Published online Jun 10, 2015. doi: 10.4253/wjge.v7.i6.665
Peer-review started: October 8, 2014
First decision: November 14, 2014
Revised: December 19, 2014
Accepted: March 16, 2015
Article in press: March 18, 2015
Published online: June 10, 2015
Processing time: 254 Days and 16.6 Hours
Progress in double-balloon endoscopy (DBE) has allowed for the diagnosis and treatment of disease in the postoperative bowel. For example, a short DBE, which has a 2.8 mm working channel and 152 cm working length, is useful for endoscopic retrograde cholangiopancreatography in bowel disease patients. However, afferent loop and Roux-limb obstruction, though rare, is caused by postoperative recurrence of biliary tract cancer with intractable complications. Most of the clinical findings involving these complications are relatively nonspecific and include abdominal pain, nausea, vomiting, fever, and obstructive jaundice. Treatments by surgery, percutaneous transhepatic biliary drainage, percutaneous enteral stent insertion, and endoscopic therapy have been reported. The general conditions of patients with these complications are poor due to cancer progression; therefore, a less invasive treatment is better. We report on the usefulness of metallic stent insertion using an overtube for afferent loop and Roux-limb obstruction caused by postoperative recurrence of biliary tract cancer under short DBE in two patients with complexly reconstructed intestines.
Core tip: Malignant afferent loop and Roux-limb obstruction are intractable complications caused by postoperative recurrence of biliary tract cancer. Metallic stent insertion using an overtube under double-balloon endoscopy is a safe and feasible treatment option in such cases.
- Citation: Fujii M, Ishiyama S, Saito H, Ito M, Fujiwara A, Niguma T, Yoshioka M, Shiode J. Metallic stent insertion with double-balloon endoscopy for malignant afferent loop obstruction. World J Gastrointest Endosc 2015; 7(6): 665-669
- URL: https://www.wjgnet.com/1948-5190/full/v7/i6/665.htm
- DOI: https://dx.doi.org/10.4253/wjge.v7.i6.665
Malignant afferent loop obstruction is a potentially life-threatening adverse event of Billroth II gastrectomy and pancreaticoduodenectomy. The occlusion is generally caused by a recurrent tumor, and often presents as chronic, progressive, partial obstruction[1-3]. This type of complication is expected to increase along with therapeutic advances for malignant tumors, thus necessitating the development of safe, effective treatments.
The general condition of patients with malignant afferent loop obstructions is poor due to cancer progression, and thus a less invasive treatment is preferred. Malignant afferent loop obstructions can be treated with surgery, percutaneous transhepatic biliary drainage, percutaneous enteral stent insertion, or endoscopic therapy[4-6]. Endoscopic stents for digestive tract obstruction are a minimally invasive, useful, and safe treatment[7-9]. The primary obstacle for endoscopic stent treatment in postoperative digestive tract obstruction is the difficulty in approaching the obstructing lesion. Of note, there are reports on the use of double-balloon endoscopy (DBE) for complicated postoperative bowel reconstructions[10,11]. Furthermore, a short DBE, which has a 2.8 mm working channel and 152 cm working length, is useful for endoscopic retrograde cholangiopancreatography in these patients[12]. However, because of the large diameter of the system for delivery of metallic stents (MS) indigestive tract obstructions, they cannot be deployed through the narrow working channel of a short DBE. Therefore, new methods are needed to deploy an MS with DBE.
We report on the usefulness of MS insertion using an overtube under a short DBE for afferent loop and Roux-limb obstruction caused by postoperative recurrence of biliary tract cancer in two patients with complexly reconstructed intestines.
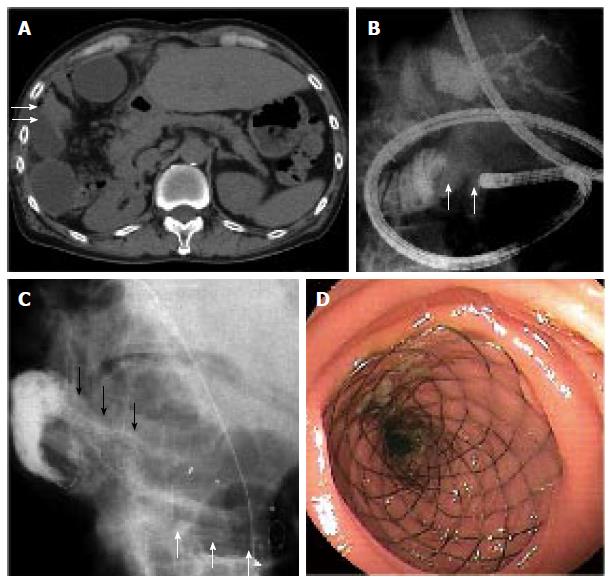
A man in his sixties underwent Roux-en-Y hepaticojejunostomy because of cholangiocarcinoma. Chemotherapy was performed one year later for recurrence of peritoneal dissemination. Two years after chemotherapy, the patient developed a fever and elevated serum transaminase levels. Laboratory tests were as follows: white blood cell (WBC) counts, 9410/μL (normal: 4500-8500/μL); C-reactive protein, 4.7 mg/dL (normal: < 0.26 mg/dL); total bilirubin, 1.2 mg/dL (normal: 0.2-1.2 mg/dL); γ-glutamyltranspeptidase (γGTP), 256 IU/L (normal: 5-40 IU/L); aspartate aminotransferase (AST), 38 IU/L (normal: 10-35 IU/L); and alanine aminotransferase (ALT), 17 IU/L (normal: 7-42 IU/L). Abdominal computed tomography (CT) showed the reconstructed jejunum that was expanded at the site of hepatectomy, mild expansion of the intrahepatic bile ducts and stenosis of the reconstructed jejunum (Figure 1A). The patient was diagnosed with malignant Roux-limb obstruction due to peritoneal dissemination and cholangitis.
Ultrasound-guided drainage was performed for the dilated jejunal Roux-limb, but repeated inflammatory aggravation with drain obstruction occurred. Therefore, a short DBE was performed with the patient under conscious sedation. The short DBE (EC-450BI5; Fujifilm, Tokyo, Japan) was inserted into the Roux-limb obstruction (Figure 1B), and a 0.035 inch guide-wire (Radifocus; Terumo, Tokyo, Japan) was passed through the site of the stricture. Then, a standard endoscopic retrograde cholangiopancreatography injection catheter (MTW Endoskopie, Düsseldorf, Germany) was inserted, and passage through the stenosis was confirmed by radiography. The guide-wire was exchanged with a 0.035 inch Jagwire (Boston Scientific Co., Natick, MA, United States), and an overtube was left to prevent bowel expansion. The DBE was then removed. Finally, an MS (2.2 cm × 6.0 cm, Wallflex duodenal stent; Boston Scientific Co.) was inserted through the overtube in combination with an over-the-wire technique (Figure 1C) and deployed (Figure 1D). There were no perioperative or postoperative adverse events.
After stent insertion, the patient’s cholangitis, general condition, and laboratory tests improved as follows: WBC count, 7960/μL; C-reactive protein, 1.86 mg/dL; total bilirubin, 0.7 mg/dL; γGTP, 96 IU/L; AST, 25 IU/L; and ALT, 19 IU/L. On CT, dilation of the Roux-limb disappeared, and chemotherapy resumed. However, this patient died because of peritonitis carcinomatosa 141 d after stent insertion.
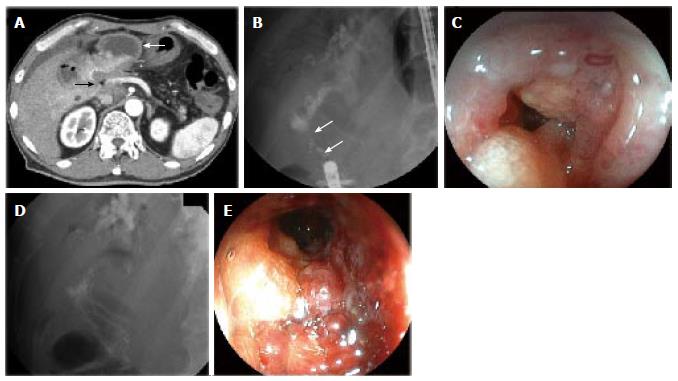
A man in his sixties underwent pancreaticoduodenectomy because of Vater’s papilla cancer. He developed a fever and jaundice approximately 10 mo after the operation. Laboratory tests were as follows: total bilirubin 9.9 mg/dL; γGTP, 401 IU/L; AST, 273 IU/L; and ALT, 283 IU/L. Abdominal CT showed ascites, dilation of the afferent loop, and a surrounding soft density (Figure 2A). The patient was thus diagnosed with malignant afferent loop obstruction due to peritoneal dissemination and cholangitis.
A short DBE (EC-450BI5; Fujifilm) was performed, which revealed stenosis with irregular mucosa at the afferent loop obstruction (Figure 2B and C). An MS (2.2 cm × 6.0 cm, Niti-S D-type stent; Taewoong Medical Inc., Seoul, South Korea) was inserted and deployed as described in case 1 (Figure 2D and E). There were no perioperative or postoperative adverse events.
After insertion of the MS, the patient’s general condition and laboratory tests improved: total bilirubin, 1.5 mg/dL; γGTP, 296 IU/L; AST, 92 IU/L; and ALT, 77 IU/L. Chemotherapy was resumed, however this patient also died from peritonitis carcinomatosa 140 d after stent insertion.
Afferent loop and Roux-limb obstruction are rare adverse events that result in the obstruction of the postoperative intestinal tract. When jaundice and/or fever occur in a postoperative cancer patient with intestinal tract reconstruction, it is important to consider afferent loop or Roux-limb obstruction due to recurrence. Obstructions are typically treated with surgery; however, the general condition of many of these patients is so poor that surgery is not possible. In such cases, insertion of an MS through the stenosis is a useful treatment.
Although percutaneous stent deployment has been reported[13,14], the endoscopic approach allows for direct identification of the stenosis. There are few reports using this method, due to the difficulty in reaching the stenosis with an endoscope, and the need for a scope with a large enough working channel diameter to permit insertion of an MS. In the cases reported here, malignant afferent loop and Roux-limb obstructions were confirmed by DBE and the stenoses were penetrated with a guide-wire. The endoscope was then removed, leaving the overtube to prevent bowel expansion and deploy the MS with an over-the-wire technique. With this method, the stents were safely and easily inserted through the stenoses using a DBE, eliminating the need for a new endoscope. DBE was chosen over a colonoscope in these cases, as it can cause patient discomfort and poses a risk to the patient’s health. Stents were safely inserted without a high degree of difficulty and did not produce major adverse events. Moreover, the patients were able to leave the hospital early.
There are other treatments for afferent loop obstruction, such as percutaneous transhepatic biliary drainage or endoscopic ultrasound-guided transhepatic drainage. When a hepatic-jejunal anastomotic stricture coexists, these methods may be particularly useful. However, biliary access can be challenging in patients without dilation of intrahepatic biliary ducts or in patients with ascites. In our cases, we could confirm the absence of judge hepatic-jejunal anastomotic strictures because the bile ducts were easily contrasted by cystography from the afferent loop. Thus, treatments should be selected depending on the patient’s condition.
In conclusion, MS insertion using an overtube for afferent loop and Roux-limb obstruction from postoperative recurrence of biliary tract cancer under short DBE is safe and feasible. However, it is necessary to accumulate more cases to determine the true rates of adverse events and confirm the effectiveness of this approach in comparison with surgery and other treatments.
Two men in their sixties who underwent Roux-en-Y hepaticojejunostomy after presenting with cholangiocarcinoma and a fever (Case 1) and pancreaticoduodenectomy due to Vater’s papilla cancer after presenting with fever and jaundice (Case 2) are reported here.
Case 1: Fever; Case 2: Fever and jaundice upon physical exam.
Pseudocyst; ileus.
Case 1: WBC, 9410/μL; C-reactive protein, 4.7 mg/dL; total bilirubin, 1.2 and 9.9 mg/dL; γ-glutamyltranspeptidase, 256 and 401 IU/L; aspartate aminotransferase, 38 and 273IU/L; and alanine aminotransferase,17 and 283 IU/L, for case 1 and case 2, respectively.
Computed tomography (CT) in case 1 revealed expansion at the site of hepatectomy in the reconstructed jejunum, mild expansion of intrahepatic bile ducts, and stenosis of reconstructed jejunum; in case 2, CT revealed ascites, dilation of the afferent loop, and a surrounding soft density.
Metallic stent insertion with double-balloon endoscopy for malignant afferent loop and Roux-limb obstruction.
Afferent loop and Roux-limb obstructions caused by postoperative recurrence of biliary tract cancer are rare and intractable.
Malignant afferent loop obstructions are rare adverse events due to the obstruction of the postoperative intestinal tract of Billroth II gastrectomy and pancreaticoduodenectomy.
Metallic stent insertion using an overtube for afferent loop and Roux-limb obstruction caused by postoperative recurrence of biliary tract cancer under short double-balloon endoscopy is safe and feasible.
The technique is interesting and clinically relevant, and will be of interest to this journal’s readership.
P- Reviewer: Botaitis SC, Camellini L, Kayaalp C, Ladas SD S- Editor: Tian YL L- Editor: A E- Editor: Wu HL
| 1. | Burdick JS, Garza AA, Magee DJ, Dykes C, Jeyarajah R. Endoscopic management of afferent loop syndrome of malignant etiology. Gastrointest Endosc. 2002;55:602-605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 32] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 2. | Aimoto T, Uchida E, Nakamura Y, Katsuno A, Chou K, Tajiri T, Naito Z. Malignant afferent loop obstruction following pancreaticoduodenectomy: report of two cases. J Nippon Med Sch. 2006;73:226-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 41] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 3. | Kim YH, Han JK, Lee KH, Kim TK, Kim KW, Choi BI. Palliative percutaneous tube enterostomy in afferent-loop syndrome presenting as jaundice: clinical effectiveness. J Vasc Interv Radiol. 2002;13:845-849. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Laasch HU. Obstructive jaundice after bilioenteric anastomosis: transhepatic and direct percutaneous enteral stent insertion for afferent loop occlusion. Gut Liver. 2010;4 Suppl 1:S89-S95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 5. | Bakes D, Cain C, King M, Dong Xda E. Management of afferent loop obstruction from recurrent metastatic pancreatic cancer using a venting gastrojejunostomy. World J Gastrointest Oncol. 2013;5:235-239. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 9] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Pannala R, Brandabur JJ, Gan SI, Gluck M, Irani S, Patterson DJ, Ross AS, Dorer R, Traverso LW, Picozzi VJ. Afferent limb syndrome and delayed GI problems after pancreaticoduodenectomy for pancreatic cancer: single-center, 14-year experience. Gastrointest Endosc. 2011;74:295-302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 69] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 7. | Repici A, de Paula Pessoa Ferreira D. Expandable metal stents for malignant colorectal strictures. Gastrointest Endosc Clin N Am. 2011;21:511-533, ix. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Sasaki T, Isayama H, Maetani I, Nakai Y, Kogure H, Kawakubo K, Mizuno S, Yagioka H, Matsubara S, Ito Y. Japanese multicenter estimation of WallFlex duodenal stent for unresectable malignant gastric outlet obstruction. Dig Endosc. 2013;25:1-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 53] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 9. | Saida Y, Enomoto T, Takabayashi K, Otsuji A, Nakamura Y, Nagao J, Kusachi S. Outcome of 141 cases of self-expandable metallic stent placements for malignant and benign colorectal strictures in a single center. Surg Endosc. 2011;25:1748-1752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 34] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 10. | Shimatani M, Matsushita M, Takaoka M, Koyabu M, Ikeura T, Kato K, Fukui T, Uchida K, Okazaki K. Effective “short” double-balloon enteroscope for diagnostic and therapeutic ERCP in patients with altered gastrointestinal anatomy: a large case series. Endoscopy. 2009;41:849-854. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 161] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 11. | Kato H, Tsutsumi K, Harada R, Okada H, Yamamoto K. Short double-balloon enteroscopy is feasible and effective for endoscopic retrograde cholangiopancreatography in patients with surgically altered gastrointestinal anatomy. Dig Endosc. 2014;26 Suppl 2:130-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | Ikeura T, Shimatani M, Takaoka M, Matsushita M, Miyoshi H, Kurishima A, Sumimoto K, Miyamoto S, Okazaki K. Intrahepatic cholangiocarcinoma diagnosed via endoscopic retrograde cholangiopancreatography with a short double-balloon enteroscope. World J Gastroenterol. 2013;19:4427-4431. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 13. | Hosokawa I, Kato A, Shimizu H, Furukawa K, Miyazaki M. Percutaneous transhepatic metallic stent insertion for malignant afferent loop obstruction following pancreaticoduodenectomy: a case report. J Med Case Rep. 2012;6:198. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 14. | Mocanu SN, González López JA, Villalba Auñón J, Artigas Raventós V. Percutaneous treatment of a tumour obstruction of the afferent loop of a hepaticojejunostomy. Cir Esp. 2014;92:209-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |