Copyright
©The Author(s) 2022.
World J Diabetes. Oct 15, 2022; 13(10): 835-850
Published online Oct 15, 2022. doi: 10.4239/wjd.v13.i10.835
Published online Oct 15, 2022. doi: 10.4239/wjd.v13.i10.835
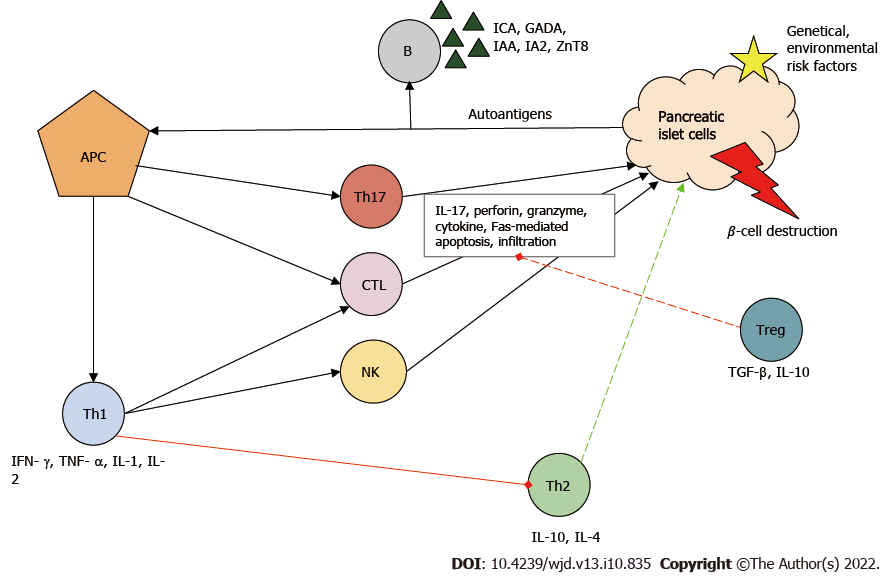
Figure 1 Immunopathogenesis of type 1 diabetes mellitus.
Autoantigens from pancreatic islet β-cells are presented by antigen-presenting cells (APCs), thereby activating T cells including helper T (Th) cells type 1 and type 17 and cytotoxic T lymphocytes (CTLs). Th type 1 cells play a key role in the development of the autoimmune response. They stimulate the activity of inflammatory T cells, macrophages and natural killer (NK) cells by producing proinflammatory cytokines and stimulate B cells (B), which produces autoantibodies and inhibits the protective Th type 2 cell function. Together, these immune cells contribute to the destruction of pancreatic β-cells. Red line: Inhibition; Green line: Stimulation. GADA: Glutamic-acid-decarboxylase antibody; IA2: Islet tyrosine phosphatase 2 antibody; IAA: Insulin autoantibody; ICA: Islet cell antibody; IL: Interleukin; IFN-γ: Interferon γ; TGF-β: Transforming growth factor β; TNF-α: Tumor necrosis factor α; Treg: Regulatory T cell; ZnT8: Zinc transporter 8 antibody.
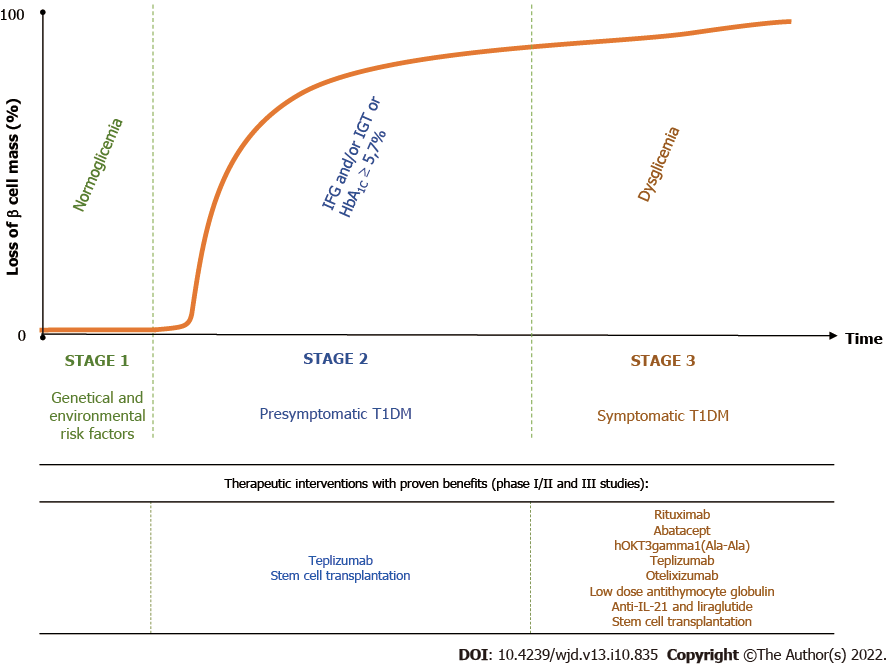
Figure 2 Stages of type 1 diabetes mellitus and options of therapeutic interventions with proven therapeutic benefits in phase II and III clinical trials.
The interaction between genetic predisposing factors, which are present from birth, and environmental factors trigger the autoreactive process. Stage 1 is characterized by individuals who exhibit at least two of the type 1 diabetes mellitus (T1DM)-associated antibodies (glutamic-acid-decarboxylase-, islet tyrosine phosphatase 2-, islet cell- and zinc transporter 8 antibodies). Stage 2 is characterized by dysglycemia due to reduced β-cell function. Stage 3 represents the onset of clinical T1DM and usually but not always the manifestation of typical symptoms. The application of the previously proposed staging system[12] in clinical trials, which even recognizes the earliest stages of T1DM, can improve the research and development of novel therapies that might delay/prevent the onset of the disease. IL: Interleukin; IFG: Impaired fasting glycemia; IGT: Impaired glucose tolerance; HBA1C: Glycated hemoglobin. Figure adapted from Insel et al[12].
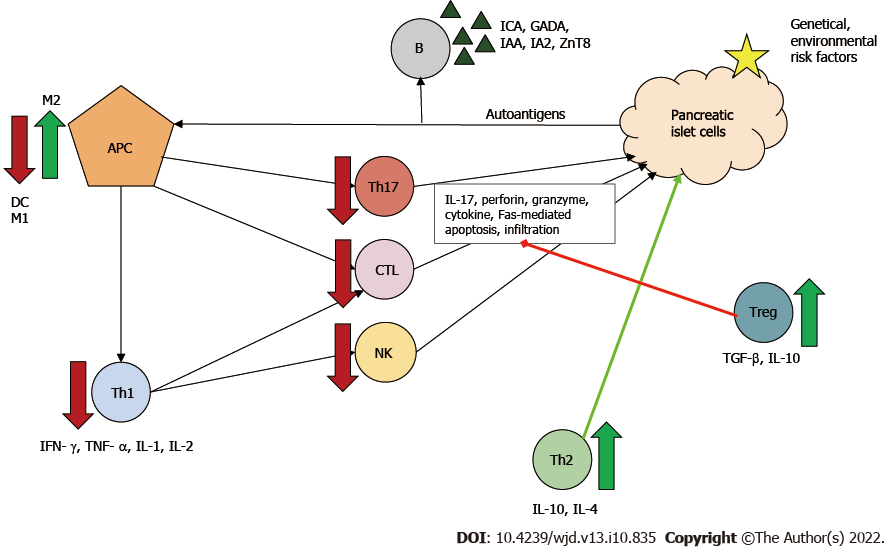
Figure 3 Immunoregulatory function of mesenchymal stem cells in type 1 diabetes mellitus.
The effects of mesenchymal stem cells ultimately result in downregulation in the proliferation and function of dendritic cells, cytotoxic T lymphocytes (CTLs), helper T (Th) type 1 and type 17 cells, natural killer (NK) cells and type 1 macrophages (M1). Meanwhile, mesenchymal stem cells increase the number of type 2 macrophages (M2) and regulatory T cells (Tregs), which can inhibit effector T cells and stimulate Th type 2 protective cells. Red arrow/line: Downregulation/inhibition; Green arrow/line: Stimulation. APC: Antigen-presenting cell; B: B cell; DC: Dendritic cell; GADA: Glutamic-acid-decarboxylase antibody; IA2: Islet tyrosine phosphatase 2 antibody; IAA: Insulin autoantibody; ICA: Islet cell antibody; IL: Interleukin; IFN-γ: Interferon γ; TGF-β: Transforming growth factor β; TNF-α: Tumor necrosis factor α; ZnT8: Zinc transporter 8 antibody.
- Citation: Nagy G, Szekely TE, Somogyi A, Herold M, Herold Z. New therapeutic approaches for type 1 diabetes: Disease-modifying therapies. World J Diabetes 2022; 13(10): 835-850
- URL: https://www.wjgnet.com/1948-9358/full/v13/i10/835.htm
- DOI: https://dx.doi.org/10.4239/wjd.v13.i10.835