Published online Jun 15, 2021. doi: 10.4239/wjd.v12.i6.780
Peer-review started: January 13, 2021
First decision: April 20, 2021
Revised: April 23, 2021
Accepted: May 19, 2021
Article in press: May 19, 2021
Published online: June 15, 2021
Processing time: 141 Days and 15.9 Hours
The new coronavirus disease 2019 (COVID-19) pandemic posed a great burden on health care systems worldwide and is an enormous and real obstacle in providing needed health care to patients with chronic diseases such as diabetes. Parallel to COVID-19, there have been great advances in technology used for management of type 1 diabetes, primarily insulin pumps, sensors, integrated and closed loop systems, ambulatory glucose profile software, and smart phone apps providing necessary essentials for telemedicine implementation right at the beginning of the COVID-19 pandemic. The results of these remote interventions are reassuring in terms of glycemic management and hemoglobin A1c reductions. However, data on long-term outcomes and cost reductions are missing as well as proper technical infrastructure and government health policy support.
Core Tip: Mortality and morbidity rates increased during the coronavirus disease 2019 pandemic partially due to disruption in health care delivery. The implementation of telemedicine imposes itself as a logical solution given technical devices and apps already available in the management of type 1 diabetes. Presently available data are scarce but encouraging regarding glycemic control in long standing type 1 diabetes and new onset type 1 diabetes and minimizing acute complications.
- Citation: Bilic Curcic I, Cigrovski Berkovic M, Kizivat T, Canecki Varzic S, Smolic R, Smolic M. Effect of COVID-19 on management of type 1 diabetes: Pushing the boundaries of telemedical healthcare. World J Diabetes 2021; 12(6): 780-785
- URL: https://www.wjgnet.com/1948-9358/full/v12/i6/780.htm
- DOI: https://dx.doi.org/10.4239/wjd.v12.i6.780
The coronavirus disease 2019 (COVID-19) pandemic is one of the biggest challenges humanity has ever encountered with unfathomable aftermaths on all aspects of our lives including the health care system or rather the disruption of health care delivery.
Interestingly, diabetes and COVID-19 are both pandemics with distinct opposite features. The COVID-19 pandemic is a newly emerged infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). In the short period of time, it caused over 1850941 deaths[1] rising as a global emergency and changing the face of health care provision in a short period of time. On the other hand, diabetes is a slow pandemic, and one of the leading causes of mortality and morbidity worldwide responsible for over 42 million deaths in 2019[2].
Moreover, clinical presentation of SARS-CoV-2 infection tends to be more severe with increased mortality rates in people with type 1 and type 2 diabetes, especially those with poor glycemic regulation and accompanying comorbidities such as obesity, kidney impairment, and cardiovascular disease[3,4]. An increase in mortality rates in diabetic patients, both type 1 and type 2, has been observed in the first 3 mo of 2020 compared with the same period in the 5 years prior (from 2014 to 2019), which could be a consequence of inadequate health care as well as COVID-19[3] emphasizing an urgent need for practical solutions in remote outpatient health care.
If anything, the COVID-19 pandemic accelerated the implementation of telemedicine worldwide due to mandatory social distancing, and many patients’ health care providers were discovering benefits attached to remote health care[5]. Patients can receive guidance and consulting from their homes thus avoiding a potential virus threat, saving time and costs of travel and parking, which is especially convenient for children and the working population.
This form of diabetes management is particularly appropriate for type 1 patients already using available software, such as Dexcom, Care Link, or LabVIEW, able to generate ambulatory glucose profile reports, and using smart insulin pens thus allowing remote monitoring of glucose management and providing consultations based on available data via phone, video calls, or smart phone applications[6-8].
Indeed, the digital revolution commenced in the type 1 community starting with insulin pumps, advancing with sensors, integrated and closed loop systems, ambulatory glucose profile software, and smart phone apps procuring necessary essentials for swift and timely telemedicine implementation right at the beginning of the COVID-19 pandemic[9].
This was clearly shown in a study performed in Italy during the COVID-19 lockdown including people with type 1 diabetes using the hybrid closed loop demonstrating improved glycemic control probably due to the availability of telemedicine and more active engagement of patients in glycemic management[10].
A study conducted on type 1 diabetes patients from 89 countries encompassing 7477 survey responses showed that 30% believed their healthcare access was negatively affected, while 28% received remote care through telephone (72%) or video calls (28%). The majority of those patients considered teleconsulting useful, and hemoglobin A1c levels positively correlated with affirmative attitude towards telemedicine[11].
In the pre-COVID-19 era, virtual consultations have proven useful, effective, and accessible in type 2 diabetes management compared to face-to-face visits[12,13]. Still, outcomes in terms of glycated hemoglobin vary by studies. For instance, Cochrane meta-analysis of 21 studies comparing standard care to telemedicine in diabetic patients demonstrated inconsistent results in hemoglobin A1c improvement but a better effect on low density lipoprotein and blood pressure levels[14]. Another study showed improvement in hemoglobin A1c levels. However, strong technical support was engaged including connected devices such as continuous glucose monitoring, remote lifestyle coaching, and clinical support with a mobile app, which are not usually on disposal for type 2 diabetes patients[15].
Data on telemedicine and type 2 diabetes in the COVID-19 era are still lacking. In a recently published study including 763 type 1 and 619 type 2 diabetics, about 40% of patients stated that all of their diabetes visits were cancelled or postponed, 40% were switched to telehealth consultations, while half reported lower overall satisfaction with these visits[16].
Infection with SARS-CoV-2 causes an inexplicable rise in glycemia, probably due to direct toxic effects of the virus itself and wide expression of angiotensin converting enzyme 2 on islet cells[17,18] presenting with acute hyperglycemia followed by ketosis or even ketoacidosis requiring an emergency room visit even in previously well-controlled patients[19,20].
Telemedicine is allowing a continuous and remote communication between patients and their health care provider and in terms of COVID-19-induced acute hyper
Recently, two case reports were published, one adult and the other pediatric, where telemedicine was effectively applied in all aspects of type 1 diabetes management, consultation, education, and monitoring through available software to generate ambulatory glucose profiles and using a combination of e-mail, Internet via Zoom, and telephone calls[22].
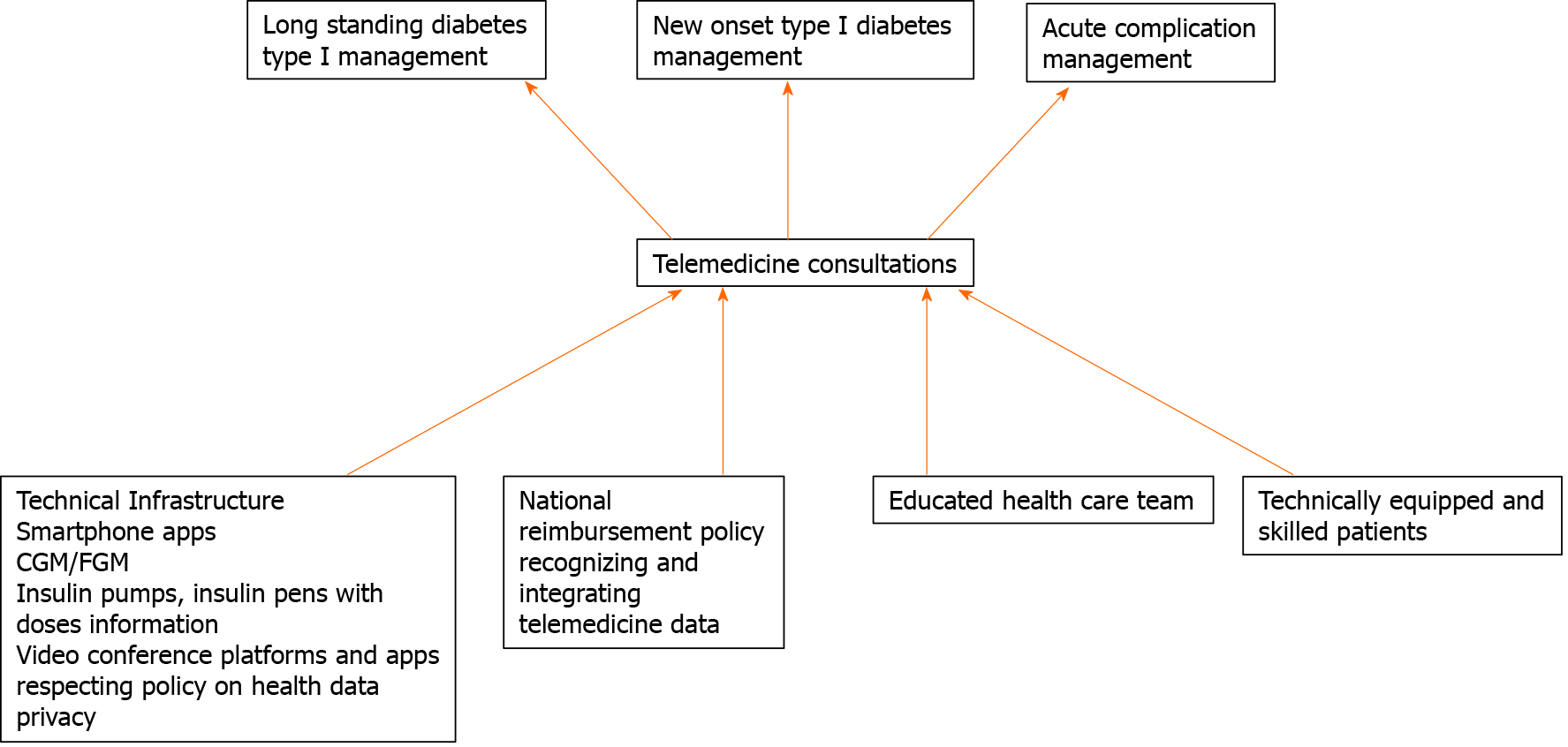
The major obstacle in telemedicine implementation are technical support issues and government reimbursement policies, which differ by country. Structured background for integration and reimbursement in most countries is missing. There are two options presented, one involving private providers depending on private insurance and the other based on free applications such as WhatsApp, Skype, or Zoom that are not in accordance with health data privacy conditions and are not an integrated part of health care registries[23]. In most countries, health insurance covers the costs of technical devices in the management of type 1 diabetes, which is not the case for type 2 diabetes. Precisely for this reason telemedicine is the most widely used in long standing type 1 diabetes management but also has potential in new onset type 1 diabetes and prevention of acute complications, especially important in the COVID-19 era (Figure 1).
Downloading data from devices is a weak link in wider implementation of telemedicine because the older population is not skilled enough or do not have technical support necessary to prepare reports for consults. Unfortunately, this population in particular could benefit the most from remote consulting due to vulnerability to SARS-CoV-2 and other infections, walking disabilities, and poorer socioeconomic status. In addition, the majority of those patients do not have smart phones and do not use the internet frequently. Thus, improvements in user support services are necessary at this stage to resolve issues in service delivery[5].
The main question is could telemedicine replace face-to-face visits? One could argue that even if we have necessary data regarding glycemic management, we still could not perform a physical exam in order to evaluate cardiovascular health or polyneuropathy. It should be emphasized that telemedicine in retinopathy screening has been long recognized[24]. On the other hand, telemedicine and constant contact with patients enables physicians to act in time, to give advice regarding hypo- or hyperglycemia, adjust insulin doses, and provide proper actions in case of emergencies.
The potential in cost reductions and advancements of health care are plausible and supported by a recently published meta-analysis including 8 studies investigating a role of telemedicine in the COVID-19 pandemic confirming that telehealth care improves accessibility of health services[25]. However, there are no definite reports on long-term outcomes or cost reduction necessary for creating government health care policies as well as building technical infrastructure.
Nonetheless, virtual consultations and/or clinics are inevitable and essential in providing healthcare in this pandemic, securing communication between type 2 diabetes patients and health care providers necessary in supporting self-management. Based on present data, technical infrastructure is imperative in delivering high quality consultations ensuring patient satisfaction.
Manuscript source: Invited manuscript
Specialty type: Endocrinology and metabolism
Country/Territory of origin: Croatia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bansal A, Liu YC S-Editor: Zhang L L-Editor: Filipodia P-Editor: Ma YJ
| 1. | Worldometer. COVID-19 coronavirus pandemic 2021. [cited 1 January 2021]. Available from: www.worldometers.info/coronavirus/. |
| 2. | International Diabetes Federation. IDF Diabetes Atlas, 8th ed. Brussels, Belgium: 2019. [cited May 4, 2020]. Available from: www.idf.org/e-library/epidemiology-research/diabetes-atlas/134-idf-diabetes-atlas-8th-edition.html. |
| 3. | Holman N, Knighton P, Kar P, O'Keefe J, Curley M, Weaver A, Barron E, Bakhai C, Khunti K, Wareham NJ, Sattar N, Young B, Valabhji J. Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: a population-based cohort study. Lancet Diabetes Endocrinol. 2020;8:823-833. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 620] [Cited by in RCA: 610] [Article Influence: 122.0] [Reference Citation Analysis (0)] |
| 4. | Williamson EJ, Walker AJ, Bhaskaran K, Bacon S, Bates C, Morton CE, Curtis HJ, Mehrkar A, Evans D, Inglesby P, Cockburn J, McDonald HI, MacKenna B, Tomlinson L, Douglas IJ, Rentsch CT, Mathur R, Wong AYS, Grieve R, Harrison D, Forbes H, Schultze A, Croker R, Parry J, Hester F, Harper S, Perera R, Evans SJW, Smeeth L, Goldacre B. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584:430-436. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4343] [Cited by in RCA: 4193] [Article Influence: 838.6] [Reference Citation Analysis (0)] |
| 5. | Wake DJ, Gibb FW, Kar P, Kennon B, Klonoff DC, Rayman G, Rutter MK, Sainsbury C, Semple RK. ENDOCRINOLOGY IN THE TIME OF COVID-19: Remodelling diabetes services and emerging innovation. Eur J Endocrinol. 2020;183:G67-G77. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 43] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 6. | Battelino T, Danne T, Bergenstal RM, Amiel SA, Beck R, Biester T, Bosi E, Buckingham BA, Cefalu WT, Close KL, Cobelli C, Dassau E, DeVries JH, Donaghue KC, Dovc K, Doyle FJ 3rd, Garg S, Grunberger G, Heller S, Heinemann L, Hirsch IB, Hovorka R, Jia W, Kordonouri O, Kovatchev B, Kowalski A, Laffel L, Levine B, Mayorov A, Mathieu C, Murphy HR, Nimri R, Nørgaard K, Parkin CG, Renard E, Rodbard D, Saboo B, Schatz D, Stoner K, Urakami T, Weinzimer SA, Phillip M. Clinical Targets for Continuous Glucose Monitoring Data Interpretation: Recommendations From the International Consensus on Time in Range. Diabetes Care. 2019;42:1593-1603. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1491] [Cited by in RCA: 2324] [Article Influence: 387.3] [Reference Citation Analysis (0)] |
| 7. | Sangave NA, Aungst TD, Patel DK. Smart Connected Insulin Pens, Caps, and Attachments: A Review of the Future of Diabetes Technology. Diabetes Spectr. 2019;32:378-384. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 49] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 8. | Iyengar K, Upadhyaya GK, Vaishya R, Jain V. COVID-19 and applications of smartphone technology in the current pandemic. Diabetes Metab Syndr. 2020;14:733-737. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 158] [Cited by in RCA: 119] [Article Influence: 23.8] [Reference Citation Analysis (0)] |
| 9. | Danne T, Limbert C. COVID-19, type 1 diabetes, and technology: why paediatric patients are leading the way. Lancet Diabetes Endo. 2020;8:465-467. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 10. | Longo M, Caruso P, Petrizzo M, Castaldo F, Sarnataro A, Gicchino M, Bellastella G, Esposito K, Maiorino MI. Glycemic control in people with type 1 diabetes using a hybrid closed loop system and followed by telemedicine during the COVID-19 pandemic in Italy. Diabetes Res Clin Pract. 2020;169:108440. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 36] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 11. | Scott SN, Fontana FY, Züger T, Laimer M, Stettler C. Use and perception of telemedicine in people with type 1 diabetes during the COVID-19 pandemic-Results of a global survey. Endocrinol Diabetes Metab. 2021;4:e00180. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 41] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 12. | Armstrong N, Hearnshaw H, Powell J, Dale J. Stakeholder perspectives on the development of a virtual clinic for diabetes care: qualitative study. J Med Internet Res. 2007;9:e23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 22] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 13. | Greenhalgh T, Vijayaraghavan S, Wherton J, Shaw S, Byrne E, Campbell-Richards D, Bhattacharya S, Hanson P, Ramoutar S, Gutteridge C, Hodkinson I, Collard A, Morris J. Virtual online consultations: advantages and limitations (VOCAL) study. BMJ Open. 2016;6:e009388. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 162] [Cited by in RCA: 158] [Article Influence: 17.6] [Reference Citation Analysis (0)] |
| 14. | Flodgren G, Rachas A, Farmer AJ, Inzitari M, Shepperd S. Interactive telemedicine: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2015;CD002098. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 259] [Cited by in RCA: 367] [Article Influence: 36.7] [Reference Citation Analysis (0)] |
| 15. | Dixon RF, Zisser H, Layne JE, Barleen NA, Miller DP, Moloney DP, Majithia AR, Gabbay RA, Riff J. A Virtual Type 2 Diabetes Clinic Using Continuous Glucose Monitoring and Endocrinology Visits. J Diabetes Sci Technol. 2020;14:908-911. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 58] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 16. | Fisher L, Polonsky W, Asuni A, Jolly Y, Hessler D. The early impact of the COVID-19 pandemic on adults with type 1 or type 2 diabetes: A national cohort study. J Diabetes Complications. 2020;34:107748. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 68] [Cited by in RCA: 79] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 17. | Bindom SM, Lazartigues E. The sweeter side of ACE2: physiological evidence for a role in diabetes. Mol Cell Endocrinol. 2009;302:193-202. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 168] [Cited by in RCA: 160] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 18. | Yang JK, Lin SS, Ji XJ, Guo LM. Binding of SARS coronavirus to its receptor damages islets and causes acute diabetes. Acta Diabetol. 2010;47:193-199. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 686] [Cited by in RCA: 780] [Article Influence: 52.0] [Reference Citation Analysis (0)] |
| 19. | Li J, Wang X, Chen J, Zuo X, Zhang H, Deng A. COVID-19 infection may cause ketosis and ketoacidosis. Diabetes Obes Metab. 2020;22:1935-1941. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 285] [Cited by in RCA: 392] [Article Influence: 78.4] [Reference Citation Analysis (0)] |
| 20. | Kim NY, Ha E, Moon JS, Lee YH, Choi EY. Acute Hyperglycemic Crises with Coronavirus Disease-19: Case Reports. Diabetes Metab J. 2020;44:349-353. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 73] [Cited by in RCA: 73] [Article Influence: 14.6] [Reference Citation Analysis (1)] |
| 21. | Cassar MR, Borg D, Camilleri L, Schembri A, Anastasi EA, Buhagiar K, Callus C, Grech M. A novel use of telemedicine during the COVID-19 pandemic. Int J Infect Dis. 2021;103:182-187. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 22. | Garg SK, Rodbard D, Hirsch IB, Forlenza GP. Managing New-Onset Type 1 Diabetes During the COVID-19 Pandemic: Challenges and Opportunities. Diabetes Technol Ther. 2020;22:431-439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 109] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 23. | Ohannessian R, Duong TA, Odone A. Global Telemedicine Implementation and Integration Within Health Systems to Fight the COVID-19 Pandemic: A Call to Action. JMIR Public Health Surveill. 2020;6:e18810. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 549] [Cited by in RCA: 592] [Article Influence: 118.4] [Reference Citation Analysis (0)] |
| 24. | Zimmer-Galler IE, Kimura AE, Gupta S. Diabetic retinopathy screening and the use of telemedicine. Curr Opin Ophthalmol. 2015;26:167-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 70] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 25. | Monaghesh E, Hajizadeh A. The role of telehealth during COVID-19 outbreak: a systematic review based on current evidence. BMC Public Health. 2020;20:1193. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 995] [Cited by in RCA: 946] [Article Influence: 189.2] [Reference Citation Analysis (0)] |