Copyright
©The Author(s) 2023.
World J Diabetes. Dec 15, 2023; 14(12): 1784-1792
Published online Dec 15, 2023. doi: 10.4239/wjd.v14.i12.1784
Published online Dec 15, 2023. doi: 10.4239/wjd.v14.i12.1784
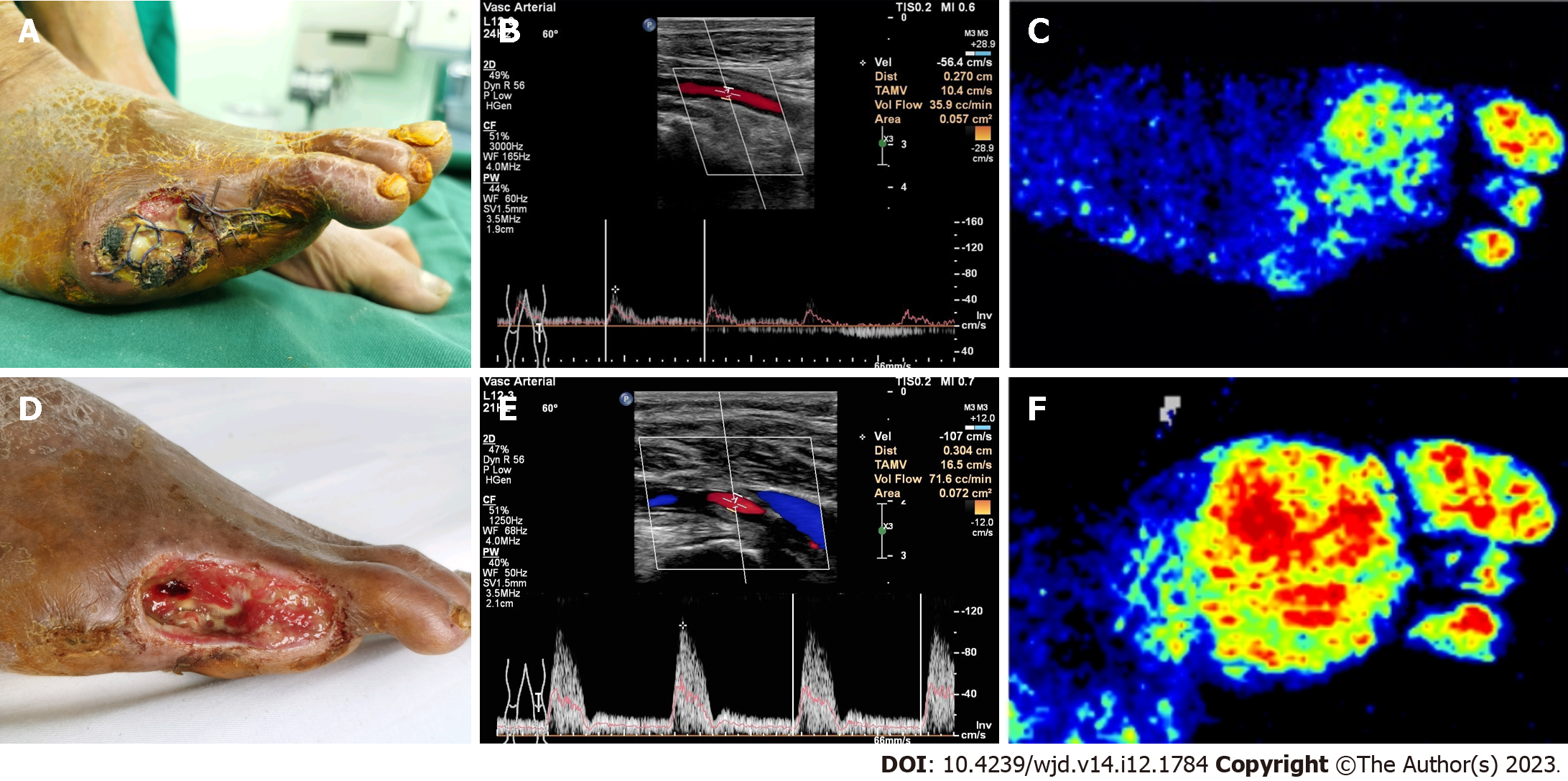
Figure 1 With left diabetic foot and Wagner grade 4 foot ulcers.
A: With left diabetic foot and Wagner grade 4 foot ulcers was amputated in a local hospital with non-healing chronic wounds and oozing; B and C: After referral to our department, the lower limb vascular score was 31 points and the popliteal artery (POA) was 36 cc/min (B) by preoperative B-ultrasound, with sparse plantar blood flow signals and poor microcirculation (C); D-F: One month after tibial transverse transport, the injured foot wound granulation was fresh and the wound was significantly reduced (D); B-ultrasound examination showed a significant increase in POA blood flow to 72 cc/min (E), abundant blood flow signals in plantar skin, and significant improvement in microcirculation (F).
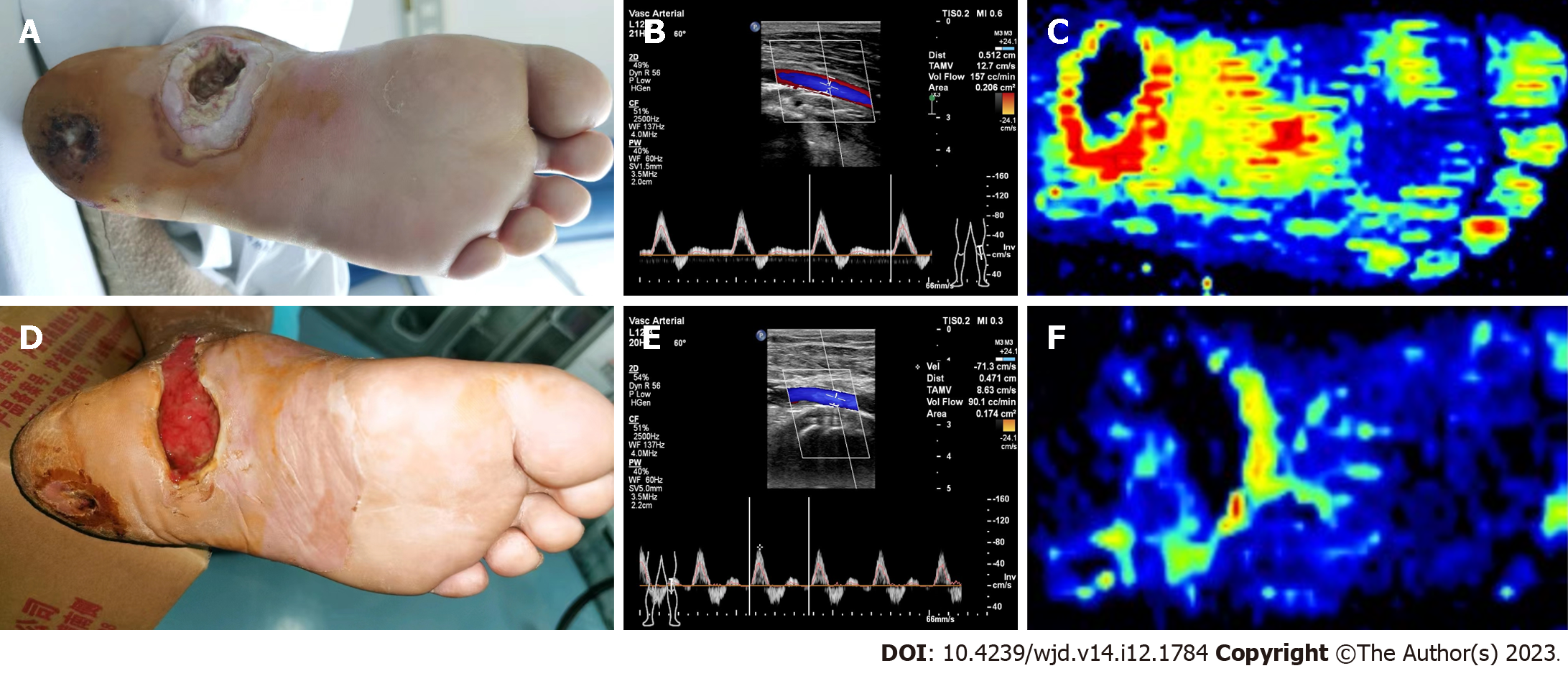
Figure 2 Right diabetic foot of Wagner grade 3.
A: Right diabetic foot of Wagner grade 3was treated by debridement and vacuum sealing drainage in the local hospital, with non-healing chronic wounds and oozing; B and C: After being referred to our department, the patient’s lower extremity vascular score was 19 points during the preoperative B-ultrasound examination, the popliteal artery (POA) blood flow was 157 cc/min (B), the plantar blood flow signals were abundant, and the microcirculation was good (C); D-F: One month after tibial transverse transport, the wounds of the affected feet were fresh with granulation, and the wounds were obviously reduced (D); the POA blood flow decreased to 90 cc/min (E) by B-ultrasound, the plantar skin blood flow signals reduced, and the microcirculation decreased obviously (F).
- Citation: Liao MM, Chen S, Cao JR, Wang MW, Jin ZH, Ye J, Ren YJ, Guo RQ. Early hemodynamics after tibial transverse transport in patients with nonarterial stenosis and arterial stenosis diabetic foot. World J Diabetes 2023; 14(12): 1784-1792
- URL: https://www.wjgnet.com/1948-9358/full/v14/i12/1784.htm
- DOI: https://dx.doi.org/10.4239/wjd.v14.i12.1784