Published online Dec 16, 2017. doi: 10.4253/wjge.v9.i12.590
Peer-review started: August 27, 2017
First decision: October 9, 2017
Revised: October 25, 2017
Accepted: November 11, 2017
Article in press: November 11, 2017
Published online: December 16, 2017
Processing time: 102 Days and 4.5 Hours
Jackhammer (hypercontractile) esophagus presents with dysphagia and chest pain. Current treatments are limited. We describe a 60-year-old man who presented with dysphagia, chest pain and heartburn for a period of 1 year. His workup showed Barrett’s esophagus on endoscopy and high-resolution manometry demonstrated jackhammer esophagus with esophagogastric junction outflow obstruction. The patient was treated with proton pump inhibitor and nifedipine but without resolution of his symptoms. He was followed up to assess the efficacy of treatment with deanxit (flupentixol + melitracen). Dysphagia and chest pain resolved during the therapeutic trial and efficacy was maintained on maintenance treatment without troublesome side effects.
Core tip: Low-dose antidepressants can improve patients’ reaction to the pain associated with esophageal dynamic disorders. The case report describes that deanxit (flupentixol + melitracen) has a positive effect on a new, rare disease, jackhammer esophagus, and speculates upon the potential relationship between mental factors and jackhammer esophagus.
- Citation: Li JY, Zhang WH, Huang CL, Huang D, Zuo GW, Liang LX. Deanxit relieves symptoms in a patient with jackhammer esophagus: A case report. World J Gastrointest Endosc 2017; 9(12): 590-593
- URL: https://www.wjgnet.com/1948-5190/full/v9/i12/590.htm
- DOI: https://dx.doi.org/10.4253/wjge.v9.i12.590
High-resolution manometry (HRM) has provided a new method for clinical diagnosis and treatment of esophageal motility disorders. Based on HRM techniques, the new Chicago classification has revised the esophageal motility disorder diagnostic criteria, mainly for achalasia and esophageal body motility disorders. Jackhammer esophagus is a new entity within spastic disorders of the esophagus[1]. Moreover, it has recently been described by a new Chicago Classification version 3.0 with at least two swallows with distal contractile integral (DCI) > 8000 mmHg-s-cm[2]. We describe a patient with impaired esophagogastric junction (EGJ) relaxation and hypercontractile peristaltic disorder, accompanying depressive disorder, which has not been reported in China. Treatment with deanxit (flupentixol + melitracen) led to an unusual recovery.
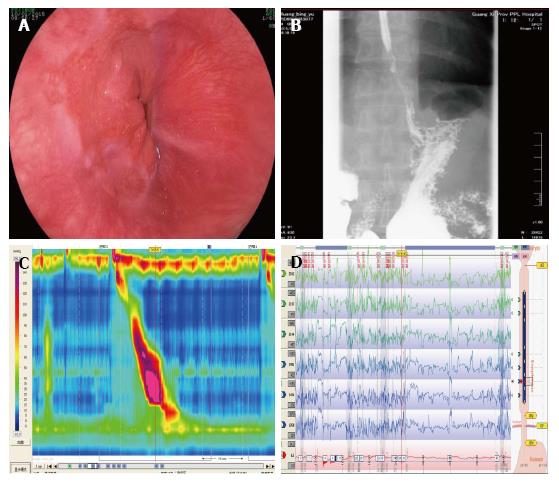
A 60-year-old man visited our hospital because of a 1-year history of intermittent and recurrent episodes of dysphagia, chest pain and heartburn in January 2015. In another hospital, he had taken proton pump inhibitors (PPIs) for > 1 mo, but he was not relieved of any symptoms. There was nothing remarkable in his medical history. Physical and laboratory examinations showed no specific findings. Endoscopy showed possible Barrett’s esophagus (BE) (Figure 1A). Moreover, esophageal mucosal biopsy suggested gastric mucosa ectopia. A barium esophagogram showed reflux esophagitis and spastic contraction in the distal esophagus (Figure 1B). He underwent HRM (Sierra Scientific Instruments, Los Angeles, CA, United States) and 24-h esophageal impedance-pH monitoring (Sierra Scientific Instruments). HRM showed that the maximum DCI was 8099.9 mmHg-s-cm and the integrated relaxation pressure (IRP) was 21.5 mmHg (Figure 1C). Pathological acid reflux was reported by 24-h esophageal impedance-pH evaluation (Figure 1D). Medical therapy with nifedipine 10 mg twice daily, esomeprazole 20 mg twice daily and teprenone 50 mg twice daily for approximately 10 mo showed no improvement in dysphagia and chest pain, but the symptoms of acid regurgitation and heartburn had relieved.
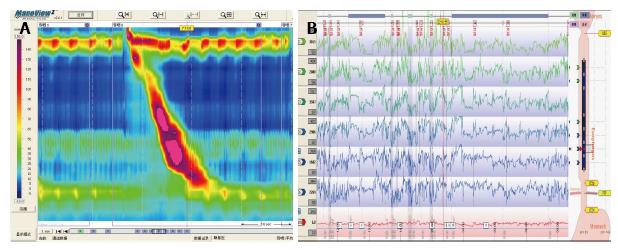
He was seen in our hospital in December 2015 with worsening dysphagia and chest pain. However, laboratory investigations were normal again including serum troponin level, electrocardiography monitoring and coronary angiography. HRM and 24-h esophageal impedance-pH monitoring were repeated. HRM showed typical hypercontractile contractions (6 swallows with DCI > 8000 mmHg-s-cm in 10 liquid swallows) and IRP 14.7 mmHg (Figure 2A), whereas impedance-pH monitoring was negative (Figure 2B). Close examination of his medical history revealed long-term sleep disorders, with difficulty falling asleep, worrying about cancer, and anxiety. The patient was judged to be in a depressive state by a psychiatrist. Drug therapy was adjusted to deanxit 0.5 mg/10 mg (one piece) twice daily, rabeprazole 10 mg twice daily and hydrotalcite 1 g three times daily, and the patient’s symptoms improved, with no obviously reflux, chest pain, and dysphagia after 5 d treatment. Moreover, he continued this therapy as-maintained basis.
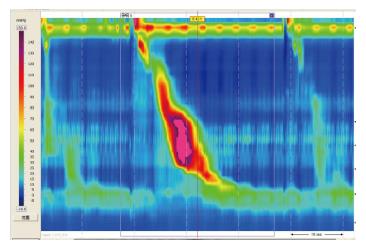
At follow-up 5 mo later, the patient described clinical improvement with only one episode of dysphagia and chest pain, because of stopping his medication without permission. However, symptoms were relieved soon after he takes medicine. He was re-examined by HRM in May 2016, which showed IRP 10.1 mmHg (normal < 15 mmHg) and mean DCI 6750 mmHg-s-cm (Figure 3). The total period of treatment was 6 mo, with deanxit dose gradually reduced until withdrawal under the guidance of a psychologist and gastroenterologist. In June 2017, the patient had recovered well without recurrence of symptoms.
Jackhammer esophagus is a rare disorder that occurs in 4% of patients referred to a tertiary center for HRM, and these patients with extreme phenotypes of esophageal hypercontractility present mainly with dysphagia, chest pain, and gastroesophageal reflux symptoms[3]. Nowadays there appears to be no clear consensus about optimal therapy, and options are similar to other esophageal dysmotility disorders. Pharmacological treatment should be considered first, with a combination of nitrates, calcium channel blockers, phosphodiesterase-5 inhibitors and PPIs having potential benefit[4]. Recently, Marjoux et al[5] reported that esophageal botulinum toxin was effective for treatment of hypertensive esophageal motility disorders. There were also recently reported cases of successful treatment with peroral endoscopic myotomy[6] and balloon dilatation[7]. Tsutomu et al[8] have reported that surgery using thoracoscopic esophageal extended myotomy is beneficial.
Patients with jackhammer esophagus can present with mechanical EGJ outflow obstruction, gastroesophageal reflux disease, or primary esophageal muscle hypercontractility[3]. Our patient had high IRP; a hypercontractile peristaltic disorder of the esophagus that overlaps with BE. The first treatment strategy of spastic disorders depends on whether there is an accompanying EGJ outflow obstruction[4]. Moreover, there is a lack of evidence for the value of pharmacological treatment alone if EGJ relaxation is impaired. Therefore, we selected medical therapy first. A trial of nifedipine and PPIs have been chosen. The IRP was normal and changed to jackhammer esophagus without EGJ outflow obstruction and pathological acid reflux.
Low-dose antidepressants can improve patients’ reaction to pain without objectively improving motility function[9]. Our patient had obvious chest pain and dysphagia with esophageal hypercontractility. We allowed him to take antidepressants (deanxit) because he had depression. The patient’s clinical and objective esophageal indexes were improved. Previous studies have established that the psychosocial aspects are related to gastroesophageal reflux disease and functional esophageal disorders, such as functional chest pain, functional dysphagia and hypersensitive esophagus[10,11]. In the present study, we examined the influence of the relationship between mental factors and jackhammer esophagus. Deanxit had surprising efficacy for this patient, so we speculated that his depressive disorder may have caused hypercontractile peristaltic disorder because of nonspecific esophageal motility disorder. Alternatively, it may be that the patient endured painful symptoms for a long period, resulting in psychiatric comorbidity of jackhammer esophagus. The underlying pathological mechanisms in this case are unclear and deserve further study.
In summary, despite the evidence of efficacy, the long-term optimal management of jackhammer esophagus is not yet established. In our patient with a rare esophageal motility disorder and depression, antianxiety and antidepressant agents relieved his symptoms. However, the duration of treatment with antidepressants in patients with jackhammer esophagus and longer follow-up need further discussion.
A 60-year-old man with a 1-year history of intermittent and recurrent episodes of dysphagia, chest pain and heartburn, who had taken PPIs for a long time, but without relief of any symptoms.
Dysphagia, chest pain and heartburn and depressive state.
Achalasia, gastroesophageal reflux disease, esophageal infections, esophageal carcinoma, coronary heart disease.
All laboratory parameters were within normal limits.
High-resolution manometry (HRM) showed six swallows with distal contractile integral (DCI) > 8000 mmHg-s-cm in 10 liquid swallows and integrated relaxation pressure (IRP) 14.7 mmHg.
Esophageal mucosa appeared as ectopia of gastric mucosa.
Deanxit for 6 mo, gradually reduced until withdrawal.
Jackhammer esophagus is a rare disorder, and current treatments are limited, such as botulinum toxin injection, peroral endoscopic myotomy, and balloon dilatation.
Jackhammer esophagus is a rare esophagus disorder, and patients with extreme phenotypes of esophageal hypercontractility present mainly with dysphagia, chest pain, and gastroesophageal reflux symptoms. Jackhammer esophagus is described by a new Chicago Classification version 3.0 with at least two swallows with DCI > 8000 mmHg-s-cm.
Patients with esophageal hypercontractility present mainly with dysphagia, chest pain, and HRM is the primary diagnostic method. Patients may also have mental illness, so at the time of diagnosis, psychological evaluation is necessary. Antianxiety and antidepressant agents are promising medical treatment to relieve symptoms in patients with jackhammer esophagus combined with psychosocial problems, but longer follow-up is needed.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Conzo G, Imagawa A, Kvolik S, Yu SP S- Editor: Gong ZM L- Editor: A E- Editor: Lu YJ
| 1. | Roman S, Pandolfino JE, Chen J, Boris L, Luger D, Kahrilas PJ. Phenotypes and clinical context of hypercontractility in high-resolution esophageal pressure topography (EPT). Am J Gastroenterol. 2012;107:37-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 115] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 2. | Kahrilas PJ, Bredenoord AJ, Fox M, Gyawali CP, Roman S, Smout AJ, Pandolfino JE; International High Resolution Manometry Working Group. The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 2015;27:160-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1373] [Cited by in RCA: 1442] [Article Influence: 144.2] [Reference Citation Analysis (0)] |
| 3. | Jia Y, Arenas J, Hejazi RA, Elhanafi S, Saadi M, McCallum RW. Frequency of Jackhammer Esophagus as the Extreme Phenotypes of Esophageal Hypercontractility Based on the New Chicago Classification. J Clin Gastroenterol. 2016;50:615-618. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 4. | Roman S, Kahrilas PJ. Management of spastic disorders of the esophagus. Gastroenterol Clin North Am. 2013;42:27-43. [PubMed] |
| 5. | Marjoux S, Brochard C, Roman S, Gincul R, Pagenault M, Ponchon T, Ropert A, Mion F. Botulinum toxin injection for hypercontractile or spastic esophageal motility disorders: may high-resolution manometry help to select cases? Dis Esophagus. 2015;28:735-741. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 36] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 6. | Ko WJ, Lee BM, Park WY, Kim JN, Cho JH, Lee TH, Hong SJ, Cho JY. Jackhammer esophagus treated by a peroral endoscopic myotomy. Korean J Gastroenterol. 2014;64:370-374. [PubMed] |
| 7. | Pelletier AL, Pospai D, Merrouche M. Balloon against Jackhammer Disorder. Case Rep Gastroenterol. 2013;7:467-469. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Nomura T, Iwakiri K, Uchida E. Thoracoscopic treatment of a patient with jackhammer esophagus. Dig Endosc. 2014;26:753-754. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Clouse RE, Lustman PJ, Eckert TC, Ferney DM, Griffith LS. Low-dose trazodone for symptomatic patients with esophageal contraction abnormalities. A double-blind, placebo-controlled trial. Gastroenterology. 1987;92:1027-1036. [PubMed] |
| 10. | Bilgi MM, Vardar R, Yıldırım E, Veznedaroğlu B, Bor S. Prevalence of Psychiatric Comorbidity in Symptomatic Gastroesophageal Reflux Subgroups. Dig Dis Sci. 2017;62:984-993. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 11. | Drossman DA. Functional Gastrointestinal Disorders: History, Pathophysiology, Clinical Features and Rome IV. Gastroenterology. 2016; Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1366] [Cited by in RCA: 1356] [Article Influence: 150.7] [Reference Citation Analysis (1)] |