Published online May 16, 2017. doi: 10.4253/wjge.v9.i5.204
Peer-review started: December 8, 2016
First decision: January 7, 2017
Revised: January 12, 2017
Accepted: February 28, 2017
Article in press: March 2, 2017
Published online: May 16, 2017
Processing time: 160 Days and 5.1 Hours
To investigate whether adenoma and polyp detection rates (ADR and PDR, respectively) in screening colonoscopies performed in the presence of fellows differ from those performed by attending physicians alone.
We performed a retrospective review of all patients who underwent a screening colonoscopy at Grady Memorial Hospital between July 1, 2009 and June 30, 2015. Patients with a history of colon polyps or cancer and those with poor colon preparation or failed cecal intubation were excluded from the analysis. Associations of fellowship training level with the ADR and PDR relative to attendings alone were assessed using unconditional multivariable logistic regression. Models were adjusted for sex, age, race, and colon preparation quality.
A total of 7503 colonoscopies met the inclusion criteria and were included in the analysis. The mean age of the study patients was 58.2 years; 63.1% were women and 88.2% were African American. The ADR was higher in the fellow participation group overall compared to that in the attending group: 34.5% vs 30.7% (P = 0.001), and for third year fellows it was 35.4% vs 30.7% (aOR = 1.23, 95%CI: 1.09-1.39). The higher ADR in the fellow participation group was evident for both the right and left side of the colon. For the PDR the corresponding figures were 44.5% vs 40.1% (P = 0.0003) and 45.7% vs 40.1% (aOR = 1.25, 95%CI: 1.12-1.41). The ADR and PDR increased with increasing fellow training level (P for trend < 0.05).
There is a stepwise increase in ADR and PDR across the years of gastroenterology training. Fellow participation is associated with higher adenoma and polyp detection.
Core tip: In this large sample of screening colonoscopies, we found that fellow participation has an overall favorable effect on adenoma and polyp detection rates, especially for fellows after their first year of training. The higher detection rate was evident in both the right and left colon. There were no differences overall regarding adenoma per colon or polyp per colon, between the fellow participation and attending groups. In summary, performance of screening colonoscopies by fellows under the strict supervision of attendings does not negatively affect the quality of the procedure, but rather increases adenoma and polyp detection.
- Citation: Qayed E, Shea L, Goebel S, Bostick RM. Association of trainee participation with adenoma and polyp detection rates. World J Gastrointest Endosc 2017; 9(5): 204-210
- URL: https://www.wjgnet.com/1948-5190/full/v9/i5/204.htm
- DOI: https://dx.doi.org/10.4253/wjge.v9.i5.204
Colorectal cancer (CRC) is the third most common cancer and second leading cause of cancer death in the United States. In 2016, it is estimated that 134490 individuals will be diagnosed with CRC, and approximately 49190 will die from this disease (26020 males and 23170 females)[1]. While these numbers are substantial, there has been an overall steady decline in the incidence of CRC, which represents a 40% decrease since 1975. More recently, between 2008 and 2012, CRC incidence decreased annually by about 3.6% in men and 3.8% in women[1]. An increase in screening for CRC with colonoscopy and other modalities is the most likely cause of those declines in CRC incidence. Colonoscopy is an important screening modality for CRC. The advantages of colonoscopy compared to the other modalities are the ability to directly examine the colonic mucosa and remove precancerous polyps during one session. The American College of Gastroenterology recommends colonoscopy as the preferred screening modality[2]. The results from several studies support that colonoscopy and polypectomy decrease mortality from colon cancer[3-5]. However, it has been consistently shown that the quality of colonoscopy varies among providers, and is dependent on several factors such as colon preparation quality, skills of the endoscopist, and length of withdrawal (examination) time. Furthermore, some studies found that colonoscopy decreases the risk of distal, but not proximal, colon cancer[6,7]. Given the importance of providing a quality colonoscopy, there is great interest in studying the effects of different procedural factors on the Adenoma and Polyp Detection Rates (ADR and PDR). Central to this discussion is the skill of the provider performing the colonoscopy. Colonoscopy quality differs widely among providers, and studies have reported a wide range of ADR (15%-50%) among endoscopists[8,9]. There is also some evidence that colonoscopies performed by gastroenterologists are associated with higher protection against colon cancer than are those performed by other providers[5].
Fellows are gastroenterology trainees who enroll in a three-year gastroenterology fellowship. Throughout their training, gastroenterology trainees acquire several procedural and non-procedural skills. They are supervised by attending gastroenterologists during procedures. First-year fellows rapidly acquire procedural skills; however, it is unclear whether their skill level changes substantially enough within the first year of training to affect their screening colonoscopy ADR and PDR. Most fellows in their third year of training have acquired adequate endoscopic skills, are ready for unsupervised practice, and are considered more skillful than first and second year fellows. Given that there is a known learning curve for colonoscopy, it is unclear whether the participation of fellows in screening colonoscopy affects the quality of the procedure, and whether their skill level at different stages of their training contributes to any changes in the quality of colonoscopy. There are relatively few reported studies that addressed this subject. In a small retrospective study of 309 patients, colonoscopies performed by fellows under the supervision of an attending had a higher ADR compared to those performed by attendings alone (37.2% vs 23%, P < 0.01)[10]. Another retrospective study found that ADRs increased as fellows advanced throughout their fellowship, with third year fellows having a higher ADR than did attendings (39.5% vs 27.7%), OR = 1.7 (1.33-2.17)[11]. Another study found that colonoscopies performed by fellows under the supervision of attendings were associated with a higher detection of small adenomas (< 5 mm), compared to procedures performed without a fellow (25% vs 17%, P = 0.001)[12]. There are several limitations to these studies, including the small sample sizes, the small number of procedures performed by fellows, inclusion of non-screening colonoscopies, and no stratification of fellows by year of training.
Herein we provide further clarification on the effect of fellow participation at different stages of training on the quality of screening colonoscopies. The primary aim of our study was to investigate whether GI fellows at various stages of training performing screening colonoscopies have different ADR and PDR compared to attendings. This was done by examining a large database of screening colonoscopies performed in patients aged 40 or older at a large teaching hospital.
This was a retrospective study using the endoscopic procedure database at Grady Memorial Hospital in Atlanta, GA. This database includes prospectively collected information about all endoscopic procedures performed in the Grady Memorial Hospital gastroenterology endoscopy unit, and includes procedure type, patient’s medical record number, age, race, procedure indication, endoscopist, fellow participation in the procedure, and fellow training level. The study included all outpatients who were at least 40 years old who underwent a screening colonoscopy between July 1, 2009 and June 30, 2015. Excluded patients included those who underwent colonoscopy for diagnostic purposes (e.g., abdominal pain, diarrhea, bleeding), surveillance for colorectal polyps, personal history of CRC, colorectal surgery, or inflammatory bowel disease. We also excluded patients whose procedures were aborted due to complications, severe pain and discomfort, failed cecal intubation, and those with poor bowel cleansing preparation (“prep”). The study was approved by the Institutional Review Board.
The computerized medical record was used to confirm the age and race of the patient, endoscopic findings, prep quality, cecal intubation, and polyp size, number, location, and histology. Race was categorized as white, black, and other. Bowel prep quality was categorized as good, fair-adequate, fair-inadequate, and poor. Colonoscopies with fair-adequate prep were those in which the prep quality was judged to allow for detection of all polyps ≥ 5 mm in size. Colonoscopies with poor prep had solid stool and generally required a repeat procedure within 3 mo. Polyp location was divided into right sided (cecum, ascending colon, hepatic flexure, and transverse colon), and left sided (descending colon, sigmoid, and rectum). Polyps were categorized into adenomatous and non-adenomatous polyps. Adenomatous polyps were categorized into advanced and non-advanced adenomas. Advanced adenomas included polyps with size ≥ 10 mm, villous or tubulovillous histology, high-grade dysplasia, or adenocarcinoma. Colonoscopies were categorized according to fellow participation as follows: Attending alone (procedure performed solely by attending) vs fellow present (fellow participated in any part of the procedure). Given that fellows start their fellowship training without endoscopic experience and rapidly accumulate endoscopic skills during their first year of training, fellow participation was also categorized as follows: Attending alone, fellow in first six months of training, fellow in second six months of training, fellow in second year, and fellow in third year.
Patients who were candidates for CRC screening were referred to the endoscopy unit from their primary care or gastroenterology clinic. Patients were given a standard 4 L of polyethylene glycol solution as a standard bowel preparation regimen. During the study period, there were 10 attendings and 34 fellows who performed the colonoscopies. In the endoscopy unit, patients were randomly assigned to endoscopy rooms during the course of the day. Attendings staffed the endoscopy rooms, with or without a fellow. All procedures were performed under moderate sedation. In colonoscopies performed with fellows, the fellow started the procedure and attempted insertion of the colonoscope to the cecum. In general, attendings intervened when there was difficulty passing a specific part of the colon, or if there was significant patient discomfort. Once the attending traversed the problematic area of the colon or the patient was better sedated, the scope was usually given back to the fellow to complete the insertion to the cecum and subsequent withdrawal of the scope. However, this was left to the discretion of the attending. Second and third year fellows are usually able to complete the colonoscopy without participation of the attending. The attending physicians strictly monitored all fellows during insertion and withdrawal of the scope.
Descriptive statistics, including mean, standard deviation, and frequencies, were used to characterize the study population. Characteristics of patients undergoing screening colonoscopy according to whether their colonoscopy was performed by an attending physician alone or with a fellow were compared using the student t test for continuous variables and the chi square test for categorical variables. Differences in the ADR, PDR, and advanced ADR across those for attendings alone and fellows at different points in training duration were assessed using the Mantel-Haenszel χ2 test to calculate the P for trend (non zero correlation). Associations of fellowship training level with the ADR, PDR, and advanced ADR (AADR) relative to attendings alone were assessed using unconditional multivariable logistic regression to calculate the adjusted odds ratios (ORs) and 95%CIs. Models were adjusted for sex, age, race, and colon preparation quality. Statistical significance was defined as a two-sided P value of ≤ 0.05% or a 95%CI that excluded 1.0. Analysis was performed using SAS version 9.4.
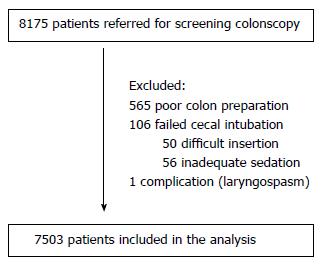
Between July 1, 2009 and July 1, 2015, 8175 colonoscopies were performed for the sole indication of screening for colon cancer. All procedures were performed under moderate sedation. Of these, 672 colonoscopies were excluded for the following reasons: 565 for poor colon preparation quality, 106 for failed cecal intubation, and 1 complication (laryngospasm). A total of 7503 screening colonoscopies were included in the analysis. Figure 1 shows the study flow diagram leading to the study population. Selected characteristics of the study patients according to whether their colonoscopy was performed by an attending physician alone or with a fellow are summarized in Table 1. The mean age of the study patients was 58.2 years, and 63.1% were women, 88.2% were African American, and 88.9% had a good colon preparation quality. A total of 67.2% of colonoscopies were performed with a training fellow, and an attending alone performed the rest.
| Characteristic | Attending alone (n = 2464, 32.8%) | Attending with fellow (n = 5039, 67.2%) | P value1 |
| Age in years (mean ± SD) | 57.9 ± 7.1 | 58.3 ± 7.1 | 0.02 |
| Female sex, n (%) | 1572 (63.8) | 3161 (62.7) | 0.37 |
| Race, n (%) | |||
| White | 120 (4.9) | 261 (5.2) | 0.15 |
| Black | 2198 (89.2) | 4423 (87.8) | |
| Other | 146 (5.9) | 355 (7.1) | |
| Preparation quality, n (%) | |||
| Good | 2199 (89.3) | 4469 (88.7) | 0.02 |
| Fair-adequate | 152 (6.2) | 382 (7.6) | |
| Fair-inadequate | 113 (4.6) | 188 (3.7) | |
| Fellow training level, n (%) | |||
| 1st 6 mo | N/A | 627 (12.4) | |
| 2nd 6 mo | N/A | 651 (12.9) | |
| 2nd year | N/A | 1413 (28.0) | |
| 3rd year | N/A | 2348 (46.6) | |
| ≥ 1 adenoma (ADR), n (%) | 756 (30.7) | 1736 (34.5) | 0.001 |
| ≥ 1 advanced adenoma (AADR), n (%) | 215 (8.7) | 416 (8.3) | 0.49 |
| ≥ 1 polyp (PDR), n (%) | 988 (40.1) | 2244 (44.5) | 0.0003 |
| ≥ 1 adenoma in right colon (RT-ADR), n (%) | 521 (21.1) | 1212 (24.1) | 0.005 |
| ≥ 1 adenoma in left colon (LT- ADR), n (%) | 365 (14.8) | 862 (17.1) | 0.01 |
| Mean number of APC | 0.61 | 0.68 | 0.03 |
| Mean number of PPC | 0.86 | 0.96 | 0.01 |
Differences in the ADR, PDR, and advanced ADR across those for attendings alone and fellows at different points in training duration are summarized in Tables 1 and 2. The ADR in the fellow participation group (all levels of training combined) was higher than that in the attending group (34.5% vs 30.7%, P = 0.001). The higher ADR in the fellow group was mainly related to second and third year fellows, but not first year fellows. Fellows in their third year of training had a higher ADR than did attendings alone (35.4% vs 30.7%; aOR = 1.23, 95%CI: 1.09-1.39). The higher ADR was evident in both the right and left colon. Similarly, the PDR was higher in procedures performed with fellows compared to those performed by attendings alone (44.5% vs 40.1%, P = 0.0003). Fellows in their third year of training had a higher PDR than did attendings alone (45.7% vs 40.1%, aOR = 1.25, 95%CI: 1.12-1.41). The ADR and PDR statistically significantly increased with increasing fellow training level (trend P value < 0.05). Fellows also detected more adenomas and polyps than did attendings. The mean number of adenoma per colon (APC) was higher in the fellows’ group than in the attendings alone group (0.68 vs 0.61, P = 0.03). Similarly, the mean number of polyps per colon (PPC) was higher in the fellows’ group than in the attendings alone group (0.96 vs 0.86, P = 0.01).
| Outcome | Fellowship training level | Detection rate | Trend P value1 | aOR2 | 95%CI | P value |
| ≥ 1 adenoma (ADR) | Attending alone (reference) | 30.7% | 0.0003 | 1.00 | - | |
| Fellow in 1st 6 mo | 32.4% | 1.07 | 0.89-1.3 | 0.47 | ||
| Fellow in 2nd 6 mo | 33.3% | 1.16 | 0.96-1.39 | 0.13 | ||
| Fellow in 2nd year | 34.4% | 1.15 | 1.00-1.32 | 0.06 | ||
| Fellow in 3rd year | 35.4% | 1.23 | 1.09-1.39 | 0.001 | ||
| ≥ 1 polyp (PDR) | Attending alone (reference) | 40.1% | < 0.0001 | 1.00 | - | |
| Fellow in 1st 6 mo | 42.4% | 1.10 | 0.92-1.32 | 0.28 | ||
| Fellow in 2nd 6 mo | 42.7% | 1.14 | 0.96-1.36 | 0.14 | ||
| Fellow in 2nd year | 44.4% | 1.17 | 1.02-1.33 | 0.02 | ||
| Fellow in 3rd year | 45.7% | 1.25 | 1.12-1.41 | 0.0001 | ||
| ≥ 1 advanced adenoma (AADR) | Attending alone (reference) | 8.7% | 0.7 | 1.00 | - | |
| Fellow in 1st 6 mo | 4.8% | 0.52 | 0.35-0.76 | 0.001 | ||
| Fellow in 2nd 6 mo | 9.1% | 1.06 | 0.78-1.44 | 0.71 | ||
| Fellow in 2nd year | 9.3% | 1.05 | 0.83-1.31 | 0.7 | ||
| Fellow in 3rd year | 8.3% | 0.93 | 0.76-1.15 | 0.51 | ||
| ≥ 1 adenoma in right colon (RT-ADR) | Attending alone (reference) | 21.1% | 1.00 | - | ||
| Fellow in 1st 6 mo | 22.3% | 0.002 | 1.05 | 0.85-1.3 | 0.64 | |
| Fellow in 2nd 6 mo | 23.4% | 1.16 | 0.94-1.42 | 0.17 | ||
| Fellow in 2nd year | 23.9% | 1.14 | 0.98-1.34 | 0.1 | ||
| Fellow in 3rd year | 24.8% | 1.22 | 1.06-1.39 | 0.005 | ||
| ≥ 1 adenoma in left colon (LT-ADR) | Attending alone (reference) | 14.8% | 0.01 | 1.00 | - | |
| Fellow in 1st 6 mo | 16.1% | 1.16 | 0.87-1.41 | 0.42 | ||
| Fellow in 2nd 6 mo | 16.4% | 1.15 | 0.91-1.46 | 0.24 | ||
| Fellow in 2nd year | 16.8% | 1.13 | 0.94-1.35 | 0.18 | ||
| Fellow in 3rd year | 17.7% | 1.23 | 1.06-1.44 | 0.01 |
There was no difference in the AADR between the fellows group and the attending group (8.3% vs 8.7%, P = 0.49). However, fellows in their first six months of training had a lower AADR than did attendings alone (4.8% vs 8.7%, aOR = 0.52, 95%CI: 0.35-0.76). We further analyzed this finding by examining the proportion of procedures that had a large adenoma (≥ 1 cm), villous histology, or high-grade dysplasia (HGD) and/or cancer (Table 3). The lower AADR in the fellows in their first six months of training was mainly related to lower detection of large adenomas (3.4% vs 7.9%, P < 0.0001). There were no differences in the detection of adenomas with villous histology or those with HGD and/or cancer. In addition, there was no difference in the detection of right or left sided adenomas. On average, fellows in their first six months of training and attendings detected a similar number of adenomas per colon (0.64 vs 0.61, P = 0.54).
| Attending alone n = 2464 n (%) | Fellows 1st 6 mo n = 627 n (%) | P value1 | |
| ≥ 1 advanced adenoma (AADR) | 215 (8.7) | 30 (4.8) | 0.001 |
| ≥ 1 adenoma ≥ 1 cm | 194 (7.9) | 21 (3.4) | < 0.0001 |
| ≥ 1 adenoma with villous histology | 83 (3.4) | 14 (2.2) | 0.15 |
| ≥ 1 adenoma with HGD and/or cancer | 26 (1.1) | 4 (0.6) | 0.34 |
| Mean number of APC | 0.61 | 0.64 | 0.54 |
Our results suggest that the participation of gastroenterology fellows overall in screening colonoscopy may be associated with higher adenoma and polyp detection. In our study, a higher level of detection was manifested both as the number of colonoscopies with at least one adenoma or polyp (ADR and PDR), and the mean number of adenomas and polyps per colon. Furthermore, our findings suggest that fellow’s level of training and experience is directly associated with polyp detection. There was a stepwise increase in adenoma and polyp detection with higher levels of fellow training. Fellows in the first year of training and attendings had similar ADRs and PDRs, while fellows in their second and third year of training had higher values. The higher ADR in the fellows group was seen in both the right and left colon. These findings have clinical significance. Performance of colonoscopies by gastroenterology fellows, who have less experience than attendings, does not appear to negatively affect adenoma and polyp detection in colonoscopy, provided that they are adequately supervised, and may be associated with somewhat greater adenoma and polyp detection. The higher detection of polyps in procedures in which fellows participate could be related to the presence of an additional observer who monitors the screen with the primary endoscopist, and can lead to an increased recognition of small polyps. Previous studies found that endoscopy nurse participation leads to increased polyp detection[13,14]. In addition, participation of fellows could lead to a more focused withdrawal of the colonoscope in which the attending physician actively instructs the fellow to examine behind each colonic fold, thereby increasing the chances of detecting polyps. Our findings also suggest that detection of polyps is a learned skill that continues to improve during fellowship training, highlighting the importance of gaining adequate experience during training to maximize polyp detection.
Our study had several strengths. Unlike previous studies that included non-screening colonoscopies, we focused our analysis on outpatients presenting for the sole indication of colorectal cancer screening. The goal of colonoscopy in patients presenting with clinical indications, such as acute overt bleeding, abdominal pain or constipation, is often to diagnose the etiology of symptoms and not to detect and resect polyps. Polypectomy is often deferred in these patients with acute indications until their symptoms resolve. In addition, our study included a large number of colonoscopies performed by trainees at different levels of training. Finally, comparisons of colonoscopy quality between attendings alone and fellows are more meaningful when the level of fellow training is considered. We categorized the level of fellow training in a way that reflects their learning curve, as fellows rapidly gain endoscopic skills in the first 6 mo of training, and progress to become more independent endoscopists in their second and third year. Finally, the retrospective nature of this study eliminated the possibility of the “Hawthorne effect”, in which endoscopists alter their behavior as they know that detection rates are being recorded and compared, which is more likely to occur in a prospective study design. One study found that when endoscopists know that their procedures are being recorded for review, they improve the quality of their exam (luminal distension, cleaning of the colon, and length of inspection time), resulting in an increased ADR[15].
Our study had several limitations. It was a retrospective study and it was not possible to accurately describe the degree of fellow participation in colonoscopy. It is possible that attendings performed the withdrawal part of some procedures, and therefore we cannot directly attribute the differences in adenoma and polyp detection to the fellow’s technical skills. We had no data on the colonoscopy insertion and withdrawal times. This would have provided insight about the observed increased polyp detection in second and third year fellows. Longer withdrawal times have been linked to higher adenoma detection rates in screening colonoscopy[16]. It is unclear whether the higher detection rate in second and third year fellows was related to longer withdrawal times or to the technical skill of the fellow combined with the guidance and supervision from the attending, or both. In addition, we did not account for several factors that affect polyp and adenoma prevalence, such as family history of colon cancer, smoking, and aspirin use, the data for which were unavailable. However, we accounted for several important confounders such as age, race, sex, and colonoscopy preparation quality. Given the nature of patient flow through the endoscopy unit where patients are shared between attendings, it is unlikely that there was significant difference in the proportion of patients with a family history of CRC, aspirin use, or other unmeasured confounders between the attending alone and the fellows group. Finally, our study was limited to one training program, and thus may not be generalizable to others.
The finding of a lower AADR in fellows in their first six months of training than in attendings alone was unexpected. This difference was likely primarily attributable to there having been a higher percentage of colonoscopies in which one adenoma ≥ 1 cm was detected in procedures performed by attendings alone. It is unlikely that this was related to fellows underestimating polyp size while they were documenting their procedures early in their training. In general, attendings and fellows discuss findings and write down the sizes and locations of polyps during the procedure, and a final report is entered in the medical record system after the procedure is completed. In addition, attendings sign off on the colonoscopy report and make the necessary changes as they see appropriate. It is reassuring that the ADR itself was not different between fellows in the first six month of training and attendings alone (32.4% vs 30.7%, P = 0.47). Furthermore, there was no difference in the average number of adenomas per colon between these two groups (0.61 vs 0.64, P = 0.54), nor was there a difference in adenoma detection in the right vs the left colon. This suggests that fellows are finding the same number of polyps, though the size of these polyps may be smaller than those found by attendings.
In summary, we found that gastroenterology fellow involvement overall in screening colonoscopy is associated with overall higher ADR and PDR. These higher detection rates were mainly seen in procedures performed by second and third year fellows. Since the AADR was lower in procedures performed with fellows in their first six month of training, increased vigilance in these procedures and an attending joining the fellow in performing a careful withdrawal of the scope, with adequate withdrawal time and careful documentation of polyp size, are indicated. Further studies that document the exact involvement of fellows in the procedure, withdrawal time, and location of polyps would help identify factors related to higher polyp detection rates in more experienced fellows. This would ultimately allow us to optimize fellow involvement and training in screening colonoscopy, while maintaining a high quality examination.
Colonoscopy is an important screening modality for colorectal cancer. Participation of gastroenterology fellows in screening colonoscopies has been shown to have a positive effect on the quality of the procedure. However, it is unclear how participation of fellows in their early stages of training (e.g., first six months) affects the quality of colonoscopy. Furthermore, it is unclear if the effects are the same in the right and left side of the colon.
The adenoma detection rate (ADR) is an important measure of colonoscopy quality and it has been linked to the development of interval colon cancer. In addition to patient-related factors that affect ADR, it is important to study the endoscopist-related factors ADR, such as participation of fellows and their stage of training.
Similar to previous studies, they found that participation of fellows in screening colonoscopy increases ADR and polyp detection rate (PDR) compared to attendings alone. This is the first study to examine the effect of fellows in the very early stage of training (first 6 mo) on colonoscopy findings. The authors found that fellows in their first six months of training have similar ADR compared to attendings, but have lower advanced ADR. The lower ADR was mainly related to lower percentage of polyps ≥ 1 cm.
This study suggests that participation of fellows in their second and third year of training increases ADR and PDR in both the right and left side of the colon. Gastroenterology attendings should continue to adequately supervise fellows performing colonoscopy, and patients can be reassured that participation of fellows, even in their early stages of training, does not negatively affect the quality of their procedure.
Qayed and colleagues conducted a large retrospective study examined the association of trainee participation with adenoma and polyp detection rate. This is a retrospective study with all the potential limitation of that but it is very well written.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Cremers MI, Madhoun MF, Imagewa A S- Editor: Qi Y L- Editor: A E- Editor: Wu HL
| 1. | Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin. 2016;66:7-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12135] [Cited by in RCA: 12991] [Article Influence: 1443.4] [Reference Citation Analysis (2)] |
| 2. | Rex DK, Johnson DA, Anderson JC, Schoenfeld PS, Burke CA, Inadomi JM. American College of Gastroenterology guidelines for colorectal cancer screening 2009 [corrected]. Am J Gastroenterol. 2009;104:739-750. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 981] [Cited by in RCA: 1059] [Article Influence: 66.2] [Reference Citation Analysis (0)] |
| 3. | Zauber AG, Winawer SJ, O’Brien MJ, Lansdorp-Vogelaar I, van Ballegooijen M, Hankey BF, Shi W, Bond JH, Schapiro M, Panish JF. Colonoscopic polypectomy and long-term prevention of colorectal-cancer deaths. N Engl J Med. 2012;366:687-696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1952] [Cited by in RCA: 2286] [Article Influence: 175.8] [Reference Citation Analysis (2)] |
| 4. | Nishihara R, Wu K, Lochhead P, Morikawa T, Liao X, Qian ZR, Inamura K, Kim SA, Kuchiba A, Yamauchi M. Long-term colorectal-cancer incidence and mortality after lower endoscopy. N Engl J Med. 2013;369:1095-1105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 968] [Cited by in RCA: 1158] [Article Influence: 96.5] [Reference Citation Analysis (0)] |
| 5. | Baxter NN, Warren JL, Barrett MJ, Stukel TA, Doria-Rose VP. Association between colonoscopy and colorectal cancer mortality in a US cohort according to site of cancer and colonoscopist specialty. J Clin Oncol. 2012;30:2664-2669. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 228] [Cited by in RCA: 271] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 6. | Baxter NN, Goldwasser MA, Paszat LF, Saskin R, Urbach DR, Rabeneck L. Association of colonoscopy and death from colorectal cancer. Ann Intern Med. 2009;150:1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 911] [Cited by in RCA: 920] [Article Influence: 57.5] [Reference Citation Analysis (0)] |
| 7. | Singh H, Nugent Z, Demers AA, Kliewer EV, Mahmud SM, Bernstein CN. The reduction in colorectal cancer mortality after colonoscopy varies by site of the cancer. Gastroenterology. 2010;139:1128-1137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 341] [Cited by in RCA: 373] [Article Influence: 24.9] [Reference Citation Analysis (0)] |
| 8. | Kahi CJ, Ballard D, Shah AS, Mears R, Johnson CS. Impact of a quarterly report card on colonoscopy quality measures. Gastrointest Endosc. 2013;77:925-931. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 104] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 9. | Chen SC, Rex DK. Endoscopist can be more powerful than age and male gender in predicting adenoma detection at colonoscopy. Am J Gastroenterol. 2007;102:856-861. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 284] [Cited by in RCA: 306] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 10. | Rogart JN, Siddiqui UD, Jamidar PA, Aslanian HR. Fellow involvement may increase adenoma detection rates during colonoscopy. Am J Gastroenterol. 2008;103:2841-2846. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 78] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 11. | Peters SL, Hasan AG, Jacobson NB, Austin GL. Level of fellowship training increases adenoma detection rates. Clin Gastroenterol Hepatol. 2010;8:439-442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 70] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 12. | Buchner AM, Shahid MW, Heckman MG, Diehl NN, McNeil RB, Cleveland P, Gill KR, Schore A, Ghabril M, Raimondo M. Trainee participation is associated with increased small adenoma detection. Gastrointest Endosc. 2011;73:1223-1231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 94] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 13. | Dellon ES, Lippmann QK, Sandler RS, Shaheen NJ. GI endoscopy nurse experience and polyp detection during screening colonoscopy. Clin Gastroenterol Hepatol. 2008;6:1342-1347. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 20] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Lee CK, Park DI, Lee SH, Hwangbo Y, Eun CS, Han DS, Cha JM, Lee BI, Shin JE. Participation by experienced endoscopy nurses increases the detection rate of colon polyps during a screening colonoscopy: a multicenter, prospective, randomized study. Gastrointest Endosc. 2011;74:1094-1102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 94] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 15. | Rex DK, Hewett DG, Raghavendra M, Chalasani N. The impact of videorecording on the quality of colonoscopy performance: a pilot study. Am J Gastroenterol. 2010;105:2312-2317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 89] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 16. | Barclay RL, Vicari JJ, Doughty AS, Johanson JF, Greenlaw RL. Colonoscopic withdrawal times and adenoma detection during screening colonoscopy. N Engl J Med. 2006;355:2533-2541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 911] [Cited by in RCA: 951] [Article Influence: 50.1] [Reference Citation Analysis (0)] |