Published online Jun 25, 2015. doi: 10.4253/wjge.v7.i7.670
Peer-review started: March 16, 2015
First decision: April 10, 2015
Revised: April 24, 2015
Accepted: May 8, 2015
Article in press: May 11 2015
Published online: June 25, 2015
Processing time: 116 Days and 5.6 Hours
Patients with indeterminate colitis (IC) are significantly younger at diagnosis with onset of symptoms before the age of 18 years with significant morbidity in the interim. The successful care of IC is based on microscopic visual predict precision of eventual ulcerative colitis (UC) or Crohn’s colitis (CC) which is not offered in 15%-30% of inflammatory bowel disease (IBD) patients even after a combined state-of-the-art classification system of clinical, visual endoscopic, radiologic and histologic examination. These figures have not changed over the past 3 decades despite the introduction of newer diagnostic modalities. The patient outcomes after restorative proctocolectomy and ileal pouch-anal anastomosis may be painstaking if IC turns into CC. Our approach is aiming at developing a single sensitive and absolute accurate diagnostic test tool during the first clinic visit through endoscopic biopsy derived proteomic patterns. Matrix-assisted-laser desorption/ionization mass spectrometry (MS) and/or imaging MS technologies permit a histology-directed cellular test of endoscopy biopsy which identifies phenotype specific proteins, as biomarker that would assist clinicians more accurately delineate IC as being either a UC or CC or a non-IBD condition. These novel studies are underway on larger cohorts and are highly innovative with significances in differentiating a UC from CC in patients with IC and could lend mechanistic insights into IBD pathogenesis.
Core tip: This Editorial is introductory, dedicated to a novel and innovative study with clinical relevance regarding precision of indeterminate colitis (IC) into accurate diagnosis of either ulcerative colitis (UC) or Crohn’s colitis (CC). To date, it is very difficult to predict the clinical course of IC, whether it will evolve into UC or CC. About 90% of IC is diagnosed at the time of colectomy for fulminant colitis and subsequent management critically depends on the correct eventual diagnosis. The outcome after colectomy and pouch anastomosis may be painstaking if IC turns into CC. The undergoing studies of proteomic analysis on colon biopsy specimens, if successful will permit delineate IC into UC or CC precision which could be of great help in decision making regarding treatment indication. Although the present data is convincing and support differentiated between UC and CC, this data requires validation and confirmation on a large scale by clinical studies. Hopefully, this editorial will stimulate research into this field to trying to overcome the diagnostic accuracy challenges in inflammatory bowel diseases.
- Citation: Ballard BR, M’Koma AE. Gastrointestinal endoscopy biopsy derived proteomic patterns predict indeterminate colitis into ulcerative colitis and Crohn’s colitis. World J Gastrointest Endosc 2015; 7(7): 670-674
- URL: https://www.wjgnet.com/1948-5190/full/v7/i7/670.htm
- DOI: https://dx.doi.org/10.4253/wjge.v7.i7.670
In endoscopic medicine, predicting the phenotypic outcomes of “indeterminate colitis (IC)”, given its unpredictable clinical presentation and disease course, is challenging[1,2]. Inadequate differentiated diagnoses of the two predominantly colonic inflammatory bowel diseases (IBD), ulcerative colitis (UC) and Crohn’s colitis (CC), may lead to the inconclusive IC diagnosis even when a state-of-the-art classification system of combined clinical, endoscopic, radiologic and histologic tools[1,2] are used. Unless there is a unique and yet unclassified class of colitis, the field needs to develop supplemental molecular biomarker tools for precise and rapid distinction between UC and CC for patients that will otherwise be diagnosed with IC. Previous studies using mucosal biopsy[3,4] have been successful as prognostic indicators for IBD whether the colitis is in a quiescent or active state, but have not been able to distinguish UC from CC[3,4]. Patients with IC are significantly younger at diagnosis (M ± SEM, 9.53 ± 4.8 years)[5-8] with onset of symptoms before the age of 18 years[9-13]. IC shows an equal gender distribution[8,14,15]. In contrast, UC is predominant among males and the mean age at onset is 36-39 years[14-18]. These figures have not changed over the past 3 decades despite the introduction of newer diagnostic modalities[1,2,5,10,13,19]. Even after long-term surveillance, a substantial number of patients with IC still have an unchanged diagnosis[5,19,20], with significant patient suffering in the interim[5,19,20]. The continued presence of an IC diagnosis over a long period of time supports part of our hypothesis that IBD may represent a spectrum of diseases rather than just two entities, Crohn’s disease (CD) and UC[21].
The need for IC classification into either UC or CC is important for proper care in patients suffering from IBD, with obvious therapeutic and prognostic implications[22]. Early and accurate diagnosis and sub-classification of UC and CC is therefore the cornerstone for personalized and evidence-based interventional care[23-25]. These two pathologies have differing therapeutic strategies and prognoses. Most patients with UC, or IC likely to develop UC[22], will require pouch surgery for resolution[26-30]. Pouch surgery is well-established[22] and restores gut continuity, defecation, deferral, and discrimination, but is only successful if the UC and/or IC likely to develop UC diagnosis is correct[31,32]. However, IC and UC are mistakenly diagnosed in patients with CC[1,33]. Current data show that 15% of IBD patients who undergo pouch surgery for presumed definitive UC (or IC likely to develop UC) subsequently are diagnosed with de novo CD in the ileal pouch[34,35]. Identifying patients with CC and positive outcomes after pouch surgery is a painstaking clinical experience[4,34,35]. Ileal pouch anal anastomosis is acceptable standard care for UC patients, and restorative proctocolectomy should be contraindicated for CC patients[4,36,37] .
Pouch complications are significantly higher in patients with CC (± 64%) and IC (± 43%) vs patients having UC (± 22%) (P < 0.05)[23,38,39]. This diagnostic dilemma holds potential morbidity from unnecessary and/or inappropriate surgery, and underscores the need for a research strategy focused on developing molecular biometrics to improve diagnosis of colitides at initial endoscopic biopsy[21,40-44]. De novo CD in the ileal pouch is the diagnosis most feared by IBD patients and doctors due to its intractable nature and associated complications which often necessitate excision of the pouch with a permanent end-ileostomy[45-49].
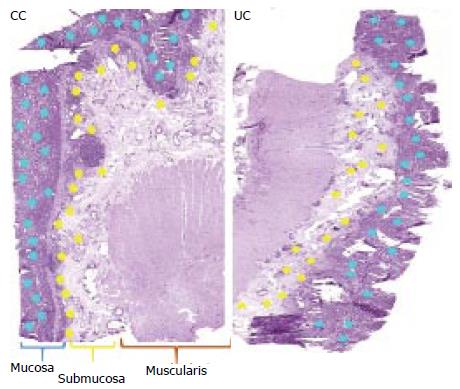
Mass spectrometry (MS) and imaging mass spectrometry (IMS)[21] are non-invasive technologies that can measure individual molecules in complex endoscopic and surgical clinical specimens[40,41]. These analyses provide quantitative and qualitative data about cellular systems, and can differentiate diseased from normal tissue, and can identify diseases within the same organ[40,41,50]. These characteristics offer significant diagnostic and prognostic potential for clinical medicine and could supplement known clinicopathologic variables for delineating IC into UC or CC at a patient’s first clinical visit. Due to the current alarming epidemiologic studies indicate that the incidence and prevalence of IBD is widening worldwide, especially in developing nations[9,21,51-60], established techniques like MS and IMS, which are affordable, non-invasive, easier, accurate and faster at screening for potential delineation of IBD, ought to be considered for clinical applications in IBD laboratories. The basic steps of the MS/IMS methodology of histology-directed proteomic patterns profiling are outlined in Figure 1.
The authors are thankful to Jared Elzey, CRA, from the Meharry Research Concierge Services (supported by NIH grants U54MD007593 and UL1TR000445) for comments, suggestions and for language editing.
P- Reviewer: Kato M, Mais V, Sharma SS, Zhu YL S- Editor: Tian YL L- Editor: A E- Editor: Wu HL
| 1. | Burakoff R. Indeterminate colitis: clinical spectrum of disease. J Clin Gastroenterol. 2004;38:S41-S43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 2. | Carvalho RS, Abadom V, Dilworth HP, Thompson R, Oliva-Hemker M, Cuffari C. Indeterminate colitis: a significant subgroup of pediatric IBD. Inflamm Bowel Dis. 2006;12:258-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 57] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 3. | Fukushima K, Yonezawa H, Fiocchi C. Inflammatory bowel disease-associated gene expression in intestinal epithelial cells by differential cDNA screening and mRNA display. Inflamm Bowel Dis. 2003;9:290-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Shkoda A, Werner T, Daniel H, Gunckel M, Rogler G, Haller D. Differential protein expression profile in the intestinal epithelium from patients with inflammatory bowel disease. J Proteome Res. 2007;6:1114-1125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 93] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 5. | Malaty HM, Mehta S, Abraham B, Garnett EA, Ferry GD. The natural course of inflammatory bowel disease-indeterminate from childhood to adulthood: within a 25 year period. Clin Exp Gastroenterol. 2013;6:115-121. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 6. | Hildebrand H, Fredrikzon B, Holmquist L, Kristiansson B, Lindquist B. Chronic inflammatory bowel disease in children and adolescents in Sweden. J Pediatr Gastroenterol Nutr. 1991;13:293-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 54] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 7. | Hildebrand H, Brydolf M, Holmquist L, Krantz I, Kristiansson B. Incidence and prevalence of inflammatory bowel disease in children in south-western Sweden. Acta Paediatr. 1994;83:640-645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 39] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Lindberg E, Lindquist B, Holmquist L, Hildebrand H. Inflammatory bowel disease in children and adolescents in Sweden, 1984-1995. J Pediatr Gastroenterol Nutr. 2000;30:259-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 127] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 9. | Malaty HM, Fan X, Opekun AR, Thibodeaux C, Ferry GD. Rising incidence of inflammatory bowel disease among children: a 12-year study. J Pediatr Gastroenterol Nutr. 2010;50:27-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 160] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 10. | Kugathasan S, Judd RH, Hoffmann RG, Heikenen J, Telega G, Khan F, Weisdorf-Schindele S, San Pablo W, Perrault J, Park R. Epidemiologic and clinical characteristics of children with newly diagnosed inflammatory bowel disease in Wisconsin: a statewide population-based study. J Pediatr. 2003;143:525-531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 441] [Cited by in RCA: 399] [Article Influence: 18.1] [Reference Citation Analysis (0)] |
| 11. | Loftus EV. Clinical epidemiology of inflammatory bowel disease: Incidence, prevalence, and environmental influences. Gastroenterology. 2004;126:1504-1517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2085] [Cited by in RCA: 2154] [Article Influence: 102.6] [Reference Citation Analysis (1)] |
| 12. | Turunen P, Kolho KL, Auvinen A, Iltanen S, Huhtala H, Ashorn M. Incidence of inflammatory bowel disease in Finnish children, 1987-2003. Inflamm Bowel Dis. 2006;12:677-683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 130] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 13. | Abraham BP, Mehta S, El-Serag HB. Natural history of pediatric-onset inflammatory bowel disease: a systematic review. J Clin Gastroenterol. 2012;46:581-589. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 158] [Cited by in RCA: 140] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 14. | Lee KS, Medline A, Shockey S. Indeterminate colitis in the spectrum of inflammatory bowel disease. Arch Pathol Lab Med. 1979;103:173-176. [PubMed] |
| 15. | Ekbom A. The epidemiology of IBD: a lot of data but little knowledge. How shall we proceed? Inflamm Bowel Dis. 2004;10 Suppl 1:S32-S34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 49] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 16. | Wells PT, Halliwell M, Skidmore R, Webb AJ, Woodcock JP. Tumour detection by ultrasonic Doppler blood-flow signals. Ultrasonics. 1977;15:231-232. [PubMed] [DOI] [Full Text] |
| 17. | Dayton MT, Larsen KR, Christiansen DD. Similar functional results and complications after ileal pouch-anal anastomosis in patients with indeterminate vs ulcerative colitis. Arch Surg. 2002;137:690-694; discussion 694-695. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 61] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 18. | Geboes K, De Hertogh G. Indeterminate colitis. Inflamm Bowel Dis. 2003;9:324-331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 45] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 19. | Meucci G, Bortoli A, Riccioli FA, Girelli CM, Radaelli F, Rivolta R, Tatarella M. Frequency and clinical evolution of indeterminate colitis: a retrospective multi-centre study in northern Italy. GSMII (Gruppo di Studio per le Malattie Infiammatorie Intestinali). Eur J Gastroenterol Hepatol. 1999;11:909-913. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 58] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 20. | Kangas E, Matikainen M, Mattila J. Is “indeterminate colitis” Crohn’s disease in the long-term follow-up? Int Surg. 1994;79:120-123. [PubMed] |
| 21. | M’Koma AE. Diagnosis of inflammatory bowel disease: Potential role of molecular biometrics. World J Gastrointest Surg. 2014;6:208-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 22. | Telakis E, Tsironi E. Indeterminate colitis - definition, diagnosis, characteristics and management. Ann Gastroenterol. 2008;3:173-179. |
| 23. | Tremaine WJ. Is indeterminate colitis determinable? Curr Gastroenterol Rep. 2012;14:162-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 24. | Koktysz R, Kozlowski W, Trawinski J, Wojtun S, Gil J. Histoclinic of “indeterminate colitis”. Pol Merkur Lekarski. 2007;22:446-448. [PubMed] |
| 25. | Tremaine WJ. Review article: Indeterminate colitis--definition, diagnosis and management. Aliment Pharmacol Ther. 2007;25:13-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 22] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 26. | Tatsumi K, Sugita A, Koganei K, Futatsuki R, Kuroki H, Yamada K, Nakao S, Sako M, Kimura H, Arai K. [Long-term outcomes of ileal pouch-anal canal anastomosis in children with ulcerative colitis]. Nihon Shokakibyo Gakkai Zasshi. 2013;110:2081-2088. [PubMed] |
| 27. | Pellino G, Sciaudone G, Candilio G, De Fatico GS, Landino I, Canonico S, Selvaggi F. Restorative proctocolectomy with ileal pouch-anal anastomosis is safe and effective in selected very elderly patients suffering from ulcerative colitis. Int J Surg. 2014;12 Suppl 2:S56-S59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 28. | Ceriati E, De Peppo F, Rivosecchi M. Role of surgery in pediatric ulcerative colitis. Pediatr Surg Int. 2013;29:1231-1241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 29. | Bikhchandani J, Polites SF, Wagie AE, Habermann EB, Cima RR. National trends of 3- versus 2-stage restorative proctocolectomy for chronic ulcerative colitis. Dis Colon Rectum. 2015;58:199-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 49] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 30. | Pellino G, Sciaudone G, Miele E, Candilio G, De Fatico GS, Riegler G, Staiano A, Canonico S, Selvaggi F. Functional outcomes and quality of life after restorative proctocolectomy in paediatric patients: a case-control study. Gastroenterol Res Pract. 2014;2014:340341. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 35] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 31. | Shen B, Remzi FH, Brzezinski A, Lopez R, Bennett AE, Lavery IC, Queener E, Fazio VW. Risk factors for pouch failure in patients with different phenotypes of Crohn’s disease of the pouch. Inflamm Bowel Dis. 2008;14:942-948. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 50] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 32. | Shen B. Crohn’s disease of the ileal pouch: reality, diagnosis, and management. Inflamm Bowel Dis. 2009;15:284-294. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 37] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 33. | Price AB. Overlap in the spectrum of non-specific inflammatory bowel disease--’colitis indeterminate’. J Clin Pathol. 1978;31:567-577. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 277] [Cited by in RCA: 221] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 34. | Wagner-Bartak NA, Levine MS, Rubesin SE, Laufer I, Rombeau JL, Lichtenstein GR. Crohn’s disease in the ileal pouch after total colectomy for ulcerative colitis: findings on pouch enemas in six patients. AJR Am J Roentgenol. 2005;184:1843-1847. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 35. | Gu J, Stocchi L, Kiran RP, Shen B, Remzi FH. Do clinical characteristics of de novo pouch Crohn’s disease after restorative proctocolectomy affect ileal pouch retention? Dis Colon Rectum. 2014;57:76-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 36. | Panis Y. Is there a place for ileal pouch-anal anastomosis in patients with Crohn’s colitis? Neth J Med. 1998;53:S47-S51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 37. | Panis Y, Bonhomme N, Hautefeuille P, Valleur P. Ileal pouch-anal anastomosis with mesorectal excision for rectal cancer complicating familial adenomatous polyposis. Eur J Surg. 1996;162:817-821. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 127] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 38. | Mitchell PJ, Rabau MY, Haboubi NY. Indeterminate colitis. Tech Coloproctol. 2007;11:91-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 39. | Brown CJ, Maclean AR, Cohen Z, Macrae HM, O’Connor BI, McLeod RS. Crohn’s disease and indeterminate colitis and the ileal pouch-anal anastomosis: outcomes and patterns of failure. Dis Colon Rectum. 2005;48:1542-1549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 108] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 40. | M’Koma AE, Seeley EH, Washington MK, Schwartz DA, Muldoon RL, Herline AJ, Wise PE, Caprioli RM. Proteomic profiling of mucosal and submucosal colonic tissues yields protein signatures that differentiate the inflammatory colitides. Inflamm Bowel Dis. 2011;17:875-883. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 51] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 41. | Seeley EH, Washington MK, Caprioli RM, M’Koma AE. Proteomic patterns of colonic mucosal tissues delineate Crohn’s colitis and ulcerative colitis. Proteomics Clin Appl. 2013;7:541-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 42] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 42. | M’Koma AE, Seeley EH, Wise PE, Washingtoin MK, Schwartz DA, Herline AJ, Muldon RL, Caprioli RM. Proteomic analysis of colonic submucosa differentiates Crohn’s and ulcerative colitis. Chicago, IL: Annual Congress - Digestive Disease Week 2009; 600. |
| 43. | M’Koma AE, Wise PE, Schwartz DA, Washington MK, Muldoon RL, El-Rifai WM, Herline AJ. Gene Expression of Colonic Submucosa Differs Between the Inflammatory Colitides. Minneapolis, MN: Annual Congress - The American Society of Colon and Rectal Surgeons 2010; 117. |
| 44. | Tontini GE, Vecchi M, Pastorelli L, Neurath MF, Neumann H. Differential diagnosis in inflammatory bowel disease colitis: state of the art and future perspectives. World J Gastroenterol. 2015;21:21-46. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 120] [Cited by in RCA: 146] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 45. | Deutsch AA, McLeod RS, Cullen J, Cohen Z. Results of the pelvic-pouch procedure in patients with Crohn’s disease. Dis Colon Rectum. 1991;34:475-477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 108] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 46. | Grobler SP, Hosie KB, Affie E, Thompson H, Keighley MR. Outcome of restorative proctocolectomy when the diagnosis is suggestive of Crohn’s disease. Gut. 1993;34:1384-1388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 74] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 47. | Keighley MR. The final diagnosis in pouch patients for presumed ulcerative colitis may change to Crohn’s disease: patients should be warned of the consequences. Acta Chir Iugosl. 2000;47:27-31. [PubMed] |
| 48. | Mylonakis E, Allan RN, Keighley MR. How does pouch construction for a final diagnosis of Crohn’s disease compare with ileoproctostomy for established Crohn’s proctocolitis? Dis Colon Rectum. 2001;44:1137-1142; discussion 1142-1143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 32] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 49. | Achkar JP, Shen B. Medical management of postoperative complications of inflammatory bowel disease: pouchitis and Crohn’s disease recurrence. Curr Gastroenterol Rep. 2001;3:484-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 50. | M’Koma AE, Blum DL, Norris JL, Koyama T, Billheimer D, Motley S, Ghiassi M, Ferdowsi N, Bhowmick I, Chang SS. Detection of pre-neoplastic and neoplastic prostate disease by MALDI profiling of urine. Biochem Biophys Res Commun. 2007;353:829-834. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 76] [Cited by in RCA: 66] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 51. | Molodecky NA, Soon IS, Rabi DM, Ghali WA, Ferris M, Chernoff G, Benchimol EI, Panaccione R, Ghosh S, Barkema HW. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012;142:46-54.e42; quiz e30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3789] [Cited by in RCA: 3527] [Article Influence: 271.3] [Reference Citation Analysis (5)] |
| 52. | Desai HG, Gupte PA. Increasing incidence of Crohn’s disease in India: is it related to improved sanitation? Indian J Gastroenterol. 2005;24:23-24. [PubMed] |
| 53. | Benchimol EI, Fortinsky KJ, Gozdyra P, Van den Heuvel M, Van Limbergen J, Griffiths AM. Epidemiology of pediatric inflammatory bowel disease: a systematic review of international trends. Inflamm Bowel Dis. 2011;17:423-439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 749] [Cited by in RCA: 711] [Article Influence: 50.8] [Reference Citation Analysis (0)] |
| 54. | Zaahl MG, Winter TA, Warnich L, Kotze MJ. The -237C--& gt; T promoter polymorphism of the SLC11A1 gene is associated with a protective effect in relation to inflammatory bowel disease in the South African population. Int J Colorectal Dis. 2006;21:402-408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 55. | Zaahl MG, Winter T, Warnich L, Kotze MJ. Analysis of the three common mutations in the CARD15 gene (R702W, G908R and 1007fs) in South African colored patients with inflammatory bowel disease. Mol Cell Probes. 2005;19:278-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 28] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 56. | Esmat S, El Nady M, Elfekki M, Elsherif Y, Naga M. Epidemiological and clinical characteristics of inflammatory bowel diseases in Cairo, Egypt. World J Gastroenterol. 2014;20:814-821. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 38] [Cited by in RCA: 39] [Article Influence: 3.5] [Reference Citation Analysis (1)] |
| 57. | Ukwenya AY, Ahmed A, Odigie VI, Mohammed A. Inflammatory bowel disease in Nigerians: still a rare diagnosis? Ann Afr Med. 2011;10:175-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 58. | Siala N, Benzarti A, Boukthir S, Brini I, Sammoud A, Bousnina S, Ben Becher S, Lakhoua R, Fethi B, Harbi A. [Pediatric Crohn’s disease in Tunisia]. Tunis Med. 2013;91:715-723. [PubMed] |
| 59. | Senbanjo IO, Oshikoya KA, Onyekwere CA, Abdulkareem FB, Njokanma OF. Ulcerative colitis in a Nigerian girl: a case report. BMC Res Notes. 2012;5:564. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |