Published online May 15, 2022. doi: 10.4239/wjd.v13.i5.387
Peer-review started: May 31, 2021
First decision: July 3, 2021
Revised: July 18, 2021
Accepted: April 28, 2022
Article in press: April 28, 2022
Published online: May 15, 2022
Processing time: 346 Days and 20.6 Hours
Diabetic complications, chiefly seen in long-term situations, are persistently deleterious to a large extent, requiring multi-factorial risk reduction strategies beyond glycemic control. Diabetic cardiomyopathy is one of the most common deleterious diabetic complications, being the leading cause of mortality among diabetic patients. The mechanisms of diabetic cardiomyopathy are multi-factorial, involving increased oxidative stress, accumulation of advanced glycation end products (AGEs), activation of various pro-inflammatory and cell death signaling pathways, and changes in the composition of extracellular matrix with enhanced cardiac fibrosis. The novel lipid signaling system, the endocannabinoid system, has been implicated in the pathogenesis of diabetes and its complications through its two main receptors: Cannabinoid receptor type 1 and cannabinoid receptor type 2, alongside other components. However, the role of the endocannabinoid system in diabetic cardiomyopathy has not been fully investigated. This review aims to elucidate the possible mechanisms through which cannabinoids and the endocannabinoid system could interact with the pathogenesis and the development of diabetic cardiomyopathy. These mechanisms include oxidative/ nitrative stress, inflammation, accumulation of AGEs, cardiac remodeling, and autophagy. A better understanding of the role of cannabinoids and the endocannabinoid system in diabetic cardiomyopathy may provide novel strategies to manipulate such a serious diabetic complication.
Core Tip: Diabetic cardiomyopathy is considered to be one of the most common deleterious diabetic complications being the leading cause of mortality among diabetic patients. The endocannabinoid system has been implicated in the pathogenesis of diabetes and its complications. However, the role of the endocannabinoid system in diabetic cardiomyopathy has not been fully investigated. This review aims to elucidate the possible mechanisms through which cannabinoids and the endocannabinoid system could interact with the pathogenesis of diabetic cardiomyopathy. Better understanding of the role of cannabinoids and the endocannabinoid system in diabetic cardiomyopathy may provide novel strategies to manipulate this serious diabetic complication.
- Citation: El-Azab MF, Wakiel AE, Nafea YK, Youssef ME. Role of cannabinoids and the endocannabinoid system in modulation of diabetic cardiomyopathy. World J Diabetes 2022; 13(5): 387-407
- URL: https://www.wjgnet.com/1948-9358/full/v13/i5/387.htm
- DOI: https://dx.doi.org/10.4239/wjd.v13.i5.387
Diabetes mellitus is one of the most common chronic disorders worldwide, and it continues to increase in number and significance. The total number of individuals with diabetes worldwide is 463 million, with a prevalence rate of 9.3% according to the International Diabetes Federation[1]. It is estimated that the prevalence of diabetes on a global scale could reach 578 million by 2030 and 700 million by 2045. In 2017, diabetes-related mortality accounted for 4 million people worldwide and the total healthcare expenditure reached 727 billion United States Dollars[2].
Diabetes mellitus is a complex metabolic condition that is characterized by hyperglycemia resulting from a lack of absolute or relative insulin[3]. It is linked to insulin resistance in many instances. Type 1 diabetes is caused by an autoimmune destruction of insulin-secreting cells in the pancreas, and type 2 diabetes is caused by insufficient compensatory insulin production in the presence of peripheral insulin resistance. Ninety percent of diabetes cases are of the latter type[4].
Both microvascular (retinopathy, nephropathy, and neuropathy)[5-9] and macrovascular (cardiovascular disease) problems are linked to diabetes[6-10]. Despite substantial advances in anti-diabetic therapy, diabetic complications, which are most commonly recognized in the long-term, are consistently harmful to a large extent, necessitating multi-factorial risk reduction measures beyond glycemic control[11]. Diabetes-related morbidity and mortality are primarily caused by cardiovascular problems[12]. Indeed, 50% of diabetic patients die of a cardiovascular disease[13]. Endothelial dysfunction, coronary artery disease, and myocardial left ventricular dysfunction (which leads to heart failure) are all well-known cardiovascular problems[14]. Diabetic patients have a 2-4 times higher risk of heart failure than non-diabetic patients, according to clinical research[15,16].
Diabetic cardiomyopathy is a deficiency in ventricular contractile function that occurs in diabetic individuals regardless of the presence of coronary artery disease or other cardiovascular disorders. It is a complicated diabetes-related condition marked by severe alterations in the heart's physiology, anatomy, and mechanical performance[17]. Diabetic cardiomyopathy is a complicated and poorly understood process. To explain the structural and functional alterations associated with diabetic cardiomyopathy, several pathogenic processes have been explored and suggested[18]. Increased oxidative/nitrative stress[19-21], accumulation of advanced glycation end products (AGEs)[22], activation of various pro-inflammatory and cell death signaling pathways[23], and changes in the composition of extracellular matrix with elevated cardiac fibrosis[24] are some of the proposed pathological mechanisms. Unfortunately, despite the growing body of information concerning diabetic cardiomyopathy over the last few decades, therapeutic choices remain inadequate. Other treatments for diabetic cardiomyopathy's multi-factorial pathogenic pathways have yet to be developed.
The endocannabinoid system is an endogenous lipid signaling system that consists of: (1) Two main receptors identified as cannabinoid receptor type 1 (CB1) and cannabinoid receptor type 2 (CB2); (2) Endogenous ligands for these two receptors known as endocannabinoids; and (3) Proteins that control endocannabinoid tissue levels (anabolic and catabolic enzymes)[25]. The endocannabinoid system has become a novel therapeutic target in a range of cardiovascular illnesses in the last decade, including atherosclerosis, myocardial infarction, and heart failure[26]. Furthermore, the significance of the endocannabinoid system in the development of diabetes and associated consequences has been suggested in various pre-clinical and clinical research[27-29]. The possible mechanisms through which cannabinoids and the endocannabinoid system could modulate the pathogenesis of diabetic cardiomyopathy are highlighted in this review (Table 1), an approach that could pave the way for the use of this system as an effective tool in the management of these harmful diabetic complications.
| Cannabinoid agent | Mechanism | Role in diabetes |
| Anandamide | Endogenous cannabinoid | Elevated in diabetic patients[26] |
| CB1 agonist | ||
| CB2 agonist | ||
| Rimonabant (SR141716A) | CB1 antagonist | Reduced weight[62] |
| Reduced hemoglobin A1c levels[62] | ||
| Reduced fasting blood glucose levels[62] | ||
| Reduced high density lipoprotein, cholesterol and triglyceride levels[62] | ||
| Improved systolic blood pressure[62] | ||
| Δ9-tetrahydrocannabinol (THC) | Psychoactive cannabinoid | Lowered blood glucose level[65]; Preserved pancreatic insulin content[65] |
| CB1 partial agonist | ||
| CB2 partial agonist | ||
| Cannabidiol | Non-psychoactive cannabinoid | Reduced the incidence of type I diabetes[66] |
| Low affinity to CB1 and CB2 | Immunosuppressive effect[66] |
Cardiomyopathies are a group of diseases characterized by myocardial dysfunction that is not induced by common causes, such as coronary artery disease, valvular dysfunction, or hypertension. Cardiomyopathies are divided into four categories depending on hemodynamic characteristics: Dilated, hypertrophic, restrictive, and obliterative cardiomyopathy[30]. Dilated cardiomyopathy is characterized by ventricular dilatation and systolic dysfunction, which commonly affects both ventricles. The most common symptom of hypertrophic cardiomyopathy is significant ventricular hypertrophy. Restrictive cardiomyopathy is characterized by inflexible and poorly distensible myocardium, resulting in poor compliance. Endo-myocardial fibrosis is a symptom of obliterative cardiomyopathy. The endocardium's severe fibrosis encroaches on and reduces the size of the ventricular cavities[31]. Diabetic cardiomyopathy can be classified as either dilated or hypertrophied cardiomyopathy[32].
Rubler et al[33] coined the name diabetic cardiomyopathy in 1972 after observing a specific type of cardiomyopathy in diabetic patients who did not have other cardiovascular issues such as coronary artery disease, valvular or congenital heart disease, or hypertension. Diabetic cardiomyopathy is defined by a series of cardiac alterations, including interstitial fibrosis, myocardial hypertrophy, and microcirculatory abnormalities, that arise due to diabetes mellitus. These circulatory issues impair heart function, eventually leading to cardiac failure[4]. Heart failure lowers an individual's quality of life and makes diabetes control more difficult. As a result, early diagnosis and treatment of these patients are regarded as top priorities[34].
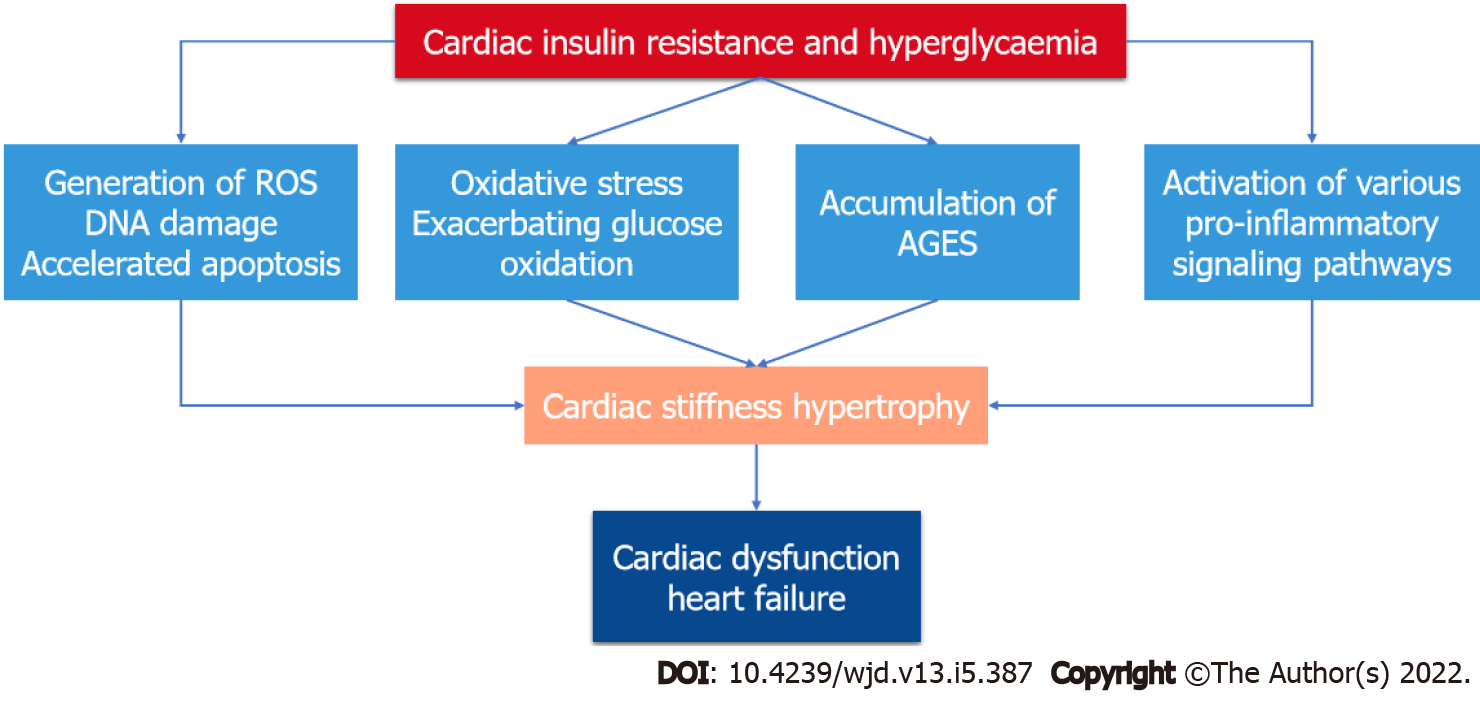
Insulin resistance and hyperglycemia are significant drivers in diabetic patients, activating a variety of adaptive and maladaptive responses that ultimately affect cardiac function[35]. To explain the complicated structural and functional abnormalities associated with diabetic cardiomyopathy, several pathogenic processes have been examined and proposed (Figure 1). These systems work in concert and may even enhance one another[36]. Hyperglycemia increases oxidative stress by accelerating glucose oxidation and mitochondrial production of reactive oxygen species (ROS), which induce DNA damage and promote apoptosis[37]. AGEs build up in tissues, including the myocardium, and have been linked to structural abnormalities in diabetic hearts[22]. Activation of numerous pro-inflammatory and stress signaling pathways, such as mitogen activated protein kinases (MAPKs), also stimulates apoptotic pathways and cell death, and promote myocardial cell death[23,38]. Finally, there is increased collagen formation in the myocardium that leads to fibrosis and reduced contractile function of the heart[24,39].
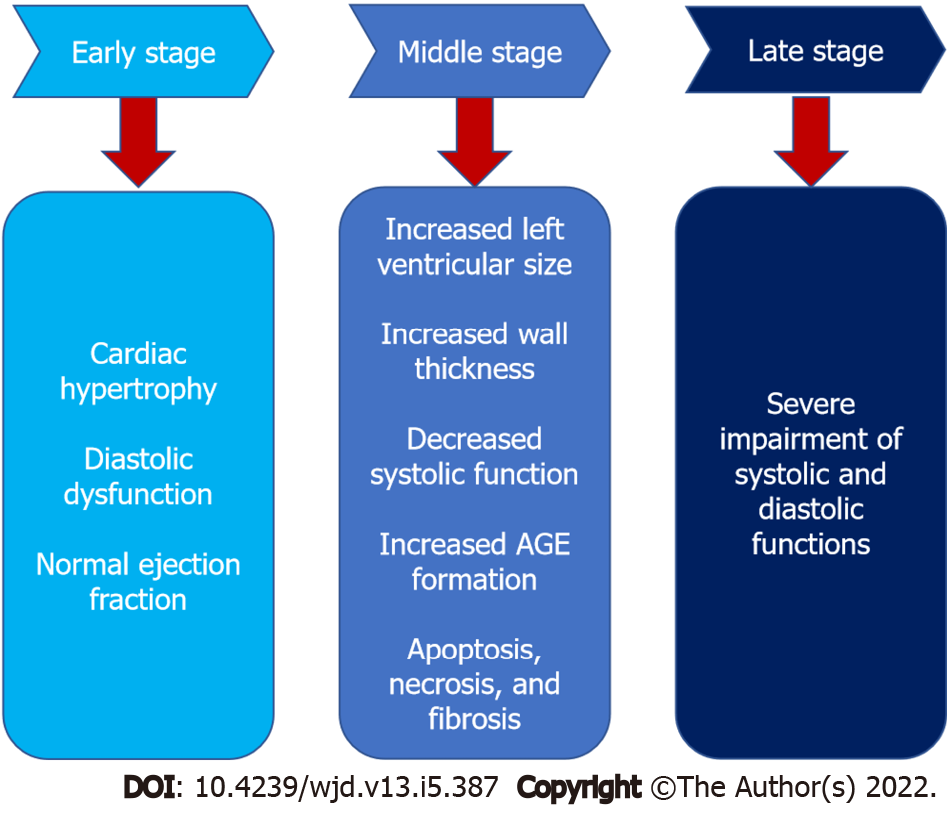
Diabetic cardiomyopathy is divided into three stages (Figure 2): Early-stage, middle-stage, and late-stage[4]. In the early stage, the heart develops hypertrophy and has diastolic dysfunction with normal ejection fraction, and it is asymptomatic[40]. Increased left ventricular size, wall thickness, and mass, as well as diastolic dysfunction and a modest decline in systolic performance, characterize the intermediate stage. Insulin resistance, AGE formation, elevated renin-angiotensin-aldosterone system levels, apoptosis, necrosis, and fibrosis are all associated with this stage[41]. As the disease progresses from the medium to late stage, it becomes more severe, impairing both systolic and diastolic functioning[13].
The discovery of the endogenous signaling system now recognized as the endocannabinoid system began with the chemical detection of 9-tetrahydrocannabinol (THC), the main psychoactive component of Cannabis sativa[42]. THC's psychotropic and immunomodulatory effects are due to the ability to bind to and activate specific receptors, including the CB1 receptor, which is one of the most abundant G-protein-coupled receptors in the central nervous system[43], and the CB2 receptor, which is abundantly expressed in several immune cells and tissues[44].
The existence of endogenous substances (the endocannabinoids) capable of binding to and activating CB1 and CB2 receptors was suggested. Anandamide (N-arachidonoyl ethanolamine)[45] and 2-arachidonoyl glycerol (2-AG)[46] are the two most well-studied examples of these compounds. The endocannabinoid system is made up of cannabinoid receptors, endocannabinoids, and proteins that catalyze endocannabinoid biosynthesis (N-acyl-phosphatidylethanolamine phospholipase-D for anandamide and diacylglycerol lipases for 2-AG), transport, and inactivation [fatty acid amide hydrolase (FAAH) for anandamide and monoacyl glycerol lipase for 2-AG][47]. Signaling via CB1 and CB2 receptors is complex, involving inhibition (and activation in some cases) of adenyl cyclase activity, activation of various MAPKs [e.g., p38- and p44/42-MAPKs, c-Jun N-terminal kinase (JNK) and extracellular signal–regulated kinase (ERK)], protein kinases A and C (PKA and PKC), and modulation of various calcium and potassium channels[48].
Since its discovery about two decades ago, the endocannabinoid system has gained considerable importance as a fundamental signaling system implicated in almost all physiological and pathological processes in animals[49]. In a wide range of pathological conditions, including mood and anxiety disorders, movement disorders, neuropathic pain, multiple sclerosis, cancer, glaucoma, osteoporosis, reproductive disorders, immune dysfunction, cardiovascular and metabolic disorders, there is growing evidence that the endocannabinoid system plays pivotal roles and holds tremendous therapeutic options[50,51].
Besides the primary distribution of CB1 receptors in the CNS and CB2 receptors in immune cells, as these are responsible for the psychoactive and immunomodulatory effects of cannabinoids, both receptors have been found to be expressed in cardiovascular system cells such as cardiomyocytes, fibroblasts, endothelial and vascular smooth muscle cells, and infiltrating immune cells[26]. CB1 receptors activation by endocannabinoids or synthetic ligands has complex depressive effects in the cardiovascular system and has been linked to the development of pathophysiological alterations and compromised cardiovascular function in various forms of shock[51] and heart failure[52]. In addition, several studies indicated that stimulation of CB1 receptors in the cells of the cardiovascular system is associated with activation of stress signaling pathways promoting cell death, ROS production, and induction of inflammatory cascades[26,52]. On the other hand, an increased CB2 receptor expression has been reported in the cardiovascular system under pathophysiological conditions such as inflammatory stimulation or tissue injury, which likely reflects a protective response to limit these effects[53]. A great body of evidence suggest a protective role of CB2 receptors in experimental models of cardiovascular disorders including mouse models of atherosclerosis[54], restenosis[55] and myocardial ischemia/ reperfusion injury[56].
Different expression patterns of CB1 and CB2 receptors together with other components of the endocannabinoid system such as synthesizing and degrading enzymes have been reported in islet cells of humans, rats and mice[57-59]. There are controversial results regarding the role of CB1 receptors in insulin secretion with studies showing an increased insulin secretion in islet cells by activation of CB1 receptors[57,58], and others showing decreased insulin secretion[60]. In addition, activation of CB2 receptors in islet cells has also been shown to either stimulate[61] or attenuate insulin secretion[57]. Several studies have found that the endocannabinoid system plays a significant role in the etiology of diabetes. Serum levels of anandamide and 2-AG have been found to be greater in type 2 diabetics than in healthy individuals[27]. Furthermore, in these diabetic patients, subcutaneous tissue levels of anandamide were found to be elevated, indicating endocannabinoid system overactivity[28].
A clinical trial was conducted in obese patients with type 2 diabetes inadequately controlled by either metformin or sulfonylureas using the CB1 antagonist rimonabant (SR141716A). Rimonabant treatment caused a reduction in weight, hemoglobin A1c levels, fasting blood glucose, high-density lipoprotein cholesterol and triglycerides, as well as improvement in systolic blood pressure[62]. In the type 2 diabetic patients naive to anti-diabetic treatment, rimonabant showed similar results with improved glycemic control and metabolic profile[63]. Another study demonstrated that the treatment of type 2 diabetic patients on standard insulin treatment with rimonabant also improved glycemic control and the metabolic profile[64]. The psychoactive cannabinoid THC was shown to attenuate the severity of autoimmune responses in an experimental model of autoimmune diabetes in addition to lowering blood glucose level and preserving pancreatic insulin content[65]. Unfortunately, the psychoactive effects of THC hampered this therapeutic approach. The non-psychoactive cannabidiol (CBD) reduced the incidence of diabetes in a mouse model of type 1 diabetes, an effect that involved immunosuppressive and anti-inflammatory effects[66].
The majority of diabetic complications are linked to abnormalities in the vascular system[67]. Hyperglycemia has been related to a number of critical processes, including oxidative/nitrative damage, AGE buildup, and inflammatory system stimulation[68]. Endothelial dysfunction occurs in arteries, which contributes to the development of numerous diabetes problems. Indeed, cannabinoids and the endocannabinoid system represent an outstanding therapeutic approach to manage these deleterious complications. Interestingly, this notion is supported by a great body of evidence implicating the endocannabinoid system in the pathogenesis of nearly all diabetic complications including nephropathy, retinopathy, and neuropathy, in addition to cardiovascular complications, mainly through modulation of the aforementioned mechanisms[29]. Still, the role of the endocannabinoid system in diabetic cardiomyopathy; the distinct diabetic complication, has not been fully investigated in detail.
Nearly 95% of oxygen consumed by tissues is used in metabolic processes to produce adenosine triphosphate (ATP), and approximately 5% of oxygen consumed is transformed into superoxide (O2–) radical, the principal oxygen free radical produced by mitochondria[69]. The antioxidant enzymes superoxide dismutase (SOD1, SOD2, and SOD3) quickly convert superoxide to hydrogen peroxide (H2O2) within the cell[70]. Antioxidant enzymes such as catalase, glutathione peroxidase, and other peroxidases generally convert excess H2O2 to harmless water[71]. Although H2O2 is not a free radical, it can undergo the Fenton reaction with reduced transition metals [e.g., ferrous ion (Fe2+)] or with superoxide in the presence of metal ions (usually iron or copper) to produce the highly reactive hydroxyl radical (OH), which is a far more damaging molecule to the cell[72]. Superoxide radicals can quickly react with nitric oxide (NO) to produce cytotoxic peroxynitrite anions (ONOO–) in addition to producing H2O2[73]. Superoxide and NO are less reactive than peroxynitrite, which might combine with carbon dioxide to generate nitrotyrosine, that triggers protein degradation and lipid oxidation[74].
Besides mitochondria, other cellular sources of reactive oxygen and nitrogen species (RNS) exist. NADPH oxidase, for example, promotes the enzymatic conversion of oxygen to superoxide anion. Several critical cytosolic proteins (p44phox, p67phox, p40phox, and Rac2) must be translocated to the cellular membrane for NADPH oxidase activation[75]. Other sources of ROS and RNS, in addition to NADPH oxidase, include nitric oxide synthase (NOS), which stimulates NO synthesis[76], and peroxisomes, that are known to create H2O2 primarily through fatty acid oxidation[77] and phagocytic cell activation[78].
The oxidative stress pathway has emerged as a common thread connecting all major diabetic cardiomyopathy pathophysiological mechanisms[79]. These pathways are the result of a single hyperglycemia-induced process: The overproduction of superoxide by the mitochondrial electron transport chain[80]. Formation of AGE products, auto-oxidation of glucose, activation of PKC, and NADPH oxidase are some of the other sources of ROS in diabetes[81]. Once oxidative stress develops, it results in a vicious self-sustaining cycle of generating more free radicals and causing more stress as a result of the activation of multiple stress-induced pathways and due to its ability to cause damaging effects to multiple components within the cell[82].
Through a variety of mechanisms, ROS induce cellular damage in the diabetic myocardium. Increased ROS directly damage cellular proteins and DNA[83]. In addition, ROS activate matrix metalloproteinases, which modify the extracellular matrix architecture and cause fibrosis[84], as well as regulating signal transduction pathways that cause cardiomyocyte hypertrophy[85] and apoptosis, which results in the loss of contractile tissue[86]. In a similar manner, peroxynitrite induces vasoconstriction, enhanced leukocyte adherence, platelet activation, oxidation, pro-thrombotic state, impaired coagulation, and vascular inflammation, among other pro-atherosclerotic pathogenic processes[87]. In type 1 diabetic mice, selective suppression of mitochondrial ROS was demonstrated to prevent diabetic cardiac abnormalities, confirming the importance of mitochondrial ROS role in developing cardiac abnormalities[88]. Moreover, Rac1 increases mitochondrial ROS generation via NADPH oxidase activation and plays an important role in cardiomyocyte death and cardiac failure in streptozotocin-induced diabetes in mice[89].
Previous studies have shown that the endocannabinoid system can influence ROS and RNS production, implying that modulating the endocannabinoid system and administering exogenous cannabinoids with antioxidant properties could be beneficial in the treatment of diabetes-related cardiovascular complications, such as diabetic cardiomyopathy[29].
It has been shown that genetic deletion of CB1 receptors attenuated the rise in markers of oxidative [4-hydroxy-trans-2-nonenal (4-HNE)] and nitrative (nitrotyrosine) stress in the myocardium of mice treated with acute or chronic doses of the potent, cardio-toxicant, anticancer drug doxorubicin[90]. In addition, doxorubicin treatment led to decreased myocardial content of the components of the antioxidant defense system: Glutathione, glutathione peroxidase, and SOD. These changes were significantly reduced in the myocardium of CB1 knockout mice[90]. Consistent with the data obtained from rodents, activation of CB1 receptors by anandamide or the potent agonist HU210, with or without doxorubicin, induced ROS production in human primary cardiomyocytes (HCM). The previous deleterious effect was attenuated by the use of CB1 antagonists: SR141716A or AM281[90].
Mukhopadhyay et al[52] similarly found that pharmacological blockage of CB1 receptors with AM281 or SR141716A reduced doxorubicin-induced oxidative/nitrative stress and related cell death. In comparison to their wild-type counterparts, mice lacking the FAAH gene showed a significant increase in acute and chronic doxorubicin-induced cardiac oxidative and nitrative stress, as well as impaired antioxidant defense and tissue injury[91]. Furthermore, anandamide increased the sensitivity of inflammatory cells isolated from FAAH mutant mice to ROS generation. These findings imply that, in pathological situations involving oxidative/nitrative stress (such as doxorubicin-induced myocardial injury), FAAH plays an important role in regulating endocannabinoid-induced cardiac cell injury, which is mediated in part by CB1 receptor activation because these effects may be attenuated by selective CB1 antagonists[91].
The role of the endocannabinoid system in oxidative stress control has also been proven in atherosclerosis models such as the apolipoprotein E (ApoE) deficient animal model. In ApoE and CB2 double knockout mice, the release of superoxide radical was increased two-fold in intact aortic segments compared to ApoE knockout mice. The selective CB2 agonist JWH-133 reduced ROS release in ApoE knockout mice to comparable levels to those in wild-type animals[54].
The first evidence of a direct link between the endocannabinoid system and the pathogenesis of diabetic cardiomyopathy came from the interesting study conducted by Rajesh and co-workers in 2011. This research group demonstrated an increased expression of CB1 receptors and anandamide levels in the myocardium of streptozotocin-induced diabetic mice compared to their non-diabetic counterparts[92]. Streptozotocin-induced diabetic cardiomyopathy was characterized by a profound accumulation of markers of oxidative and nitrative stress in the myocardium, an effect that was ameliorated by genetic deletion of CB1 receptors. In addition, genetic deletion of CB1 mitigated the expression of the p40phoxNADPH oxidase active subunit in myocardial tissue of diabetic mice[92].
Earlier, the same research group demonstrated a protective effect of CBD in diabetic cardiomyopathy[92]. CBD is the most common non-psychotropic cannabinoid in Cannabis sativa, and it has been approved for the treatment of inflammation, pain, and spasms associated with multiple sclerosis in humans[93]. CBD exerts several actions that are independent of the CB1 and CB2 receptors[94]. In this study, CBD therapy was found to reduce oxidative and nitrative stress in the myocardium of streptozotocin-induced diabetic mice. Additionally, CBD was found to reduce ROS production as well as the expression of active ROS-generating NADPH oxidase isoforms p22phox, p67phox, and gp91phox. It also increased glutathione levels and SOD activity and reduced nitrotyrosine production. These protective effects of CBD against oxidative/nitrative stress were also demonstrated in vitro in human primary cardiomyocytes[95].
In a study published in 2017, Vella et al[96] found that giving cannabinoids to diabetic rats reversed changes in lipid peroxidation and oxidative stress markers, as well as blocking maladaptive alterations in the structure and function of the heart and blood vessels. Similar findings were previously published by Rajesh's group, who reported that administering CBD to diabetic C57BL/6J mice for 11 wk reduced the formation of lipid peroxides, protein carbonyls, and ROS in the heart[95]. Furthermore, the binding site of anandamide has been linked to NO release[97], implying a possible mechanism by which cannabinoids could increase NO bioavailability. THC treatment of STZ-induced diabetic rats resulted in a controlled redox state that granted improvements in end organ function of the myocardium and vasculature[96]. This was demonstrated by preservation of myocardial pump function, cardiac electrophysiology, noradrenergic-mediated contraction, and endothelial-dependent relaxation of resistance arteries. These findings suggested that cannabinoid receptor activation in an experimental type I diabetes animal might be a potential pharmacological target for diabetic cardiomyopathy management[96] (Table 2).
| Cannabinoid agent | Mechanism | Effect |
| Endocannabinoids | Oxidative/Nitrative stress | Influenced ROS and RNS production[28] |
| Myocardial remodeling | Triggered activation of signaling pathways (e.g., p38 and JNK-MAPKs), promoting cell death[50,137] | |
| Inflammation | Increased during inflammation[107] | |
| Modulating T and B lymphocyte proliferation and apoptosis, inflammatory cytokine production and immune cell activation by inflammatory stimuli[107,108,111] | ||
| AM281 | Oxidative/Nitrative stress | Attenuated doxorubicin-induced oxidative stress[52] |
| SR141716A | Oxidative/Nitrative stress | Attenuated doxorubicin-induced oxidative stress[52] |
| Inflammation | Reduced plasma levels of the pro-inflammatory cytokines MCP-1 and IL-12 in low density lipoprotein deficient mice[113] | |
| Inhibited LPS-induced pro-inflammatory IL-6 and TNF-α expression[113] | ||
| Myocardial remodeling | Reduced activation of p38 and JNK/MAPK[90] | |
| Improved myocardial dysfunction induced in a mouse model of diabetic cardiomyopathy[92] | ||
| Reduced markers of cell death (activated caspase-3 and chromatin fragmentation)[92] | ||
| JWH133 | Oxidative/Nitrative stress | Reduced ROS release in ApoE knockout mice[54] |
| Inflammation | Decreased leukocyte recruitment in ApoE-knockout mice[54] | |
| Attenuated TNF-α-induced NF-κB activation[116] | ||
| Attenuated ICAM-1 and VCAM-1 up-regulation[116] | ||
| Cannabidiol | Oxidative/Nitrative stress | Attenuated oxidative and nitrative stress in the myocardium of streptozotocin-induced diabetic mice[93] |
| Prevented changes in markers of lipid peroxidation and oxidative stress in diabetic rats[96] | ||
| Inflammation | Inhibited IκB-α phosphorylation and subsequent p65 NF-κB nuclear translocation[93] | |
| Attenuated high glucose-induced NF-κB activation in primary human cardiomyocytes[93] | ||
| Myocardial remodeling | Attenuated the established systolic and diastolic dysfunction in diabetic mice[93] | |
| Attenuated the activation of stress signaling pathways: p38 and JNK/MAPKs[93] | ||
| Enhanced the activity of the pro-survival AKT pathway in diabetic myocardium[93] | ||
| Decreased the activity of the pro-apoptotic enzyme caspase-3[93] | ||
| Autophagy | Promoted endothelial cell survival via HO-1 mediated autophagy[170] | |
| Anandamide | Oxidative/Nitrative stress | Induced NO bioavailability[97] |
| Myocardial remodeling | Decrease rat heart mitochondrial O2 consumption[135] | |
| Increased activation of p38 and JNK/MAPK, followed by cell death[90] | ||
| Enhanced doxorubicin-induced MAPK activation and cell death[90] | ||
| Δ9-tetrahydrocannabinol (THC) | Oxidative/Nitrative stress | Regulated redox state in diabetic rats[96] |
| Myocardial remodeling | Decreased rat heart mitochondrial O2 consumption[135] | |
| WIN55, 212-2 | Inflammation | Reduced atherosclerotic lesion macrophage content and IL-6 and TNF-α levels[114,115] |
| Reduced adhesion molecules VCAM-1 and ICAM-1 as well as NF-κB activation[114,115] | ||
| HU-308 | Inflammation | Attenuated TNF-α-induced NF-κB activation, ICAM-1 and VCAM-1 up-regulation[116] |
| Decreased endothelial cell activation and suppression of the acute inflammatory response[56,117] | ||
| Autophagy | Enhanced autophagy levels in heart tissues with diabetic cardiomyopathy[171] | |
| Increased AMPK phosphorylation while decreasing the phosphorylation of mTOR[171] | ||
| HU-210 | Myocardial remodeling | Decrease rat heart mitochondrial O2 consumption[135] |
| Increased activation of p38 and JNK/MAPK, followed by cell death[90] | ||
| Enhanced doxorubicin-induced MAPK activation and cell death[90] | ||
| Enhanced left ventricular performance in rats with myocardial infarction[143] | ||
| AM251 | Myocardial remodeling | Improved cardiac function in carbon tetrachloride-induced cirrhosis in rats[140] |
| Reduced activation of p38 and JNK/MAPK[90] |
Inflammation is a complex nonspecific response of vascular tissues to harmful stimuli such as pathogens, damaged cells, or irritants, and it involves several functional and molecular mediators, such as the recruitment and activation of leukocytes such as mast cells, neutrophils, and monocytes/ macrophages. On an acute basis, inflammation is usually good since it represents the organism's defensive attempt to eliminate damaging stimuli and begin the healing process. Inflammation, on the other hand, might have negative consequences if it continues for a long period[98]. The increased expression of many inflammatory proteins is regulated at the level of gene transcription through the activation of pro-inflammatory transcription factors which play a critical role in amplifying and perpetuating the inflammatory process[99].
Activation of the transcription factor nuclear factor-kappa B (NF-κB), which binds to DNA and activates gene transcription, appears to play a pivotal role in the regulation of inducible enzymes such as inducible nitric oxide synthase (iNOS), inflammatory cytokines such as tumor necrosis factor-α (TNF-α), interleukin-1β (IL-1β) and IL-6, prostaglandins, cell adhesion molecules such as intercellular adhesion molecule-1 (ICAM-1) and vascular cell adhesion molecule-1 (VCAM-1), in addition to other substances that are initiators or enhancers of the inflammatory process[100,101]. The aforementioned inflammatory mediators bind to specific target receptors on the cells and may increase vascular permeability, promote inflammatory cell chemotaxis, stimulate smooth muscle contraction, increase direct enzymatic activity, induce pain, and/or mediate oxidative damage[102].
Numerous investigations have indicated that inflammatory processes play a critical role in the development of diabetes macro- and microvascular complications[29,103]. Cardiac inflammation is a common and early symptom of diabetes, and it plays a key role in the progression of heart failure in diabetic cardiomyopathy[104]. Furthermore, various research on the heart of diabetic or diabetic hypertensive rats has shown that NF-κB plays a major role in the development of diabetic cardiomyopathy[105,106].
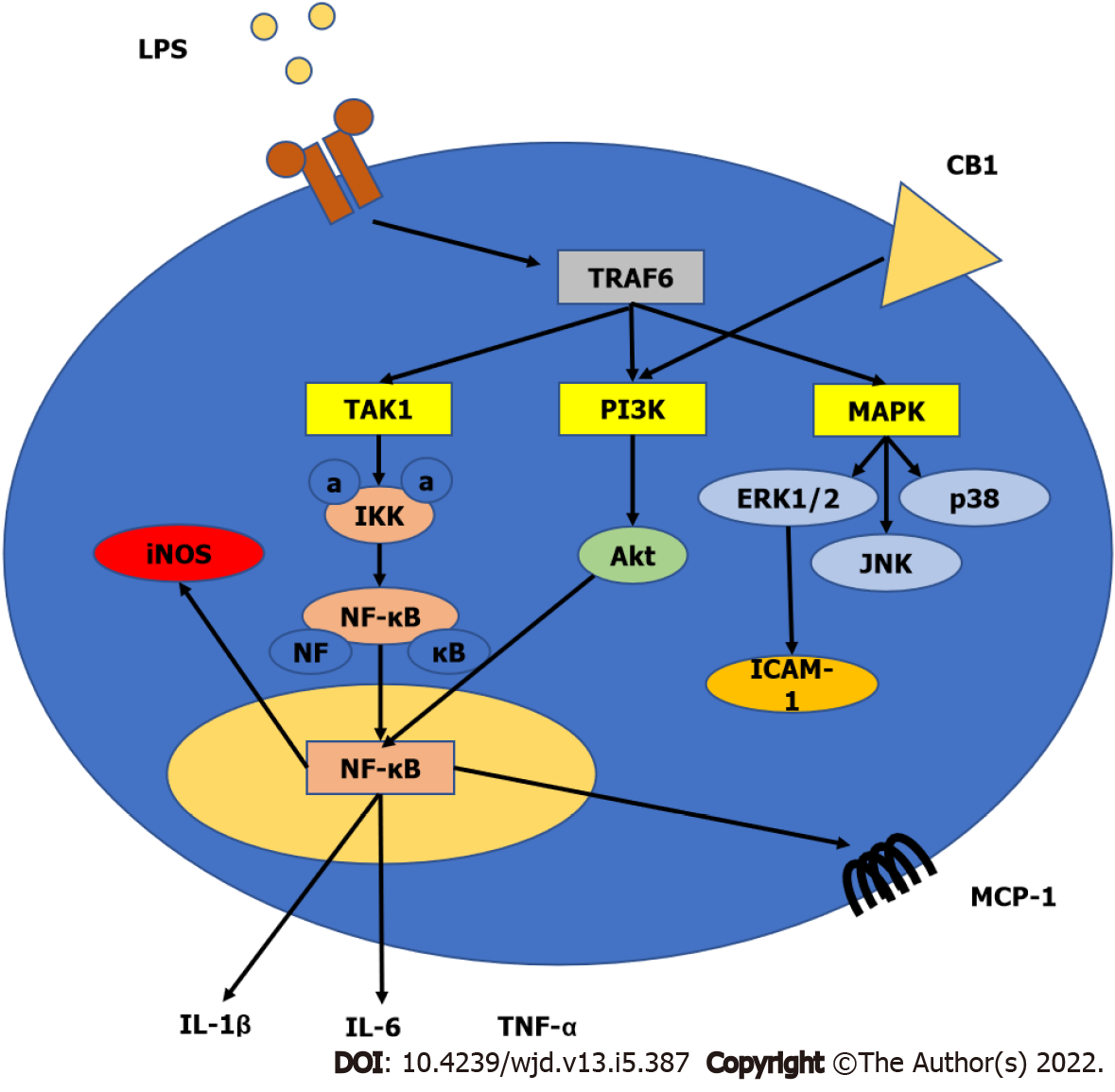
Cannabinoid receptor expression in immune cells can be influenced by various inflammatory factors and other triggers activating these cells[107]. Inflammatory stimuli may potentially boost the synthesis of endocannabinoids in immune cells (e.g., macrophages, monocytes, and dendritic cells) by activating multiple biosynthetic pathways and/or decreasing the expression of metabolic enzymes that degrade them[107,108]. THC and other natural or synthetic cannabinoids have been studied for their immunomodulatory effects in mice and/or rats in vivo, as well as in cultured human immune cells. Overall, cannabinoid ligands exhibit suppressive effects on B-lymphocytes, T-lymphocytes, natural killer cells, and macrophages[109,110], which are most likely due to both CB1 and CB2 receptor-dependent and –independent mechanisms. Other studies have revealed that endocannabinoids can influence immune functions by modulating T and B lymphocyte proliferation and apoptosis, inflammatory cytokine production and immune cells activation in response to inflammatory stimuli, macrophage-mediated killing of sensitized cells, chemotaxis, and inflammatory cell migration[107,110,111]. Furthermore, cannabinoids may influence the expression of iNOS and the formation of ROS in immune cells, which play significant roles in the defense against invading pathogens and in modulation of the inflammatory response[21]. The involvement of cannabinoid receptors in inflammation is shown in Figure 3.
Han et al[112] demonstrated that CB1 receptors promote pro-inflammatory responses of macrophages through ROS production, and subsequent synthesis of TNF-α and monocyte chemoattractant protein-1 (MCP-1). This effect was negatively regulated by CB2 and was attenuated by CB1 blockade. In a mouse model of atherosclerosis, the CB1 antagonist SR141716A (rimonabant) was able to reduce plasma levels of the pro-inflammatory cytokines MCP-1 and IL-12 in low density lipoprotein deficient mice fed with a high fat diet[113]. In addition, rimonabant inhibited lipopolysaccharide (LPS)-induced pro-inflammatory IL-6 and TNF-α expression in mouse peritoneal macrophages in vitro. Importantly, this effect was still observed when cells from CB1-knockout mice were used, suggesting a CB1-independent anti-inflammatory effect of rimonabant[113]. In another model of atherosclerosis, Hoyer and co-workers demonstrated a severe vascular leukocyte infiltration in ApoE and CB2 double knockout mice which was more intense than that observed in ApoE-knockout mice[54]. Interestingly, treatment with the selective CB2 agonist JWH-133 decreased leukocyte recruitment in ApoE-knockout mice compared to their wild-type counterparts[54]. In 2010, Zhao et al[114,115] showed that treatment with the synthetic cannabinoid WIN55,212-2 reduced atherosclerotic lesion macrophage content and mRNA levels of inflammatory markers IL-6 and TNF-α; adhesion molecules VCAM-1 and ICAM-1 as well as NF-κB activation in ApoE-deficient mice fed on high-cholesterol diets. In human coronary artery endothelial cells, activation of CB2 receptors with the selective agonists HU-308 or JWH-133 attenuated the TNF-α-induced NF-κB activation, ICAM-1 and VCAM-1 up-regulation, MCP-1 release, as well as trans-endothelial migration and adhesion of monocytes, which are hallmarks of the development of atherosclerosis[116].
The beneficial effects of CB2 receptor activation by selective synthetic ligands, such as JWH-133 and HU-308, was largely attributed to decreased endothelial cell activation and suppression of the acute inflammatory response in animal models of myocardial ischemia/reperfusion injury, which are characterized by a rapid increase in cytokines and chemokines in addition to an enhanced influx of leukocytes into the vulnerable region. Attenuated expression of adhesion molecules, chemokine secretion, leukocyte chemotaxis, adherence to endothelium, stimulation of trans-endothelial migration, and linked oxidative/nitrative stress associated with reperfusion damage were all beneficial effects of CB2 receptor activation[56,117].
In a mouse model of streptozotocin-induced diabetic cardiomyopathy, which is characterized by up-regulation of the expression of various inflammatory cytokines in the myocardium, genetic deletion, or pharmacological blockade of CB1 receptors resulted in attenuation of the expression of: Inflammatory cytokines such as TNF-α and IL-1β, adhesion molecules such as ICAM-1 and VCAM-1, iNOS, and cyclooxygenase 2 (COX2)[92]. In another study using the same model of diabetic cardiomyopathy, it was shown that there was a marked phosphorylation of the inhibitor of NF-κB (IκB-α) in the cytosol of diabetic hearts, leading to the release of the active p65 subunit of NF-κB, which subsequently translocated to the nucleus to induce the expression of inflammatory and apoptotic genes[95]. Treatment with CBD, the non-psychoactive cannabinoid, inhibited the IκB-α phosphorylation and subsequent p65 NF-κB nuclear translocation. The CBD treatment also inhibited the NF-κB-dependent mRNA and/or protein expression of adhesion molecules (ICAM-1 and VCAM-1), the pro-inflammatory cytokine TNF-α, and iNOS in the diabetic myocardial tissues. Cannabidiol (CBD) was also able to attenuate high glucose-induced NF-κB activation in primary human cardiomyocytes[95] (Table 2).
An important consequence of high glucose-induced cellular injury is the formation of AGEs. AGEs are a heterogeneous group of compounds formed by the non-enzymatic glycation reaction of glucose and other glycating compounds with proteins and, to a lesser extent, lipids, and DNA[118]. In addition, AGEs can easily make covalent cross-linkages (adducts) with macromolecules like proteins and, in this way, can change the structure and function of these proteins[119]. In diabetic patients, the rate of formation of AGEs is increased. Thus, over time, even modest hyperglycemic excursions can result in significant adduct accumulation in long-lived macromolecules[120]. It is now well established that AGEs interact with cell surface receptors and binding proteins to evoke varied downstream responses. These include the pro-inflammatory responses that could play a critical role in the pathogenesis of diabetic complications including cardiomyopathy[121]. The receptor for AGEs (RAGE) is the most established and the best characterized AGE binding protein[122]. The RAGE is a trans-membrane receptor that belongs to the immunoglobulin super-family and is constitutively expressed in a range of tissues including neurons, endothelium, smooth muscle, epithelium, and inflammatory cells[123].
There are two basic methods by which AGEs might alter myocardial function. AGEs, for starters, can form covalent adducts with proteins including collagen, laminin, and elastin[118,124]. As shown in the myocardium of an animal model of type 2 diabetes, this can inhibit collagen degradation, resulting in collagen buildup and fibrosis, producing increased myocardial stiffness, and reduced ventricular relaxation[19]. Second, soluble extracellular AGEs can bind to RAGE, causing up-regulation of transforming growth factor–β (TGF–β) and NADPH oxidase, resulting in the generation of substantial quantities of cytoplasmic and extracellular superoxide, which can then interact with NO to produce RNS[118]. Furthermore, when the RAGE receptor is active, it promotes the transcription factor NF-κB and associated genes by elevating intracellular free radical levels and by triggering multiple other signaling pathways[125].
In the literature, little is known about the interaction of the endocannabinoid system and the AGE and/or RAGE. In a mouse model of streptozotocin-induced diabetic cardiomyopathy, genetic deletion of CB1 receptors attenuated accumulation of AGEs and the expression of RAGE in the myocardium of diabetic mice[92] (Table 2).
Diabetes has a multifactorial nature, therefore there are changes at the cellular and molecular levels that predispose the heart to pathological, structural, and functional remodeling[4]. Diabetic cardiomyopathy is characterized by an unusually increased left ventricular mass and myocardial fibrosis. Left ventricular hypertrophy has been associated with hyperinsulinemia, insulin resistance, increased non-esterified fatty acids, and activation of the renin-angiotensin-aldosterone system[82]. Chronic cardiac remodeling and structural alterations are promoted by a continual cycle of increased ROS production[126,127]. Diastolic dysfunction is defined as an elevation in ventricular wall stiffness and prolonged diastolic relaxation time, and it is common in the early stages of cardiomyopathy[128].
Increased triglyceride buildup and decreased calcium absorption have been linked to diastolic dysfunction[128]. The progression of systolic dysfunction is marked by dilated cardiac remodeling, which leads to heart failure[129]. Cardiomyocyte mortality is accompanied by fibroblast replacement, which leads to interstitial fibrosis driven predominantly by TGF-β[130]. Cardiomyocyte death is mediated by activation of various stress signaling pathways and consequent apoptosis. The deleterious effect of accumulating free fatty acids on mitochondrial biogenesis eventually leads to mitochondrial apoptosis and lowered ATP generation, which is insufficient to meet cardiac demands, resulting in impaired cardiac contractility and lowered ejection fraction[128]. Myocardial dysfunction is caused by impaired endothelial function linked with insulin resistance[13].
Cannabinoid receptors are believed to have the ability to control apoptosis since they may signal through both pro- and anti-apoptotic pathways. Due to the lipophilic nature of their structures, they may be able to operate intracellularly without the help of a membrane transporter[131]. A number of cannabinoid drugs, including HU-210, THC, and anandamide, have been demonstrated to reduce cardiac mitochondrial O2 consumption in rats[132], as well as the role of mitochondria in marijuana-induced cell death[133]. Stimulation of CB1 receptors by endocannabinoids has also been linked to the activation of signaling pathways (e.g., p38 and JNK-MAPKs) and cell death in various clinical circumstances[51,134]. It is reasonable to conclude, based on earlier results and observations of reduced cardiac apoptosis in FAAH-null animals, that endocannabinoids have strong potential for the regulation of apoptosis, and hence remodeling, in the heart[135].
Doxorubicin treatment is linked to increased anandamide levels in the myocardium, but not to alterations in CB1 or CB2 receptor expression[52]. Doxorubicin triggered apoptosis in a cardiac cell line (H9c2) that was reduced by CB1 receptor blockage, but the result was not sensitive to a CB2 blocker or CB1 and CB2 receptor agonists[52]. Similarly, studies on cardiac function suggest that endocannabinoids have a role in cirrhosis-related cardiac dysfunction[136]. AM251, which blocks CB1 receptors, enhanced cardiac function in rats with carbon tetrachloride-induced cirrhosis, and anandamide levels were shown to be elevated in the hearts of cirrhotic rats compared to controls[137]. In contrast, aging-associated cardiac dysfunction is reduced in FAAH-null mice, which could be interpreted as showing a need for increased endocannabinoid activity in the heart[135].
Mukhopadhyay et al[90] demonstrated that genetic deletion of CB1 receptors attenuated cardiac dysfunction induced by doxorubicin in mice. In this study, doxorubicin-induced activation of stress signaling pathways (p-38 and JNK/MAPKs) with subsequent apoptosis was attenuated in CB1 knockout mice. In addition, these findings were supported in vitro in human primary cardiomyocytes as the activation of CB1 receptors by anandamide or HU210 resulted in increased activation of p38 and JNK/MAPK, followed by cell death, which are effects that were attenuated by both selective CB1 antagonists (SR141716A or AM281) and MAPK inhibitors[90]. Furthermore, doxorubicin-induced MAPK activation and cell death in human cardiomyocytes were significantly enhanced when doxorubicin was co-administered with anandamide or HU210, an effect which could also be attenuated by both CB1 antagonists and MAPK inhibitors[90]. Another aspect of doxorubicin-induced cardiotoxicity is the induction of myocardial fibrosis, an effect that was attenuated by genetic deletion of CB1 indicating its role in this model of cardiotoxicity[90]. In another study using the same model of doxorubicin-induced cardiotoxicity in mice, it has been shown that FAAH knockout mice exhibited significantly increased doxorubicin-induced cardiac dysfunction and myocardial cell death compared to their wild-type counterparts. The effects of doxorubicin in FAAH knockouts were attenuated by CB1 receptor antagonists[91].
Acute myocardial infarction causes cardiomyocyte necrosis, which triggers repair mechanisms that result in scarring[138]. This post-infarction cardiac remodeling process involves adaptive changes in the ventricular shape, size, and function, which can lead to contractile dysfunction and heart failure[138]. In ischemic cardiomyocyte death, fibrosis, and cardiac dysfunction, Defer and coworkers showed considerable evidence for the protective impact of CB2 receptors[139]. CB2-knockout mouse hearts displayed larger infarcts and more persistent cell loss 3 d after ischemia, as well as accelerated damage and apoptosis in the non-ischemic remote myocardium compared to wild-type mice[139]. Cardiomyocytes and fibroblasts lacking CB2 were more vulnerable to oxidative stress-induced cell death in vitro. Long-term effects of cardiac remodeling in CB2-knockout hearts involved marked fibrosis, accelerated cardiomyocyte hypertrophy, dilated cardiomyopathy, and cardiac dysfunction, as reported 4 wk post-infarction[139]. On other hand, wild-type post-ischemic hearts acquired mild fibrosis and cardiomyocyte hypertrophy while maintaining cardiac function[139]. Wagner and colleagues revealed another investigation where the administration of the CB1 antagonist AM251 for 12 wk after an experimentally induced infarction exacerbated the decline in left ventricular function, but administration of the non-selective cannabinoid agonist HU-210 improved left ventricular performance[140].
A previous study conducted by Liao and co-workers demonstrated that CB1 deficiency contributed to the exacerbation of chronic cardiac remodeling induced by pressure overload in mice, revealing a new role of CB1 in the pathophysiology of congestive heart failure[141]. Genetic deletion of CB1 was found to worsen left ventricular hemodynamics and exacerbate cardiac hypertrophy compared to wild-type mice. Furthermore, it was found that CB1 deficiency led to enhanced activation of the epidermal growth factor receptor, p38, and ERK/MAPKs, which contributed to the exacerbation of cardiac hypertrophy[141].
In patients with chronic heart failure, clinical data revealed an increase in cardiac CB2 expression as well as increased levels of the endocannabinoids, anandamide, and 2-AG[142]. Additionally, in these patients, cannabinoid receptor expression was also found to be slightly downregulated[142]. It was believed that CB2 up-regulation could have a negative inotropic effect due to lower cyclic adenosine monophosphate (cAMP) levels, which could lead to ventricular weakness. CB2 receptors, on the other hand, may mediate positive inotropic effects via cAMP-independent processes, hence serving as a compensation strategy to sustain heart function[53]. Furthermore, as demonstrated in rats, CB2 upregulation could be a protective response to counteract structural alterations caused by chronic heart failure[139]. Recently, it has been shown that in biopsies collected from the hypertrophic myocardium of patients with aortic stenosis, there were elevated concentrations of anandamide, higher expression of its degrading enzyme FAAH, and of CB2 receptors[143].
Rajesh et al[92] indicated that myocardial dysfunction induced in a mouse model of diabetic cardiomyopathy was improved in CB1-knockout mice or in diabetic mice treated with CB1 antagonists (SR141716A or AM281). This was demonstrated by improved indices of left ventricular systolic and diastolic dysfunction, ejection fraction, contractility, and ventricular stiffness. In the same study, there was attenuated activity of MAPKs and reduced markers of cell death (activated caspase-3 and chromatin fragmentation) in the myocardium of diabetic CB1-knockout mice and in diabetic wild-type mice treated with the CB1 antagonist (SR141716A). Diabetic mice developed myocardial fibrosis as a structural consequence of diabetic cardiomyopathy, and this was characterized by increased accumulation of collagen and enhanced expression of markers of fibrosis such as TGF-β and fibronectin. Interestingly, these changes were attenuated by genetic deletion or pharmacological blockade of CB1 receptors[92]. In another study using the same model, chronic treatment of diabetic mice with the non-psychoactive CBD attenuated the established systolic and diastolic dysfunction in diabetic mice[95]. In addition, CBD treatment attenuated the activation of stress signaling pathways: p38 and JNK/MAPKs. It also enhanced the activity of the pro-survival AKT pathway in diabetic myocardium. Another beneficial effect of CBD treatment in this model was its ability to decrease the activity of the pro-apoptotic enzyme caspase-3 and to reduce the rate of cell death in diabetic myocardium. Finally, CBD treatment protected diabetic myocardium from the deleterious process of fibrosis by decreasing myocardial collagen content and attenuating the expression of fibrosis markers: TGF-β, fibronectin, and the enzyme matrix metalloproteinase[95] (Table 2).
Autophagy, an essential metabolic process, is a self-degradative and recycling procedure dependent on lysosomes. It targets dysfunctional organelles and long-lived proteins[144,145]. This occurs through the biogenesis of double-membrane vesicles containing cytoplasmic components destined for lysosomal degradation, these vesicles are known as autophagosomes[146]. Autophagosome biogenesis entails nucleation, expansion, and closure of the phagophore (a cup-shaped membrane) thereby sequestering cytoplasmic cargo. This is followed by fusion with endolysosomal compartments to facilitate degradation of the sequestered material[146].
Autophagy is performed by genes called autophagy-related (ATG) genes[147]. The discovery of ATG genes in yeast in the 1990s allowed researchers to identify how autophagy works[148]. Today, 36 ATG proteins have been identified as being particularly significant for autophagy, with 18 of them belonging to the basic machinery[149]. Through the Unc-51-like kinases, ULK1 and ULK2 (mammalian homologues of ATG1), two protein kinases (mTOR and AMPK) control autophagy in mammals[150]. The ULK kinases are dephosphorylated and activated when autophagy is induced. Beclin-1 (mammalian ortholog of ATG6), which is part of a protein complex, is phosphorylated and activated by the ULK[151]. The active ULK and Beclin-1 complexes translocate to the phagophore, the site of autophagosome initiation, where they both help to stimulate downstream autophagy components[152].
Autophagosome production requires two ubiquitin-like conjugation mechanisms[153]. The first one covalently binds the ubiquitin-like protein ATG12 to ATG5. The conjugate protein subsequently attaches to ATG16L1, forming an E3-like complex that is part of the second ubiquitin-like conjugation system[154]. This complex binds and activates ATG3, which covalently binds to the mammalian homologues of the ubiquitin-like yeast protein LC3 to the lipid phosphatidylethanolamine (PE) on autophagosome surfaces[155]. Lipidated LC3 aids autophagosome closure[156] and facilitates the docking of particular cargos and adaptor proteins such as Sequestosome-1/p62[157]. The autophagosome then unites with a lysosome to produce an autolysosome. The autolysosome's contents are then destroyed, and their constituents are liberated from the vesicle[158].
Autophagy has a role in the control of cardiovascular disorders such as myocardial infarction and atherosclerosis[159]. Increased autophagy levels have been shown to protect against diabetic cardiomyopathy[160,161]. As a result, pharmacological activation of autophagy might be a promising therapeutic strategy for diabetic cardiomyopathy.
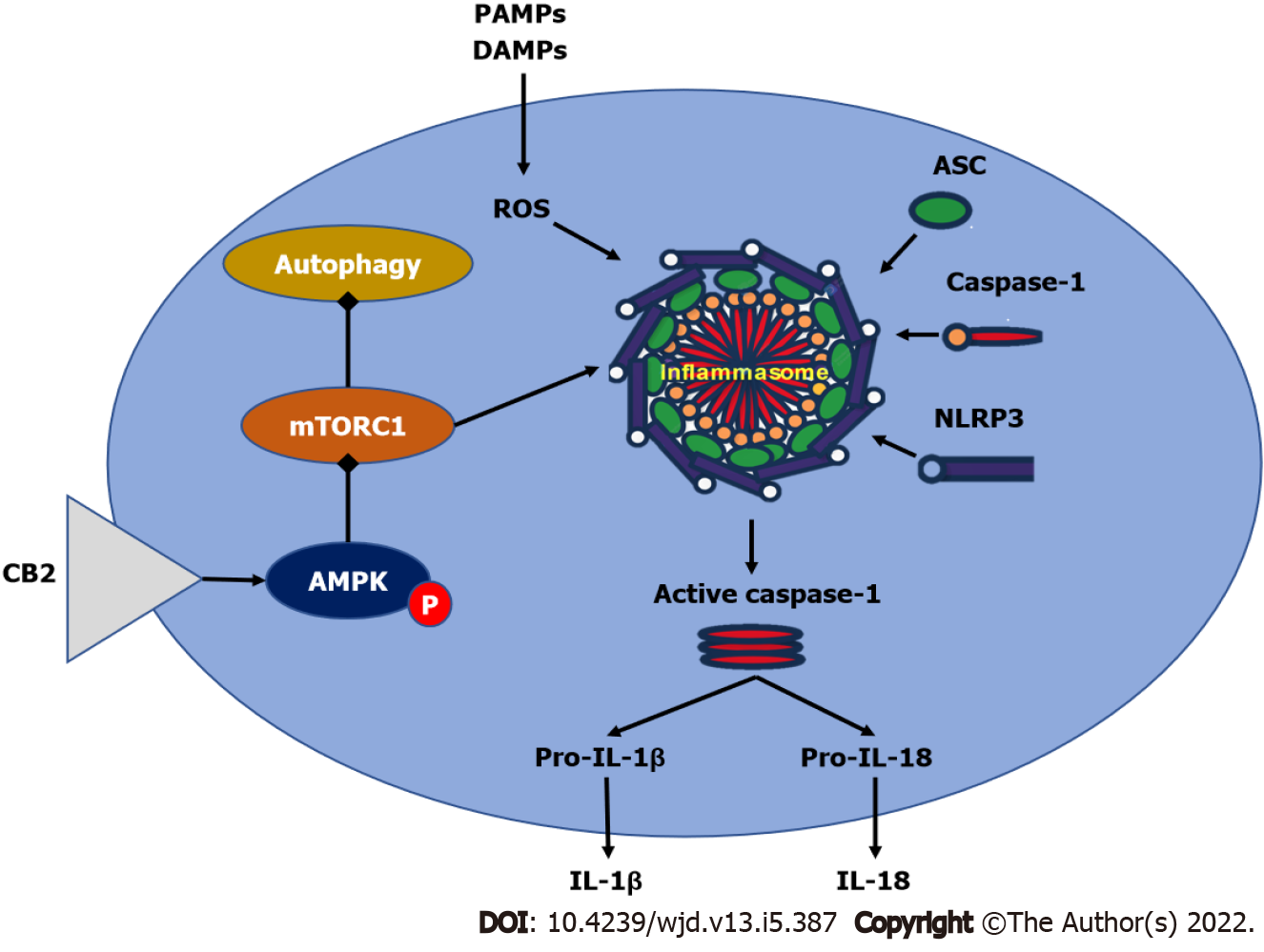
Autophagy also plays an essential role in the functioning of a variety of receptors. In the case of cannabinoid receptors, autophagy has been related to the protective effects of CB2 in a variety of disorders[162-164], suggesting the relevance of autophagy in disease treatment. Autophagy was previously shown to contribute to the alleviative effects mediated by CB2 activation in inflammatory disorders such as multiple sclerosis, alcoholic liver disease, and inflammatory bowel disease[162-164]. Activating CB2 improved inflammatory bowel disease in mouse models by inhibiting the NLRP3 inflammasome and triggering autophagy in murine macrophages, according to Ke and colleagues[163]. In mouse multiple sclerosis models, a similar relationship between CB2 and autophagy was discovered[164].
In the case of autophagy in diabetic cardiomyopathy, it was shown that increasing autophagy levels contributed to improving the condition. Several treatments have been demonstrated to be beneficial in reducing the etiology and development of diabetic cardiac myopathy by utilizing enhanced autophagy levels[160,161,165,166]. CB2 activation via autophagy induction provided protection against diabetic cardiomyopathy, according to a recent study by Wu and coworkers[167]. They used HU308 to selectively activate CB2, resulting in a substantial increase in autophagy levels in diabetic cardiomyopathy heart tissues in vivo and hyperglycemia-challenged cardiomyocytes in vitro. Furthermore, inhibiting autophagy with bafilomycin A1 reduced the cardioprotective effect of HU308 in both in vitro and in vivo models. Wu et al[167] concluded that CB2-induced autophagy was involved in the CB2-mediated cardio-protective effect.
Resveratrol, an autophagy inducer, was discovered to have a cardio-protective impact in cardiomyocytes exposed to hyperglycemia via the AMPK-mTOR-p70S6K signaling pathway[168]. AMPK-mTOR signaling contributed to the cardio-protective effect in STZ-induced diabetic mice by increasing autophagy[161,169]. According to these findings, Wu et al[167] found that administering HU308 to selectively activate CB2 enhanced AMPK phosphorylation while lowering mTOR and p70S6K phosphorylation, initiating the AMPK-mTOR-p70S6K signaling cascade in murine primary ventricular cardiomyocytes. Furthermore, using compound C, an AMPK inhibitor, significantly reduced the cardio-protective effect of HU308, showing that AMPK-mTOR-p70S6K signaling-induced autophagy was essential in CB2-mediated cardiac protection in dilated cardiomyopathy[167]. However, because the mechanisms behind CB2-mediated autophagy activation are complex, more research is required. Figure 4 summarizes the effect of cannabinoid receptors on AMPK/mTORC1/NLRP3 signaling.
Cannabidiol (CBD), has recently gained increased interest for therapeutic use. Indeed, CBD has been shown to suppress a high glucose-induced inflammatory response and barrier disruption of endothelial cells[170] and to attenuate myocardial dysfunction, cardiac fibrosis, oxidative/nitrative stress, inflammation, cell death, and interrelated signaling pathways in a mouse model of type I diabetic cardiomyopathy[95]. The critical role of HO-1 has been evident in the regulation of autophagy, with survival-enhancing effects in various cell types, including endothelial cells[171-173]. Moreover, HO-1 showed positive in vivo effects in animal models of atherosclerosis and restenosis[174]. Böckmann and Hinz have recently proved that CBD promoted endothelial cell survival via HO-1 mediated autophagy[170] (Table 2).
Diabetes-induced cardiomyopathy is a deleterious complication of the cardiovascular system characterized by structural and functional changes in the myocardium that ultimately lead to cardiac failure. The mechanisms underlying the development of diabetic cardiomyopathy are complex and involve several pathogenic pathways. A great body of evidence supported a special role of oxidative/nitrative stress and inflammation in the pathogenesis of diabetic cardiomyopathy. The endocannabinoid system has been implicated in the development of several pathological conditions including cardiovascular disorders. Several mechanisms have been proposed as targets by which cannabinoids and the endocannabinoid system could modulate cardiovascular disorders and recent evidence suggested the involvement of this system in the pathogenesis of diabetic cardiomyopathy. Indeed, the manipulation of the endocannabinoid system could represent a promising therapeutic approach for diabetic cardiomyopathy, and several mechanisms have been proposed for this role including its effects on oxidative/nitrative stress, inflammatory pathways, and autophagy together with possible effects on cardiac remodeling. However, more research is needed to define the exact mechanisms of the intervention of the different components of this system in diabetic cardiomyopathy.
The authors would like to thank Dr. Moshira Ibrahim; Professor of Pharmacology at Al-Azhar University (Girls), for her sincere guidance and supervision of AEW during writing the initial draft.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Endocrinology and metabolism
Country/Territory of origin: Egypt
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Koustas E, Greece; Wang CY, Taiwan; Zhang ZL, China S-Editor: Fan JR L-Editor: Webster JR P-Editor: Fan JR
| 1. | Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, Colagiuri S, Guariguata L, Motala AA, Ogurtsova K, Shaw JE, Bright D, Williams R; IDF Diabetes Atlas Committee. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract. 2019;157:107843. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5345] [Cited by in RCA: 5938] [Article Influence: 989.7] [Reference Citation Analysis (8)] |
| 2. | Guariguata L, Whiting D, Weil C, Unwin N. The International Diabetes Federation diabetes atlas methodology for estimating global and national prevalence of diabetes in adults. Diabetes Res Clin Pract. 2011;94:322-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 167] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 3. | Battiprolu PK, Gillette TG, Wang ZV, Lavandero S, Hill JA. Diabetic Cardiomyopathy: Mechanisms and Therapeutic Targets. Drug Discov Today Dis Mech. 2010;7:e135-e143. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 111] [Cited by in RCA: 110] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 4. | Chavali V, Tyagi SC, Mishra PK. Predictors and prevention of diabetic cardiomyopathy. Diabetes Metab Syndr Obes. 2013;6:151-160. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 66] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 5. | Rahman S, Rahman T, Ismail AA, Rashid AR. Diabetes-associated macrovasculopathy: pathophysiology and pathogenesis. Diabetes Obes Metab. 2007;9:767-780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 158] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 6. | Nguyen DV, Shaw LC, Grant MB. Inflammation in the pathogenesis of microvascular complications in diabetes. Front Endocrinol (Lausanne). 2012;3:170. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 112] [Cited by in RCA: 139] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 7. | El-Azab MF, Hazem RM, Moustafa YM. Role of simvastatin and/or antioxidant vitamins in therapeutic angiogenesis in experimental diabetic hindlimb ischemia: effects on capillary density, angiogenesis markers, and oxidative stress. Eur J Pharmacol. 2012;690:31-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 30] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 8. | Mysona BA, Al-Gayyar MM, Matragoon S, Abdelsaid MA, El-Azab MF, Saragovi HU, El-Remessy AB. Erratum to: Modulation of p75(NTR) prevents diabetes- and proNGF-induced retinal inflammation and blood-retina barrier breakdown in mice and rats. Diabetologia. 2015;58:644. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 9. | Eissa LD, Ghobashy WA, El-Azab MF. Inhibition of thioredoxin-interacting protein and inflammasome assembly using verapamil mitigates diabetic retinopathy and pancreatic injury. Eur J Pharmacol. 2021;901:174061. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 10. | Youssef ME, Abdelrazek HM, Moustafa YM. Cardioprotective role of GTS-21 by attenuating the TLR4/NF-κB pathway in streptozotocin-induced diabetic cardiomyopathy in rats. Naunyn Schmiedebergs Arch Pharmacol. 2021;394:11-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 25] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 11. | American Diabetes Association. Standards of medical care in diabetes--2013. Diabetes Care. 2013;36 Suppl 1:S11-S66. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2371] [Cited by in RCA: 2484] [Article Influence: 207.0] [Reference Citation Analysis (0)] |
| 12. | Dal Canto E, Ceriello A, Rydén L, Ferrini M, Hansen TB, Schnell O, Standl E, Beulens JW. Diabetes as a cardiovascular risk factor: An overview of global trends of macro and micro vascular complications. Eur J Prev Cardiol. 2019;26:25-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 175] [Article Influence: 29.2] [Reference Citation Analysis (0)] |
| 13. | Goyal BR, Mehta AA. Diabetic cardiomyopathy: pathophysiological mechanisms and cardiac dysfuntion. Hum Exp Toxicol. 2013;32:571-590. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 87] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 14. | Bugger H, Abel ED. Rodent models of diabetic cardiomyopathy. Dis Model Mech. 2009;2:454-466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 203] [Cited by in RCA: 215] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 15. | Mathew V, Gersh BJ, Williams BA, Laskey WK, Willerson JT, Tilbury RT, Davis BR, Holmes DR Jr. Outcomes in patients with diabetes mellitus undergoing percutaneous coronary intervention in the current era: a report from the Prevention of REStenosis with Tranilast and its Outcomes (PRESTO) trial. Circulation. 2004;109:476-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 151] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 16. | Kannel WB, McGee DL. Diabetes and cardiovascular disease. The Framingham study. JAMA. 1979;241:2035-2038. [PubMed] |
| 17. | van Melle JP, Bot M, de Jonge P, de Boer RA, van Veldhuisen DJ, Whooley MA. Diabetes, glycemic control, and new-onset heart failure in patients with stable coronary artery disease: data from the heart and soul study. Diabetes Care. 2010;33:2084-2089. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 84] [Cited by in RCA: 103] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 18. | Boudina S, Abel ED. Diabetic cardiomyopathy, causes and effects. Rev Endocr Metab Disord. 2010;11:31-39. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 566] [Cited by in RCA: 556] [Article Influence: 37.1] [Reference Citation Analysis (0)] |
| 19. | Duerr GD, Heinemann JC, Kley J, Eichhorn L, Frede S, Weisheit C, Wehner S, Bindila L, Lutz B, Zimmer A, Dewald O. Myocardial maladaptation to pressure overload in CB2 receptor-deficient mice. J Mol Cell Cardiol. 2019;133:86-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 20. | Li X, Xu Z, Li S, Rozanski GJ. Redox regulation of Ito remodeling in diabetic rat heart. Am J Physiol Heart Circ Physiol. 2005;288:H1417-H1424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 43] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 21. | Pacher P, Beckman JS, Liaudet L. Nitric oxide and peroxynitrite in health and disease. Physiol Rev. 2007;87:315-424. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4983] [Cited by in RCA: 4459] [Article Influence: 247.7] [Reference Citation Analysis (0)] |
| 22. | Murarka S, Movahed MR. Diabetic cardiomyopathy. J Card Fail. 2010;16:971-979. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 99] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 23. | Westermann D, Rutschow S, Van Linthout S, Linderer A, Bücker-Gärtner C, Sobirey M, Riad A, Pauschinger M, Schultheiss HP, Tschöpe C. Inhibition of p38 mitogen-activated protein kinase attenuates left ventricular dysfunction by mediating pro-inflammatory cardiac cytokine levels in a mouse model of diabetes mellitus. Diabetologia. 2006;49:2507-2513. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 127] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 24. | Fowlkes V, Clark J, Fix C, Law BA, Morales MO, Qiao X, Ako-Asare K, Goldsmith JG, Carver W, Murray DB, Goldsmith EC. Type II diabetes promotes a myofibroblast phenotype in cardiac fibroblasts. Life Sci. 2013;92:669-676. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 68] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 25. | Di Marzo V. The endocannabinoid system: its general strategy of action, tools for its pharmacological manipulation and potential therapeutic exploitation. Pharmacol Res. 2009;60:77-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 264] [Cited by in RCA: 282] [Article Influence: 17.6] [Reference Citation Analysis (0)] |
| 26. | Pacher P, Steffens S. The emerging role of the endocannabinoid system in cardiovascular disease. Semin Immunopathol. 2009;31:63-77. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 111] [Cited by in RCA: 101] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 27. | Matias I, Gonthier MP, Orlando P, Martiadis V, De Petrocellis L, Cervino C, Petrosino S, Hoareau L, Festy F, Pasquali R, Roche R, Maj M, Pagotto U, Monteleone P, Di Marzo V. Regulation, function, and dysregulation of endocannabinoids in models of adipose and beta-pancreatic cells and in obesity and hyperglycemia. J Clin Endocrinol Metab. 2006;91:3171-3180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 507] [Cited by in RCA: 519] [Article Influence: 27.3] [Reference Citation Analysis (0)] |
| 28. | Annuzzi G, Piscitelli F, Di Marino L, Patti L, Giacco R, Costabile G, Bozzetto L, Riccardi G, Verde R, Petrosino S, Rivellese AA, Di Marzo V. Differential alterations of the concentrations of endocannabinoids and related lipids in the subcutaneous adipose tissue of obese diabetic patients. Lipids Health Dis. 2010;9:43. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 62] [Cited by in RCA: 62] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 29. | Horváth B, Mukhopadhyay P, Haskó G, Pacher P. The endocannabinoid system and plant-derived cannabinoids in diabetes and diabetic complications. Am J Pathol. 2012;180:432-442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 111] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 30. | Elliott P, Andersson B, Arbustini E, Bilinska Z, Cecchi F, Charron P, Dubourg O, Kühl U, Maisch B, McKenna WJ, Monserrat L, Pankuweit S, Rapezzi C, Seferovic P, Tavazzi L, Keren A. Classification of the cardiomyopathies: a position statement from the European Society Of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J. 2008;29:270-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1766] [Cited by in RCA: 1893] [Article Influence: 105.2] [Reference Citation Analysis (0)] |
| 31. | Merlo M, Cannatà A, Gobbo M, Stolfo D, Elliott PM, Sinagra G. Evolving concepts in dilated cardiomyopathy. Eur J Heart Fail. 2018;20:228-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 237] [Article Influence: 29.6] [Reference Citation Analysis (0)] |
| 32. | Dyntar D. Diabetic cardiomyopathy: effects of fatty acids and glucose on adult rat cardiac cells. ETH. 2003;. [DOI] [Full Text] |
| 33. | Rubler S, Dlugash J, Yuceoglu YZ, Kumral T, Branwood AW, Grishman A. New type of cardiomyopathy associated with diabetic glomerulosclerosis. Am J Cardiol. 1972;30:595-602. [PubMed] |
| 34. | Pappachan JM, Varughese GI, Sriraman R, Arunagirinathan G. Diabetic cardiomyopathy: Pathophysiology, diagnostic evaluation and management. World J Diabetes. 2013;4:177-189. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 111] [Cited by in RCA: 125] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 35. | Bertero E, Maack C. Metabolic remodelling in heart failure. Nat Rev Cardiol. 2018;15:457-470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 232] [Cited by in RCA: 447] [Article Influence: 74.5] [Reference Citation Analysis (0)] |
| 36. | Dei Cas A, Spigoni V, Ridolfi V, Metra M. Diabetes and chronic heart failure: from diabetic cardiomyopathy to therapeutic approach. Endocr Metab Immune Disord Drug Targets. 2013;13:38-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 37. | Giacco F, Brownlee M. Oxidative stress and diabetic complications. Circ Res. 2010;107:1058-1070. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3956] [Cited by in RCA: 3625] [Article Influence: 241.7] [Reference Citation Analysis (0)] |
| 38. | Calle MC, Fernandez ML. Inflammation and type 2 diabetes. Diabetes Metab. 2012;38:183-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 251] [Cited by in RCA: 362] [Article Influence: 27.8] [Reference Citation Analysis (0)] |
| 39. | Fang ZY, Prins JB, Marwick TH. Diabetic cardiomyopathy: evidence, mechanisms, and therapeutic implications. Endocr Rev. 2004;25:543-567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 669] [Cited by in RCA: 675] [Article Influence: 32.1] [Reference Citation Analysis (0)] |
| 40. | Boyer JK, Thanigaraj S, Schechtman KB, Pérez JE. Prevalence of ventricular diastolic dysfunction in asymptomatic, normotensive patients with diabetes mellitus. Am J Cardiol. 2004;93:870-875. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 335] [Cited by in RCA: 346] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 41. | Miki T, Yuda S, Kouzu H, Miura T. Diabetic cardiomyopathy: pathophysiology and clinical features. Heart Fail Rev. 2013;18:149-166. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 280] [Cited by in RCA: 352] [Article Influence: 29.3] [Reference Citation Analysis (0)] |
| 42. | Gaoni Y, Mechoulam R. Isolation, structure, and partial synthesis of an active constituent of hashish. J Am Chem Soc. 1964;86:1646-1647. |
| 43. | Devane WA, Dysarz FA 3rd, Johnson MR, Melvin LS, Howlett AC. Determination and characterization of a cannabinoid receptor in rat brain. Mol Pharmacol. 1988;34:605-613. [PubMed] |
| 44. | Munro S, Thomas KL, Abu-Shaar M. Molecular characterization of a peripheral receptor for cannabinoids. Nature. 1993;365:61-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3564] [Cited by in RCA: 3653] [Article Influence: 114.2] [Reference Citation Analysis (0)] |
| 45. | Devane WA, Hanus L, Breuer A, Pertwee RG, Stevenson LA, Griffin G, Gibson D, Mandelbaum A, Etinger A, Mechoulam R. Isolation and structure of a brain constituent that binds to the cannabinoid receptor. Science. 1992;258:1946-1949. [PubMed] |
| 46. | Mechoulam R, Ben-Shabat S, Hanus L, Ligumsky M, Kaminski NE, Schatz AR, Gopher A, Almog S, Martin BR, Compton DR. Identification of an endogenous 2-monoglyceride, present in canine gut, that binds to cannabinoid receptors. Biochem Pharmacol. 1995;50:83-90. [PubMed] |
| 47. | Di Marzo V, Bifulco M, De Petrocellis L. The endocannabinoid system and its therapeutic exploitation. Nat Rev Drug Discov. 2004;3:771-784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 710] [Cited by in RCA: 766] [Article Influence: 36.5] [Reference Citation Analysis (0)] |
| 48. | Howlett AC. Cannabinoid receptor signaling. Handb Exp Pharmacol. 2005;53-79. [PubMed] |
| 49. | Montecucco F, Di Marzo V. At the heart of the matter: the endocannabinoid system in cardiovascular function and dysfunction. Trends Pharmacol Sci. 2012;33:331-340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 116] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 50. | Mackie K. Cannabinoid receptors as therapeutic targets. Annu Rev Pharmacol Toxicol. 2006;46:101-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 361] [Cited by in RCA: 375] [Article Influence: 19.7] [Reference Citation Analysis (0)] |
| 51. | Pacher P, Bátkai S, Kunos G. The endocannabinoid system as an emerging target of pharmacotherapy. Pharmacol Rev. 2006;58:389-462. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1655] [Cited by in RCA: 1546] [Article Influence: 81.4] [Reference Citation Analysis (0)] |
| 52. | Mukhopadhyay P, Bátkai S, Rajesh M, Czifra N, Harvey-White J, Haskó G, Zsengeller Z, Gerard NP, Liaudet L, Kunos G, Pacher P. Pharmacological inhibition of CB1 cannabinoid receptor protects against doxorubicin-induced cardiotoxicity. J Am Coll Cardiol. 2007;50:528-536. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 170] [Cited by in RCA: 174] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 53. | Steffens S, Pacher P. Targeting cannabinoid receptor CB(2) in cardiovascular disorders: promises and controversies. Br J Pharmacol. 2012;167:313-323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 102] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 54. | Hoyer FF, Steinmetz M, Zimmer S, Becker A, Lütjohann D, Buchalla R, Zimmer A, Nickenig G. Atheroprotection via cannabinoid receptor-2 is mediated by circulating and vascular cells in vivo. J Mol Cell Cardiol. 2011;51:1007-1014. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 47] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 55. | Tallant EA, Howlett A, Grabenauer M, Thomas BF, Gallagher PE. The CB2 Cannabinoid Receptor Mediates the Anti-Proliferative Actions of Angiotensin-(1-7) in Vascular Smooth Muscle Cells. Am Heart Assoc. 2013;. |
| 56. | Montecucco F, Lenglet S, Braunersreuther V, Burger F, Pelli G, Bertolotto M, Mach F, Steffens S. CB(2) cannabinoid receptor activation is cardioprotective in a mouse model of ischemia/reperfusion. J Mol Cell Cardiol. 2009;46:612-620. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 142] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 57. | Bermúdez-Silva FJ, Suárez J, Baixeras E, Cobo N, Bautista D, Cuesta-Muñoz AL, Fuentes E, Juan-Pico P, Castro MJ, Milman G, Mechoulam R, Nadal A, Rodríguez de Fonseca F. Presence of functional cannabinoid receptors in human endocrine pancreas. Diabetologia. 2008;51:476-487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 145] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 58. | Li C, Bowe JE, Jones PM, Persaud SJ. Expression and function of cannabinoid receptors in mouse islets. Islets. 2010;2:293-302. [PubMed] |
| 59. | Vilches-Flores A, Delgado-Buenrostro NL, Navarrete-Vázquez G, Villalobos-Molina R. CB1 cannabinoid receptor expression is regulated by glucose and feeding in rat pancreatic islets. Regul Pept. 2010;163:81-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 29] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 60. | Nakata M, Yada T. Cannabinoids inhibit insulin secretion and cytosolic Ca2+ oscillation in islet beta-cells via CB1 receptors. Regul Pept. 2008;145:49-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 87] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 61. | Li C, Jones PM, Persaud SJ. Cannabinoid receptors are coupled to stimulation of insulin secretion from mouse MIN6 beta-cells. Cell Physiol Biochem. 2010;26:187-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 45] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 62. | Scheen AJ, Finer N, Hollander P, Jensen MD, Van Gaal LF; RIO-Diabetes Study Group. Efficacy and tolerability of rimonabant in overweight or obese patients with type 2 diabetes: a randomised controlled study. Lancet. 2006;368:1660-1672. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 550] [Cited by in RCA: 501] [Article Influence: 26.4] [Reference Citation Analysis (0)] |
| 63. | Rosenstock J, Hollander P, Chevalier S, Iranmanesh A; SERENADE Study Group. SERENADE: the Study Evaluating Rimonabant Efficacy in Drug-naive Diabetic Patients: effects of monotherapy with rimonabant, the first selective CB1 receptor antagonist, on glycemic control, body weight, and lipid profile in drug-naive type 2 diabetes. Diabetes Care. 2008;31:2169-2176. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 89] [Cited by in RCA: 91] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 64. | Hollander PA, Amod A, Litwak LE, Chaudhari U; ARPEGGIO Study Group. Effect of rimonabant on glycemic control in insulin-treated type 2 diabetes: the ARPEGGIO trial. Diabetes Care. 2010;33:605-607. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 34] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 65. | Li X, Kaminski NE, Fischer LJ. Examination of the immunosuppressive effect of delta9-tetrahydrocannabinol in streptozotocin-induced autoimmune diabetes. Int Immunopharmacol. 2001;1:699-712. [PubMed] |
| 66. | Weiss L, Zeira M, Reich S, Slavin S, Raz I, Mechoulam R, Gallily R. Cannabidiol arrests onset of autoimmune diabetes in NOD mice. Neuropharmacology. 2008;54:244-249. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 122] [Cited by in RCA: 108] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 67. | Cade WT. Diabetes-related microvascular and macrovascular diseases in the physical therapy setting. Phys Ther. 2008;88:1322-1335. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 733] [Cited by in RCA: 641] [Article Influence: 37.7] [Reference Citation Analysis (0)] |
| 68. | Varga ZV, Giricz Z, Liaudet L, Haskó G, Ferdinandy P, Pacher P. Interplay of oxidative, nitrosative/nitrative stress, inflammation, cell death and autophagy in diabetic cardiomyopathy. Biochim Biophys Acta. 2015;1852:232-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 229] [Cited by in RCA: 221] [Article Influence: 22.1] [Reference Citation Analysis (0)] |
| 69. | Kalyanaraman B. Teaching the basics of redox biology to medical and graduate students: Oxidants, antioxidants and disease mechanisms. Redox Biol. 2013;1:244-257. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 314] [Cited by in RCA: 338] [Article Influence: 28.2] [Reference Citation Analysis (0)] |
| 70. | Culotta VC. Superoxide dismutase, oxidative stress, and cell metabolism. Curr Top Cell Regul. 2000;36:117-132. [PubMed] |
| 71. | Matés JM, Pérez-Gómez C, Núñez de Castro I. Antioxidant enzymes and human diseases. Clin Biochem. 1999;32:595-603. [PubMed] |
| 72. | Webster NR, Nunn JF. Molecular structure of free radicals and their importance in biological reactions. British J Anaes. 1988;60:98-108. |
| 73. | Beckman JS, Beckman TW, Chen J, Marshall PA, Freeman BA. Apparent hydroxyl radical production by peroxynitrite: implications for endothelial injury from nitric oxide and superoxide. Proc Natl Acad Sci U S A. 1990;87:1620-1624. [PubMed] |
| 74. | Huie RE, Padmaja S. The reaction of no with superoxide. Free Radic Res Commun. 1993;18:195-199. [PubMed] |
| 75. | Babior BM. NADPH oxidase. Curr Opin Immunol. 2004;16:42-47. [PubMed] |
| 76. | White KA, Marletta MA. Nitric oxide synthase is a cytochrome P-450 type hemoprotein. Biochemistry. 1992;31:6627-6631. [PubMed] |
| 77. | Dröge W. Free radicals in the physiological control of cell function. Physiol Rev. 2002;82:47-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6483] [Cited by in RCA: 6354] [Article Influence: 276.3] [Reference Citation Analysis (0)] |
| 78. | Broeke RT, Leusink-Muis T, Hilberdink R, Van Ark I, van den Worm E, Villain M, De Clerck F, Blalock JE, Nijkamp FP, Folkerts G. Specific modulation of calmodulin activity induces a dramatic production of superoxide by alveolar macrophages. Lab Invest. 2004;84:29-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 79. | Zhang X, Chen C. A new insight of mechanisms, diagnosis and treatment of diabetic cardiomyopathy. Endocrine. 2012;41:398-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 48] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 80. | Nishikawa T, Edelstein D, Brownlee M. The missing link: a single unifying mechanism for diabetic complications. Kidney Int Suppl. 2000;77:S26-S30. [PubMed] |
| 81. | Nishikawa T, Edelstein D, Du XL, Yamagishi S, Matsumura T, Kaneda Y, Yorek MA, Beebe D, Oates PJ, Hammes HP, Giardino I, Brownlee M. Normalizing mitochondrial superoxide production blocks three pathways of hyperglycaemic damage. Nature. 2000;404:787-790. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3116] [Cited by in RCA: 3105] [Article Influence: 124.2] [Reference Citation Analysis (0)] |
| 82. | Mandavia CH, Aroor AR, Demarco VG, Sowers JR. Molecular and metabolic mechanisms of cardiac dysfunction in diabetes. Life Sci. 2013;92:601-608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 146] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 83. | Halliwell B. Biochemistry of oxidative stress. Biochem Soc Trans. 2007;35:1147-1150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 889] [Cited by in RCA: 903] [Article Influence: 53.1] [Reference Citation Analysis (0)] |
| 84. | King MK, Coker ML, Goldberg A, McElmurray JH 3rd, Gunasinghe HR, Mukherjee R, Zile MR, O'Neill TP, Spinale FG. Selective matrix metalloproteinase inhibition with developing heart failure: effects on left ventricular function and structure. Circ Res. 2003;92:177-185. [PubMed] |
| 85. | Cesselli D, Jakoniuk I, Barlucchi L, Beltrami AP, Hintze TH, Nadal-Ginard B, Kajstura J, Leri A, Anversa P. Oxidative stress-mediated cardiac cell death is a major determinant of ventricular dysfunction and failure in dog dilated cardiomyopathy. Circ Res. 2001;89:279-286. [PubMed] |
| 86. | Takano H, Zou Y, Hasegawa H, Akazawa H, Nagai T, Komuro I. Oxidative stress-induced signal transduction pathways in cardiac myocytes: involvement of ROS in heart diseases. Antioxid Redox Signal. 2003;5:789-794. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 156] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 87. | Imrie H, Abbas A, Kearney M. Insulin resistance, lipotoxicity and endothelial dysfunction. Biochim Biophys Acta. 2010;1801:320-326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 52] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 88. | Ni R, Cao T, Xiong S, Ma J, Fan GC, Lacefield JC, Lu Y, Le Tissier S, Peng T. Therapeutic inhibition of mitochondrial reactive oxygen species with mito-TEMPO reduces diabetic cardiomyopathy. Free Radic Biol Med. 2016;90:12-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 227] [Article Influence: 25.2] [Reference Citation Analysis (0)] |
| 89. | Kowluru RA, Kowluru A, Veluthakal R, Mohammad G, Syed I, Santos JM, Mishra M. TIAM1-RAC1 signalling axis-mediated activation of NADPH oxidase-2 initiates mitochondrial damage in the development of diabetic retinopathy. Diabetologia. 2014;57:1047-1056. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 115] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 90. | Mukhopadhyay P, Rajesh M, Bátkai S, Patel V, Kashiwaya Y, Liaudet L, Evgenov OV, Mackie K, Haskó G, Pacher P. CB1 cannabinoid receptors promote oxidative stress and cell death in murine models of doxorubicin-induced cardiomyopathy and in human cardiomyocytes. Cardiovasc Res. 2010;85:773-784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 167] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 91. | Mukhopadhyay P, Horváth B, Rajesh M, Matsumoto S, Saito K, Bátkai S, Patel V, Tanchian G, Gao RY, Cravatt BF, Haskó G, Pacher P. Fatty acid amide hydrolase is a key regulator of endocannabinoid-induced myocardial tissue injury. Free Radic Biol Med. 2011;50:179-195. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 71] [Cited by in RCA: 71] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 92. | Rajesh M, Bátkai S, Kechrid M, Mukhopadhyay P, Lee WS, Horváth B, Holovac E, Cinar R, Liaudet L, Mackie K, Haskó G, Pacher P. Cannabinoid 1 receptor promotes cardiac dysfunction, oxidative stress, inflammation, and fibrosis in diabetic cardiomyopathy. Diabetes. 2012;61:716-727. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 215] [Cited by in RCA: 213] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 93. | Barnes MP. Sativex: clinical efficacy and tolerability in the treatment of symptoms of multiple sclerosis and neuropathic pain. Expert Opin Pharmacother. 2006;7:607-615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 100] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 94. | Izzo AA, Borrelli F, Capasso R, Di Marzo V, Mechoulam R. Non-psychotropic plant cannabinoids: new therapeutic opportunities from an ancient herb. Trends Pharmacol Sci. 2009;30:515-527. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 525] [Cited by in RCA: 572] [Article Influence: 35.8] [Reference Citation Analysis (0)] |
| 95. | Rajesh M, Mukhopadhyay P, Bátkai S, Patel V, Saito K, Matsumoto S, Kashiwaya Y, Horváth B, Mukhopadhyay B, Becker L, Haskó G, Liaudet L, Wink DA, Veves A, Mechoulam R, Pacher P. Cannabidiol attenuates cardiac dysfunction, oxidative stress, fibrosis, and inflammatory and cell death signaling pathways in diabetic cardiomyopathy. J Am Coll Cardiol. 2010;56:2115-2125. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 411] [Cited by in RCA: 390] [Article Influence: 26.0] [Reference Citation Analysis (0)] |
| 96. | Vella RK, Jackson DJ, Fenning AS. Δ9-Tetrahydrocannabinol Prevents Cardiovascular Dysfunction in STZ-Diabetic Wistar-Kyoto Rats. Biomed Res Int. 2017;2017:7974149. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 97. | Dresner LS, Wang SP, West MW, Ponomarenko IN, Mueller CM, Wait RB. Nitric oxide inhibition simulates the enhancement of alpha 1 agonist-induced vasoconstriction in diabetes. J Surg Res. 1997;70:119-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 98. | Iwalewa EO, McGaw LJ, Naidoo V, Eloff JN. Inflammation: the foundation of diseases and disorders. A review of phytomedicines of South African origin used to treat pain and inflammatory conditions. Afr J Biotechnol. 2007;6. |
| 99. | Esch T, Stefano G. Proinflammation: a common denominator or initiator of different pathophysiological disease processes. Med Sci Monit. 2002;8:HY1-HY9. [PubMed] |
| 100. | Buyken AE, Flood V, Empson M, Rochtchina E, Barclay AW, Brand-Miller J, Mitchell P. Carbohydrate nutrition and inflammatory disease mortality in older adults. Am J Clin Nutr. 2010;92:634-643. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 48] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 101. | Pahl HL. Activators and target genes of Rel/NF-kappaB transcription factors. Oncogene. 1999;18:6853-6866. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3079] [Cited by in RCA: 3117] [Article Influence: 119.9] [Reference Citation Analysis (0)] |
| 102. | Coleman JW. Nitric oxide: a regulator of mast cell activation and mast cell-mediated inflammation. Clin Exp Immunol. 2002;129:4-10. [PubMed] |
| 103. | King GL. The role of inflammatory cytokines in diabetes and its complications. J Periodontol. 2008;79:1527-1534. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 376] [Cited by in RCA: 440] [Article Influence: 25.9] [Reference Citation Analysis (0)] |
| 104. | Lorenzo O, Picatoste B, Ares-Carrasco S, Ramírez E, Egido J, Tuñón J. Potential role of nuclear factor κB in diabetic cardiomyopathy. Mediators Inflamm. 2011;2011:652097. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 106] [Cited by in RCA: 132] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 105. | Chen S, Khan ZA, Cukiernik M, Chakrabarti S. Differential activation of NF-kappa B and AP-1 in increased fibronectin synthesis in target organs of diabetic complications. Am J Physiol Endocrinol Metab. 2003;284:E1089-E1097. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 120] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 106. | Al-Maghrebi M, Benter IF, Diz DI. Endogenous angiotensin-(1-7) reduces cardiac ischemia-induced dysfunction in diabetic hypertensive rats. Pharmacol Res. 2009;59:263-268. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 68] [Cited by in RCA: 68] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 107. | Klein TW. Cannabinoid-based drugs as anti-inflammatory therapeutics. Nat Rev Immunol. 2005;5:400-411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 499] [Cited by in RCA: 529] [Article Influence: 26.5] [Reference Citation Analysis (0)] |
| 108. | Di Marzo V, Petrosino S. Endocannabinoids and the regulation of their levels in health and disease. Curr Opin Lipidol. 2007;18:129-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 222] [Cited by in RCA: 220] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 109. | Cabral GA, Staab A. Effects on the immune system. Handb Exp Pharmacol. 2005;385-423. [PubMed] |
| 110. | Klein TW, Newton C, Larsen K, Lu L, Perkins I, Nong L, Friedman H. The cannabinoid system and immune modulation. J Leukoc Biol. 2003;74:486-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 368] [Cited by in RCA: 378] [Article Influence: 17.2] [Reference Citation Analysis (0)] |
| 111. | Cencioni MT, Chiurchiù V, Catanzaro G, Borsellino G, Bernardi G, Battistini L, Maccarrone M. Anandamide suppresses proliferation and cytokine release from primary human T-lymphocytes mainly via CB2 receptors. PLoS One. 2010;5:e8688. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 166] [Cited by in RCA: 189] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 112. | Han KH, Lim S, Ryu J, Lee CW, Kim Y, Kang JH, Kang SS, Ahn YK, Park CS, Kim JJ. CB1 and CB2 cannabinoid receptors differentially regulate the production of reactive oxygen species by macrophages. Cardiovasc Res. 2009;84:378-386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 187] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 113. | Dol-Gleizes F, Paumelle R, Visentin V, Marés AM, Desitter P, Hennuyer N, Gilde A, Staels B, Schaeffer P, Bono F. Rimonabant, a selective cannabinoid CB1 receptor antagonist, inhibits atherosclerosis in LDL receptor-deficient mice. Arterioscler Thromb Vasc Biol. 2009;29:12-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 104] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 114. | Zhao Y, Liu Y, Zhang W, Xue J, Wu YZ, Xu W, Liang X, Chen T, Kishimoto C, Yuan Z. WIN55212-2 ameliorates atherosclerosis associated with suppression of pro-inflammatory responses in ApoE-knockout mice. Eur J Pharmacol. 2010;649:285-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 41] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 115. | Zhao Y, Yuan Z, Liu Y, Xue J, Tian Y, Liu W, Zhang W, Shen Y, Xu W, Liang X, Chen T. Activation of cannabinoid CB2 receptor ameliorates atherosclerosis associated with suppression of adhesion molecules. J Cardiovasc Pharmacol. 2010;55:292-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 65] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 116. | Hashiesh HM, Sharma C, Goyal SN, Jha NK, Ojha S. Pharmacological Properties, Therapeutic Potential and Molecular Mechanisms of JWH133, a CB2 Receptor-Selective Agonist. Front Pharmacol. 2021;12:702675. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 117. | Pacher P, Haskó G. Endocannabinoids and cannabinoid receptors in ischaemia-reperfusion injury and preconditioning. Br J Pharmacol. 2008;153:252-262. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 174] [Cited by in RCA: 179] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 118. | Wang J, Song Y, Wang Q, Kralik PM, Epstein PN. Causes and characteristics of diabetic cardiomyopathy. Rev Diabet Stud. 2006;3:108-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 108] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 119. | Acar E, Ural D, Bildirici U, Sahin T, Yılmaz I. Diabetic cardiomyopathy. Anadolu Kardiyol Derg. 2011;11:732-737. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 22] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 120. | Monnier VM, Sell DR, Genuth S. Glycation products as markers and predictors of the progression of diabetic complications. Ann N Y Acad Sci. 2005;1043:567-581. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 125] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 121. | Xu J, Chen LJ, Yu J, Wang HJ, Zhang F, Liu Q, Wu J. Involvement of Advanced Glycation End Products in the Pathogenesis of Diabetic Retinopathy. Cell Physiol Biochem. 2018;48:705-717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 96] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 122. | Singh VP, Bali A, Singh N, Jaggi AS. Advanced glycation end products and diabetic complications. Korean J Physiol Pharmacol. 2014;18:1-14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 750] [Cited by in RCA: 961] [Article Influence: 87.4] [Reference Citation Analysis (0)] |
| 123. | Neeper M, Schmidt AM, Brett J, Yan SD, Wang F, Pan YC, Elliston K, Stern D, Shaw A. Cloning and expression of a cell surface receptor for advanced glycosylation end products of proteins. J Biol Chem. 1992;267:14998-15004. [PubMed] |
| 124. | Hartog JW, Voors AA, Bakker SJ, Smit AJ, van Veldhuisen DJ. Advanced glycation end-products (AGEs) and heart failure: pathophysiology and clinical implications. Eur J Heart Fail. 2007;9:1146-1155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 198] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 125. | Lepetsos P, Papavassiliou KA, Papavassiliou AG. Redox and NF-κB signaling in osteoarthritis. Free Radic Biol Med. 2019;132:90-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 296] [Cited by in RCA: 274] [Article Influence: 45.7] [Reference Citation Analysis (0)] |
| 126. | D'Souza A, Howarth FC, Yanni J, Dobryznski H, Boyett MR, Adeghate E, Bidasee KR, Singh J. Left ventricle structural remodelling in the prediabetic Goto-Kakizaki rat. Exp Physiol. 2011;96:875-888. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 44] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 127. | Watanabe K, Thandavarayan RA, Harima M, Sari FR, Gurusamy N, Veeraveedu PT, Mito S, Arozal W, Sukumaran V, Laksmanan AP, Soetikno V, Kodama M, Aizawa Y. Role of differential signaling pathways and oxidative stress in diabetic cardiomyopathy. Curr Cardiol Rev. 2010;6:280-290. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 63] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 128. | Mandavia CH, Pulakat L, DeMarco V, Sowers JR. Over-nutrition and metabolic cardiomyopathy. Metabolism. 2012;61:1205-1210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 55] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 129. | Hayden MR, Tyagi SC. Myocardial redox stress and remodeling in metabolic syndrome, type 2 diabetes mellitus, and congestive heart failure. Med Sci Monit. 2003;9:SR35-SR52. [PubMed] |
| 130. | Schreier B, Rabe S, Schneider B, Ruhs S, Grossmann C, Hauptmann S, Blessing M, Neumann J, Gekle M. Aldosterone/NaCl-induced renal and cardiac fibrosis is modulated by TGF-β responsiveness of T cells. Hypertens Res. 2011;34:623-629. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 26] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 131. | Hiley CR, Ford WR. Cannabinoid pharmacology in the cardiovascular system: potential protective mechanisms through lipid signalling. Biol Rev Camb Philos Soc. 2004;79:187-205. [PubMed] |
| 132. | Athanasiou A, Clarke AB, Turner AE, Kumaran NM, Vakilpour S, Smith PA, Bagiokou D, Bradshaw TD, Westwell AD, Fang L, Lobo DN, Constantinescu CS, Calabrese V, Loesch A, Alexander SP, Clothier RH, Kendall DA, Bates TE. Cannabinoid receptor agonists are mitochondrial inhibitors: a unified hypothesis of how cannabinoids modulate mitochondrial function and induce cell death. Biochem Biophys Res Commun. 2007;364:131-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 112] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 133. | Sarafian TA, Habib N, Oldham M, Seeram N, Lee RP, Lin L, Tashkin DP, Roth MD. Inhaled marijuana smoke disrupts mitochondrial energetics in pulmonary epithelial cells in vivo. Am J Physiol Lung Cell Mol Physiol. 2006;290:L1202-L1209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 48] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 134. | Di Marzo V. Targeting the endocannabinoid system: to enhance or reduce? Nat Rev Drug Discov. 2008;7:438-455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 602] [Cited by in RCA: 631] [Article Influence: 37.1] [Reference Citation Analysis (0)] |
| 135. | Chanda D, Neumann D, Glatz JFC. The endocannabinoid system: Overview of an emerging multi-faceted therapeutic target. Prostaglandins Leukot Essent Fatty Acids. 2019;140:51-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 55] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 136. | Hiley CR. Endocannabinoids and the heart. J Cardiovasc Pharmacol. 2009;53:267-276. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 62] [Cited by in RCA: 59] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 137. | Rabino M, Mallia S, Castiglioni E, Rovina D, Pompilio G, Gowran A. The Endocannabinoid System and Cannabidiol: Past, Present, and Prospective for Cardiovascular Diseases. Pharmaceuticals (Basel). 2021;14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 138. | Sun Y. Myocardial repair/remodelling following infarction: roles of local factors. Cardiovasc Res. 2009;81:482-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 217] [Cited by in RCA: 227] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 139. | Defer N, Wan J, Souktani R, Escoubet B, Perier M, Caramelle P, Manin S, Deveaux V, Bourin MC, Zimmer A, Lotersztajn S, Pecker F, Pavoine C. The cannabinoid receptor type 2 promotes cardiac myocyte and fibroblast survival and protects against ischemia/reperfusion-induced cardiomyopathy. FASEB J. 2009;23:2120-2130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 102] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 140. | Wagner JA, Hu K, Karcher J, Bauersachs J, Schäfer A, Laser M, Han H, Ertl G. CB(1) cannabinoid receptor antagonism promotes remodeling and cannabinoid treatment prevents endothelial dysfunction and hypotension in rats with myocardial infarction. Br J Pharmacol. 2003;138:1251-1258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 46] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 141. | Liao Y, Bin J, Luo T, Zhao H, Ledent C, Asakura M, Xu D, Takashima S, Kitakaze M. CB1 cannabinoid receptor deficiency promotes cardiac remodeling induced by pressure overload in mice. Int J Cardiol. 2013;167:1936-1944. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 142. | Weis F, Beiras-Fernandez A, Sodian R, Kaczmarek I, Reichart B, Beiras A, Schelling G, Kreth S. Substantially altered expression pattern of cannabinoid receptor 2 and activated endocannabinoid system in patients with severe heart failure. J Mol Cell Cardiol. 2010;48:1187-1193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 55] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 143. | Duerr GD, Heinemann JC, Dunkel S, Zimmer A, Lutz B, Lerner R, Roell W, Mellert F, Probst C, Esmailzadeh B, Welz A, Dewald O. Myocardial hypertrophy is associated with inflammation and activation of endocannabinoid system in patients with aortic valve stenosis. Life Sci. 2013;92:976-983. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 144. | Cortes CJ, La Spada AR. TFEB dysregulation as a driver of autophagy dysfunction in neurodegenerative disease: Molecular mechanisms, cellular processes, and emerging therapeutic opportunities. Neurobiol Dis. 2019;122:83-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 138] [Article Influence: 19.7] [Reference Citation Analysis (0)] |
| 145. | Shao BZ, Han BZ, Zeng YX, Su DF, Liu C. The roles of macrophage autophagy in atherosclerosis. Acta Pharmacol Sin. 2016;37:150-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 182] [Article Influence: 20.2] [Reference Citation Analysis (0)] |
| 146. | Lamb CA, Yoshimori T, Tooze SA. The autophagosome: origins unknown, biogenesis complex. Nat Rev Mol Cell Biol. 2013;14:759-774. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1033] [Cited by in RCA: 1043] [Article Influence: 86.9] [Reference Citation Analysis (0)] |
| 147. | Klionsky DJ. Look people, "Atg" is an abbreviation for "autophagy-related." That's it. Autophagy. 2012;8:1281-1282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 148. | Tsukada M, Ohsumi Y. Isolation and characterization of autophagy-defective mutants of Saccharomyces cerevisiae. FEBS Lett. 1993;333:169-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1305] [Cited by in RCA: 1387] [Article Influence: 43.3] [Reference Citation Analysis (0)] |
| 149. | Suzuki H, Osawa T, Fujioka Y, Noda NN. Structural biology of the core autophagy machinery. Curr Opin Struct Biol. 2017;43:10-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 93] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 150. | Chan EY. Regulation and function of uncoordinated-51 Like kinase proteins. Antioxid Redox Signal. 2012;17:775-785. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 53] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 151. | Russell RC, Tian Y, Yuan H, Park HW, Chang YY, Kim J, Kim H, Neufeld TP, Dillin A, Guan KL. ULK1 induces autophagy by phosphorylating Beclin-1 and activating VPS34 Lipid kinase. Nat Cell Biol. 2013;15:741-750. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1001] [Cited by in RCA: 1234] [Article Influence: 102.8] [Reference Citation Analysis (0)] |
| 152. | Di Bartolomeo S, Corazzari M, Nazio F, Oliverio S, Lisi G, Antonioli M, Pagliarini V, Matteoni S, Fuoco C, Giunta L, D'Amelio M, Nardacci R, Romagnoli A, Piacentini M, Cecconi F, Fimia GM. The dynamic interaction of AMBRA1 with the dynein motor complex regulates mammalian autophagy. J Cell Biol. 2010;191:155-168. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 414] [Cited by in RCA: 390] [Article Influence: 26.0] [Reference Citation Analysis (0)] |
| 153. | Dooley HC, Razi M, Polson HE, Girardin SE, Wilson MI, Tooze SA. WIPI2 Links LC3 conjugation with PI3P, autophagosome formation, and pathogen clearance by recruiting Atg12-5-16L1. Mol Cell. 2014;55:238-252. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 617] [Cited by in RCA: 674] [Article Influence: 61.3] [Reference Citation Analysis (0)] |
| 154. | Hanada T, Noda NN, Satomi Y, Ichimura Y, Fujioka Y, Takao T, Inagaki F, Ohsumi Y. The Atg12-Atg5 conjugate has a novel E3-like activity for protein lipidation in autophagy. J Biol Chem. 2007;282:37298-37302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 777] [Cited by in RCA: 855] [Article Influence: 47.5] [Reference Citation Analysis (0)] |
| 155. | Kabeya Y, Mizushima N, Yamamoto A, Oshitani-Okamoto S, Ohsumi Y, Yoshimori T. LC3, GABARAP and GATE16 Localize to autophagosomal membrane depending on form-II formation. J Cell Sci. 2004;117:2805-2812. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1017] [Cited by in RCA: 1132] [Article Influence: 56.6] [Reference Citation Analysis (0)] |
| 156. | Fujita N, Hayashi-Nishino M, Fukumoto H, Omori H, Yamamoto A, Noda T, Yoshimori T. An Atg4B mutant hampers the lipidation of LC3 paralogues and causes defects in autophagosome closure. Mol Biol Cell. 2008;19:4651-4659. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 416] [Cited by in RCA: 424] [Article Influence: 24.9] [Reference Citation Analysis (0)] |
| 157. | Park S, Choi SG, Yoo SM, Son JH, Jung YK. Choline dehydrogenase interacts with SQSTM1/p62 to recruit LC3 and stimulate mitophagy. Autophagy. 2014;10:1906-1920. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 98] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 158. | Kim YM, Jung CH, Seo M, Kim EK, Park JM, Bae SS, Kim DH. mTORC1 phosphorylates UVRAG to negatively regulate autophagosome and endosome maturation. Mol Cell. 2015;57:207-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 221] [Article Influence: 20.1] [Reference Citation Analysis (0)] |
| 159. | Saha S, Panigrahi DP, Patil S, Bhutia SK. Autophagy in health and disease: A comprehensive review. Biomed Pharmacother. 2018;104:485-495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 280] [Cited by in RCA: 384] [Article Influence: 54.9] [Reference Citation Analysis (0)] |
| 160. | Wang GY, Bi YG, Liu XD, Zhao Y, Han JF, Wei M, Zhang QY. Autophagy was involved in the protective effect of metformin on hyperglycemia-induced cardiomyocyte apoptosis and Connexin43 downregulation in H9c2 cells. Int J Med Sci. 2017;14:698-704. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 43] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 161. | Yang F, Zhang L, Gao Z, Sun X, Yu M, Dong S, Wu J, Zhao Y, Xu C, Zhang W, Lu F. Exogenous H2S Protects Against Diabetic Cardiomyopathy by Activating Autophagy via the AMPK/mTOR Pathway. Cell Physiol Biochem. 2017;43:1168-1187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 59] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 162. | Denaës T, Lodder J, Chobert MN, Ruiz I, Pawlotsky JM, Lotersztajn S, Teixeira-Clerc F. The Cannabinoid Receptor 2 Protects Against Alcoholic Liver Disease Via a Macrophage Autophagy-Dependent Pathway. Sci Rep. 2016;6:28806. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 76] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 163. | Ke P, Shao BZ, Xu ZQ, Wei W, Han BZ, Chen XW, Su DF, Liu C. Activation of Cannabinoid Receptor 2 Ameliorates DSS-Induced Colitis through Inhibiting NLRP3 Inflammasome in Macrophages. PLoS One. 2016;11:e0155076. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 70] [Cited by in RCA: 85] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 164. | Shao BZ, Wei W, Ke P, Xu ZQ, Zhou JX, Liu C. Activating cannabinoid receptor 2 alleviates pathogenesis of experimental autoimmune encephalomyelitis via activation of autophagy and inhibiting NLRP3 inflammasome. CNS Neurosci Ther. 2014;20:1021-1028. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 119] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 165. | Pei Z, Deng Q, Babcock SA, He EY, Ren J, Zhang Y. Inhibition of advanced glycation endproduct (AGE) rescues against streptozotocin-induced diabetic cardiomyopathy: Role of autophagy and ER stress. Toxicol Lett. 2018;284:10-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 49] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 166. | Xiao Y, Wu QQ, Duan MX, Liu C, Yuan Y, Yang Z, Liao HH, Fan D, Tang QZ. TAX1BP1 overexpression attenuates cardiac dysfunction and remodeling in STZ-induced diabetic cardiomyopathy in mice by regulating autophagy. Biochim Biophys Acta Mol Basis Dis. 2018;1864:1728-1743. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 47] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 167. | Wu A, Hu P, Lin J, Xia W, Zhang R. Activating Cannabinoid Receptor 2 Protects Against Diabetic Cardiomyopathy Through Autophagy Induction. Front Pharmacol. 2018;9:1292. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 168. | Xu K, Liu XF, Ke ZQ, Yao Q, Guo S, Liu C. Resveratrol Modulates Apoptosis and Autophagy Induced by High Glucose and Palmitate in Cardiac Cells. Cell Physiol Biochem. 2018;46:2031-2040. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 44] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 169. | Zhou B, Leng Y, Lei SQ, Xia ZY. AMPK activation restores ischemic postconditioning cardioprotection in STZinduced type 1 diabetic rats: Role of autophagy. Mol Med Rep. 2017;16:3648-3656. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 170. | Böckmann S, Hinz B. Cannabidiol Promotes Endothelial Cell Survival by Heme Oxygenase-1-Mediated Autophagy. Cells. 2020;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 38] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 171. | Lin TK, Chen SD, Chuang YC, Lin HY, Huang CR, Chuang JH, Wang PW, Huang ST, Tiao MM, Chen JB, Liou CW. Resveratrol partially prevents rotenone-induced neurotoxicity in dopaminergic SH-SY5Y cells through induction of heme oxygenase-1 dependent autophagy. Int J Mol Sci. 2014;15:1625-1646. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 112] [Cited by in RCA: 125] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 172. | Surolia R, Karki S, Kim H, Yu Z, Kulkarni T, Mirov SB, Carter AB, Rowe SM, Matalon S, Thannickal VJ, Agarwal A, Antony VB. Heme oxygenase-1-mediated autophagy protects against pulmonary endothelial cell death and development of emphysema in cadmium-treated mice. Am J Physiol Lung Cell Mol Physiol. 2015;309:L280-L292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 60] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 173. | Waltz P, Carchman EH, Young AC, Rao J, Rosengart MR, Kaczorowski D, Zuckerbraun BS. Lipopolysaccaride induces autophagic signaling in macrophages via a TLR4, heme oxygenase-1 dependent pathway. Autophagy. 2011;7:315-320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 101] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 174. | Schwartz M, Böckmann S, Hinz B. Up-regulation of heme oxygenase-1 expression and inhibition of disease-associated features by cannabidiol in vascular smooth muscle cells. Oncotarget. 2018;9:34595-34616. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 28] [Article Influence: 4.0] [Reference Citation Analysis (0)] |