Published online Dec 16, 2017. doi: 10.4253/wjge.v9.i12.579
Peer-review started: February 6, 2017
First decision: March 6, 2017
Revised: March 31, 2017
Accepted: April 23, 2017
Article in press: April 23, 2017
Published online: December 16, 2017
Processing time: 306 Days and 0.1 Hours
Epithelioid sarcoma (ES), a mesenchymatous malign neoformation, is often diagnosed in later stages and associated with high recurrence index, metastasis and mortality. We report a case of a 65 years old male, with history of abdominal pain and upper gastrointestinal bleeding. Endoscopy demonstrated a posterior duodenal wall perforation communicating with a solid retroperitoneal neoformation. Endoscopic biopsy was performed, with a final report of ES. The patient was submitted for surgical palliation due to the tumor’s unresectability. Retroperitoneal ES is an extremely rare condition with limited reports in the literature where guidelines for its optimal treatment are not well established.
Core tip: Epithelioid sarcoma (ES) is a rare malign neoformation, often diagnosed in later stages and associated with high recurrence index and mortality. We report a case of a 65 years old male with a posterior duodenal wall perforation found during endoscopy, communicating with a solid retroperitoneal neoformation. Endoscopic biopsies were sufficient for the diagnosis. Retroperitoneal ES is an extremely rare condition with limited reports, where guidelines for its optimal treatment are not well established.
- Citation: Coronado JA, Chávez MÁ, Manrique MA, Cerna J, Trejo AL. Retroperitoneal epithelioid sarcoma: A case report. World J Gastrointest Endosc 2017; 9(12): 579-582
- URL: https://www.wjgnet.com/1948-5190/full/v9/i12/579.htm
- DOI: https://dx.doi.org/10.4253/wjge.v9.i12.579
Epithelioid sarcoma (ES) was originally described in 1970 by Enzinger[1]. It is a rare malignant mesenchymatous tumor more frequently found in young patients from 23 to 40 years old; however with a range of presentation between 4 and 90 years of age[2]. Due to its diverse clinical scenario, diagnosis is generally delayed. Usually divided in proximal and distal presentation, with predominant topography on distal zones such as upper extremities, mainly fingers, hands and wrists[3]. The distal form is composed of spindle to polygonal epithelioid cells arranged in nodules with central necrosis. The proximal form was described in 1997, arising in the deep part of the pelvis, perineum and genital tract. It presents large epithelioid carcinoma-like cells and has a more aggressive clinical course than the distal presentation[4].
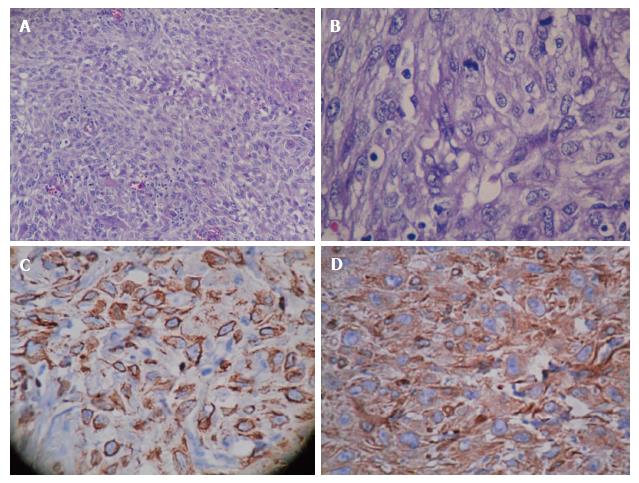
Microscopic appearance of ES ranges from spindle cells to large polygonal cells with an acidophilic cytoplasm[5]. Diagnosis can be confirmed with immunochemical staining positive for epithelial markers such as cytokeratin and epithelial membrane antigen, a mesenchymatous marker (vimentin) and CD34[6]. Finally, in some small series cytogenetic analysis has been performed, finding genetic alterations at the long arm of chromosome 22[7].
ES is distinguished by its high recurrence rate, with local recurrences reported in up to 77%, and an elevated percentage of node and lung metastasis (36%-44%)[8]. Five year, and 10-year survival are 65.3% and from 25% to 50% respectively[6]. However, the mean time from recurrence to death in patients older than 36 years stands at 5.6 ± 4.5 mo and in younger patients at 15.2 ± 17.2 mo[3]. Furthermore, the specific treatment for this pathology has not been established by international consensus; where a distal type ES tends to avoid amputation, a local recurrence is treated with local excision plus radiotherapy[7]. But, in tumors with unfavorable factors such as, proximal type or size greater than 5 cm, a systemic treatment plus surgical intervention should be evaluated[9].
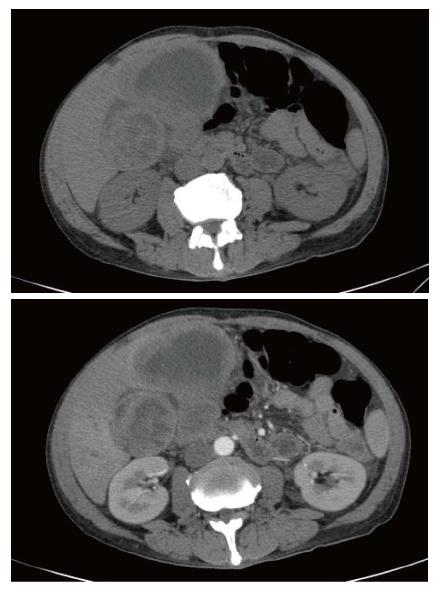
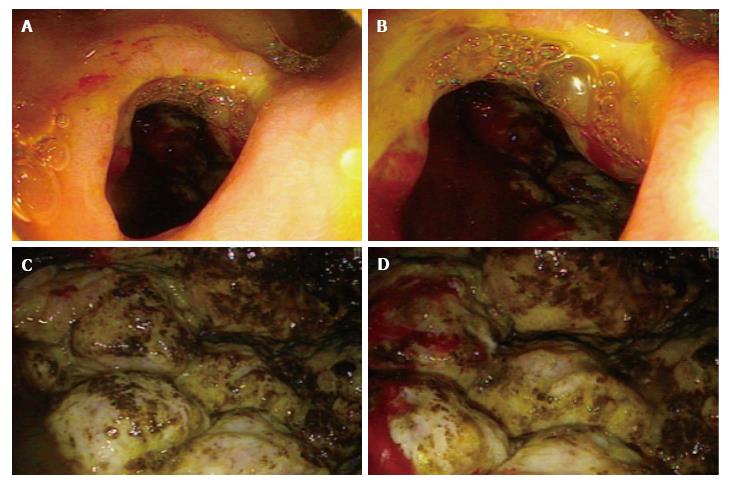
A 65 years old Hispanic male with a remarkable medical history, presented with a one month history of right upper quadrant abdominal pain and upper gastrointestinal bleeding characterized by intermittent melena. Episodes of fever were also reported. Physical examination revealed a palpable right upper quadrant abdominal mass extending up to 4 cm below the costal margin. CT scan reported an infiltrative lesion in duodenum and gallbladder affecting the splenic, hepatic and mesenteric vascularity (Figures 1 and 2). Endoscopy was performed finding a 2 cm opening from the posterior duodenal wall communicating with a solid retroperitoneal mass, irregular, indurated and extremely friable measuring more than 10 cm in diameter (Figure 3).
The patient was treated with palliative surgery, performing a gastro-jejunal anastomosis, with a postoperative report of retroperitoneal tumor invading duodenum and gallbladder. Final histopathological report stated the presence of retroperitoneal ES positive for cytokeratin and vimentin (Figure 4). Lastly, the patient was deceased two weeks after the initial diagnosis.
ES is a soft tissue malignant entity with a high recurrence rate and mortality. Thus, the importance of reporting this case in order to increase awareness of this rare disease; since it seems only an early diagnosis with definite surgical treatment can improve prognosis. In this particular case, endoscopy was helpful as the duodenal perforation allowed direct examination and prompt biopsy samples from the lesion. However, urgent surgical consultation was needed once the bowel perforation was found. In conclusion, ES is an infrequent variant of malignant sarcoma, with a very aggressive behavior, and which will only benefit with a prompt diagnosis and intensive multidisciplinary treatment.
A 65 years old Hispanic male with right upper quadrant abdominal pain and upper gastrointestinal bleeding characterized by intermittent melena.
Palpable right upper quadrant abdominal mass extending up to 4 cm below the costal margin.
Primary neoplasm arising from a retroperitoneal structure (pancreas, adrenal glands, kidneys and duodenum), lymphoma.
All labs were within normal limits except for chronic moderate anemia.
CT scan showed an infiltrative lesion in duodenum and gallbladder affecting the splenic, hepatic and mesenteric vascularity.
Endoscopy showed a 2 cm opening from the posterior duodenal wall communicating with a solid retroperitoneal mass, irregular, indurated and extremely friable measuring more than 10 cm in diameter.
Retroperitoneal epithelioid sarcoma (ES) positive for cytokeratin and vimentin.
Palliative surgery, a gastro-jejunal anastomosis.
Epitheliod sarcoma is a malign entity with distal and proximal forms. The proximal form arising in the deep part of the pelvis, perineum and genital tract or retroperitoneum has been very rarely reported.
ES is a rare malignant mesenchymatous tumor more frequently found in young patients from 23 to 40 years old. Usually divided in proximal and distal presentation, with predominant topography on distal zones such as upper extremities, mainly fingers, hands and wrists. The proximal form originates in the deep part of the pelvis, perineum and genital tract. It presents large epithelioid carcinoma-like cells and has a more aggressive clinical course than the distal presentation.
Retroperitonal ES is an extremely rare pathology, the duodenal perforation allowed the passage of a videoendoscope providing a very unusual and direct endoscopic view of the neoformation.
The authors describe a rare and an interesting case of ES.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Mexico
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): D, D
Grade E (Poor): 0
P- Reviewer: Cui J, Ikeuchi N, Mais V, Vynios D, Zhu YL S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Enzinger FM. Epihtelioid sarcoma: a sarcoma simulating a granuloma or a carcinoma. Cancer. 1970;26:1029-1041. [DOI] [Full Text] |
| 2. | Wolf PS, Flum DR, Tanas MR, Rubin BP, Mann GN. Epithelioid sarcoma: the University of Washington experience. Am J Surg. 2008;196:407-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 46] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 3. | Han CH, Li X, Khanna N. Epithelioid sarcoma of the vulva and its clinical implication: A case report and review of the literature. Gynecol Oncol Rep. 2016;15:31-33. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 4. | Chbani L, Guillou L, Terrier P, Decouvelaere AV, Grégoire F, Terrier-Lacombe MJ, Ranchère D, Robin YM, Collin F, Fréneaux P. Epithelioid sarcoma: a clinicopathologic and immunohistochemical analysis of 106 cases from the French sarcoma group. Am J Clin Pathol. 2009;131:222-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 120] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 5. | Kim HJ, Kim MH, Kwon J, Kim JY, Park K, Ro JY. Proximal-type epithelioid sarcoma of the vulva with INI1 diagnostic utility. Ann Diagn Pathol. 2012;16:411-415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | Deyrup AT, Weiss SW. Grading of soft tissue sarcomas: the challenge of providing precise information in an imprecise world. Histopathology. 2006;48:42-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 79] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 7. | Manzanares-Campillo MC, Mu-oz V, Sánchez Susana, Gil A, Jara A. Martin J. Sarcoma epitelioide de tipo proximal en pubis. Cir Cir. 2011;79:560-563. |
| 8. | Ross HM, Lewis JJ, Woodruff JM, Brennan MF. Epithelioid sarcoma: clinical behavior and prognostic factors of survival. Ann Surg Oncol. 1997;4:491-495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 85] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 9. | Herr MJ, Harmsen WS, Amadio PC, Scully SP. Epithelioid sarcoma of the hand. Clin Orthop Relat Res. 2005;2005:193-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 36] [Article Influence: 1.8] [Reference Citation Analysis (0)] |