Published online Jan 16, 2017. doi: 10.4253/wjge.v9.i1.12
Peer-review started: June 24, 2016
First decision: August 10, 2016
Revised: August 25, 2016
Accepted: November 1, 2016
Article in press: November 3, 2016
Published online: January 16, 2017
Processing time: 193 Days and 9.8 Hours
To investigate endoscopic therapy efficacy for refractory benign biliary strictures (BBS) with multiple biliary stenting and clarify predictors.
Ten consecutive patients with stones in the pancreatic head and BBS due to chronic pancreatitis who underwent endoscopic therapy were evaluated. Endoscopic insertion of a single stent failed in all patients. We used plastic stents (7F, 8.5F, and 10F) and increased stents at intervals of 2 or 3 mo. Stents were removed approximately 1 year after initial stenting. BBS and common bile duct (CBD) diameter were evaluated using cholangiography. Patients were followed for ≥ 6 mo after therapy, interviewed for cholestasis symptoms, and underwent liver function testing every visit. Patients with complete and incomplete stricture dilations were compared.
Endoscopic therapy was completed in 8 (80%) patients, whereas 2 (20%) patients could not continue therapy because of severe acute cholangitis and abdominal abscess, respectively. The mean number of stents was 4.1 ± 1.2. In two (20%) patients, BBS did not improve; thus, a biliary stent was inserted. BBS improved in six (60%) patients. CBD diameter improved more significantly in the complete group than in the incomplete group (6.1 ± 1.8 mm vs 13.7 ± 2.2 mm, respectively, P = 0.010). Stricture length was significantly associated with complete stricture dilation (complete group; 20.5 ± 3.0 mm, incomplete group; 29.0 ± 5.1 mm, P = 0.011). Acute cholangitis did not recur during the mean follow-up period of 20.6 ± 7.3 mo.
Sequential endoscopic insertion of multiple stents is effective for refractory BBS caused by chronic calcifying pancreatitis. BBS length calculation can improve patient selection procedure for therapy.
Core tip: Endoscopic biliary stenting for benign biliary strictures (BBS) is useful for symptom relief and less invasive than surgery. Therefore, BBS caused by chronic pancreatitis (CP) is often managed by biliary stenting. However, subsequent treatment for refractory BBS caused by CP is unclear and no predictive factors for therapeutic success have been defined. The results of the present study indicated that endoscopic therapy with multiple biliary stenting was effective against the refractory BBS caused by chronic calcifying pancreatitis. Moreover, our study indicated that stricture length was correlated with therapeutic outcome.
- Citation: Ohyama H, Mikata R, Ishihara T, Sakai Y, Sugiyama H, Yasui S, Tsuyuguchi T. Efficacy of multiple biliary stenting for refractory benign biliary strictures due to chronic calcifying pancreatitis. World J Gastrointest Endosc 2017; 9(1): 12-18
- URL: https://www.wjgnet.com/1948-5190/full/v9/i1/12.htm
- DOI: https://dx.doi.org/10.4253/wjge.v9.i1.12
Chronic pancreatitis (CP) is characterized by progressive inflammation of the pancreas, which leads to permanent damage of pancreatic structure, function, or both, resulting in episodic or intractable abdominal pain with progressive exocrine and endocrine insufficiency[1]. Inflammation associated with CP occurs in 2.7% to 45.6% of cases and leads to stricture formation in the common bile duct (CBD)[2]. The stasis of bile caused by strictures increases intraluminal pressure in the CBD and induces cholangitis, choledocholithiasis, and secondary biliary cirrhosis[2,3]. Therefore, to reduce CBD pressure, biliary dilation for benign biliary stricture (BBS) should be attempted, while pressure increase as a result of CP can be managed by surgery or endoscopic therapy.
Nealon et al[4] reported that surgical intervention offered a definitive solution for BBS, but was associated with significant morbidity and mortality. Endoscopic biliary dilation by endoscopic retrograde cholangiopancreatography (ERCP) is less invasive than surgery and is the most successful option for patients who are not candidates for surgery[5-7]. Thus, the European Society of Gastrointestinal Endoscopy (ESGE) has recommended endoscopic therapy as a useful therapeutic approach for BBS[8].
A previous study reported the effectiveness of endoscopic therapy with a single stent for BBS due to CP[9]. By comparing single vs multiple simultaneous biliary stenting for treatment of strictures, use of multiple stents appeared to be superior to use of a single stent[10]. Other studies suggest that sequential endoscopic insertion of multiple biliary stents leads to medium and long-term success of stricture dilation[11,12]. Patients with calcifications of the pancreatic head were identified as a group nonresponsive to endoscopic single stent insertion[9] and BBS with pancreatic stones was reported as intractable to therapy with multiple biliary stenting[12]. However, the efficacy of multiple biliary stenting for patients with pancreatic stones has not been investigated in detail and predictive factors of therapeutic success remain undefined. The aim of this study was to assess the usefulness of endoscopic therapy for refractory BBS as a result of chronic calcifying pancreatitis with multiple biliary stenting, and to clarify predictors.
From November 2012 to April 2014, 50 patients with CP visited at the Chiba University Hospital. Of these 50 patients, ten consecutive patients for whom endoscopic therapy with a single stent was unsuccessful were evaluated. Patients aged < 20 years and with a diagnosis of malignant diseases, existence of coagulopathy, a history of biliary surgery, inability to provide informed consent, or medical contraindications for multiple biliary stenting were excluded from the study. Patients were followed after therapy and interviewed for symptoms of cholestasis. Biochemical testing of liver function was performed at each visit. Written informed consent was obtained from all patients who underwent endoscopic therapy. The study protocol was approved by the institutional review board of Chiba University.
Side-viewing duodenoscopes (JF-240/260V, TJF-260V; Olympus Medical Systems, Tokyo, Japan) were used to perform all endoscopic procedures. Endoscopic sphincterotomy was performed for all patients. After insertion of a catheter into the CBD, the existence of a BBS was evaluated and the length of the stricture and CBD diameter, which was upstream of the stricture, was measured by cholangiography in all patients. A flexible guide wire was passed through the stricture and a single plastic stent was inserted beyond the stricture. Plastic stents (7F, 8.5F, and 10F) and increased stents at intervals of 2 or 3 mo were used to avoid clogging and development of cholangitis[13]. When symptoms and abnormal liver function test results following cholestasis appeared, stents or exchanged stents were inserted. All stents were removed approximately one year after initial stenting. Then, the stricture and CBD diameter were evaluated by comparisons with values before therapy.
The main study outcome was the usefulness of multiple biliary stenting for refractory BBSs for symptom relief and maintenance. Diagnosis of CP was based on clinical history and morphological abnormalities of the pancreas, as identified by computed tomography, magnetic resonance cholangiopancreatography, ERCP, and endoscopic ultrasound[14]. Diagnosis of a BBS was based on signs and symptoms of biliary obstruction and evidence of upstream biliary dilatation on imaging[15]. Symptomatic biliary obstruction was defined by clinical and laboratory findings of obstructive jaundice. The stricture was considered sufficiently dilated if there was easy passage of an 8.5 mm balloon and rapid emptying of contrast was evident fluoroscopically[12]. Accordingly, patients with complete stricture dilation were included in the complete group and those with incomplete stricture dilation were included in the incomplete group. Characteristics of the two groups were compared to identify therapeutic predictors. Patient sex, age, body mass index (BMI), etiology, history of alcohol abuse, duration of CP, treatment period, CBD diameter, length of stricture, number of pancreatic stones, pancreatic stone location, pancreatic stone diameter, number of ERCP sessions, and number of biliary stents were evaluated as potential predictors. During the follow-up period, symptom relapse was defined as the appearance of symptomatic biliary obstruction. Complications related to endoscopic therapy were recorded. The severity of these complications was defined and graded according to the consensus criteria proposed by Cotton et al[16].
The Mann-Whitney U test was used to compare continuous variables, while the Fisher’s exact test was used for comparison of categorical variables. The Wilcoxon signed-rank test was used to identify differences in the median values of proposed predictors. A probability (P) value of < 0.05 was considered statistically significant. All statistical analyses were performed using SPSS software version 20.0 (IBM-SPSS, Inc., Chicago, IL, United States).
Baseline patient characteristics, imaging findings, and interventions of all patients enrolled in this study are summarized in Table 1. ERCP procedures were tolerated in all patients. The mean number of biliary stents was 4.1 ± 1.2. Completion of endoscopic therapy was achieved in eight (80.0%) patients. Complete stricture dilation after therapy was achieved in six (60.0%) patients. BBS was not improved in two (20%) patients, thus biliary stents were inserted. CBD diameter was significantly improved after therapy (before therapy; 12.5 ± 2.7 mm, after therapy; 8.7 ± 3.9 mm, P = 0.022).
| Variable | Value |
| Patient characteristics | |
| Sex, n (%) | |
| Male | 10 (100.0) |
| Female | 0 (0.0) |
| Age, mean ± SD, yr | 56.9 ± 6.9 |
| BMI, mean ± SD, kg/m2 | 19.2 ± 2.6 |
| Etiology, n (%) | |
| Alcohol | 9 (90.0) |
| Other | 1 (10.0) |
| Alcohol abuse, n (%) | |
| Presence | 8 (80.0) |
| Absence | 2 (20.0) |
| Duration of CP, mean ± SD, mo | 106.4 ± 72.4 |
| Treatment period, mean ± SD, d | 350.6 ± 61.0 |
| Follow up period, mean ± SD, mo (complete group) | 20.6 ± 7.3 |
| Imaging findings | |
| CBD diameter, mean ± SD, mm | 12.5 ± 2.7 |
| Length of stricture, mean ± SD, mm | 23.9 ± 5.7 |
| No. of pancreatic stones, n (%) | |
| Single | 5 (50.0) |
| Multiple | 5 (50.0) |
| Pancreatic stone location, n (%) | |
| Head | 10 (100.0) |
| Body + Tail | 0 (0.0) |
| Pancreatic stone diameter, mean ± SD, mm | 10.2 ± 5.5 |
| Interventions | |
| No. of ERCP sessions, mean ± SD | 4.5 ± 1.0 |
| No. of stents, mean ± SD | 4.1 ± 1.2 |
| Dilation of CBD stricture, n (%) | |
| Presence | 0 (0.0) |
| Absence | 10 (100.0) |
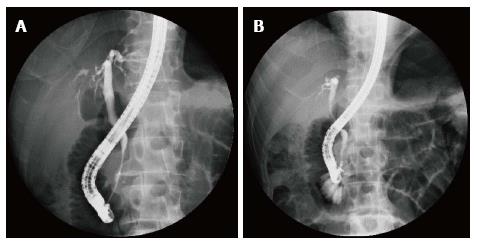
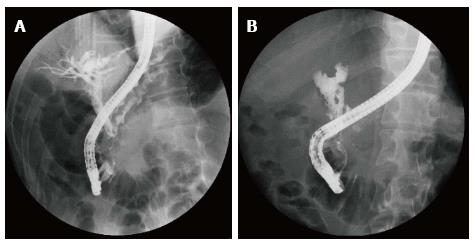
All patients were male and had pancreatic stones in the pancreatic head. Therefore, patient sex and pancreatic stone location were excluded from analysis of therapeutic outcome predictors. Patients’ age, BMI, etiology history of alcohol abuse, duration of CP, treatment period, number of pancreatic stones, pancreatic stone diameter, number of ERCP sessions, and number of biliary stents were similar in complete and incomplete groups. CBD diameter improvement was more significant in the complete group than the incomplete group (6.1 ± 1.8 mm vs 13.7 ± 2.2 mm, respectively, P = 0.010). Furthermore, only the stricture length was significantly associated with complete stricture dilation (complete group; 20.5 ± 3.0 mm, incomplete group; 29.0 ± 5.1 mm, P = 0.011) (Table 2). Successful results were obtained only in patients with a stricture length of less than 24.0 mm (Table 3, Figures 1 and 2).
| Variable | Complete (n = 6) | Incomplete (n = 4) | P value |
| Patient characteristics | |||
| Sex, n (%) | |||
| Male | 6 (100.0) | 4 (100.0) | |
| Female | 0 (0.0) | 0 (0.0) | |
| Age, mean ± SD, yr | 58.8 ± 8.2 | 54.0 ± 3.4 | 0.61 |
| BMI, mean ± SD, kg/m2 | 18.0 ± 1.7 | 20.6 ± 3.1 | 0.114 |
| Etiology, n (%) | 0.6 | ||
| Alcohol | 5 (83.3) | 4 (100.0) | |
| Other | 1 (16.7) | 0 (0.0) | |
| Alcohol abuse, n (%) | 0.667 | ||
| Presence | 1 (16.7) | 1 (25.0) | |
| Absence | 5 (83.3) | 3 (75.0) | |
| Duration of CP, mean ± SD, mo | 83.7 ± 79.4 | 140.5 ± 51.4 | 0.257 |
| Treatment period, mean ± SD, d | 384.5 ± 16.4 | 299.8 ± 70.6 | 0.171 |
| Imaging findings | |||
| CBD diameter before therapy, mean ± SD, mm | 12.4 ± 2.3 | 12.8 ± 3.7 | 0.762 |
| Length of stricture, mean ± SD, mm | 20.5 ± 3.0 | 29.0 ± 5.1 | 0.011 |
| No. of pancreatic stones, n (%) | 0.738 | ||
| Single | 3 (50.0) | 2 (50.0) | |
| Multiple | 3 (50.0) | 2 (50.0) | |
| Pancreatic stone location, n (%) | |||
| Head | 6 (100.0) | 4 (100.0) | |
| Body + Tail | 0 (0.0) | 0 (0.0) | |
| Pancreatic stone diameter, mean ± SD, mm | 7.4 ± 3.7 | 14.2 ± 6.2 | 0.067 |
| Interventions | |||
| No. of ERCP sessions, mean ± SD | 4.5 ± 0.8 | 4.5 ± 1.3 | > 0.999 |
| No. of biliary stents, mean ± SD | 4.0 ± 0.9 | 4.3 ± 1.7 | 0.767 |
| Patient No. | Length of stricture (mm) | Outcomes of stricture dilation |
| 1 | 23.2 | Complete |
| 2 | 20.7 | Complete |
| 3 | 19.3 | Complete |
| 4 | 36 | Incomplete |
| 5 | 20.4 | Complete |
| 6 | 24.9 | Incomplete |
| 7 | 29.4 | Incomplete |
| 8 | 25.5 | Incomplete |
| 9 | 24 | Complete |
| 10 | 15.5 | Complete |
All six patients who achieved complete stricture dilation at least 6 mo after therapy were followed-up for a mean period of 20.6 ± 7.3 mo. During the follow-up period, there was no incidence of recurrence of symptomatic biliary obstruction.
Endoscopic therapy could not be completed in two (20%) patients because of acute cholangitis and abdominal abscess, respectively. Therefore, each underwent endoscopic biliary stenting and both recovered following conservative therapy. There were no complications related to ERCP. No instance of severe complication or patient death was noted during the follow-up period.
BBS formation is a common complication from either hepato-biliary surgery or diseases, such as CP and primary sclerosing cholangitis, among others[17]. BBS complicates the course of CP in 3% to 23% of patients[18]. BBS causes cholestasis that frequently results in cholangitis. Therefore, endoscopic therapy or surgery for BBS should be attempted. A postoperative BBS is managed with endoscopic therapy, which can improve long-term and very long-term results[12,19,20]. According to the ESGE guidelines, if endoscopic therapy is selected for BBS caused by CP, temporary (one-year) placement of multiple, side-by-side, plastic biliary stents is recommended[8]. Therefore, many patients with BBS caused by CP are managed with multiple biliary stenting. However, Draganov et al[12] reported that endoscopic therapy for these patients tended to be more unsuccessful than for patients with postoperative stricture and the results are worse for those with pancreatic stones. This study aimed to evaluate the efficacy of endoscopic therapy for refractory BBS caused by chronic calcifying pancreatitis with multiple biliary stenting and to clarify predictors of therapeutic success.
Alcohol is the most common cause of CP in Japan[21] and is regarded as the leading cause of CP in Western countries[14]. Disease in patients with alcoholic CP often progresses to pancreatic degeneration and pancreatic stone formation occurs more rapidly than in those with idiopathic CP[22]. Moreover, patient compliance tends to be poor[8]. Our study had a relatively larger proportion of patients with alcoholic CP (90.0%) than reported in previous studies (54.1%-69.0%)[6,9]. Since all patients in our study had refractory BBS, those with alcoholic CP were likely the majority. Although alcoholic CP mainly affects men[14], prognosis of all patients in this study might be generally consistent with that of males.
Biliary stenting was routinely exchanged every 3 mo to avoid clogging and resulting cholangitis based on a study by Dumonceau et al[8] and supported by findings of Greiner’s group[13,23]. Besides, the ESGE recommends temporary (one-year) placement of multiple, side-by-side, plastic biliary stents. In our study, the mean number of biliary stents was 4.1 ± 1.2 and the mean number of ERCP sessions was 4.5 ± 1.0, similar to those reported in previous studies[5,6,10-12,19,24].
Patients with BBS caused by CP were previously treated by single stent insertion to dilate the stricture, according to the recommendations of Kahl et al[9]. Endoscopic therapy was successful for some patients, especially those with a short BBS length. Although the presence of calcification in the pancreatic head and stricture location according to the Bismuth classification was used to predict complete stricture dilation in previous studies[9,12], no report has investigated the relevance of BBS length. Therefore, we evaluated the impact of BBS length on treatment outcome and found that BBS length was indeed a prognostic factor for procedural success. Calculation of BBS length improves the patient selection procedure for therapy. Although it is important to select patients who are likely to achieve favorable outcomes with complete stricture dilation, alternative therapies, including surgery, and avoidance of repetitive therapies could improve the quality of life of others.
In this study, complete stricture dilation was observed in 60% of patients, consistent with previous studies (44%-92%)[6,10-12]. The results suggest that multiple biliary stenting is a useful procedure for treatment of refractory BBS.
Complications were observed in two (20.0%) patients: one developed cholangitis and the other an abdominal abscess. Both recovered by conservative therapy and biliary stent insertion. Moreover, the frequency of these findings was comparable with other reports[6,9,10,12].
In our study, the sample size was small and the patients were all male. In addition, this study was investigated by a single center. Additional multicenter studies with large number of patients involving both male and female patient population are needed to confirm our study.
In conclusion, the results of the present study indicated that endoscopic therapy with multiple biliary stenting was effective against refractory BBS caused by chronic calcifying pancreatitis. Moreover, the stricture length was correlated with therapeutic outcomes. A stricture length of < 24.0 mm is a predictor of good prognosis of complete stricture dilation. Therefore, the use of this threshold could help in the planning of alternative therapeutic options for patients for whom incomplete stricture dilation is likely.
The authors would like to thank Enago (https://www.enago.jp/) for the English language review.
To reduce common bile duct (CBD) pressure, biliary dilation for benign biliary stricture (BBS) is often attempted by endoscopic therapy with multiple biliary stenting. However, the efficacy of multiple biliary stenting for patients with pancreatic stones has not been investigated in detail and predictive factors of therapeutic success remain undefined.
Identifying predictors of good prognosis of complete stricture dilation may help in the planning of alternative therapeutic options for patients for whom incomplete stricture dilation is likely.
Endoscopic therapy with multiple biliary stenting was effective against refractory BBS caused by chronic calcifying pancreatitis. Moreover, the stricture length was correlated with therapeutic outcomes.
This study suggests that calculation of BBS length improves the patient selection procedure for therapy.
BBS refers to benign biliary stricture. Inflammation associated with chronic pancreatitis leads to stricture formation in the CBD. The stasis of bile caused by BBS induces cholangitis, choledocholithiasis, and secondary biliary cirrhosis.
This is a meaningful and innovative manuscript based on endoscopic retrograde cholangiopancreatography stenting and BBS therapy. This is an interesting cohort study with small group of patients. However, the data presented is important in identifying a large cohort group involving both male and female patient population in future studies. The studies including the patient selection has been carefully performed. Data analysis was performed carefully and could have been improved with a larger cohort.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Chowdhury P, Yin HK S- Editor: Gong ZM L- Editor: A E- Editor: Lu YJ
| 1. | Mitchell RM, Byrne MF, Baillie J. Pancreatitis. Lancet. 2003;361:1447-1455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 2. | Delhaye M, Matos C, Devière J. Endoscopic management of chronic pancreatitis. Gastrointest Endosc Clin N Am. 2003;13:717-742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 42] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 3. | Ng C, Huibregtse K. The role of endoscopic therapy in chronic pancreatitis-induced common bile duct strictures. Gastrointest Endosc Clin N Am. 1998;8:181-193. [PubMed] |
| 4. | Nealon WH, Urrutia F. Long-term follow-up after bilioenteric anastomosis for benign bile duct stricture. Ann Surg. 1996;223:639-645; discussion 645-648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 59] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 5. | Dumonceau JM, Macias-Gomez C. Endoscopic management of complications of chronic pancreatitis. World J Gastroenterol. 2013;19:7308-7315. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 21] [Cited by in RCA: 21] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Regimbeau JM, Fuks D, Bartoli E, Fumery M, Hanes A, Yzet T, Delcenserie R. A comparative study of surgery and endoscopy for the treatment of bile duct stricture in patients with chronic pancreatitis. Surg Endosc. 2012;26:2902-2908. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 21] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 7. | Smits ME, Rauws EA, van Gulik TM, Gouma DJ, Tytgat GN, Huibregtse K. Long-term results of endoscopic stenting and surgical drainage for biliary stricture due to chronic pancreatitis. Br J Surg. 1996;83:764-768. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 94] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 8. | Dumonceau JM, Delhaye M, Tringali A, Dominguez-Munoz JE, Poley JW, Arvanitaki M, Costamagna G, Costea F, Devière J, Eisendrath P. Endoscopic treatment of chronic pancreatitis: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2012;44:784-800. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 203] [Cited by in RCA: 188] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 9. | Kahl S, Zimmermann S, Genz I, Glasbrenner B, Pross M, Schulz HU, Mc Namara D, Schmidt U, Malfertheiner P. Risk factors for failure of endoscopic stenting of biliary strictures in chronic pancreatitis: a prospective follow-up study. Am J Gastroenterol. 2003;98:2448-2453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 91] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 10. | Catalano MF, Linder JD, George S, Alcocer E, Geenen JE. Treatment of symptomatic distal common bile duct stenosis secondary to chronic pancreatitis: comparison of single vs. multiple simultaneous stents. Gastrointest Endosc. 2004;60:945-952. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 118] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 11. | Pozsár J, Sahin P, László F, Forró G, Topa L. Medium-term results of endoscopic treatment of common bile duct strictures in chronic calcifying pancreatitis with increasing numbers of stents. J Clin Gastroenterol. 2004;38:118-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 55] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 12. | Draganov P, Hoffman B, Marsh W, Cotton P, Cunningham J. Long-term outcome in patients with benign biliary strictures treated endoscopically with multiple stents. Gastrointest Endosc. 2002;55:680-686. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 217] [Cited by in RCA: 162] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 13. | Hoffman BJ, Marsh WH, Cunningham JT. Periodic exchange of biliary stents. Gastrointest Endosc. 1995;41:267-268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 14. | Braganza JM, Lee SH, McCloy RF, McMahon MJ. Chronic pancreatitis. Lancet. 2011;377:1184-1197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 373] [Cited by in RCA: 343] [Article Influence: 24.5] [Reference Citation Analysis (0)] |
| 15. | Rustagi T, Jamidar PA. Endoscopic management of benign biliary strictures. Curr Gastroenterol Rep. 2015;17:422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Cotton PB, Eisen GM, Aabakken L, Baron TH, Hutter MM, Jacobson BC, Mergener K, Nemcek A, Petersen BT, Petrini JL. A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc. 2010;71:446-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1238] [Cited by in RCA: 1842] [Article Influence: 122.8] [Reference Citation Analysis (1)] |
| 17. | Kaffes AJ. Management of benign biliary strictures: current status and perspective. J Hepatobiliary Pancreat Sci. 2015;22:657-663. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 18. | Abdallah AA, Krige JE, Bornman PC. Biliary tract obstruction in chronic pancreatitis. HPB (Oxford). 2007;9:421-428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 95] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 19. | Costamagna G, Pandolfi M, Mutignani M, Spada C, Perri V. Long-term results of endoscopic management of postoperative bile duct strictures with increasing numbers of stents. Gastrointest Endosc. 2001;54:162-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 299] [Cited by in RCA: 269] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 20. | Costamagna G, Tringali A, Mutignani M, Perri V, Spada C, Pandolfi M, Galasso D. Endotherapy of postoperative biliary strictures with multiple stents: results after more than 10 years of follow-up. Gastrointest Endosc. 2010;72:551-557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 94] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 21. | Hirota M, Shimosegawa T, Masamune A, Kikuta K, Kume K, Hamada S, Kanno A, Kimura K, Tsuji I, Kuriyama S. The seventh nationwide epidemiological survey for chronic pancreatitis in Japan: clinical significance of smoking habit in Japanese patients. Pancreatology. 2014;14:490-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 71] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 22. | Nagata A, Homma T, Tamai K, Ueno K, Shimakura K, Oguchi H, Furuta S, Oda M. A study of chronic pancreatitis by serial endoscopic pancreatography. Gastroenterology. 1981;81:884-891. [PubMed] |
| 23. | Weickert U, Venzke T, König J, Janssen J, Remberger K, Greiner L. Why do bilioduodenal plastic stents become occluded? A clinical and pathological investigation on 100 consecutive patients. Endoscopy. 2001;33:786-790. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 65] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 24. | Baron TH, Davee T. Endoscopic management of benign bile duct strictures. Gastrointest Endosc Clin N Am. 2013;23:295-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 2.8] [Reference Citation Analysis (0)] |