Copyright
©The Author(s) 2023.
World J Diabetes. May 15, 2023; 14(5): 549-559
Published online May 15, 2023. doi: 10.4239/wjd.v14.i5.549
Published online May 15, 2023. doi: 10.4239/wjd.v14.i5.549
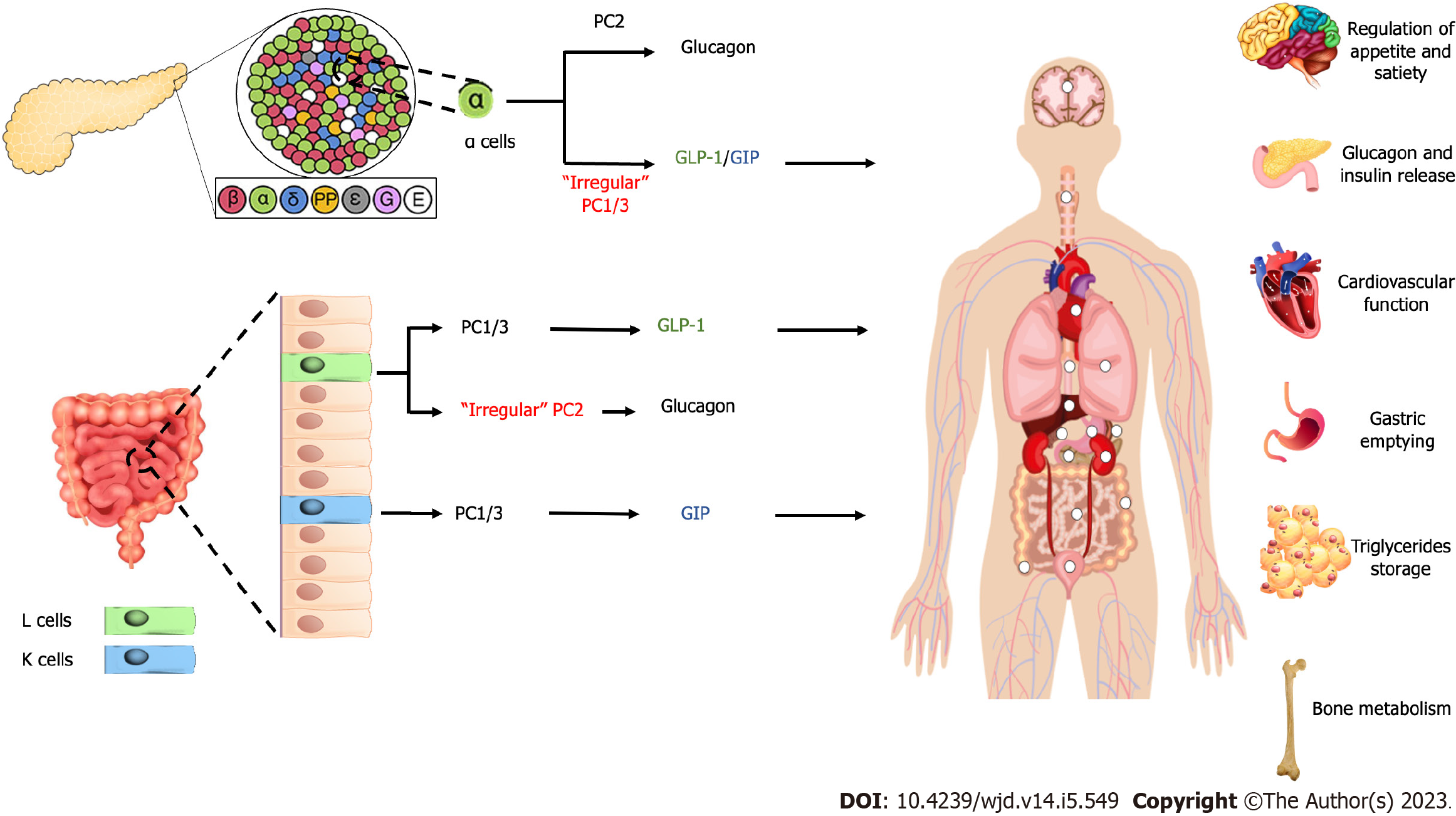
Figure 1 Production of incretin and its benefits.
Glucagon-like peptide-1 and glucose-dependent insulinotropic polypeptide produced in the pancreas and intestine mediated by prohormone convertase. The incretin hormones affect appetite and satiety, glucagon and insulin release, cardiovascular function, gastric emptying, triglycerides, and bone metabolism. GIP: Glucose-dependent insulinotropic polypeptide; GLP-1: Glucagon-like peptide-1; PC1/3: Prohormone convertase 1/3; PC2: Prohormone convertase 2.
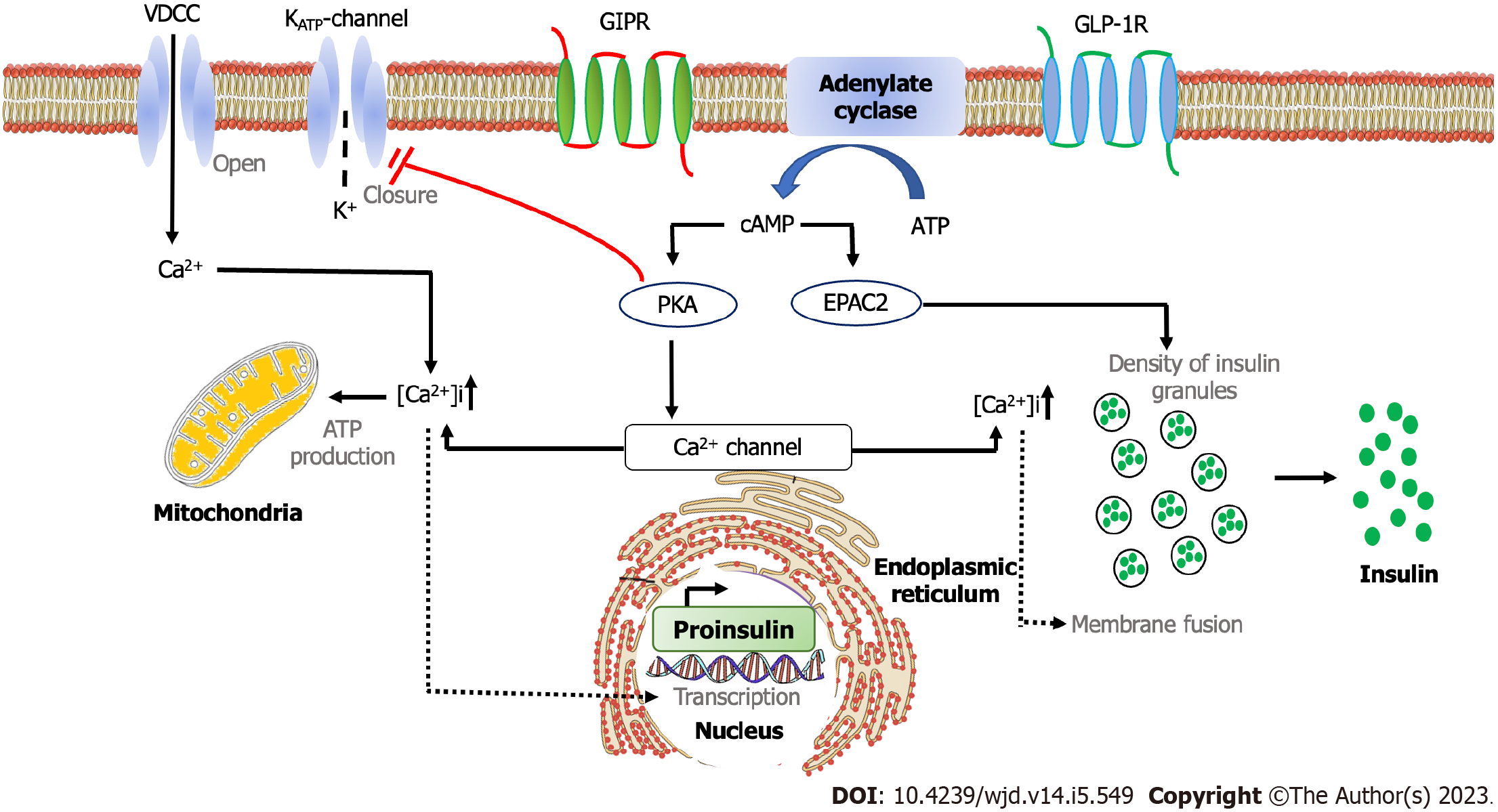
Figure 2 Intracellular mechanism of incretin hormones.
The binding of glucose-dependent insulinotropic polypeptide and glucagon-like peptide-1 with their respective receptors increase cyclic adenosine monophosphate and activation of protein kinase A. This result in the increase of Ca2+ levels, mediating the fusion of insulin-containing granules with the plasma membrane and insulin secretion from pancreatic β cells. ATP: Adenosine triphosphate; cAMP: Cyclic adenosine monophosphate; Ca2+: Calcium; [Ca2+]i: Calcium influx; EPAC2: Exchange protein activated by cAMP2; GIPR: Glucose-dependent insulinotropic polypeptide receptor; GLP-1R: Glucagon-like peptide-1 receptor; KATP-channel: ATP-sensitive potassium channel; K+: Kalium; PKA: Protein kinase A; VDCC: Voltage-gated calcium channels.
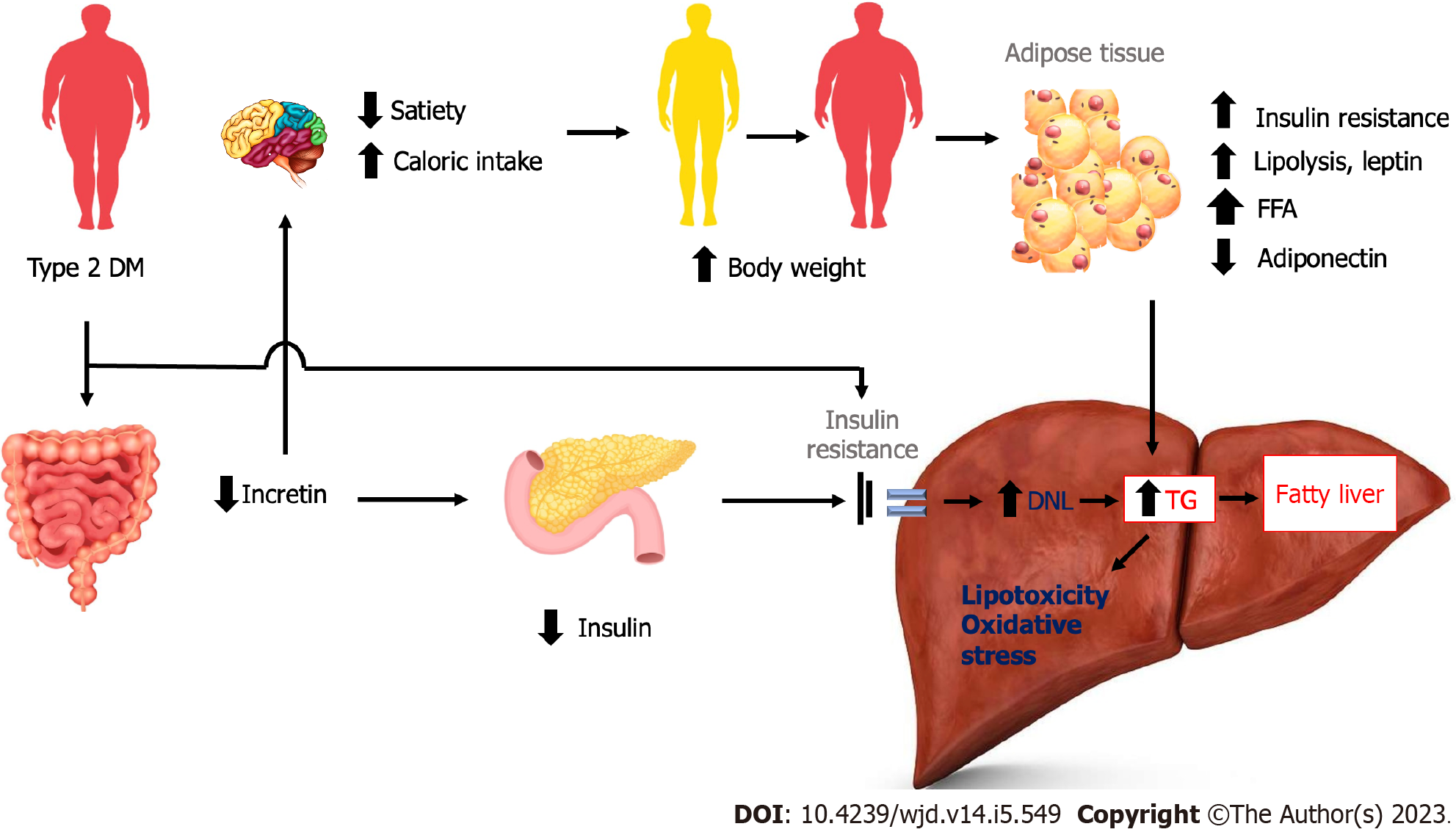
Figure 3 The effect of type 2 diabetes mellitus on incretin hormone and the development of non-alcoholic fatty liver disease.
Increased body weight as the result of reduced incretin effects leads to adipose tissue insulin resistance, increased lipolysis and leptin, and decreased adiponectin, resulting in hepatic fat deposition. DM: Diabetes Mellitus; DNL: De novo lipogenesis; FFA: Free fatty acids; TG: Triglycerides.
- Citation: Wibawa IDN, Mariadi IK, Somayana G, Krisnawardani Kumbara CIY, Sindhughosa DA. Diabetes and fatty liver: Involvement of incretin and its benefit for fatty liver management. World J Diabetes 2023; 14(5): 549-559
- URL: https://www.wjgnet.com/1948-9358/full/v14/i5/549.htm
- DOI: https://dx.doi.org/10.4239/wjd.v14.i5.549