Published online Jul 10, 2015. doi: 10.4253/wjge.v7.i8.830
Peer-review started: December 9, 2014
First decision: January 8, 2015
Revised: April 13, 2015
Accepted: April 27, 2015
Article in press: April 29, 2015
Published online: July 10, 2015
Processing time: 217 Days and 17.9 Hours
Indigocarmine chromoendoscopy has been proven to improve the detection of colonic lesions during screening colonoscopy, and is associated with increased adenoma detection rates. Furthermore, it is commonly used to help in the delineation and characterization of colorectal neoplasms. However, it usually requires the use of a spraying catheter that decreases the suction capacity of the endoscope, and is time- consuming. Herein, we report on the feasibility of indigo carmine chromoendoscopy during colonoscopy without using a spraying catheter, with the dye being administered through the air/water channel of the endoscope. Since the suction channel remains free, the air can be exsufflated and the staining then applies uniformly onto the colonic walls with the excess indigocarmine dye being immediately eliminated. In our experience with various types of colonoscopes and cap-assisted colonoscopy, this procedure makes indigocarmine chromoendoscopy much easier and quicker to perform, and might save the use of a spray catheter.
Core tip: We report on the feasibility of indigocarmine chromoendoscopy during colonoscopy without using a spraying catheter, with the dye being administered through the air/water channel of the endoscope.
- Citation: Barret M, Camus M, Leblanc S, Coriat R, Prat F, Chaussade S. Toward an easier indigocarmine chromoendoscopy. World J Gastrointest Endosc 2015; 7(8): 830-832
- URL: https://www.wjgnet.com/1948-5190/full/v7/i8/830.htm
- DOI: https://dx.doi.org/10.4253/wjge.v7.i8.830
Indigocarmine chromoendoscopy has proven useful in increasing the overall diagnostic yield of colonoscopy and the adenoma detection rate[1]. This technique is currently recommended in routine colorectal cancer screening in patients with long-standing inflammatory colitis or hereditary nonpolyposis colorectal cancer[2]. The standard technique implies pancolonic spraying with 0.2% indigocarmine delivered through a spraying catheter inserted in the accessory channel of the colonoscope. Spraying is performed segmentally during withdrawal of the endoscope and excess dye is suctioned before mucosal examination.
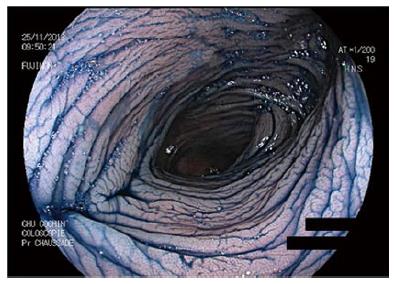
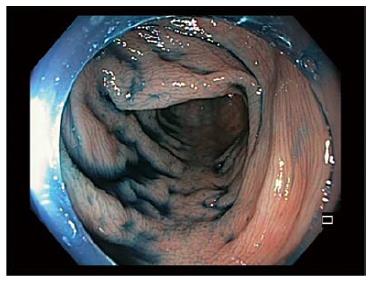
However, the use of a spray catheter has a certain cost, limits the suction capacity of the endoscope and often requires several passages with the endoscope, which can sometimes be difficult in some patients. We report on the feasibility of the indigocarmine dye application directly through the colonoscope air/water channel. Upon cecal intubation, the indigo carmine solution is prepared in the water bottle, using two 10 mL vials of 1% indigocarmine diluted in 80 mL of water, in order to obtain the 0.2% concentration (Figure 1). The indigo carmine dye is delivered by pressing on the air/water valve while orienting the head of the endoscope against the colonic walls and withdrawing the colonoscope. The indigocamine dye application is shown on Figure 2. It should be noted that the indigocarmine stained water does not remain on the objective lens of the endoscope rendering clear water unnecessary for the cleaning of the tip of the endoscope during the chromoendoscopy procedure. Once the end of a colonic segment has been reached, suction of the air allows uniform application of the dye on the mucosa and elimination of excess fluid. New air insufflation is then needed for the colonic mucosal examination. Immediately after the procedure, the air/water channel of the endoscope is flushed with water from another water bottle until the outflow is clear, to make sure that no indigocarmine dye remains inside the channel. After standard washing, we did not observe any residual staining in the water bottles. Our preliminary experience with 15 patients suggests that this simplified indigocarmine chromoendoscopic technique is feasible with Olympus® or Fujifilm® colonoscopes, with or without a cap (Figures 3-5) and with a median withdrawal time of 21 ± 12 min.
P- Reviewer: Amornyotin S, Garcia AZG, Kikuchi H S- Editor: Gong XM L- Editor: A E- Editor: Wu HL
| 1. | Kahi CJ, Anderson JC, Waxman I, Kessler WR, Imperiale TF, Li X, Rex DK. High-definition chromocolonoscopy vs. high-definition white light colonoscopy for average-risk colorectal cancer screening. Am J Gastroenterol. 2010;105:1301-1307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 160] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 2. | Kamiński MF, Hassan C, Bisschops R, Pohl J, Pellisé M, Dekker E, Ignjatovic-Wilson A, Hoffman A, Longcroft-Wheaton G, Heresbach D. Advanced imaging for detection and differentiation of colorectal neoplasia: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2014;46:435-449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 194] [Cited by in RCA: 196] [Article Influence: 17.8] [Reference Citation Analysis (0)] |