [Article Influence: 45.2] [Reference Citation Analysis (0)] |
| 12. | Brem H, Tomic-Canic M. Cellular and molecular basis of wound healing in diabetes. J Clin Invest. 2007;117:1219-1222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1013] [Cited by in RCA: 1169] [Article Influence: 64.9] [Reference Citation Analysis (0)] |
| 13. | Pastar I, Ojeh N, Glinos GD, Stojadinovic O, Tomic-Canic M. Physiology and Pathophysiology of Wound Healing in Diabetes. In: The Diabetic Foot. 2018: 109-130. [DOI] [Full Text] |
| 14. | Maruyama K, Asai J, Ii M, Thorne T, Losordo DW, D'Amore PA. Decreased macrophage number and activation lead to reduced lymphatic vessel formation and contribute to impaired diabetic wound healing. Am J Pathol. 2007;170:1178-1191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 324] [Cited by in RCA: 364] [Article Influence: 20.2] [Reference Citation Analysis (0)] |
| 15. | Okizaki S, Ito Y, Hosono K, Oba K, Ohkubo H, Amano H, Shichiri M, Majima M. Suppressed recruitment of alternatively activated macrophages reduces TGF-β1 and impairs wound healing in streptozotocin-induced diabetic mice. Biomed Pharmacother. 2015;70:317-325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 96] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 16. | Falanga V. Wound healing and its impairment in the diabetic foot. Lancet. 2005;366:1736-1743. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1532] [Cited by in RCA: 1651] [Article Influence: 82.6] [Reference Citation Analysis (1)] |
| 17. | LoGerfo FW, Coffman JD. Current concepts. Vascular and microvascular disease of the foot in diabetes. Implications for foot care. N Engl J Med. 1984;311:1615-1619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 349] [Cited by in RCA: 269] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 18. | Dinh T, Veves A. Microcirculation of the diabetic foot. Curr Pharm Des. 2005;11:2301-2309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 87] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 19. | Dinh TL, Veves A. A review of the mechanisms implicated in the pathogenesis of the diabetic foot. Int J Low Extrem Wounds. 2005;4:154-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 86] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 20. | Lima AL, Illing T, Schliemann S, Elsner P. Cutaneous Manifestations of Diabetes Mellitus: A Review. Am J Clin Dermatol. 2017;18:541-553. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 112] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 21. | Andrade TAM, Masson-Meyers DS, Caetano GF, Terra VA, Ovidio PP, Jordão-Júnior AA, Frade MAC. Skin changes in streptozotocin-induced diabetic rats. Biochem Biophys Res Commun. 2017;490:1154-1161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 44] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 22. | Kim JH, Yoon NY, Kim DH, Jung M, Jun M, Park HY, Chung CH, Lee K, Kim S, Park CS, Liu KH, Choi EH. Impaired permeability and antimicrobial barriers in type 2 diabetes skin are linked to increased serum levels of advanced glycation end-product. Exp Dermatol. 2018;27:815-823. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 46] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 23. | Blakytny R, Jude EB. Altered molecular mechanisms of diabetic foot ulcers. Int J Low Extrem Wounds. 2009;8:95-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 89] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 24. | Ryan MC, Lee K, Miyashita Y, Carter WG. Targeted disruption of the LAMA3 gene in mice reveals abnormalities in survival and late stage differentiation of epithelial cells. J Cell Biol. 1999;145:1309-1323. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 256] [Cited by in RCA: 250] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 25. | Ramirez HA, Liang L, Pastar I, Rosa AM, Stojadinovic O, Zwick TG, Kirsner RS, Maione AG, Garlick JA, Tomic-Canic M. Comparative Genomic, MicroRNA, and Tissue Analyses Reveal Subtle Differences between Non-Diabetic and Diabetic Foot Skin. PLoS One. 2015;10:e0137133. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 50] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 26. | Maione AG, Smith A, Kashpur O, Yanez V, Knight E, Mooney DJ, Veves A, Tomic-Canic M, Garlick JA. Altered ECM deposition by diabetic foot ulcer-derived fibroblasts implicates fibronectin in chronic wound repair. Wound Repair Regen. 2016;24:630-643. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 90] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 27. | Liang L, Stone RC, Stojadinovic O, Ramirez H, Pastar I, Maione AG, Smith A, Yanez V, Veves A, Kirsner RS, Garlick JA, Tomic-Canic M. Integrative analysis of miRNA and mRNA paired expression profiling of primary fibroblast derived from diabetic foot ulcers reveals multiple impaired cellular functions. Wound Repair Regen. 2016;24:943-953. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 67] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 28. | Maione AG, Brudno Y, Stojadinovic O, Park LK, Smith A, Tellechea A, Leal EC, Kearney CJ, Veves A, Tomic-Canic M, Mooney DJ, Garlick JA. Three-dimensional human tissue models that incorporate diabetic foot ulcer-derived fibroblasts mimic in vivo features of chronic wounds. Tissue Eng Part C Methods. 2015;21:499-508. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 67] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 29. | Berlanga-Acosta J, Mendoza-Mari Y, Martínez MD, Valdés-Perez C, Ojalvo AG, Armstrong DG. Expression of cell proliferation cycle negative regulators in fibroblasts of an ischemic diabetic foot ulcer. A clinical case report. Int Wound J. 2013;10:232-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 30. | Caballero S, Sengupta N, Afzal A, Chang KH, Li Calzi S, Guberski DL, Kern TS, Grant MB. Ischemic vascular damage can be repaired by healthy, but not diabetic, endothelial progenitor cells. Diabetes. 2007;56:960-967. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 203] [Cited by in RCA: 197] [Article Influence: 10.9] [Reference Citation Analysis (1)] |
| 31. | Liu ZJ, Velazquez OC. Hyperoxia, endothelial progenitor cell mobilization, and diabetic wound healing. Antioxid Redox Signal. 2008;10:1869-1882. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 216] [Cited by in RCA: 201] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 32. | Yu CG, Zhang N, Yuan SS, Ma Y, Yang LY, Feng YM, Zhao D. Endothelial Progenitor Cells in Diabetic Microvascular Complications: Friends or Foes? Stem Cells Int. 2016;2016:1803989. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 33. | Mirza RE, Fang MM, Novak ML, Urao N, Sui A, Ennis WJ, Koh TJ. Macrophage PPARγ and impaired wound healing in type 2 diabetes. J Pathol. 2015;236:433-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 124] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 34. | Krisp C, Jacobsen F, McKay MJ, Molloy MP, Steinstraesser L, Wolters DA. Proteome analysis reveals antiangiogenic environments in chronic wounds of diabetes mellitus type 2 patients. Proteomics. 2013;13:2670-2681. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 83] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 35. | Liu Y, Min D, Bolton T, Nubé V, Twigg SM, Yue DK, McLennan SV. Increased matrix metalloproteinase-9 predicts poor wound healing in diabetic foot ulcers. Diabetes Care. 2009;32:117-119. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 245] [Cited by in RCA: 272] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 36. | Lobmann R, Ambrosch A, Schultz G, Waldmann K, Schiweck S, Lehnert H. Expression of matrix-metalloproteinases and their inhibitors in the wounds of diabetic and non-diabetic patients. Diabetologia. 2002;45:1011-1016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 396] [Cited by in RCA: 409] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 37. | Obrosova IG. Update on the pathogenesis of diabetic neuropathy. Curr Diab Rep. 2003;3:439-445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 54] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 38. | Wang C, Li C, Peng H, Ye Z, Zhang J, Liu X, Lou T. Activation of the Nrf2-ARE pathway attenuates hyperglycemia-mediated injuries in mouse podocytes. Cell Physiol Biochem. 2014;34:891-902. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 30] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 39. | Lee YJ, Kwon SB, An JM, Kim CH, Lee SH, Choi CY, Nam DH, Park JW, Nam HS, Lee MW, Cho MK. Increased protein oxidation and decreased expression of nuclear factor E2-related factor 2 protein in skin tissue of patients with diabetes. Clin Exp Dermatol. 2015;40:192-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 40. | Long M, Rojo de la Vega M, Wen Q, Bharara M, Jiang T, Zhang R, Zhou S, Wong PK, Wondrak GT, Zheng H, Zhang DD. An Essential Role of NRF2 in Diabetic Wound Healing. Diabetes. 2016;65:780-793. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 144] [Cited by in RCA: 192] [Article Influence: 21.3] [Reference Citation Analysis (0)] |
| 41. | Fadini GP, Menegazzo L, Rigato M, Scattolini V, Poncina N, Bruttocao A, Ciciliot S, Mammano F, Ciubotaru CD, Brocco E, Marescotti MC, Cappellari R, Arrigoni G, Millioni R, Vigili de Kreutzenberg S, Albiero M, Avogaro A. NETosis Delays Diabetic Wound Healing in Mice and Humans. Diabetes. 2016;65:1061-1071. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 228] [Article Influence: 25.3] [Reference Citation Analysis (0)] |
| 42. | Deng L, Du C, Song P, Chen T, Rui S, Armstrong DG, Deng W. The Role of Oxidative Stress and Antioxidants in Diabetic Wound Healing. Oxid Med Cell Longev. 2021;2021:8852759. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 368] [Cited by in RCA: 305] [Article Influence: 76.3] [Reference Citation Analysis (0)] |
| 43. | Yamaoka H, Sasaki H, Yamasaki H, Ogawa K, Ohta T, Furuta H, Nishi M, Nanjo K. Truncal pruritus of unknown origin may be a symptom of diabetic polyneuropathy. Diabetes Care. 2010;33:150-155. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 70] [Cited by in RCA: 55] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 44. | Decker P, Muller S. Modulating poly (ADP-ribose) polymerase activity: potential for the prevention and therapy of pathogenic situations involving DNA damage and oxidative stress. Curr Pharm Biotechnol. 2002;3:275-283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 176] [Cited by in RCA: 170] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 45. | Caporali A, Meloni M, Völlenkle C, Bonci D, Sala-Newby GB, Addis R, Spinetti G, Losa S, Masson R, Baker AH, Agami R, le Sage C, Condorelli G, Madeddu P, Martelli F, Emanueli C. Deregulation of microRNA-503 contributes to diabetes mellitus-induced impairment of endothelial function and reparative angiogenesis after limb ischemia. Circulation. 2011;123:282-291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 336] [Cited by in RCA: 314] [Article Influence: 22.4] [Reference Citation Analysis (0)] |
| 46. | Rafehi H, El-Osta A, Karagiannis TC. Epigenetic mechanisms in the pathogenesis of diabetic foot ulcers. J Diabetes Complications. 2012;26:554-561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 26] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 47. | Madhyastha R, Madhyastha H, Nakajima Y, Omura S, Maruyama M. MicroRNA signature in diabetic wound healing: promotive role of miR-21 in fibroblast migration. Int Wound J. 2012;9:355-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 134] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 48. | Wang X, Cao Q, Yu L, Shi H, Xue B. Epigenetic regulation of macrophage polarization and inflammation by DNA methylation in obesity. JCI Insight. 2016;1:e87748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 152] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 49. | Yan J, Tie G, Wang S, Tutto A, DeMarco N, Khair L, Fazzio TG, Messina LM. Diabetes impairs wound healing by Dnmt1-dependent dysregulation of hematopoietic stem cells differentiation towards macrophages. Nat Commun. 2018;9:33. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 99] [Cited by in RCA: 157] [Article Influence: 22.4] [Reference Citation Analysis (0)] |
| 50. | Ling L, Ren M, Yang C, Lao G, Chen L, Luo H, Feng Z, Yan L. Role of site-specific DNA demethylation in TNFα-induced MMP9 expression in keratinocytes. J Mol Endocrinol. 2013;50:279-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 51. | Zhang J, Yang C, Wang C, Liu D, Lao G, Liang Y, Sun K, Luo H, Tan Q, Ren M, Yan L. AGE-induced keratinocyte MMP-9 expression is linked to TET2-mediated CpG demethylation. Wound Repair Regen. 2016;24:489-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 38] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 52. | Dhawan S, Tschen SI, Zeng C, Guo T, Hebrok M, Matveyenko A, Bhushan A. DNA methylation directs functional maturation of pancreatic β cells. J Clin Invest. 2015;125:2851-2860. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 130] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 53. | Chen Z, Miao F, Paterson AD, Lachin JM, Zhang L, Schones DE, Wu X, Wang J, Tompkins JD, Genuth S, Braffett BH, Riggs AD; DCCT/EDIC Research Group, Natarajan R. Epigenomic profiling reveals an association between persistence of DNA methylation and metabolic memory in the DCCT/EDIC type 1 diabetes cohort. Proc Natl Acad Sci U S A. 2016;113:E3002-E3011. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 169] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 54. | Robert I, Aussems M, Keutgens A, Zhang X, Hennuy B, Viatour P, Vanstraelen G, Merville MP, Chapelle JP, de Leval L, Lambert F, Dejardin E, Gothot A, Chariot A. Matrix Metalloproteinase-9 gene induction by a truncated oncogenic NF-kappaB2 protein involves the recruitment of MLL1 and MLL2 H3K4 histone methyltransferase complexes. Oncogene. 2009;28:1626-1638. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 34] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 55. | Carson WF 4th, Cavassani KA, Soares EM, Hirai S, Kittan NA, Schaller MA, Scola MM, Joshi A, Matsukawa A, Aronoff DM, Johnson CN, Dou Y, Gallagher KA, Kunkel SL. The STAT4/MLL1 Epigenetic Axis Regulates the Antimicrobial Functions of Murine Macrophages. J Immunol. 2017;199:1865-1874. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 56. | Wang X, Zhu K, Li S, Liao Y, Du R, Zhang X, Shu HB, Guo AY, Li L, Wu M. MLL1, a H3K4 methyltransferase, regulates the TNFα-stimulated activation of genes downstream of NF-κB. J Cell Sci. 2012;125:4058-4066. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 49] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 57. | Kimball AS, Joshi A, Carson WF 4th, Boniakowski AE, Schaller M, Allen R, Bermick J, Davis FM, Henke PK, Burant CF, Kunkel SL, Gallagher KA. The Histone Methyltransferase MLL1 Directs Macrophage-Mediated Inflammation in Wound Healing and Is Altered in a Murine Model of Obesity and Type 2 Diabetes. Diabetes. 2017;66:2459-2471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 76] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 58. | Gallagher KA, Joshi A, Carson WF, Schaller M, Allen R, Mukerjee S, Kittan N, Feldman EL, Henke PK, Hogaboam C, Burant CF, Kunkel SL. Epigenetic changes in bone marrow progenitor cells influence the inflammatory phenotype and alter wound healing in type 2 diabetes. Diabetes. 2015;64:1420-1430. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 131] [Cited by in RCA: 158] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 59. | De Santa F, Totaro MG, Prosperini E, Notarbartolo S, Testa G, Natoli G. The histone H3 Lysine-27 demethylase Jmjd3 Links inflammation to inhibition of polycomb-mediated gene silencing. Cell. 2007;130:1083-1094. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 696] [Cited by in RCA: 762] [Article Influence: 42.3] [Reference Citation Analysis (1)] |
| 60. | Zimmermann M, Aguilera FB, Castellucci M, Rossato M, Costa S, Lunardi C, Ostuni R, Girolomoni G, Natoli G, Bazzoni F, Tamassia N, Cassatella MA. Chromatin remodelling and autocrine TNFα are required for optimal interleukin-6 expression in activated human neutrophils. Nat Commun. 2015;6:6061. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 80] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 61. | Na J, Shin JY, Jeong H, Lee JY, Kim BJ, Kim WS, Yune TY, Ju BG. JMJD3 and NF-κB-dependent activation of Notch1 gene is required for keratinocyte migration during skin wound healing. Sci Rep. 2017;7:6494. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 47] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 62. | den Dekker A, Davis FM, Kunkel SL, Gallagher KA. Targeting epigenetic mechanisms in diabetic wound healing. Transl Res. 2019;204:39-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 159] [Article Influence: 26.5] [Reference Citation Analysis (0)] |
| 63. | Thimmappaiah Jagadeesh A, Prakash PY, Karthik Rao N, Ramya V. Culture characterization of the skin microbiome in Type 2 diabetes mellitus: A focus on the role of innate immunity. Diabetes Res Clin Pract. 2017;134:1-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 64. | Dörr S, Holland-Letz AK, Weisser G, Chatzitomaris A, Lobmann R. Bacterial Diversity, Antibiotic Resistance, and the Risk of Lower Limb Amputation in Younger and Older Individuals With Diabetic Foot Infection. Int J Low Extrem Wounds. 2021;1534734621992290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 65. | Radzieta M, Sadeghpour-Heravi F, Peters TJ, Hu H, Vickery K, Jeffries T, Dickson HG, Schwarzer S, Jensen SO, Malone M. A multiomics approach to identify host-microbe alterations associated with infection severity in diabetic foot infections: a pilot study. NPJ Biofilms Microbiomes. 2021;7:29. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 32] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 66. | Gardner SE, Hillis SL, Heilmann K, Segre JA, Grice EA. The neuropathic diabetic foot ulcer microbiome is associated with clinical factors. Diabetes. 2013;62:923-930. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 200] [Cited by in RCA: 223] [Article Influence: 18.6] [Reference Citation Analysis (0)] |
| 67. | van Asten SA, La Fontaine J, Peters EJ, Bhavan K, Kim PJ, Lavery LA. The microbiome of diabetic foot osteomyelitis. Eur J Clin Microbiol Infect Dis. 2016;35:293-298. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 58] [Cited by in RCA: 73] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 68. | Ezeani IU, Ugwu ET, Adeleye FO, Gezawa ID, Okpe IO, Enamino MI. Determinants of wound healing in patients hospitalized for diabetic foot ulcer: results from the MEDFUN study. Endocr Regul. 2020;54:207-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 69. | Sumitomo T, Mori Y, Nakamura Y, Honda-Ogawa M, Nakagawa S, Yamaguchi M, Matsue H, Terao Y, Nakata M, Kawabata S. Streptococcal Cysteine Protease-Mediated Cleavage of Desmogleins Is Involved in the Pathogenesis of Cutaneous Infection. Front Cell Infect Microbiol. 2018;8:10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 70. | Greener B, Hughes AA, Bannister NP, Douglass J. Proteases and pH in chronic wounds. J Wound Care. 2005;14:59-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 112] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 71. | McArdle CD, Lagan KM, McDowell DA. Effects of pH on the Antibiotic Resistance of Bacteria Recovered from Diabetic Foot Ulcer Fluid An In Vitro Study. J Am Podiatr Med Assoc. 2018;108:6-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 72. | Armstrong DG, Lavery LA. Diabetic foot ulcers: prevention, diagnosis and classification. Am Fam Physician. 1998;57:1325-1332, 1337. [PubMed] |
| 73. | Bowering CK. Diabetic foot ulcers. Pathophysiology, assessment, and therapy. Can Fam Physician. 2001;47:1007-1016. [PubMed] |
| 74. | Frykberg RG. Diabetic foot ulcers: pathogenesis and management. Am Fam Physician. 2002;66:1655-1662. [PubMed] |
| 75. | Lavery LA, Peters EJ, Williams JR, Murdoch DP, Hudson A, Lavery DC; International Working Group on the Diabetic Foot. Reevaluating the way we classify the diabetic foot: restructuring the diabetic foot risk classification system of the International Working Group on the Diabetic Foot. Diabetes Care. 2008;31:154-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 105] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 76. | Schaper NC, Nabuurs-Franssen MH. The diabetic foot: pathogenesis and clinical evaluation. Semin Vasc Med. 2002;2:221-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 77. | Searles JM Jr, Colen LB. Foot reconstruction in diabetes mellitus and peripheral vascular insufficiency. Clin Plast Surg. 1991;18:467-483. [PubMed] |
| 78. | Boulton AJ, Kirsner RS, Vileikyte L. Clinical practice. Neuropathic diabetic foot ulcers. N Engl J Med. 2004;351:48-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 394] [Cited by in RCA: 331] [Article Influence: 15.8] [Reference Citation Analysis (1)] |
| 79. | Chand G, Mishra AK, Kumar S, Agarwal A. Diabetic foot. Clinl Queries Nephrol. 2012;2:144-150. |
| 80. | Vallianou N, Evangelopoulos A, Koutalas P. Alpha-lipoic Acid and diabetic neuropathy. Rev Diabet Stud. 2009;6:230-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 67] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 81. | Benrath J, Zimmermann M, Gillardon F. Substance P and nitric oxide mediate would healing of ultraviolet photodamaged rat skin: evidence for an effect of nitric oxide on keratinocyte proliferation. Neurosci Lett. 1995;200:17-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 64] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 82. | Ghersi G, Chen W, Lee EW, Zukowska Z. Critical role of dipeptidyl peptidase IV in neuropeptide Y-mediated endothelial cell migration in response to wounding. Peptides. 2001;22:453-458. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 92] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 83. | Peleg AY, Weerarathna T, McCarthy JS, Davis TM. Common infections in diabetes: pathogenesis, management and relationship to glycaemic control. Diabetes Metab Res Rev. 2007;23:3-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 326] [Cited by in RCA: 348] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 84. | Smith K, Collier A, Townsend EM, O'Donnell LE, Bal AM, Butcher J, Mackay WG, Ramage G, Williams C. One step closer to understanding the role of bacteria in diabetic foot ulcers: characterising the microbiome of ulcers. BMC Microbiol. 2016;16:54. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 96] [Cited by in RCA: 98] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 85. | Basu Mallik S, Jayashree BS, Shenoy RR. Epigenetic modulation of macrophage polarization- perspectives in diabetic wounds. J Diabetes Complications. 2018;32:524-530. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 63] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 86. | Kwon KT, Armstrong DG. Microbiology and Antimicrobial Therapy for Diabetic Foot Infections. Infect Chemother. 2018;50:11-20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 65] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 87. | Brownlee M. The pathobiology of diabetic complications: a unifying mechanism. Diabetes. 2005;54:1615-1625. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3494] [Cited by in RCA: 3615] [Article Influence: 180.8] [Reference Citation Analysis (0)] |
| 88. | Alavi A, Sibbald RG, Mayer D, Goodman L, Botros M, Armstrong DG, Woo K, Boeni T, Ayello EA, Kirsner RS. Diabetic foot ulcers: Part I. Pathophysiology and prevention. J Am Acad Dermatol. 2014;70:1.e1-18; quiz 19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 193] [Article Influence: 17.5] [Reference Citation Analysis (0)] |
| 89. | Tsalamandris S, Antonopoulos AS, Oikonomou E, Papamikroulis GA, Vogiatzi G, Papaioannou S, Deftereos S, Tousoulis D. The Role of Inflammation in Diabetes: Current Concepts and Future Perspectives. Eur Cardiol. 2019;14:50-59. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 952] [Cited by in RCA: 834] [Article Influence: 139.0] [Reference Citation Analysis (0)] |
| 90. | Loot MA, Kenter SB, Au FL, van Galen WJ, Middelkoop E, Bos JD, Mekkes JR. Fibroblasts derived from chronic diabetic ulcers differ in their response to stimulation with EGF, IGF-I, bFGF and PDGF-AB compared to controls. Eur J Cell Biol. 2002;81:153-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 154] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 91. | Nishikori Y, Shiota N, Okunishi H. The role of mast cells in cutaneous wound healing in streptozotocin-induced diabetic mice. Arch Dermatol Res. 2014;306:823-835. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 32] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 92. | Tellechea A, Leal EC, Kafanas A, Auster ME, Kuchibhotla S, Ostrovsky Y, Tecilazich F, Baltzis D, Zheng Y, Carvalho E, Zabolotny JM, Weng Z, Petra A, Patel A, Panagiotidou S, Pradhan-Nabzdyk L, Theoharides TC, Veves A. Mast Cells Regulate Wound Healing in Diabetes. Diabetes. 2016;65:2006-2019. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 90] [Cited by in RCA: 117] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 93. | Bevan D, Gherardi E, Fan TP, Edwards D, Warn R. Diverse and potent activities of HGF/SF in skin wound repair. J Pathol. 2004;203:831-838. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 101] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 94. | Singh K, Agrawal NK, Gupta SK, Mohan G, Chaturvedi S, Singh K. Decreased expression of heat shock proteins may lead to compromised wound healing in type 2 diabetes mellitus patients. J Diabetes Complications. 2015;29:578-588. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 95. | Luong M, Zhang Y, Chamberlain T, Zhou T, Wright JF, Dower K, Hall JP. Stimulation of TLR4 by recombinant HSP70 requires structural integrity of the HSP70 protein itself. J Inflamm (Lond). 2012;9:11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 96. | Park KH, Han SH, Hong JP, Han SK, Lee DH, Kim BS, Ahn JH, Lee JW. Topical epidermal growth factor spray for the treatment of chronic diabetic foot ulcers: A phase III multicenter, double-blind, randomized, placebo-controlled trial. Diabetes Res Clin Pract. 2018;142:335-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 63] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 97. | Barrientos S, Stojadinovic O, Golinko MS, Brem H, Tomic-Canic M. Growth factors and cytokines in wound healing. Wound Repair Regen. 2008;16:585-601. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2237] [Cited by in RCA: 2535] [Article Influence: 149.1] [Reference Citation Analysis (2)] |
| 98. | Greenhalgh DG, Sprugel KH, Murray MJ, Ross R. PDGF and FGF stimulate wound healing in the genetically diabetic mouse. Am J Pathol. 1990;136:1235-1246. [PubMed] |
| 99. | Doxey DL, Ng MC, Dill RE, Iacopino AM. Platelet-derived growth factor levels in wounds of diabetic rats. Life Sci. 1995;57:1111-1123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 73] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 100. | Li H, Fu X, Zhang L, Huang Q, Wu Z, Sun T. Research of PDGF-BB gel on the wound healing of diabetic rats and its pharmacodynamics. J Surg Res. 2008;145:41-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 53] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 101. | Lobmann R, Zemlin C, Motzkau M, Reschke K, Lehnert H. Expression of matrix metalloproteinases and growth factors in diabetic foot wounds treated with a protease absorbent dressing. J Diabetes Complications. 2006;20:329-335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 101] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 102. | Curran MP, Plosker GL. Bilayered bioengineered skin substitute (Apligraf): a review of its use in the treatment of venous leg ulcers and diabetic foot ulcers. BioDrugs. 2002;16:439-455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 76] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 103. | Tsuboi R, Rifkin DB. Recombinant basic fibroblast growth factor stimulates wound healing in healing-impaired db/db mice. J Exp Med. 1990;172:245-251. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 221] [Cited by in RCA: 239] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 104. | Connolly DT, Stoddard BL, Harakas NK, Feder J. Human fibroblast-derived growth factor is a mitogen and chemoattractant for endothelial cells. Biochem Biophys Res Commun. 1987;144:705-712. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 58] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 105. | Kurokawa M, Nakamura H, inventors; Polypeptide with epidermal regeneration accelerating minimal amino acid sequences, a polyalkylenepolyamine and/or polyarylenepolyamine, and a sheet. United States patent 7576051. 2009 August 18.. |
| 106. | Presta LG, Chen H, O'Connor SJ, Chisholm V, Meng YG, Krummen L, Winkler M, Ferrara N. Humanization of an anti-vascular endothelial growth factor monoclonal antibody for the therapy of solid tumors and other disorders. Cancer Res. 1997;57:4593-4599. [PubMed] |
| 107. | Zhou K, Ma Y, Brogan MS. Chronic and non-healing wounds: The story of vascular endothelial growth factor. Med Hypotheses. 2015;85:399-404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 48] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 108. | Angelo LS, Kurzrock R. Vascular endothelial growth factor and its relationship to inflammatory mediators. Clin Cancer Res. 2007;13:2825-2830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 204] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 109. | Hardwicke JT, Hart J, Bell A, Duncan R, Thomas DW, Moseley R. The effect of dextrin-rhEGF on the healing of full-thickness, excisional wounds in the (db/db) diabetic mouse. J Control Release. 2011;152:411-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 66] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 110. | Brown DL, Kane CD, Chernausek SD, Greenhalgh DG. Differential expression and localization of insulin-like growth factors I and II in cutaneous wounds of diabetic and nondiabetic mice. Am J Pathol. 1997;151:715-724. [PubMed] |
| 111. | Bruhn-Olszewska B, Korzon-Burakowska A, Gabig-Cimińska M, Olszewski P, Węgrzyn A, Jakóbkiewicz-Banecka J. Molecular factors involved in the development of diabetic foot syndrome. Acta Biochim Pol. 2012;59:507-513. [PubMed] |
| 112. | Bhora FY, Dunkin BJ, Batzri S, Aly HM, Bass BL, Sidawy AN, Harmon JW. Effect of growth factors on cell proliferation and epithelialization in human skin. J Surg Res. 1995;59:236-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 121] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 113. | Armstrong DG, Jude EB. The role of matrix metalloproteinases in wound healing. J Am Podiatr Med Assoc. 2002;92:12-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 236] [Cited by in RCA: 231] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 114. | Lobmann R, Pap T, Ambrosch A, Waldmann K, König W, Lehnert H. Differential effects of PDGF-BB on matrix metalloproteases and cytokine release in fibroblasts of Type 2 diabetic patients and normal controls in vitro. J Diabetes Complications. 2006;20:105-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 115. | Gary Sibbald R, Woo KY. The biology of chronic foot ulcers in persons with diabetes. Diabetes Metab Res Rev. 2008;24 Suppl 1:S25-S30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 113] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 116. | Dash NR, Dash SN, Routray P, Mohapatra S, Mohapatra PC. Targeting nonhealing ulcers of lower extremity in human through autologous bone marrow-derived mesenchymal stem cells. Rejuvenation Res. 2009;12:359-366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 217] [Cited by in RCA: 227] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 117. | Yang M, Sheng L, Zhang TR, Li Q. Stem cell therapy for lower extremity diabetic ulcers: where do we stand? Biomed Res Int. 2013;2013:462179. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 45] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 118. | Chong HC, Chan JS, Goh CQ, Gounko NV, Luo B, Wang X, Foo S, Wong MT, Choong C, Kersten S, Tan NS. Angiopoietin-like 4 stimulates STAT3-mediated iNOS expression and enhances angiogenesis to accelerate wound healing in diabetic mice. Mol Ther. 2014;22:1593-1604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 95] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 119. | Laing T, Hanson R, Chan F, Bouchier-Hayes D. Effect of pravastatin on experimental diabetic wound healing. J Surg Res. 2010;161:336-340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 26] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 120. | Bagheri M, Jahromi BM, Mirkhani H, Solhjou Z, Noorafshan A, Zamani A, Amirghofran Z. Azelnidipine, a new calcium channel blocker, promotes skin wound healing in diabetic rats. J Surg Res. 2011;169:e101-e107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 30] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 121. | Leu JG, Chiang MH, Chen CY, Lin JT, Chen HM, Chen YL, Liang YJ. Adenine accelerated the diabetic wound healing by PPAR delta and angiogenic regulation. Eur J Pharmacol. 2018;818:569-577. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 122. |
Lee Y, Chang JJ, Yang MC, Chien CT, Lai, WF Acceleration of wound healing in diabetic rats by layered hydrogel dressing.
|
| 123. | Aly UF. Preparation and evaluation of novel topical gel preparations for wound healing in diabetics. Int J Pharm Pharm Sci. 2012;4:76-77. |
| 124. | Moon KC, Lee JS, Han SK, Lee HW, Dhong ES. Effects of human umbilical cord blood-derived mesenchymal stromal cells and dermal fibroblasts on diabetic wound healing. Cytotherapy. 2017;19:821-828. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 125. | Dixon D, Edmonds M. Managing Diabetic Foot Ulcers: Pharmacotherapy for Wound Healing. Drugs. 2021;81:29-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 121] [Article Influence: 24.2] [Reference Citation Analysis (0)] |
| 126. | Ramirez-Acuña JM, Cardenas-Cadena SA, Marquez-Salas PA, Garza-Veloz I, Perez-Favila A, Cid-Baez MA, Flores-Morales V, Martinez-Fierro ML. Diabetic Foot Ulcers: Current Advances in Antimicrobial Therapies and Emerging Treatments. Antibiotics (Basel). 2019;8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 84] [Article Influence: 14.0] [Reference Citation Analysis (3)] |
| 127. | Kavitha KV, Tiwari S, Purandare VB, Khedkar S, Bhosale SS, Unnikrishnan AG. Choice of wound care in diabetic foot ulcer: A practical approach. World J Diabetes. 2014;5:546-556. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 83] [Cited by in RCA: 94] [Article Influence: 8.5] [Reference Citation Analysis (3)] |
| 128. | Tecilazich F, Dinh TL, Veves A. Emerging drugs for the treatment of diabetic ulcers. Expert Opin Emerg Drugs. 2013;18:207-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 40] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 129. | Karri VV, Kuppusamy G, Talluri SV, Yamjala K, Mannemala SS, Malayandi R. Current and emerging therapies in the management of diabetic foot ulcers. Curr Med Res Opin. 2016;32:519-542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 46] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 130. | Hingorani A, LaMuraglia GM, Henke P, Meissner MH, Loretz L, Zinszer KM, Driver VR, Frykberg R, Carman TL, Marston W, Mills JL Sr, Murad MH. The management of diabetic foot: A clinical practice guideline by the Society for Vascular Surgery in collaboration with the American Podiatric Medical Association and the Society for Vascular Medicine. J Vasc Surg. 2016;63:3S-21S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 267] [Cited by in RCA: 361] [Article Influence: 40.1] [Reference Citation Analysis (0)] |
| 131. | Everett E, Mathioudakis N. Update on management of diabetic foot ulcers. Ann N Y Acad Sci. 2018;1411:153-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 430] [Cited by in RCA: 507] [Article Influence: 72.4] [Reference Citation Analysis (1)] |
| 132. | Nayak C, Singh V, Singh K, Singh H, Gupta J, Ali MS, Ponnam HB. A prospective observational study to ascertain the role of homeopathic therapy in the management of diabetic foot ulcer. Indian J Res Homoeopathy. 2012;6:22-31. |
| 133. | Ponnam HB, Gupta J. Role of silicea in diabetic foot ulcer: A retrospectively analysed case series. Homœopathic Links. 2020;33:53-58. [DOI] [Full Text] |
| 134. | Huang YY, Lin CW, Cheng NC, Cazzell SM, Chen HH, Huang KF, Tung KY, Huang HL, Lin PY, Perng CK, Shi B, Liu C, Ma Y, Cao Y, Li Y, Xue Y, Yan L, Li Q, Ning G, Chang SC. Effect of a Novel Macrophage-Regulating Drug on Wound Healing in Patients With Diabetic Foot Ulcers: A Randomized Clinical Trial. JAMA Netw Open. 2021;4:e2122607. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 73] [Article Influence: 18.3] [Reference Citation Analysis (0)] |
| 135. | Bagher ALM, Ramin H, Bahrami A, Delshad H, Ranjbar Omrani G, Mohammad K, Heydarpour R, Mohajeri Tehrani MR, Kamali K, Farhadi M, Gharib Doust F, Madani SH. Effects of intravenous semelil (angiparstm) on diabetic foot ulcers healing: A multicenter clinical trial. DARU J Pharma Sci. 2008;16:35-40. |
| 136. | Nasiri M, Fayazi S, Jahani S, Yazdanpanah L, Haghighizadeh MH. The effect of topical olive oil on the healing of foot ulcer in patients with type 2 diabetes: a double-blind randomized clinical trial study in Iran. J Diabetes Metab Disord. 2015;14:38. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 28] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 137. | Viswanathan V, Kesavan R, Kavitha KV, Kumpatla S. A pilot study on the effects of a polyherbal formulation cream on diabetic foot ulcers. Indian J Med Res. 2011;134:168-173. [PubMed] |
| 138. | Masoompour SM, Bagheri MH, Borhani Haghighi A, Novitsky YA, Sadeghi B, Gharibdoust F, Larijani B, Ranjbar Omrani G. Effect of ANGIPARS™, a new herbal drug on diabetic foot ulcer: A phase 2 clinical study. DARU. 2008;16:31-34. |
| 139. | Mohammadi MH, Molavi B, Mohammadi S, Nikbakht M, Mohammadi AM, Mostafaei S, Norooznezhad AH, Ghorbani Abdegah A, Ghavamzadeh A. Evaluation of wound healing in diabetic foot ulcer using platelet-rich plasma gel: A single-arm clinical trial. Transfus Apher Sci. 2017;56:160-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 53] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 140. | Prakasam N, Prabakar MS, Reshma S, Loganathan K, Senguttuvan K. A clinical study of platelet rich plasma vs conventional dressing in management of diabetic foot ulcers. Int Surg J. 2018;5:3210-3216. [DOI] [Full Text] |
| 141. | Hong JP, Jung HD, Kim YW. Recombinant human epidermal growth factor (EGF) to enhance healing for diabetic foot ulcers. Ann Plast Surg. 2006;56:394-8; discussion 399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 109] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 142. | Viswanathan V, Juttada U, Babu M. Efficacy of Recombinant Human Epidermal Growth Factor (Regen-D 150) in Healing Diabetic Foot Ulcers: A Hospital-Based Randomized Controlled Trial. Int J Low Extrem Wounds. 2020;19:158-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 143. | Rangaswamy P, Rubby SA, Prasanth K. Prospective study of platelet derived growth factor in wound healing of diabetic foot ulcers in Indian population. Int Surg J. 2017;4:194-199. [DOI] [Full Text] |
| 144. | Samuel S, Mahajan A, Mam MK, Prakash JS. Platelet derived growth factor in diabetic lower extremity ulcer: A randomized, double blind, placebo controlled study in Indian condition. Int J Pharm Sci Res. 2016;7:3887-3892. [DOI] [Full Text] |
| 145. | UCHI H, IGARASHI A, URABE K, KOGA T, NAKAYAMA J, KAWAMORI R, TAMAKI K, HIRAKATA H, OHURA T, FURUE M. Clinical efficacy of basic fibroblast growth factor (bFGF) for diabetic ulcer. Eur J Dermatol. 2009;19:461-468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 123] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 146. | Serena TE, Bullock NM, Cole W, Lantis J, Li L, Moore S, Patel K, Sabo M, Wahab N, Price P. Topical oxygen therapy in the treatment of diabetic foot ulcers: a multicentre, open, randomised controlled clinical trial. J Wound Care. 2021;30:S7-S14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 39] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 147. | Löndahl M, Katzman P, Nilsson A, Hammarlund C. Hyperbaric oxygen therapy facilitates healing of chronic foot ulcers in patients with diabetes. Diabetes Care. 2010;33:998-1003. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 259] [Cited by in RCA: 253] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 148. | Maranna H, Lal P, Mishra A, Bains L, Sawant G, Bhatia R, Kumar P, Beg MY. Negative pressure wound therapy in grade 1 and 2 diabetic foot ulcers: A randomized controlled study. Diabetes Metab Syndr. 2021;15:365-371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 21] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 149. | Alamdari NM, Mehraneroodi B, Gholizadeh B, Zeinalpour A, Safe P, Besharat S. The efficacy of negative pressure wound therapy compared with conventional dressing in treating infected diabetic foot ulcers: a randomized controlled trial. Int J Diabetes Dev Ctries. 2021;41:664-668. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 150. | Kaviani A, Djavid GE, Ataie-Fashtami L, Fateh M, Ghodsi M, Salami M, Zand N, Kashef N, Larijani B. A randomized clinical trial on the effect of low-level laser therapy on chronic diabetic foot wound healing: a preliminary report. Photomed Laser Surg. 2011;29:109-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 90] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 151. | Salvi M, Rimini D, Molinari F, Bestente G, Alberto Bruno M. D. Effect of low-level light therapy on diabetic foot ulcers: a near-infrared spectroscopy study. J Biomed Optics. 2017;22:038001. [RCA] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 152. | Omar MT, Alghadir A, Al-Wahhabi KK, Al-Askar AB. Efficacy of shock wave therapy on chronic diabetic foot ulcer: a single-blinded randomized controlled clinical trial. Diabetes Res Clin Pract. 2014;106:548-554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 48] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 153. | Jeppesen SM, Yderstraede KB, Rasmussen BS, Hanna M, Lund L. Extracorporeal shockwave therapy in the treatment of chronic diabetic foot ulcers: a prospective randomised trial. J Wound Care. 2016;25:641-649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 39] [Article Influence: 4.9] [Reference Citation Analysis (1)] |
| 154. | Maksimova N, Krasheninnikov M, Zhang Y, Ponomarev E, Pomytkin I, Melnichenko G, Lyundup A. Early passage autologous mesenchymal stromal cells accelerate diabetic wound re-epithelialization: A clinical case study. Cytotherapy. 2017;19:1548-1550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 155. | Qin HL, Zhu XH, Zhang B, Zhou L, Wang WY. Clinical Evaluation of Human Umbilical Cord Mesenchymal Stem Cell Transplantation After Angioplasty for Diabetic Foot. Exp Clin Endocrinol Diabetes. 2016;124:497-503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 83] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 156. | Edmonds ME, Bodansky HJ, Boulton AJM, Chadwick PJ, Dang CN, D'Costa R, Johnston A, Kennon B, Leese G, Rajbhandari SM, Serena TE, Young MJ, Stewart JE, Tucker AT, Carter MJ. Multicenter, randomized controlled, observer-blinded study of a nitric oxide generating treatment in foot ulcers of patients with diabetes-ProNOx1 study. Wound Repair Regen 2018; 26: 228-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 41] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 157. | Rullan M, Cerdà L, Frontera G, Masmiquel L, Llobera J. Treatment of chronic diabetic foot ulcers with bemiparin: a randomized, triple-blind, placebo-controlled, clinical trial. Diabet Med. 2008;25:1090-1095. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 29] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 158. | Imran M, Hussain MB, Baig M. A Randomized, Controlled Clinical Trial of Honey-Impregnated Dressing for Treating Diabetic Foot Ulcer. J Coll Physicians Surg Pak. 2015;25:721-725. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 159. | Lullove EJ, Liden B, Winters C, McEneaney P, Raphael A, Lantis II JC. A multicenter, blinded, randomized controlled clinical trial evaluating the effect of omega-3–rich fish skin in the treatment of chronic, nonresponsive diabetic foot ulcers. Wounds 2021; 33: 169-177. [RCA] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 42] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 160. | Del Pino-Sedeño T, Trujillo-Martín MM, Andia I, Aragón-Sánchez J, Herrera-Ramos E, Iruzubieta Barragán FJ, Serrano-Aguilar P. Platelet-rich plasma for the treatment of diabetic foot ulcers: A meta-analysis. Wound Repair Regen. 2019;27:170-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 61] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 161. | Golledge J, Thanigaimani S. Novel therapeutic targets for diabetes-related wounds or ulcers: an update on preclinical and clinical research. Expert Opin Ther Targets. 2021;25:1061-1075. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 162. | Mahdipour E, Sahebkar A. The Role of Recombinant Proteins and Growth Factors in the Management of Diabetic Foot Ulcers: A Systematic Review of Randomized Controlled Trials. J Diabetes Res. 2020;2020:6320514. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 163. | Ma C, Hernandez MA, Kirkpatrick VE, Liang LJ, Nouvong AL, Gordon II. Topical platelet-derived growth factor vs placebo therapy of diabetic foot ulcers offloaded with windowed casts: a randomized, controlled trial. Wounds. 2015;27:83-91. [PubMed] |
| 164. | Jaiswal SS, Gambhir RP, Agrawal A, Harish S. Efficacy of topical recombinant human platelet derived growth factor on wound healing in patients with chronic diabetic lower limb ulcers. Indian J Surg. 2010;72:27-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 165. | Liu Y, Liu Y, Deng J, Li W, Nie X. Fibroblast Growth Factor in Diabetic Foot Ulcer: Progress and Therapeutic Prospects. Front Endocrinol (Lausanne). 2021;12:744868. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 119] [Cited by in RCA: 107] [Article Influence: 26.8] [Reference Citation Analysis (0)] |
| 166. | Richard JL, Parer-Richard C, Daures JP, Clouet S, Vannereau D, Bringer J, Rodier M, Jacob C, Comte-Bardonnet M. Effect of topical basic fibroblast growth factor on the healing of chronic diabetic neuropathic ulcer of the foot. A pilot, randomized, double-blind, placebo-controlled study. Diabetes Care. 1995;18:64-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 154] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 167. | Xu J, Min D, Guo G, Liao X, Fu Z. Experimental study of epidermal growth factor and acidic fibroblast growth factor in the treatment of diabetic foot wounds. Exp Ther Med. 2018;15:5365-5370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 168. | Borys S, Hohendorff J, Frankfurter C, Kiec-Wilk B, Malecki MT. Negative pressure wound therapy use in diabetic foot syndrome-from mechanisms of action to clinical practice. Eur J Clin Invest. 2019;49:e13067. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 50] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 169. | Liu S, He CZ, Cai YT, Xing QP, Guo YZ, Chen ZL, Su JL, Yang LP. Evaluation of negative-pressure wound therapy for patients with diabetic foot ulcers: systematic review and meta-analysis. Ther Clin Risk Manag. 2017;13:533-544. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 66] [Cited by in RCA: 81] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 170. | Liu Z, Dumville JC, Hinchliffe RJ, Cullum N, Game F, Stubbs N, Sweeting M, Peinemann F. Negative pressure wound therapy for treating foot wounds in people with diabetes mellitus. Cochrane Database Syst Rev. 2018;10:CD010318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 55] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 171. | Huang J, Chen J, Xiong S, Huang J, Liu Z. The effect of low-level laser therapy on diabetic foot ulcers: A meta-analysis of randomised controlled trials. Int Wound J 2021; 18: 763-776. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 172. | Huang Q, Yan P, Xiong H, Shuai T, Liu J, Zhu L, Lu J, Shi X, Yang K. Extracorporeal Shock Wave Therapy for Treating Foot Ulcers in Adults With Type 1 and Type 2 Diabetes: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Can J Diabetes. 2020;44:196-204.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 173. | Yu Q, Qiao GH, Wang M, Yu L, Sun Y, Shi H, Ma TL. Stem Cell-Based Therapy for Diabetic Foot Ulcers. Front Cell Dev Biol. 2022;10:812262. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 42] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 174. | Ahmed R, Augustine R, Chaudhry M, Akhtar UA, Zahid AA, Tariq M, Falahati M, Ahmad IS, Hasan A. Nitric oxide-releasing biomaterials for promoting wound healing in impaired diabetic wounds: State of the art and recent trends. Biomed Pharmacother. 2022;149:112707. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 63] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 175. | Kong M, Xie K, Lv M, Li J, Yao J, Yan K, Wu X, Xu Y, Ye D. Anti-inflammatory phytochemicals for the treatment of diabetes and its complications: Lessons learned and future promise. Biomed Pharmacother. 2021;133:110975. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 62] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 176. | Carvalho MTB, Araújo-Filho HG, Barreto AS, Quintans-Júnior LJ, Quintans JSS, Barreto RSS. Wound healing properties of flavonoids: A systematic review highlighting the mechanisms of action. Phytomedicine. 2021;90:153636. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 76] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 177. | Oguntibeju OO. Medicinal plants and their effects on diabetic wound healing. Vet World. 2019;12:653-663. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 37] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 178. | Gallelli G, Cione E, Serra R, Leo A, Citraro R, Matricardi P, Di Meo C, Bisceglia F, Caroleo MC, Basile S, Gallelli L. Nano-hydrogel embedded with quercetin and oleic acid as a new formulation in the treatment of diabetic foot ulcer: A pilot study. Int Wound J. 2020;17:485-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 72] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 179. | Majumdar K, Dtta NK, Dastidar SG, Motohashi N, Shirataki Y. Phytochemical isoflavones against diabetic foot bacteria. Adv Tradit Med. 2004;4:261-266. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 180. | Thanganadar Appapalam S, Paul B, Arockiasamy S, Panchamoorthy R. Phytofabricated silver nanoparticles: Discovery of antibacterial targets against diabetic foot ulcer derived resistant bacterial isolates. Mater Sci Eng C Mater Biol Appl. 2020;117:111256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |