Published online Jul 15, 2020. doi: 10.4239/wjd.v11.i7.269
Peer-review started: February 17, 2020
First decision: May 5, 2020
Revised: May 11, 2020
Accepted: May 28, 2020
Article in press: May 28, 2020
Published online: July 15, 2020
Processing time: 147 Days and 12.5 Hours
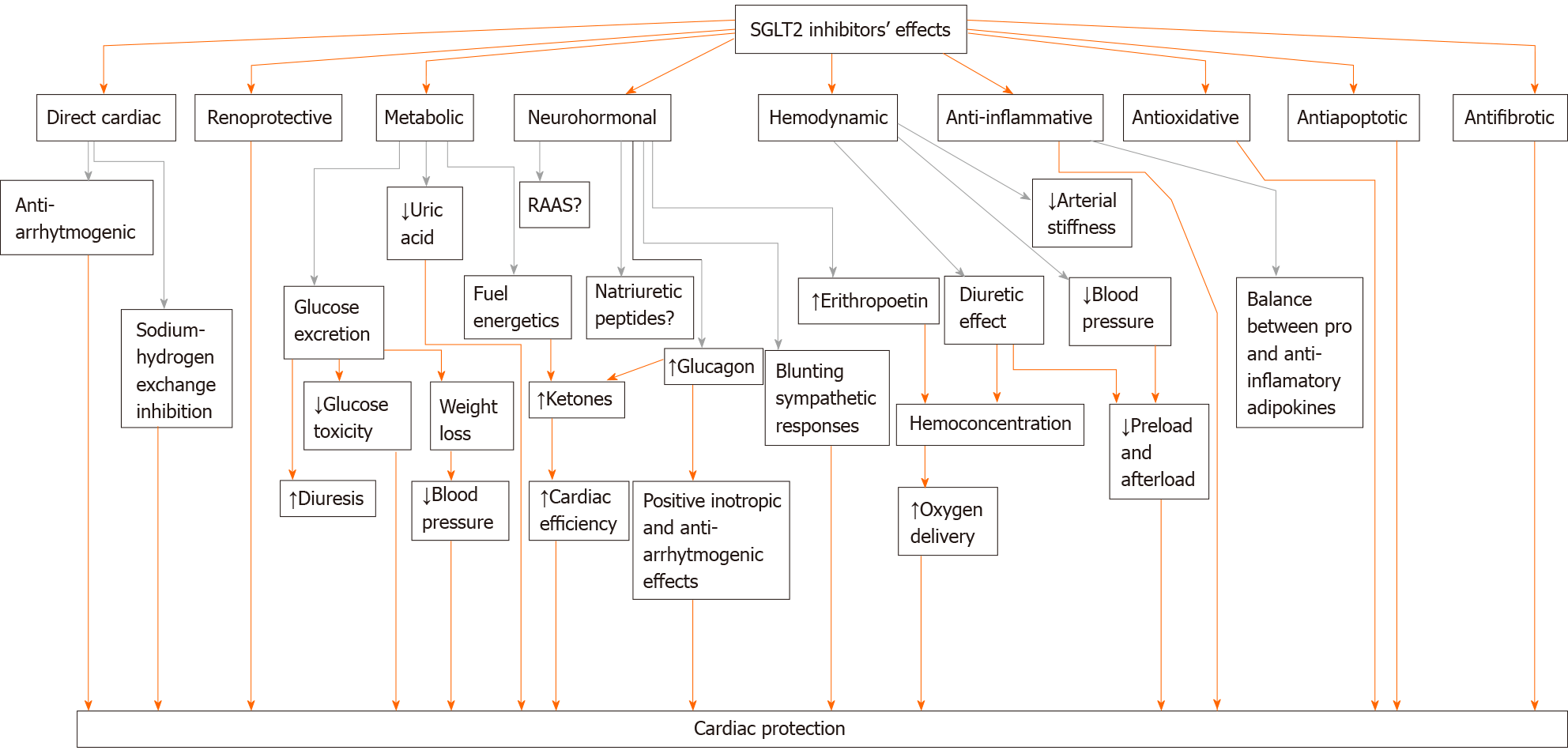
Three major cardiovascular outcome trials (CVOTs) with a new class of antidiabetic drugs - sodium-glucose cotransporter 2 (SGLT2) inhibitors (EMPA-REG OUTCOME trial with empagliflozin, CANVAS Program with canagliflozin, DECLARE-TIMI 58 with dapagliflozin) unexpectedly showed that cardiovascular outcomes could be improved possibly due to a reduction in heart failure risk, which seems to be the most sensitive outcome of SGLT2 inhibition. No other CVOT to date has shown any significant benefit on heart failure events. Even more impressive findings came recently from the DAPA-HF trial in patients with confirmed and well-treated heart failure: Dapagliflozin was shown to reduce heart failure risk for patients with heart failure with reduced ejection fraction regardless of diabetes status. Nevertheless, despite their possible wide clinical implications, there is much doubt about the mechanisms of action and a lot of questions to unravel, especially now when their benefits translated to non-diabetic patients, rising doubts about the validity of some current mechanistic assumptions.The time frame of their cardiovascular benefits excludes glucose-lowering and antiatherosclerotic-mediated effects and multiple other mechanisms, direct cardiac as well as systemic, are suggested to explain their early cardiorenal benefits. These are: Anti-inflammatory, antifibrotic, antioxidative, antiapoptotic properties, then renoprotective and hemodynamic effects, attenuation of glucotoxicity, reduction of uric acid levels and epicardial adipose tissue, modification of neurohumoral system and cardiac fuel energetics, sodium-hydrogen exchange inhibition. The most logic explanation seems that SGLT2 inhibitors timely target various mechanisms underpinning heart failure pathogenesis. All the proposed mechanisms of their action could interfere with evolution of heart failure and are discussed separately within the main text.
Core tip: Three major cardiovascular outcome trials with a new class of antidiabetic drugs-sodium-glucose cotransporter 2 inhibitors unexpectedly showed that cardiovascular outcomes could be improved due to a reduction in heart failure events. Moreover, recently dapagliflozin was shown to reduce heart failure risk for patients with heart failure with reduced ejection fraction regardless of diabetic status. Currently, there is much doubt regarding the mechanisms of action of these drugs. The most logic explanation is that they are timely targeting various mechanisms underpinning heart failure pathogenesis due to pleiotropic effects which are discussed in the main text.
- Citation: Grubić Rotkvić P, Cigrovski Berković M, Bulj N, Rotkvić L, Ćelap I. Sodium-glucose cotransporter 2 inhibitors’ mechanisms of action in heart failure. World J Diabetes 2020; 11(7): 269-279
- URL: https://www.wjgnet.com/1948-9358/full/v11/i7/269.htm
- DOI: https://dx.doi.org/10.4239/wjd.v11.i7.269
Atherosclerotic cardiovascular disease is the leading cause of morbidity and mortality among diabetic patients. Due to US Food and Drug Administration requirements, since 2008 a series of large clinical trials with new hypoglycemic drugs have been designed to rule out cardiovascular harm and to show noninferiority on the cardiovascular outcomes while improving glucose control[1]. Three major cardiovascular outcome trials (CVOTs) with a new class of drugs - sodium-glucose cotransporter 2 (SGLT2) inhibitors (EMPA-REG OUTCOME trial with empagliflozin, CANVAS Program with canagliflozin, DECLARE-TIMI 58 with dapagliflozin; Table 1 unexpectedly showed that cardiovascular outcomes could be improved possibly due to a reduction in heart failure risk, which seems to be the most sensitive outcome of SGLT2 inhibition[2-4]. It is worthwhile to mention that no other CVOT to date has shown any significant benefit on heart failure events[5].These observations set the stage for the new game changers in cardiometabolic pharmacotherapy and opened up new possibilities in heart failure strategies, along with its standard medical therapy with neurohormonal antagonists [mineralocorticoid receptor antagonists, β-blockers, angiotensin-converting enzyme (ACE) inhibitors/angiotensin receptor blockers(ARBs), neprilysin inhibitors]. American Diabetes Association has already recommended new strategies in the treatment of diabetic patients with established atherosclerotic cardiovascular disease and patients with heart failure, and that is the preferential use of SGLT2 inhibitors (empa-, dapa- and canagliflozin) in these patients[1]. Furthermore, even more impressive findings came recently from the DAPA-HF trial in patients with confirmed and well-treated heart failure: dapagliflozin was shown to reduce heart failure risk in patients with heart failure with reduced ejection fraction (HFrEF) regardless of their diabetic status[6]. So, at present, there are evidences that these new drugs work both for diabetic and nondiabetic patients, regardless of existing atherosclerotic cardiovascular disease or heart failure, and probably in both HFrEF and heart failure with preserved ejection fraction (HFpEF), making them unique and important for clinical practice[7,8]. Nevertheless, despite their possible wide clinical implications, there is much doubt regarding the mechanisms of action and a lot of questions still left to unravel. While scientific and professional community is struggling in pursuing those answers, at the same time, we are expecting the results of several ongoing studies of SGLT2 inhibitors in heart failure to fully evaluate their therapeutic potential. In this review we will try to give some mechanistic insights of SGLT2 inhibitors’ mode of action regarding heart failure, from current hypotheses of possible mechanisms of action to explain cardiac protection to the controversies and gaps in evidence, as well as potential future developments in the field.
| Parameters | EMPA-REG OUTCOME | CANVAS program | DECLARE-TIMI 58 |
| Intervention | Empagliflozin/placebo | Canagliflozin/placebo | Dapagliflozin/placebo |
| Median follow-up (yr) | 3.1 | 3.6 | 4.2 |
| Number of patients | 7020 | 10142 | 17160 |
| Prior cardiovascular disease/heart failure (%) | 99/10 | 65.6/14.4 | 40/10 |
| Primary outcome (3-point MACE) | 0.86 (95%CI: 0.74-0.99) Noninferiority, P < 0.001; Superiority, P = 0.04 | 0.86 (95%CI: 0.75-0.97) Noninferiority, P < 0.001; Superiority, P = 0.02 | 0.93 (95%CI: 0.84-1.03) Noninferiority, P < 0.001; Superiority, P = 0.17 |
| Cardiovascular death | 0.62 (0.49-0.77)1 | 0.87 (0.72-1.06) | 0.98 (0.81-1.17) |
| Myocardial infarction | 0.87 (0.70-1.09) | 0.89 (0.73-1.09) | 0.89 (0.77-1.01) |
| Stroke | 1.18 (0.89-1.56) | 0.87 (0.69-1.09) | 1.01 (0.84-1.21) |
| Heart failure hospitalization | 0.65 (0.50-0.85)1 | 0.67 (0.52-0.87)1 | 0.73 (0.61-0.88)1 |
| All cause mortality | 0.68 (0.57-0.82)1 | 0.87 (0.74-1.01) | 0.93 (0.82-1.04) |
Sodium-dependent glucose cotransporters are a family of active glucose transporter proteins. SGLT1 is widely expressed in numerous organs (heart, liver, small intestine, lung, kidney), while SGLT2 is mainly expressed in the renal proximal tubule. Under normal conditions, glucose is filtered into the urine at the glomerulus and reabsorbed in the proximal tubuli by SGLT2 (90%) and SGLT1 (the remaining 10%). In hyperglycemic conditions SGLT2 expression is increased, paradoxically augmenting the threshold for urinary glucose excretion in diabetic patients. SGLT2 inhibitors are a novel class of antidiabetic agents that promote urinary glucose excretion by inhibiting glucose and sodium reabsorption from the renal proximal tubules and have recently been investigated in several large randomized controlled trials for cardiovascular safety and efficacy in patients with type 2 diabetes[9-11]. Enhancing urinary glucose excretion by targeting SGLT2 represents an alternative strategy to the traditional antihyperglycemic interventions that have been focused on restoring β-cell activity, insulin sensitivity or tissue glucose uptake to normalize plasma glucose levels in patients with diabetes. SGLT2 inhibitors are generally well tolerated, and the risk of hypoglycemia is low because the efficacy of SGLT2 inhibitors to increase glucose excretion attenuates at lower plasma glucose levels[12,13]. Since regulatory agencies have issued safety warnings for several adverse events (urinary tract infections, diabetic ketoacidosis, acute kidney injury, bone fractures, lower limb amputations) based primarily on case report data, a meta-analysis of randomized controlled trials with SGLT2 inhibitors was performed and concluded that current evidences do not suggest an increased risk of harm with SGLT2 inhibitors as a class over placebo or active comparators with respect to acute kidney injury, diabetic ketoacidosis, urinary tract infections and bone fractures[14]. Further research is required to ascertain whether there is an increased risk of amputations associated with SGLT2 inhibitors. Evidence on the risk of lower limb amputations is limited to the results from CANVAS trial. There was an increased risk of amputations, although the overall incidence of these events was low and the study was not powerful enough to detect significant differences among the studied population[13,14].
According to a recent meta-analysis of the three major CVOTs with these drugs (the EMPA-REG OUTCOME trial, the CANVAS Program and the DECLARE-TIMI 58 trial), even though the exact inclusion criteria and definitions of endpoints varied among them, the presence of established atherosclerotic disease and heart failure was investigator-reported and no heart failure phenotyping was performed, SGLT2 inhibitors, as a class, have moderate benefits on atherosclerotic major adverse cardiovascular events in patients with established atherosclerotic cardiovascular disease but also have robust benefits on reducing hospitalization for heart failure and progression of renal disease regardless of existing atherosclerotic disease or a history of heart failure (they reduced the risk of heart failure hospitalization by 31% and progression of renal disease by 45%)[6,15]. This efficacy in the prevention (primary as well as secondary) of heart failure has already translated to efficacy in the treatment of heart failure as shown in the above-mentioned DAPA-HF trial including patients with HFrEF. But SGLT2 inhibitors may also be valuable in the treatment of HFpEF according to the subanalyses of CVOTs and accumulating mechanistic insights[8,16,17]. Till now, in trials of HFpEF, several established treatments for HFrEF have shown no efficacy. So, if results of ongoing studies with SGLT2 inhibitors in HFpEF would show effectiveness, this will represent a true breakthrough in heart failure treatment (Table 2).
| Trial | Drug | Ejection fraction | Diabetic/nondiabetic |
| Emperor-reduced | empagliflozin | HFrEF | Both |
| Emperor-preserved | empagliflozin | HFpEF | Both |
| Deliver | dapagliflozin | HFpEF | Both |
Heart failure comprises an array of patients categorized by their symptoms and ejection fraction (HFrEF with EF < 40%, midrange EF between 40% and 49%, and HFpEF with EF > 50%). It is a growing public health problem, with an estimated 63 million people affected worldwide[16]. Heart failure has a progressive nature and preventive strategies have to be adopted early because starting treatment at the preclinical stage may improve its outcomes[18]. Hospitalization for heart failure carries a 10% mortality rate at 30 days postdischarge, 20% at 1 year, the readmission rate at 6 months is 50%, and the risk of mortality is greater with each hospitalization[16]. Despite established treatment options for HFrEF that are associated with reduced mortality, the prognosis of heart failure is still very poor. In the recent US study of Shah et al[19] patients across the ejection fraction spectrum have a similarly 5-year mortality around 75% with an elevated risk for heart failure and cardiovascular hospitalizations. These data warn us that treatment strategies of patients with heart failure need to be improved.
Heart failure is a particularly common complication of diabetes, with poor 5-year survival rates, but it seems to have been neglected because more attention was given to atherothrombotic complications of disease. Furthermore, patients with diabetes are predisposed to a distinct cardiomyopathy - diabetic cardiomyopathy which is independent of concomitant diabetic macro- and microvascular complications. It is still poorly understood, but of great clinical importance, given the robust association of diabetes mellitus with heart failure and increased cardiovascular mortality[20,21]. Could SGLT2 inhibitors be the new heart savers in diabetes and beyond diabetes? How is their effect so ubiquitous across the spectrum of heart failure? Are we missing something in the pathophysiology of heart failure or there is just a lot of work to do with the pleiotropic mechanisms of SGLT2 inhibitors? There are still a lot of questions regarding SGLT2 inhibitors that are awaiting answers.
Physiological mechanisms responsible for SGLT2 inhibitors’ benefits are not yet well defined and the situation has become even more complicated since their benefits have recently translated to non-diabetic patients which raised doubts about the validity of some current mechanistic assumptions. The time frame of their effects excludes glucose-lowering and antiatherosclerotic-mediated mechanism of action[22]. Namely, separation of the cardiovascular event curves for SGLT2 inhibitors occurred early in the studies and persisted for the entire duration of the treatment than would be expected from effects on atherosclerosis. Furthermore, it is known that hyperglycemia is a weak risk for cardiovascular disease[23,24]. So, multiple different mechanisms, direct cardiac as well as systemic, are suggested to explain the early cardiorenal benefits of SGLT2 inhibitors seen in CVOTs and they are presented in Figure 1 and discussed below: (1) Lowering elevated blood glucose levels with SGLT2 inhibitors which promote glucose excretion and not uptake could reduce glucose toxicity, improve β-cell function and insulin sensitivity as it was shown in the metabolic study of Ferrannini et al[25]. Reduced effects of glucotoxicity on the heart, could also reduce the risk of heart failure in diabetic patients[23]. But as it was shown in DAPA-HF, the benefits of dapaglifozin on the progression of heart failure occurred regardless of diabetes, which somehow undermine the hypothesis of glucotoxicity[24]. Nevertheless, it could be that in the group of patients with diabetic cardiomyopathy this particular mechanism played a role; (2) Reduced body fat and fluid loss are observed with SGLT2 inhibition due to glucose excretion. This could partially account for the blood pressure reduction, weight loss and, even though the magnitude of this effects is modest, could contribute to cardiovascular risk reduction and heart unloading[26-28]; (3) SGLT2 inhibitors produce natriuresis and osmotic diuresis that in turn cause a reduction in blood pressure and intravascular volume and in this way simultaneously reduce both preload and afterload of the heart which could give rapid results observed with SGLT2 inhibitors. Reduced arterial stiffness observed with SGLT2 inhibition and, as already mentioned, weight loss also contribute to blood pressure lowering[29]. However, how could this affect primary heart failure prevention and to which extent it can play a role in non- diabetic patients when it is known that SGLT2 inhibitors induce a greater level of glycosuria (consequently osmotic diuresis) in patients with diabetes compared to normal individuals, needs to be clarified[30]. Furthermore, previous investigations did not show that commonly used diuretics were associated with reduction in cardiovascular death, while in CVOTs and DAPA-HF, SGLT2 inhibitors reduced cardiovascular death as well as sudden death[24]; (4) Therapy with SGLT2 inhibitors is associated with small plasma uric acid reduction but this potential benefit requires further investigation[31]. It is known that uric acid may be associated with an adverse prognosis in heart failure and may play a causative role in metabolic syndrome, hypertension, renal damage or endothelial dysfunction[32,33]. In rats, hypertension associated with hyperuricemia is linked to reduced expression of macula densa neuronal nitric oxide synthase. This synthase affects cardiac function facilitating sarcoplasmic reticulum calcium release and thus modulating cardiac excitation-contraction coupling which could be a potential mechanism of SGLT2 inhibitors in cardiovascular protection and heart failure[34]; (5) SGLT2 inhibition induce volume contraction which is accompanied by an increase in circulating renin-angiotensin-aldosterone system (RAAS) mediators even though this effect do not raise the blood pressure during treatment with SGLT2 inhibitors[35]. Combined use of RAAS and SGLT2 inhibitors may lead to synergistic beneficial cardiovascular effects. Although most of the patients in CVOTs and DAPA HF had already been taking ACE inhibitors or ARBs, this combined treatment strategy needs further investigation[36]. Furthermore, SGLT2 inhibitor treatment is associated with afferent vasoconstriction rather than efferent vasodilatation associated with RAAS inhibitors which attenuate renal hyperfiltration and contribute to renal protection in diabetes[35]; (6) Renoprotection of SGLT2 inhibitors could play a role in the observed cardiac benefits since the heart and kidney are inextricably linked (cardiorenal syndrome) and renal disease adversely impacts heart failure outcomes[16]. Recently, the CREDENCE trial (Canagliflozin and Renal Events in Diabetes with Established Nephropathy Clinical Evaluation) was prematurely stopped because of the achievement of the prespecified criteria for the primary composite endpoint (time to first occurrence of end-stage kidney disease, cardiovascular/renal death, doubling of serum creatinine) when investigating canagliflozin versus placebo. The trial also confirmed significant reductions in secondary endpoints of cardiovascular death or hospitalization for heart failure[24]. These results emphasize that cardiovascular benefit induced by SGLT2 inhibitors and renal protection may be connected. Sano proposed that SGLT2 inhibitors rest the exhausted kidney proximal tubular epithelial cells and restore functional and structural manifestation of diabetic kidney disease[37,38]; (7) Increased cardiac efficiency may be linked to increased oxygen delivery due to hemoconcentration and raised erythropoietin associated with SGLT2 inhibition[23,39]. On the other hand, in the study with erythropoietin-mimetic agents in patients with heart failure of Swedberg et al[40] the correction of anemia did not reduce the rate of death or hospitalization among patients with systolic heart failure and there was even a significant increase in the thromboembolic risk. This increase in hematocrit value during SGLT2 inhibition could be alternatively explained as being a surrogate marker of renal recovery from tubulointerstitial injury[37]. Nevertheless, the issue needs to be further clarified; (8) Increased heart rate was not observed during SGLT2 inhibitor treatment even though they affect blood pressure and induce volume contraction. It seems that the diuretic effects of SGLT2 inhibitors do not activate neurohumoral factors which is beneficial in heart failure[37]. Maybe the pharmacological implications of SGLT expression found in the brain could be manifested through this mechanism[41,42]; (9) Raised glucagon levels have been linked to SGLT2 inhibitor therapy and, considering glucagon inotropic effect independent of the catecholamine release it induces, this could lead to a better cardiac performance[25,43,44]. Glucagon inotropic effect declines with the failing heart which means that it could contribute to the maintaining of the heart function when heart failure is in its commencing stage. It has also anti-arrhythmogenic property which may be linked to the reduction of sudden death[45]. Moreover, glucagon is known for hepatic glucose production that could contribute to low risk of hypoglycemia with SGLT2 inhibition and it enhances ketogenesis, so the consequences of glucagon effects could account for SGLT2 inhibitors’ benefits even in non-diabetic patients[9,46,47]. On the other hand, since this hormone has been traditionally considered harmful in diabetes, its activity regarding SGLT2 inhibition therapy needs to be further clarified; (10) SGLT2 inhibitors can redirect metabolism from glucose to fatty acid oxidation. This augments the synthesis of ketones which release energy more efficiently than glucose or fatty acids and can be used as alternate fuel source in the failing heart. These findings could contribute to increased heart function observed with SGLT2 inhibitors even in non-diabetic patients but they need further investigation[47-51]. Ketone bodies participate in epigenetic and cellular signaling and have antioxidative and anti-inflammatory properties. Oxidative stress and inflammation are key contributors to the development of diabetic cardiomyopathy but also play a role in the pathophysiology of heart failure irrespective of diabetes[52-57]; (11) From experimental animal models it is known that SGLT2 inhibitors exert systemic and cardiac anti-inflammatory effects[9]. For example, inflammatory M1 macrophages preferentially utilize glucose, so SGLT2 inhibitors could dampen inflammatory processes decreasing glucose flux and thus promoting polarization of macrophage phenotype to non-inflammatory[23]. Treatment with SGLT2 inhibitors also showed reduction in pro-inflammatory cytokines profile such as TNFα and IL-6[9]. As it was stated before, inflammation is one of the mechanisms involved in diabetic cardiomyopathy pathogenesis but also plays a role in the failing heart irrespective of diabetes. Furthermore, heart failure and inflammation are strongly connected and mutually enhance each other creating a vicious circle[58]. No doubt that SGLT2 inhibitors’ anti-inflammatory capacities could be beneficial in the failing heart, but more studies in humans are needed; (12) SGLT2 inhibition is associated to antifibrotic effects in animal models. According to the study of Lin et al[59] empagliflozin significantly ameliorated pericoronary arterial fibrosis, cardiac interstitial fibrosis, coronary arterial thickening, cardiac interstitial macrophage infiltration and cardiac superoxide levels in db/db mice. The authors also stated that the observations might be attributable to the attenuation of oxidative stress. Recently, in a randomized trial with empagliflozin (EMPA HEART CardioLink-6 trial) it has been shown that empagliflozin caused a reduction in left ventricular mass index assessed by cardiac magnetic resonance imaging over a 6-month period in patients with type 2 diabetes mellitus and coronary disease[60]. The issue of antifibrotic effects needs further investigation in humans since it could be of great importance in heart failure and cardiac reverse remodeling; (13) Antioxidative features are attributable to SGLT2 inhibitors as it was shown in animal experiments[9]. Oxidative stress plays an important role in the pathogenesis of cardiac remodeling, and substantial evidence indicate that oxidative stress is increased both in the myocardium and systemically in patients with heart failure[56]; (14) By current evidence from experimental animal models SGLT2 inhibitors attenuate apoptosis of myocardial cells in models of myocardial ischaemia-reperfusion injury and diabetic cardiomyopathy which could be very important since apoptosis is likely to play an important role in heart failure[9,61]. Nevertheless, further clarification is required; (15) SGLT2 inhibitors could reestablish the balance between pro- and anti-inflammatory adipokines that can influence atherosclerosis, insulin resistance, inflammation, coagulation and fibrinolysis[15,62]. Additionally, perivascular and epicardial fat, through altered paracrine regulation of adipokines, is implicated in pathogenesis of heart failure[63]. According to the study of Sato et al[64] dapagliflozin might reduce epicardial adipose tissue volume and in this way could contribute to heart failure reduction risk while canagliflozin, in comparison with glimepiride, reduces serum leptin levels and increases the levels of the anti-inflammatory adipokine adiponectin[65]; (16) SGLT2 inhibitors could exert direct cardiac effect through sodium-hydrogen exchange inhibition. This may lead to a reduction in cardiac remodeling, injury, hypertrophy, fibrosis, and systolic dysfunction, as well as reduce cytoplasmic sodium and calcium levels, while increasing mitochondrial calcium levels[66,67]. Since heart failure is associated with intracellular cardiomyocyte sodium and calcium loading, this could affect the origin of heart failure[68,69]; (17) SGLT2 inihibitors could modulate electrophysiology in the heart. Besides the already mentioned glucagon anti-arrhythmogenic effect, one retrospective study showed that treatment with SGLT2 inhibitors reverses ventricular repolarization heterogeneity in people with type 2 diabetes, independently of their effect on glycemic control[70]. The findings may be linked to the reduction of fatal arrhythmias and thus reduced cardiovascular death seen with the SGLT2 inhibition so more studies on mechanisms of arrhythmias and SGLT2 inhibition are encouraged; and (18) The effects of SGLT2 inhibitors on plasma biomarker N-terminal pro-brain natriuretic peptide (NT-proBNP) have been inconsistent in studies on humans and in experimental studies[39,71-73]. To better elucidate SGLT2 inhibitors’ action, it would be appropriate to determine their effects on NT-proBNP and other natriuretic peptides in patients with developed heart failure as well as in asymptomatic individuals. There are interesting findings of Majowicz et al[74] with the atrial natriuretic peptide (ANP) and endothelin-3. In their study, it has been shown that these vasoactive agents inhibit SGLT2 activity in the kidney. If SGLT2 transporters would be inhibited via SGLT2 inhibitors, ANP could exert and enhance other functions besides its natriuretic and diuretic actions, for example inhibition of RAAS and aldosterone production, protection against angiotensin II induced cardiac remodeling by minimizing macrophage infiltration and expression of pro-inflammatory factors, and modulation of arterial and cardiac baroreflex mechanism, e.g., blunting sympathetic response. This could also give synergic effect with neprilysin inhibitors. The hypothesis still needs to be tested but theoretically it could partially contribute to SGLT2 inhibitors’ cardioprotection, in asymptomatic left ventricle dysfunction and especially in the failing heart where the natriuretic peptides are significantly elevated[75,76].
In conclusion, based on current evidence, SGLT2 inhibitors are agents with pleiotropic effects that are valuable in treating diabetes and preventing its complications. They reduce the burden of cardiovascular adverse events especially through decreasing heart failure risk. In addition, these drugs represent a new add-on strategy in the treatment of normoglycemic patients with HFrEF and carry the potential to be useful even in patients with HFpEF, but the dedicated studies are still ongoing. The benefits seen on heart failure appear to be mediated via glucose-independent mechanisms. Translational clues to the heart failure benefits recorded in clinical trials so far, should be sought in mechanisms of their action, which are not completely explained and are yet to be revealed. Particularly missing are human studies designed with enough power to elucidate some potential mechanisms essential for their mode of action. These data are important since SGLT2 inhibitors have great clinical potential through wide indications across the spectrum of heart failure and could lessen polypragmasy since they can target various mechanisms underpinning heart failure pathogenesis. The most logical explanation of their benefits is the timely targeting of various mechanisms implicated in the evolution of heart failure.
Manuscript source: Invited manuscript
Specialty type: Endocrinology and metabolism
Country/Territory of origin: Croatia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Petretta M S-Editor: Wang J L-Editor: A E-Editor: Ma YJ
| 1. | American Diabetes Association. 10. Cardiovascular Disease and Risk Management: Standards of Medical Care in Diabetes-2020. Diabetes Care. 2020;43:S111-S134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 324] [Cited by in RCA: 378] [Article Influence: 75.6] [Reference Citation Analysis (0)] |
| 2. | Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, Mattheus M, Devins T, Johansen OE, Woerle HJ, Broedl UC, Inzucchi SE; EMPA-REG OUTCOME Investigators. Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes. N Engl J Med. 2015;373:2117-2128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7124] [Cited by in RCA: 8248] [Article Influence: 824.8] [Reference Citation Analysis (1)] |
| 3. | Neal B, Perkovic V, Mahaffey KW, de Zeeuw D, Fulcher G, Erondu N, Shaw W, Law G, Desai M, Matthews DR; CANVAS Program Collaborative Group. Canagliflozin and Cardiovascular and Renal Events in Type 2 Diabetes. N Engl J Med. 2017;377:644-657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4498] [Cited by in RCA: 5372] [Article Influence: 671.5] [Reference Citation Analysis (0)] |
| 4. | Wiviott SD, Raz I, Bonaca MP, Mosenzon O, Kato ET, Cahn A, Silverman MG, Zelniker TA, Kuder JF, Murphy SA, Bhatt DL, Leiter LA, McGuire DK, Wilding JPH, Ruff CT, Gause-Nilsson IAM, Fredriksson M, Johansson PA, Langkilde AM, Sabatine MS; DECLARE–TIMI 58 Investigators. Dapagliflozin and Cardiovascular Outcomes in Type 2 Diabetes. N Engl J Med. 2019;380:347-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4652] [Cited by in RCA: 4225] [Article Influence: 704.2] [Reference Citation Analysis (0)] |
| 5. | Giugliano D, Meier JJ, Esposito K. Heart failure and type 2 diabetes: From cardiovascular outcome trials, with hope. Diabetes Obes Metab. 2019;21:1081-1087. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 37] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 6. | McMurray JJV, Solomon SD, Inzucchi SE, Køber L, Kosiborod MN, Martinez FA, Ponikowski P, Sabatine MS, Anand IS, Bělohlávek J, Böhm M, Chiang CE, Chopra VK, de Boer RA, Desai AS, Diez M, Drozdz J, Dukát A, Ge J, Howlett JG, Katova T, Kitakaze M, Ljungman CEA, Merkely B, Nicolau JC, O'Meara E, Petrie MC, Vinh PN, Schou M, Tereshchenko S, Verma S, Held C, DeMets DL, Docherty KF, Jhund PS, Bengtsson O, Sjöstrand M, Langkilde AM; DAPA-HF Trial Committees and Investigators. Dapagliflozin in Patients with Heart Failure and Reduced Ejection Fraction. N Engl J Med. 2019;381:1995-2008. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2953] [Cited by in RCA: 4399] [Article Influence: 733.2] [Reference Citation Analysis (0)] |
| 7. | Zelniker TA, Wiviott SD, Raz I, Im K, Goodrich EL, Bonaca MP, Mosenzon O, Kato ET, Cahn A, Furtado RHM, Bhatt DL, Leiter LA, McGuire DK, Wilding JPH, Sabatine MS. SGLT2 inhibitors for primary and secondary prevention of cardiovascular and renal outcomes in type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Lancet. 2019;393:31-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1634] [Cited by in RCA: 1909] [Article Influence: 318.2] [Reference Citation Analysis (0)] |
| 8. | Figtree GA, Rådholm K, Barrett TD, Perkovic V, Mahaffey KW, de Zeeuw D, Fulcher G, Matthews DR, Shaw W, Neal B. Effects of Canagliflozin on Heart Failure Outcomes Associated With Preserved and Reduced Ejection Fraction in Type 2 Diabetes Mellitus. Circulation. 2019;139:2591-2593. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 120] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 9. | Lahnwong S, Chattipakorn SC, Chattipakorn N. Potential mechanisms responsible for cardioprotective effects of sodium-glucose co-transporter 2 inhibitors. Cardiovasc Diabetol. 2018;17:101. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 111] [Cited by in RCA: 125] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 10. | Abdul-Ghani MA, Norton L, DeFronzo RA. Renal sodium-glucose cotransporter inhibition in the management of type 2 diabetes mellitus. Am J Physiol Renal Physiol. 2015;309:F889-F900. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 115] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 11. | Rahmoune H, Thompson PW, Ward JM, Smith CD, Hong G, Brown J. Glucose transporters in human renal proximal tubular cells isolated from the urine of patients with non-insulin-dependent diabetes. Diabetes. 2005;54:3427-3434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 561] [Cited by in RCA: 597] [Article Influence: 29.9] [Reference Citation Analysis (0)] |
| 12. | Heerspink HJ, Perkins BA, Fitchett DH, Husain M, Cherney DZ. Sodium Glucose Cotransporter 2 Inhibitors in the Treatment of Diabetes Mellitus: Cardiovascular and Kidney Effects, Potential Mechanisms, and Clinical Applications. Circulation. 2016;134:752-772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 700] [Cited by in RCA: 957] [Article Influence: 106.3] [Reference Citation Analysis (0)] |
| 13. | Tamargo J. Sodium-glucose Cotransporter 2 Inhibitors in Heart Failure: Potential Mechanisms of Action, Adverse Effects and Future Developments. Eur Cardiol. 2019;14:23-32. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 40] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 14. | Donnan JR, Grandy CA, Chibrikov E, Marra CA, Aubrey-Bassler K, Johnston K, Swab M, Hache J, Curnew D, Nguyen H, Gamble JM. Comparative safety of the sodium glucose co-transporter 2 (SGLT2) inhibitors: a systematic review and meta-analysis. BMJ Open. 2019;9:e022577. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 124] [Cited by in RCA: 149] [Article Influence: 24.8] [Reference Citation Analysis (0)] |
| 15. | Verma S, McMurray JJV. SGLT2 inhibitors and mechanisms of cardiovascular benefit: a state-of-the-art review. Diabetologia. 2018;61:2108-2117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 513] [Cited by in RCA: 662] [Article Influence: 94.6] [Reference Citation Analysis (0)] |
| 16. | Lam CSP, Chandramouli C, Ahooja V, Verma S. SGLT-2 Inhibitors in Heart Failure: Current Management, Unmet Needs, and Therapeutic Prospects. J Am Heart Assoc. 2019;8:e013389. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 116] [Cited by in RCA: 122] [Article Influence: 20.3] [Reference Citation Analysis (0)] |
| 17. | Kato ET, Silverman MG, Mosenzon O, Zelniker TA, Cahn A, Furtado RHM, Kuder J, Murphy SA, Bhatt DL, Leiter LA, McGuire DK, Wilding JPH, Bonaca MP, Ruff CT, Desai AS, Goto S, Johansson PA, Gause-Nilsson I, Johanson P, Langkilde AM, Raz I, Sabatine MS, Wiviott SD. Effect of Dapagliflozin on Heart Failure and Mortality in Type 2 Diabetes Mellitus. Circulation. 2019;139:2528-2536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 322] [Cited by in RCA: 398] [Article Influence: 66.3] [Reference Citation Analysis (0)] |
| 18. | Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, Falk V, González-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GM, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P; Authors/Task Force Members; Document Reviewers. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2016;18:891-975. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4368] [Cited by in RCA: 4910] [Article Influence: 545.6] [Reference Citation Analysis (4)] |
| 19. | Shah KS, Xu H, Matsouaka RA, Bhatt DL, Heidenreich PA, Hernandez AF, Devore AD, Yancy CW, Fonarow GC. Heart Failure With Preserved, Borderline, and Reduced Ejection Fraction: 5-Year Outcomes. J Am Coll Cardiol. 2017;70:2476-2486. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 445] [Cited by in RCA: 753] [Article Influence: 94.1] [Reference Citation Analysis (1)] |
| 20. | Huynh K, Bernardo BC, McMullen JR, Ritchie RH. Diabetic cardiomyopathy: mechanisms and new treatment strategies targeting antioxidant signaling pathways. Pharmacol Ther. 2014;142:375-415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 353] [Cited by in RCA: 435] [Article Influence: 39.5] [Reference Citation Analysis (0)] |
| 21. | Levelt E, Gulsin G, Neubauer S, McCann GP. MECHANISMS IN ENDOCRINOLOGY: Diabetic cardiomyopathy: pathophysiology and potential metabolic interventions state of the art review. Eur J Endocrinol. 2018;178:R127-R139. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 54] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 22. | Verma S, McMurray JJV, Cherney DZI. The Metabolodiuretic Promise of Sodium-Dependent Glucose Cotransporter 2 Inhibition: The Search for the Sweet Spot in Heart Failure. JAMA Cardiol. 2017;2:939-940. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 125] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 23. | Staels B. Cardiovascular Protection by Sodium Glucose Cotransporter 2 Inhibitors: Potential Mechanisms. Am J Med. 2017;130:S30-S39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 56] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 24. | Packer M. Lessons learned from the DAPA-HF trial concerning the mechanisms of benefit of SGLT2 inhibitors on heart failure events in the context of other large-scale trials nearing completion. Cardiovasc Diabetol. 2019;18:129. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 46] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 25. | Ferrannini E, Muscelli E, Frascerra S, Baldi S, Mari A, Heise T, Broedl UC, Woerle HJ. Metabolic response to sodium-glucose cotransporter 2 inhibition in type 2 diabetic patients. J Clin Invest. 2014;124:499-508. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 714] [Cited by in RCA: 873] [Article Influence: 79.4] [Reference Citation Analysis (0)] |
| 26. | Bolinder J, Ljunggren Ö, Johansson L, Wilding J, Langkilde AM, Sjöström CD, Sugg J, Parikh S. Dapagliflozin maintains glycaemic control while reducing weight and body fat mass over 2 years in patients with type 2 diabetes mellitus inadequately controlled on metformin. Diabetes Obes Metab. 2014;16:159-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 324] [Cited by in RCA: 356] [Article Influence: 32.4] [Reference Citation Analysis (0)] |
| 27. | DeFronzo RA. The EMPA-REG study: What has it told us? A diabetologist's perspective. J Diabetes Complications. 2016;30:1-2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 32] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 28. | Packer M. Reconceptualization of the Molecular Mechanism by Which Sodium-Glucose Cotransporter 2 Inhibitors Reduce the Risk of Heart Failure Events. Circulation. 2019;140:443-445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 48] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 29. | Abdul-Ghani M, Del Prato S, Chilton R, DeFronzo RA. SGLT2 Inhibitors and Cardiovascular Risk: Lessons Learned From the EMPA-REG OUTCOME Study. Diabetes Care. 2016;39:717-725. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 230] [Cited by in RCA: 232] [Article Influence: 25.8] [Reference Citation Analysis (0)] |
| 30. | List JF, Whaley JM. Glucose dynamics and mechanistic implications of SGLT2 inhibitors in animals and humans. Kidney Int Suppl. 2011;S20-S27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 133] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 31. | Ptaszynska A, Hardy E, Johnsson E, Parikh S, List J. Effects of dapagliflozin on cardiovascular risk factors. Postgrad Med. 2013;125:181-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 76] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 32. | Kittleson MM, St John ME, Bead V, Champion HC, Kasper EK, Russell SD, Wittstein IS, Hare JM. Increased levels of uric acid predict haemodynamic compromise in patients with heart failure independently of B-type natriuretic peptide levels. Heart. 2007;93:365-367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 36] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 33. | Feig DI, Kang DH, Johnson RJ. Uric acid and cardiovascular risk. N Engl J Med. 2008;359:1811-1821. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1874] [Cited by in RCA: 1858] [Article Influence: 109.3] [Reference Citation Analysis (0)] |
| 34. | Hare JM, Johnson RJ. Uric acid predicts clinical outcomes in heart failure: insights regarding the role of xanthine oxidase and uric acid in disease pathophysiology. Circulation. 2003;107:1951-1953. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 125] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 35. | Cherney DZ, Perkins BA, Soleymanlou N, Maione M, Lai V, Lee A, Fagan NM, Woerle HJ, Johansen OE, Broedl UC, von Eynatten M. Renal hemodynamic effect of sodium-glucose cotransporter 2 inhibition in patients with type 1 diabetes mellitus. Circulation. 2014;129:587-597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 847] [Cited by in RCA: 977] [Article Influence: 81.4] [Reference Citation Analysis (0)] |
| 36. | Lo KB, Gul F, Ram P, Kluger AY, Tecson KM, McCullough PA, Rangaswami J. The Effects of SGLT2 Inhibitors on Cardiovascular and Renal Outcomes in Diabetic Patients: A Systematic Review and Meta-Analysis. Cardiorenal Med. 2020;10:1-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 76] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 37. | Sano M. A new class of drugs for heart failure: SGLT2 inhibitors reduce sympathetic overactivity. J Cardiol. 2018;71:471-476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 131] [Article Influence: 18.7] [Reference Citation Analysis (0)] |
| 38. | Perkovic V, Jardine MJ, Neal B, Bompoint S, Heerspink HJL, Charytan DM, Edwards R, Agarwal R, Bakris G, Bull S, Cannon CP, Capuano G, Chu PL, de Zeeuw D, Greene T, Levin A, Pollock C, Wheeler DC, Yavin Y, Zhang H, Zinman B, Meininger G, Brenner BM, Mahaffey KW; CREDENCE Trial Investigators. Canagliflozin and Renal Outcomes in Type 2 Diabetes and Nephropathy. N Engl J Med. 2019;380:2295-2306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2826] [Cited by in RCA: 3950] [Article Influence: 658.3] [Reference Citation Analysis (0)] |
| 39. | Lambers Heerspink HJ, de Zeeuw D, Wie L, Leslie B, List J. Dapagliflozin a glucose-regulating drug with diuretic properties in subjects with type 2 diabetes. Diabetes Obes Metab. 2013;15:853-862. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 540] [Cited by in RCA: 651] [Article Influence: 54.3] [Reference Citation Analysis (0)] |
| 40. | Swedberg K, Young JB, Anand IS, Cheng S, Desai AS, Diaz R, Maggioni AP, McMurray JJ, O'Connor C, Pfeffer MA, Solomon SD, Sun Y, Tendera M, van Veldhuisen DJ; RED-HF Committees; RED-HF Investigators. Treatment of anemia with darbepoetin alfa in systolic heart failure. N Engl J Med. 2013;368:1210-1219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 376] [Cited by in RCA: 464] [Article Influence: 38.7] [Reference Citation Analysis (0)] |
| 41. | Yu AS, Hirayama BA, Timbol G, Liu J, Diez-Sampedro A, Kepe V, Satyamurthy N, Huang SC, Wright EM, Barrio JR. Regional distribution of SGLT activity in rat brain in vivo. Am J Physiol Cell Physiol. 2013;304:C240-C247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 94] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 42. | Poppe R, Karbach U, Gambaryan S, Wiesinger H, Lutzenburg M, Kraemer M, Witte OW, Koepsell H. Expression of the Na+-D-glucose cotransporter SGLT1 in neurons. J Neurochem. 1997;69:84-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 105] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 43. | Jones BJ, Tan T, Bloom SR. Minireview: Glucagon in stress and energy homeostasis. Endocrinology. 2012;153:1049-1054. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 92] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 44. | Regan TJ, Lehan PH, Henneman DH, Behar A, Hellems HK. Myocardial metabolic and contractile response to glucagon and epinephrine. J Lab Clin Med. 1964;63:638-647. [PubMed] |
| 45. | Ceriello A, Genovese S, Mannucci E, Gronda E. Glucagon and heart in type 2 diabetes: new perspectives. Cardiovasc Diabetol. 2016;15:123. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 59] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 46. | Schade DS, Eaton RP. Glucagon regulation of plasma ketone body concentration in human diabetes. J Clin Invest. 1975;56:1340-1344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 37] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 47. | Ferrannini E, Baldi S, Frascerra S, Astiarraga B, Heise T, Bizzotto R, Mari A, Pieber TR, Muscelli E. Shift to Fatty Substrate Utilization in Response to Sodium-Glucose Cotransporter 2 Inhibition in Subjects Without Diabetes and Patients With Type 2 Diabetes. Diabetes. 2016;65:1190-1195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 406] [Cited by in RCA: 532] [Article Influence: 59.1] [Reference Citation Analysis (0)] |
| 48. | Mudaliar S, Alloju S, Henry RR. Can a Shift in Fuel Energetics Explain the Beneficial Cardiorenal Outcomes in the EMPA-REG OUTCOME Study? A Unifying Hypothesis. Diabetes Care. 2016;39:1115-1122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 411] [Cited by in RCA: 455] [Article Influence: 50.6] [Reference Citation Analysis (0)] |
| 49. | Daniele G, Xiong J, Solis-Herrera C, Merovci A, Eldor R, Tripathy D, DeFronzo RA, Norton L, Abdul-Ghani M. Dapagliflozin Enhances Fat Oxidation and Ketone Production in Patients With Type 2 Diabetes. Diabetes Care. 2016;39:2036-2041. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 169] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 50. | Kutoh E, Hayashi J. Effect of Canagliflozin on Heart Function Involving Ketone Bodies in Patients with Type 2 Diabetes. Drug Res (Stuttg). 2019;69:297-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 51. | Bedi KC, Snyder NW, Brandimarto J, Aziz M, Mesaros C, Worth AJ, Wang LL, Javaheri A, Blair IA, Margulies KB, Rame JE. Evidence for Intramyocardial Disruption of Lipid Metabolism and Increased Myocardial Ketone Utilization in Advanced Human Heart Failure. Circulation. 2016;133:706-716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 322] [Cited by in RCA: 495] [Article Influence: 55.0] [Reference Citation Analysis (0)] |
| 52. | Prattichizzo F, De Nigris V, Micheloni S, La Sala L, Ceriello A. Increases in circulating levels of ketone bodies and cardiovascular protection with SGLT2 inhibitors: Is low-grade inflammation the neglected component? Diabetes Obes Metab. 2018;20:2515-2522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 92] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 53. | Haces ML, Hernández-Fonseca K, Medina-Campos ON, Montiel T, Pedraza-Chaverri J, Massieu L. Antioxidant capacity contributes to protection of ketone bodies against oxidative damage induced during hypoglycemic conditions. Exp Neurol. 2008;211:85-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 138] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 54. | Newman JC, Verdin E. β-hydroxybutyrate: much more than a metabolite. Diabetes Res Clin Pract. 2014;106:173-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 201] [Cited by in RCA: 236] [Article Influence: 21.5] [Reference Citation Analysis (0)] |
| 55. | Newman JC, Verdin E. Ketone bodies as signaling metabolites. Trends Endocrinol Metab. 2014;25:42-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 582] [Cited by in RCA: 705] [Article Influence: 64.1] [Reference Citation Analysis (0)] |
| 56. | Burgoyne JR, Mongue-Din H, Eaton P, Shah AM. Redox signaling in cardiac physiology and pathology. Circ Res. 2012;111:1091-1106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 337] [Cited by in RCA: 369] [Article Influence: 28.4] [Reference Citation Analysis (0)] |
| 57. | Riehle C, Bauersachs J. Key inflammatory mechanisms underlying heart failure. Herz. 2019;44:96-106. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 88] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 58. | Van Linthout S, Tschöpe C. Inflammation - Cause or Consequence of Heart Failure or Both? Curr Heart Fail Rep. 2017;14:251-265. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 311] [Cited by in RCA: 321] [Article Influence: 40.1] [Reference Citation Analysis (0)] |
| 59. | Lin B, Koibuchi N, Hasegawa Y, Sueta D, Toyama K, Uekawa K, Ma M, Nakagawa T, Kusaka H, Kim-Mitsuyama S. Glycemic control with empagliflozin, a novel selective SGLT2 inhibitor, ameliorates cardiovascular injury and cognitive dysfunction in obese and type 2 diabetic mice. Cardiovasc Diabetol. 2014;13:148. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 220] [Cited by in RCA: 312] [Article Influence: 28.4] [Reference Citation Analysis (0)] |
| 60. | Verma S, Mazer CD, Yan AT, Mason T, Garg V, Teoh H, Zuo F, Quan A, Farkouh ME, Fitchett DH, Goodman SG, Goldenberg RM, Al-Omran M, Gilbert RE, Bhatt DL, Leiter LA, Jüni P, Zinman B, Connelly KA. Effect of Empagliflozin on Left Ventricular Mass in Patients With Type 2 Diabetes Mellitus and Coronary Artery Disease: The EMPA-HEART CardioLink-6 Randomized Clinical Trial. Circulation. 2019;140:1693-1702. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 256] [Cited by in RCA: 394] [Article Influence: 65.7] [Reference Citation Analysis (0)] |
| 61. | Abbate A, Narula J. Role of apoptosis in adverse ventricular remodeling. Heart Fail Clin. 2012;8:79-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 37] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 62. | Lau DC, Dhillon B, Yan H, Szmitko PE, Verma S. Adipokines: molecular links between obesity and atheroslcerosis. Am J Physiol Heart Circ Physiol. 2005;288:H2031-H2041. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 587] [Cited by in RCA: 577] [Article Influence: 28.9] [Reference Citation Analysis (0)] |
| 63. | Patel VB, Shah S, Verma S, Oudit GY. Epicardial adipose tissue as a metabolic transducer: role in heart failure and coronary artery disease. Heart Fail Rev. 2017;22:889-902. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 159] [Article Influence: 22.7] [Reference Citation Analysis (0)] |
| 64. | Sato T, Aizawa Y, Yuasa S, Kishi S, Fuse K, Fujita S, Ikeda Y, Kitazawa H, Takahashi M, Sato M, Okabe M. The effect of dapagliflozin treatment on epicardial adipose tissue volume. Cardiovasc Diabetol. 2018;17:6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 160] [Cited by in RCA: 260] [Article Influence: 37.1] [Reference Citation Analysis (0)] |
| 65. | Garvey WT, Van Gaal L, Leiter LA, Vijapurkar U, List J, Cuddihy R, Ren J, Davies MJ. Effects of canagliflozin versus glimepiride on adipokines and inflammatory biomarkers in type 2 diabetes. Metabolism. 2018;85:32-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 188] [Article Influence: 26.9] [Reference Citation Analysis (0)] |
| 66. | Packer M, Anker SD, Butler J, Filippatos G, Zannad F. Effects of Sodium-Glucose Cotransporter 2 Inhibitors for the Treatment of Patients With Heart Failure: Proposal of a Novel Mechanism of Action. JAMA Cardiol. 2017;2:1025-1029. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 233] [Cited by in RCA: 269] [Article Influence: 44.8] [Reference Citation Analysis (0)] |
| 67. | Baartscheer A, Schumacher CA, Wüst RC, Fiolet JW, Stienen GJ, Coronel R, Zuurbier CJ. Empagliflozin decreases myocardial cytoplasmic Na+ through inhibition of the cardiac Na+/H+ exchanger in rats and rabbits. Diabetologia. 2017;60:568-573. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 396] [Cited by in RCA: 488] [Article Influence: 61.0] [Reference Citation Analysis (0)] |
| 68. | Kohlhaas M, Liu T, Knopp A, Zeller T, Ong MF, Böhm M, O'Rourke B, Maack C. Elevated cytosolic Na+ increases mitochondrial formation of reactive oxygen species in failing cardiac myocytes. Circulation. 2010;121:1606-1613. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 276] [Cited by in RCA: 264] [Article Influence: 17.6] [Reference Citation Analysis (0)] |
| 69. | Baartscheer A, Schumacher CA, van Borren MM, Belterman CN, Coronel R, Fiolet JW. Increased Na+/H+-exchange activity is the cause of increased [Na+]i and underlies disturbed calcium handling in the rabbit pressure and volume overload heart failure model. Cardiovasc Res. 2003;57:1015-1024. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 149] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 70. | Sato T, Miki T, Ohnishi H, Yamashita T, Takada A, Yano T, Tanno M, Tsuchida A, Miura T. Effect of sodium-glucose co-transporter-2 inhibitors on impaired ventricular repolarization in people with Type 2 diabetes. Diabet Med. 2017;34:1367-1371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 71. | Tanaka H, Takano K, Iijima H, Kubo H, Maruyama N, Hashimoto T, Arakawa K, Togo M, Inagaki N, Kaku K. Factors Affecting Canagliflozin-Induced Transient Urine Volume Increase in Patients with Type 2 Diabetes Mellitus. Adv Ther. 2017;34:436-451. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 80] [Cited by in RCA: 110] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 72. | Eickhoff MK, Dekkers CCJ, Kramers BJ, Laverman GD, Frimodt-Møller M, Jørgensen NR, Faber J, Danser AHJ, Gansevoort RT, Rossing P, Persson F, Heerspink HJL. Effects of Dapagliflozin on Volume Status When Added to Renin-Angiotensin System Inhibitors. J Clin Med. 2019;8:779. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 64] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 73. | Januzzi JL, Butler J, Jarolim P, Sattar N, Vijapurkar U, Desai M, Davies MJ. Effects of Canagliflozin on Cardiovascular Biomarkers in Older Adults With Type 2 Diabetes. J Am Coll Cardiol. 2017;70:704-712. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 137] [Article Influence: 17.1] [Reference Citation Analysis (0)] |
| 74. | Majowicz MP, Gonzalez Bosc LV, Albertoni Borghese MF, Delgado MF, Ortiz MC, Sterin Speziale N, Vidal NA. Atrial natriuretic peptide and endothelin-3 target renal sodium-glucose cotransporter. Peptides. 2003;24:1971-1976. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 75. | Volpe M, Carnovali M, Mastromarino V. The natriuretic peptides system in the pathophysiology of heart failure: from molecular basis to treatment. Clin Sci (Lond). 2016;130:57-77. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 159] [Cited by in RCA: 210] [Article Influence: 23.3] [Reference Citation Analysis (0)] |
| 76. | Grubić Rotkvić P, Cigrovski Berković M, Bulj N, Rotkvić L. Minireview: are SGLT2 inhibitors heart savers in diabetes? Heart Fail Rev. 2019;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |