Published online Mar 25, 2016. doi: 10.4253/wjge.v8.i6.288
Peer-review started: October 27, 2015
First decision: December 11, 2015
Revised: December 21, 2015
Accepted: January 16, 2016
Article in press: January 19, 2016
Published online: March 25, 2016
Processing time: 147 Days and 17.7 Hours
AIM: To identify the cut-off value for predicting the ability of elderly patients with dysphagia to swallow pureed diets using a new endoscopy scoring method.
METHODS: Endoscopic swallowing evaluation of pureed diets were done in patients ≥ 65 years with dysphagia. The Hyodo-Komagane score for endoscopic swallowing evaluation is expressed as the sum (0-12) of four degrees (0-3) with four parameters: (1) salivary pooling in the vallecula and piriform sinuses; (2) the response of glottal closure reflex induced by touching the epiglottis with the endoscope; (3) the location of the bolus at the time of swallow onset assessed by “white-out” following swallowing of test jelly; and (4) pharyngeal clearance after swallowing of test jelly. We used receiver operating characteristic (ROC) curve analysis to retrospectively analyze the association between the total score and successful oral intake of pureed diets.
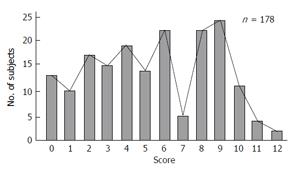
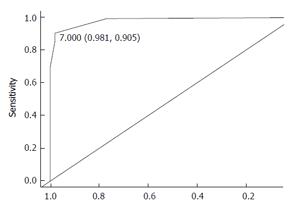
RESULTS: One hundred and seventy-eight patients were enrolled including 113 men (63%), mean age 83 years (range, 66-98). One hundred and twenty-six patients (71%) were able to eat pureed diets during the observation period (mean ± SD, 19 ± 14 d). In ROC analysis, the cut-off value of the score for eating the pureed diets was 7 (sensitivity = 0.98; specificity = 0.91).
CONCLUSION: The Hyodo-Komagane endoscopic score is useful to predict the ability to eat pureed diets in elderly patients with dysphagia.
Core tip: Predicting successful oral intake in elderly patients with dysphagia remains a challenge. The scoring method for endoscopic swallowing evaluation was based on final score (from 0 to 12) using four parameters; (1) the salivary pooling in the vallecula and piriform sinuses; (2) the response of glottal closure reflex induced by touching the epiglottis with the endoscope; (3) the location of the bolus at the time of swallow onset assessed by “white-out” after the swallowing of test jelly; and (4) the extent of pharyngeal clearance after test jelly is swallowed. A total score of 7 or less during endoscopic swallowing evaluation reliably predicted the ability to eat pureed diets.
- Citation: Sakamoto T, Horiuchi A, Makino T, Kajiyama M, Tanaka N, Hyodo M. Determination of the cut-off score of an endoscopic scoring method to predict whether elderly patients with dysphagia can eat pureed diets. World J Gastrointest Endosc 2016; 8(6): 288-294
- URL: https://www.wjgnet.com/1948-5190/full/v8/i6/288.htm
- DOI: https://dx.doi.org/10.4253/wjge.v8.i6.288
With aging of the population, dysphagia is becoming an important medical and social issue[1]. Pneumonia is the fourth most common cause of mortality in the elderly in Japan; the majority of cases in hospital-acquired pneumonia are reported to be related to aspiration[2]. Pureed diets are often used as an initial dysphagia diet for patients with moderate to severe dysphagia because, if the dysphagic patients can fulfill their nutritional requirements by eating pureed diets, they can avoid enteral feeding using a percutaneous endoscopic gastrostomy (PEG) tube. Wilkinson et al[3] previously reported PEG should be considered for people unable to tolerate a pureed diet 14 d after their stroke despite the fact that half will recover sufficiently to manage oral intake. They suggested that the texture of the pureed diet is likely to be most useful factor predictive of the need for PEG. No methods for predicting successful oral intake of pureed diets in elderly patients with dysphagia have been established.
Endoscopic and videofluoroscopic examinations are often used to evaluate swallowing and to quantify the risk of aspiration[4-7]. Our facility uses a team approach that includes a gastroenterologist and a speech therapist. Swallowing is evaluated by endoscopy using an endoscope normally used for transnasal esophagogastroduodenoscopy. We previously used this approach to study factors that influenced swallowing of pureed diets[8]. Saliva pooling and pharyngeal residues of pureed foods were shown to predict impaired swallowing of pureed foods. However, endoscopic determination of whether patients could swallow pureed diets was not always reproducible or safe especially for severely dysphagic patients. Irreproducibility was possibly related to variability in the texture and physical characteristics of the pureed diet despite being prepared in the same facility.
We previously developed a scoring system for endoscopic swallowing evaluation using blue-dyed water[9]. We modified the test meal to contain a test jelly instead of blue-dyed water so that elderly patients with severe dysphagia could undergo endoscopic examination of swallowing safely even unable to swallow pureed diets and the data would be reproducible. The aim of this study was to validate the revised scoring system to predict the ability to eat pureed diets in elderly patients with dysphagia.
From January 2012 to November 2014, 205 hospitalized patients who underwent endoscopic swallowing evaluation at Showa Inan General Hospital, a municipal local hospital, were consecutively enrolled. We included dysphagia patients able to sit in a chair or up in bed with assistance and whose oral intake had been observed at least for 5 d after endoscopic swallowing evaluation. Subjects were included irrespective of whether oral intake of dysphagic diets was successful or unsuccessful. Exclusion criteria included an age less than 65 years old or the presence of an acute infection.
Verbal and written informed consent for the endoscopic examination of swallowing was obtained from all patients. Gastroenterologists, who were experienced in transnasal esophagogastroduodenoscopy and PEG, performed the endoscopic swallowing evaluation along with a speech therapist. Results of endoscopic swallowing examination including the new scoring system (Hyodo-Komagane score) were recorded in the endoscopic database. Determination of the validity of the proposed endoscopic swallowing score was based on a retrospective review of the patients’ charts with special attention to the Hyodo-Komagane score and the status of oral intake of diets. This retrospective analysis was approved by the ethics committee of Showa Inan General Hospital.
Participants underwent the endoscopic swallowing evaluation while sitting in a chair or sitting up in bed. Two minutes prior to inserting the endoscope, 0.2-0.5 mL of 4% lidocaine was applied to the nasal cavities of each participant using a nasal splay. An endoscope (GIF-XP260N, Olympus, Tokyo, Japan) was used for endoscopic swallowing evaluations. This is a forward-viewing upper gastrointestinal videoscope with an ultra-miniature, resolution charged-coupled device with a 120 degree field of view. The insertion diameter is 5.5 mm and the videoscope has a tip deflection capability of 210/120 up/down in a single plane. The lubricated endoscope was passed transnasally, typically on the floor of the nose, to obtain a superior view of the hypopharynx. The endoscope was moved throughout the study between swallowing and post-swallow positions to collect the data as described previously[8]. Images of the oropharynx, hypopharynx and larynx were displayed on a monitor and recorded on the digital video recorder (Sony EVO-550H, Tokyo, Japan).
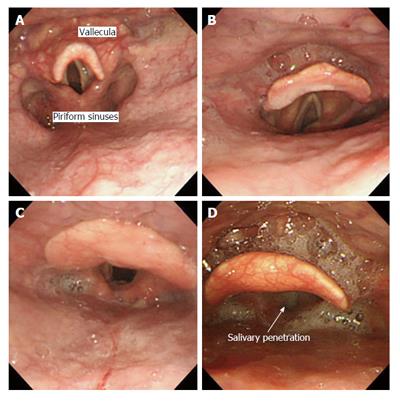
All patients underwent endoscopic swallowing evaluation at least once prior to starting oral intake. First, salivary pooling in the vallecula and piriform sinuses was evaluated. The response of the glottal closure reflex was also evaluated by touching the epiglottis with the tip of endoscope. When glottal closure reflex was not elicited by touching the epiglottis, the result was confirmed by attempting to touch the epiglottis with the endoscope at least three times before absence of glottal closure reflex was declared. The swallowing trial was then performed following ingestion of a 3 mL of test diet contained in a spoon. The interior larynx and airway were examined before and after each swallow for the presence of food within the laryngeal vestibule and/or aspiration of test materials below the true vocal folds. Silent aspiration, defined as lack of cough or gag reflex when the test materials passed into the trachea, was also noted.
This scoring system was based on our previously clinic-based scoring for endoscopic swallowing evaluation using a blue-dyed water test meal[9]. Table 1 shows the modified scoring method that consists of four parameters: (1) salivary pooling in the vallecula and piriform sinuses (Figure 1); (2) the response of glottal closure reflex induced by touching the epiglottis with the tip of the endoscope; (3) the location of the bolus at the time of swallow onset assessed by “white-out” following swallowing of test jelly; and (4) the extent of pharyngeal clearance after swallowing of test jelly. The four parameters above are scored using a 4 point scale of 0 to 3 (Table 1). The final Hyodo-Komagane score is expressed as the total score (0 to 12) of the four parameters. All patients for whom the endoscopic swallowing evaluation was performed during the time period of the study had the score recorded in the clinical chart.
| A: Salivary pooling in vallecula and piriform sinuses | |
| 0 | No pooling |
| 1 | Pooling at the only vallecula |
| 2 | Pooling in vallecula and piriform sinuses and no penetration1 into larynx |
| 3 | Pooling in vallecula and piriform sinuses and penetration into larynx |
| B: The response of glottal closure reflex induced by touching the epiglottis with the endoscope | |
| 0 | Marked reflex by one touching |
| 1 | Slow and/or weak reflex by one touching |
| 2 | Reflex by two or three touchings |
| 3 | No refex despite three touchings |
| C: The location of the bolus at the time of swallow onset assessed by "white-out"2 following swallowing of test jelly | |
| 0 | Pharyngeal |
| 1 | Vallecula |
| 2 | Piriform sinuses |
| 3 | No swallowing |
| D: The extent of pharyngeal clearance after swallowing of test jelly | |
| 0 | No residues |
| 1 | Pharyngeal residues remain, but are absent after swallowing is attempted two or three times |
| 2 | Pharyngeal residues remain, but do not penetrate into larynx |
| 3 | Pharyngeal residues remain and penetrate into larynx |
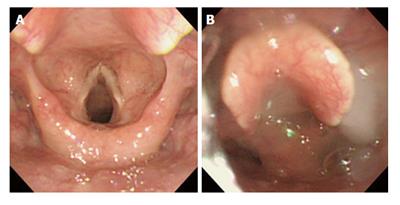
Test jelly, that is gelatin jelly (Isotonic jelly®, Nutri Co., Ltd., Yokkaichi, Japan) is shown in Figure 2. The characteristics were as follows: Hardness, 5000 N/m2; cohesiveness, 0.4; adhesiveness, 89 J/m3. The swallowing of test jelly was attempted for all subjects who underwent endoscopic swallowing evaluation. When the test jelly was absent from pharyngeal cavity after swallowing was attempted two or three times, swallowing of test jelly was regarded as successful. If swallowing of the test jelly was successful, swallowing of a semi-solid diet (Elental® jelly, Ajinomoto Pharmaceutical Co., Tokyo, Japan) and pureed diets was attempted.
The semi-solid diet (Elental® jelly) was made by adding a thickening agent (Jelly mix®, Ajinomoto Pharmaceutical Co.) which contained 11.7% agar, sugar, stabilizer, and other ingredients to an elemental diet, Elental®. The thickening agent (5.8 g) was dissolved with 150 mL of hot water, and 80 g of Elental® was added to the solution which was then cooled to harden. The texture characteristics were: Hardness, 17000 ± 640 N/m2; cohesiveness, 0.14 ± 0.0066; adhesiveness, 150 ± 49 J/m3.
Except for patients in whom pureed diet was noted to penetrate into the larynx after swallowing the pureed diet, feeding of pureed diets was attempted and assessed once each day by a speech therapist throughout the subjects’ hospitalization, irrespective of Hyodo-Komagane score. When patients were able to eat sufficient pureed diet to meet their daily nutritional requirements for at least 5 d, they were judged to be able to be managed with pureed diets. Dysphagia diets at next higher level were then attempted at the discretion of the speech therapist. The status of oral intake of dysphagia diets was noted.
Sensitivity and specificity of variables were based on receiver operating characteristic (ROC) curve analysis. In a ROC curve the true positive rate (sensitivity) is plotted in function of the false positive rate (100-specificity) for different cut-off points of a parameter. Each point on the ROC curve represents a sensitivity/specificity pair corresponding to a particular decision threshold. The area under the ROC curve is a measure of how well a parameter can distinguish between two groups (successful/unsuccessful). Statistical analysis was performed by using JMP® 9.0.2 version software (SAS Institute, Inc., Japan).
One hundred and seventy-eight dysphagic subjects were included in this study. Their demographic and clinical data are shown in Table 2. There were 113 men (63%) with a mean age of 83 years (range: 66-98). Approximately 70% (124 patients) were 80 years and over. Severe comorbid diseases such as cerebrovascular disease (38%), aspiration pneumonia (32%), and neuromuscular disease (20%) were common. Patients who had developed new cerebrovascular disease, myocardial infarction, and aspiration pneumonia within two weeks were not included. Fifty-two patients had remaining pharyngeal residue seen to penetrate into the larynx after swallowing the test jelly (D-3) (Figure 3). In nine of these patients the pureed diet also penetrated into larynx. With these patients feeding trials were not attempted to avoid aspiration pneumonia. In the remaining 169 patients, swallowing trials of the pureed diet were attempted. Overall, 126 (71%) of 178 patients were able to eat pureed diets or a higher level of dysphagia diet that fulfilled their daily nutritional needs [the observation period: Mean ± SD (range), 19 ± 14 d (5-58 d)]. The remaining 43 patients were judged to fail the subsequent pureed food tests because the amount they ate was less than their daily nutritional needs.
| n (%) | |
| Gender male, female | 113 (63), 65 (37) |
| Mean age range (yr) | 83 (66-98) |
| 65-69 | 11 (6) |
| 70-79 | 43 (24) |
| 80-89 | 88 (50) |
| 90 and over | 36 (20) |
| Comorbid diseases | |
| CVD | 68 (38) |
| Aspiration pneumonia | 57 (32) |
| Neuromuscular disease | 35 (20) |
| Others | 18 (10) |
Figure 4 shows the distribution of Hyodo-Komgane scores among the 178 patients who underwent endoscopic swallowing evaluation (lower scores are better). Using ROC curve analysis of the Hyodo-Komagane scores, the area under the curve was 98.3% (95%CI: 0.097-0.996) (Figure 5). The optimal cut-off value of successful oral intake of pureed diets was a score of 7 (sensitivity = 0.98; specificity = 0.91). In 115 patients with Hyodo-Komagane scores of 7 or less only one patient was not able to maintain adequate nutritional status with pureed diets (his Hyodo-Komagane score was 6). Ten (53%) of the 19 patients whose scores were 8 were able to eat pureed diets after a rehabilitation using the semi-solid diet made from an elemental diet. Oral intake of pureed diets was unsuccessful for those with scores of 9 or higher on the Hyodo-Komagane score (Table 3). For patients who could not eat pureed diets, enteral feeding was employed.
| Score | Oral intake of pureed diets |
| 0-7 | Successful 100% |
| 81 | Successful in some cases |
| 9-12 | Unsuccessful |
No adverse events such as cardiopulmonary events or aspiration pneumonia occurred in included subjects of this study.
The aim of this study was to obtain a cut-off value of the Hyodo-Komagane score that reliably predicted the ability to eat pureed diets in elderly patients with dysphagia. The Hyodo-Komagane scoring system differs from the original Hyodo score[9] with regard to the assessment of salivary pooling in that it uses a test jelly instead of blue-dyed water as the test meal. Jelly was used because it is very difficult for severe dysphagic patients to swallow water. In addition, we previously demonstrated a low agreement in judging the presence or absence of glottal closure response as whether the reflex was elicited depended on how and whether the endoscopists actually touched the epiglottis[9]. Because it is difficult to be confident that the tip of the endoscope touches the epiglottis, we attempted to touch the epiglottis with the endoscope at least three times prior to scoring the reflex of glottal closure as absent. We speculate that this increased the reliability of making that determination and thus the Hyodo-Komagane modification of the scoring system improved both the validity and reliability of Hyodo score.
Dysphasia diets vary considerably from facility to facility. Dysphagia diets are designed to adjust food/liquid intake in terms of amount, consistency, and timing of the meal to achieve maximal nutritional intake and minimize swallowing difficulty. Traditional oral dysphagia diets typically involve a stepwise progression of bolus consistencies. A pureed diet is the basic level of swallowing for severe dysphagia patients. When dysphagia patients can swallow pureed diets, they generally do not require enteral nutrition including PEG[3,8]. The aim of this study was to develop methods to prospectively assess whether elderly patients with severe dysphagia could eat pureed diets. ROC analysis of this study suggested that the cut-off value of the Hyodo-Komagane score for eating the pureed diets is 7 (sensitivity = 0.98; specificity = 0.91) for predicting successful oral intake of pureed diets in elderly patients with dysphagia.
In the Hyodo-Komagane score the extent of pharyngeal clearance after swallowing of test jelly was regarded as important. Pharyngeal residue has consistently been identified to be greater using endoscopic evaluation of swallowing than when using videofluoroscopy[10] and penetration/aspiration was also perceived to be more severe with endoscopic evaluation of swallowing compared to videofluoroscopy images[11]. Penetration/aspiration is thought to be a clinically important variable in patients with swallowing dysfunction and is likely to be associated with an increased risk of aspiration/pneumonia. However, the agreement between the gastroenterologists regarding the presence of penetration/aspiration was found to be poor in our previous study[8]. Here, we scored penetration/aspiration only when penetration of saliva or the pharyngeal residues of test jelly into the larynx occurred. These phenomena were adopted as A-3 or D-3 in Hyodo-Komagane score.
In addition, the response of glottal closure reflex induced by touching the epiglottis with the endoscope was examined to assess the relationship between the sensory and motor components of the swallow. The relationship between laryngopharyngeal sensation and motor function has been well documented[12] and patients with impaired pharyngeal squeeze at different levels of sensory deficits are at significantly greater risk for aspiration of pureed foods compared with those with normal squeeze[13]. While the use of 0.5 mL of 4% lidocaine during endoscopic swallowing evaluation has been reported to impair swallowing ability in patients with dysphagia, this result did not achieve statistical significance and was associated with a reduction in subjective pain and discomfort[14]. A recent study confirmed that 0.2 mL of 4% lidocaine improved examination tolerability and did not impair the swallowing activity in dysphagic patients during endoscopic swallowing evaluation[15]. Therefore, we speculated that the amount (0.2-0.5 mL) of lidocaine used in this study had minimal effects on testing the sensory aspects of swallowing.
Our study has some limitations. This study was retrospective and comparative data using established competitive techniques are absent in part because there was no gold standard for detection of failure to swallow. Comparison with the other commonly used method such as with a videofluoroscopic swallowing study may provide useful comparative data in subsequent studies. Finally, all subjects were older than 65 years. It is unknown whether the prediction based on the Hyodo-Komagane endoscopic score are applicable to those less than 65 years old.
In conclusion, the modified scoring method for endoscopic swallowing evaluation was based on final score (from 0 to 12) using four parameters: (1) the salivary pooling in the vallecula and piriform sinuses; (2) the response of glottal closure reflex induced by touching the epiglottis with the endoscope; (3) the location of the bolus at the time of swallow onset assessed by “white-out” after the swallowing of test jelly; and (4) the extent of pharyngeal clearance after test jelly is swallowed. A total score of 7 or less during endoscopic swallowing evaluation reliably predicted the ability to eat pureed diets. The use of the modified scoring system appears to be a reliable method to decide whether the elderly patients can eat pureed diets or requires enteral feeding.
The authors thank David Y Graham, MD for helping with preparation of the manuscript in English.
Pureed diets are often used as an initial dysphagia diet for patients with moderate to severe dysphagia because, if the dysphagic patients can fulfill their nutritional requirements by eating pureed diets, they can avoid enteral feeding using a percutaneous endoscopic gastrostomy tube. However, no methods for predicting successful oral intake of pureed diets in elderly patients with dysphagia have been established.
The authors’ group pioneered a scoring system for endoscopic swallowing evaluation in elderly patients with dysphagia; the authors think that the method for predicting successful oral intake of pureed diets in elderly patients with dysphagia should be established and they provide support to their hypothesis with this paper, reporting that the Hyodo-Komagane endoscopic score is useful to predict the ability to eat pureed diets in elderly patients with dysphagia.
Endoscopic and videofluoroscopic examinations have been used to evaluate swallowing and to quantify the risk of aspiration. However, endoscopic determination of whether patients could swallow pureed diets was not always reproducible or safe especially for severely dysphagic patients. Irreproducibility was possibly related to variability in the texture and physical characteristics of the pureed diet despite being prepared in the same facility. This paper shows a new scoring system for endoscopic swallowing evaluation using a test jelly so that elderly patients with severe dysphagia can undergo endoscopic examination of swallowing safely even unable to swallow pureed diets; in addition, the cut-off value of the score for eating the pureed diets was defined as 7 (sensitivity = 0.98; specificity = 0.91).
Elderly patients with dysphagia will benefit from the use of Hyodo-Komagane endoscopic score which is useful to predict the ability to eat pureed diets. If evaluated with this scoring system, avoiding unfavorable enteral feeding.
When saliva or test jelly enters the glottis (opening to the trachea) and moves as far as the vestibule above the true vocal folds, this is termed as penetration; aspiration is defined when the test materials passed into the trachea below the true vocal folds. White-out is defined as the period when the videoendoscopic image is obscured owing to pharyngeal closure.
This is a nice study, well-conceived and written.
P- Reviewer: Garg P S- Editor: Qi Y L- Editor: A E- Editor: Liu SQ
| 1. | Annual Health, Labour and Welfare Report, For the Realization of a Society of Health and Longevity. Ministry of Health, Labour and Welfare, Japan, 2014. Available from: http://www.mhlw.go.jp/english/wp/wp-hw8/dl/summary.pdf. |
| 2. | Teramoto S, Fukuchi Y, Sasaki H, Sato K, Sekizawa K, Matsuse T. High incidence of aspiration pneumonia in community- and hospital-acquired pneumonia in hospitalized patients: a multicenter, prospective study in Japan. J Am Geriatr Soc. 2008;56:577-579. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 303] [Cited by in RCA: 329] [Article Influence: 19.4] [Reference Citation Analysis (1)] |
| 3. | Wilkinson TJ, Thomas K, MacGregor S, Tillard G, Wyles C, Sainsbury R. Tolerance of early diet textures as indicators of recovery from dysphagia after stroke. Dysphagia. 2002;17:227-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Langmore SE, Schatz K, Olson N. Endoscopic and videofluoroscopic evaluations of swallowing and aspiration. Ann Otol Rhinol Laryngol. 1991;100:678-681. [PubMed] |
| 5. | Kidder TM, Langmore SE, Martin BJ. Indications and techniques of endoscopy in evaluation of cervical dysphagia: comparison with radiographic techniques. Dysphagia. 1994;9:256-261. [PubMed] |
| 6. | Wu CH, Hsiao TY, Chen JC, Chang YC, Lee SY. Evaluation of swallowing safety with fiberoptic endoscope: comparison with videofluoroscopic technique. Laryngoscope. 1997;107:396-401. [PubMed] |
| 7. | Leder SB, Sasaki CT, Burrell MI. Fiberoptic endoscopic evaluation of dysphagia to identify silent aspiration. Dysphagia. 1998;13:19-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 128] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 8. | Sakamoto T, Horiuchi A, Nakayama Y. Transnasal endoscopic evaluation of swallowing: a bedside technique to evaluate ability to swallow pureed diets in elderly patients with dysphagia. Can J Gastroenterol. 2013;27:459-462. [PubMed] |
| 9. | Hyodo M, Nishikubo K, Hirose K. [New scoring proposed for endoscopic swallowing evaluation and clinical significance]. Nihon Jibiinkoka Gakkai Kaiho. 2010;113:670-678. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 46] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 10. | Kelly AM, Leslie P, Beale T, Payten C, Drinnan MJ. Fibreoptic endoscopic evaluation of swallowing and videofluoroscopy: does examination type influence perception of pharyngeal residue severity? Clin Otolaryngol. 2006;31:425-432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 132] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 11. | Kelly AM, Drinnan MJ, Leslie P. Assessing penetration and aspiration: how do videofluoroscopy and fiberoptic endoscopic evaluation of swallowing compare? Laryngoscope. 2007;117:1723-1727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 194] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 12. | Setzen M, Cohen MA, Mattucci KF, Perlman PW, Ditkoff MK. Laryngopharyngeal sensory deficits as a predictor of aspiration. Otolaryngol Head Neck Surg. 2001;124:622-624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Perlman PW, Cohen MA, Setzen M, Belafsky PC, Guss J, Mattucci KF, Ditkoff M. The risk of aspiration of pureed food as determined by flexible endoscopic evaluation of swallowing with sensory testing. Otolaryngol Head Neck Surg. 2004;130:80-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 1.4] [Reference Citation Analysis (1)] |
| 14. | Fife TA, Butler SG, Langmore SE, Lester S, Wright SC, Kemp S, Grace-Martin K, Lintzenich CR. Use of topical nasal anesthesia during flexible endoscopic evaluation of swallowing in dysphagic patients. Ann Otol Rhinol Laryngol. 2015;124:206-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 31] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 15. | O’Dea MB, Langmore SE, Krisciunas GP, Walsh M, Zanchetti LL, Scheel R, McNally E, Kaneoka AS, Guarino AJ, Butler SG. Effect of Lidocaine on Swallowing During FEES in Patients With Dysphagia. Ann Otol Rhinol Laryngol. 2015;124:537-544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 39] [Article Influence: 3.9] [Reference Citation Analysis (0)] |