Published online Mar 16, 2015. doi: 10.4253/wjge.v7.i3.290
Peer-review started: July 6, 2014
First decision: August 28, 2014
Revised: January 5, 2015
Accepted: January 15, 2015
Article in press: January 19, 2015
Published online: March 16, 2015
Processing time: 257 Days and 8.4 Hours
Squamous papilloma of the esophagus is a rare benign lesion of the esophagus. Radiofrequency ablation is an established endoscopic technique for the eradication of Barrett esophagus. No cases of endoscopic ablation of esophageal papilloma by radiofrequency ablation (RFA) have been reported. We report a case of esophageal papilloma successfully treated with a single session of radiofrequency ablation. Endoscopic ablation of the lesion was achieved by radiofrequency using a new catheter inserted through the working channel of endoscope. The esophageal ablated tissue was removed by a specifically designed cup. Complete ablation was confirmed at 3 mo by endoscopy with biopsies. This case supports feasibility and safety of as a new potential indication for BarrxTM RFA in patients with esophageal papilloma.
Core tip: This paper reports for the first time a flexible endoscopic treatment of esophageal papilloma by a new radiofrequency system that goes into the working channel of the endoscope. This allows the endoscopist to see what he is doing along the procedure and to complete the procedure in few minutes. The procedure was performed without particular difficulties and did not required elevated skills.
- Citation: del Genio G, del Genio F, Schettino P, Limongelli P, Tolone S, Brusciano L, Avellino M, Vitiello C, Docimo G, Pezzullo A, Docimo L. Esophageal papilloma: Flexible endoscopic ablation by radiofrequency. World J Gastrointest Endosc 2015; 7(3): 290-294
- URL: https://www.wjgnet.com/1948-5190/full/v7/i3/290.htm
- DOI: https://dx.doi.org/10.4253/wjge.v7.i3.290
Esophageal benign lesion is often a major concern due to need of an effective and low risk procedure combined to unmodified physiology[1]. Radiofrequency ablation (RFA) is an established endoscopic technique for the eradication of Barrett esophagus, which has been investigated in a variety of study designs and settings[2-6].
RFA is associated with an acceptable safety profile, high rates of complete eradication of dysplasia and intestinal metaplasia, durability of effect, and a significant relative risk reduction for neoplastic progression, thus it is considered a standard of care for patients with high-grade dysplasia[7].
Squamous papilloma (SP) of the esophagus is a rare benign lesion of the esophagus. The prevalence ranges from 0.01 % to 0.45 %[8]. SP of the esophagus is usually asymptomatic and rarely causes dysphagia. Esophageal squamous papillomatosis is typically reported as a wart-like and fleshy-pink single lesion, most commonly in the middle or distal esophagus; the typical endoscopic appearance is a single, round sessile lesion[9]. The underlying etiology is unclear, but chronic reflux disease, mucosal trauma, and human papillomavirus (HPV) infection have been implicated, although most lesions are found in absence of HPV[10]. The malignant potential of the lesion is unknown, and no guidelines exist regarding follow-up of these lesions[11]. Some authors have recently reported the possibility of an endoscopic removal[12,13]. To the best of our knowledge, no cases of endoscopic ablation of esophageal papilloma by RFA has been reported. We report a case of esophageal papilloma successfully treated with a single session of RFA.
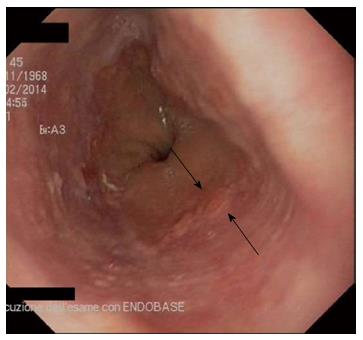
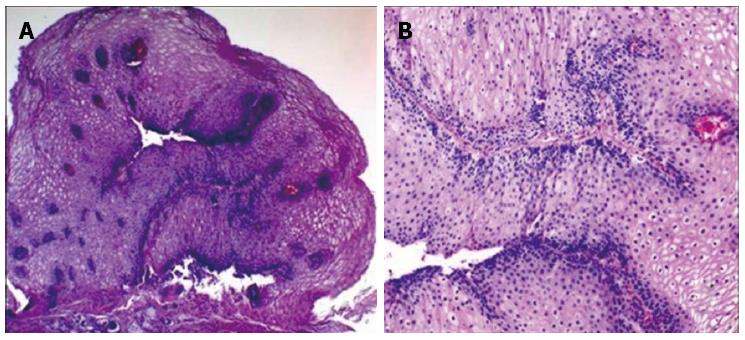
This case was conducted according to the Declaration of Helsinki and approved by the local institutional review board. In February 2014, a 52-year-old white asymptomatic woman was referred to our unit in the preoperative assessment of intragastric baloon placement for obesity. Upper gastrointestinal endoscopy (UGIE) revealed the presence of a single whitish wart-like area of about 0.5 cm in diameter which was located 37 cm from the incisors, above the Z-line (Figure 1). Narrow band imaging (NBI) confirmed the presence of an unstained area. Histologic examination showed the presence of micropapilloma of the esophagus surrounded by cilindric epithelium with congestion and flogosis (Figure 2). In April 2014 a session of RFA (BarrxTM, Covidien, CA, United States) on the dysmorphic esophageal area was performed. Total length of the procedure was 10 min. No complications occurred during the procedure. Postoperative course was uneventful.
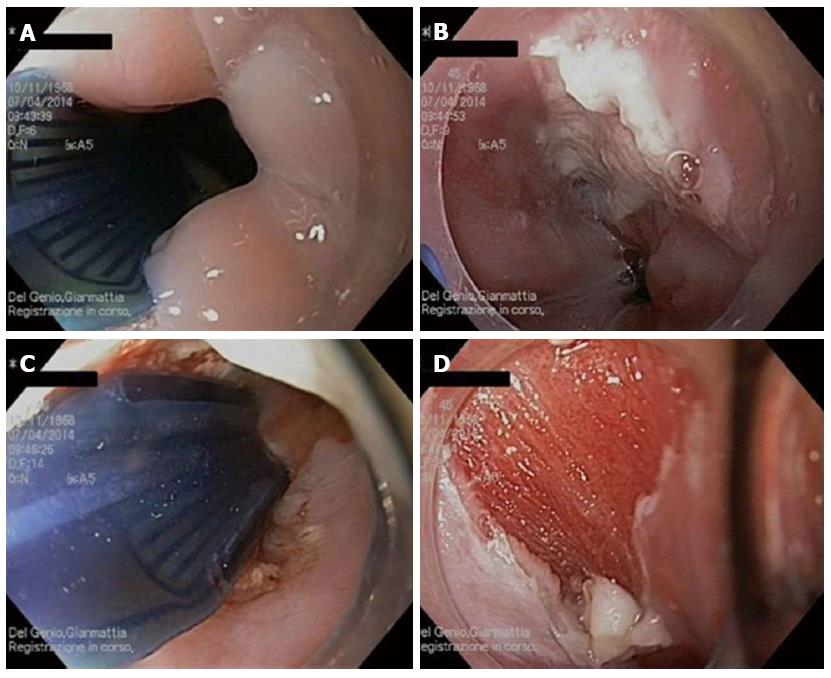
The patient was positioned in the left lateral decubitus position under monitoring of vital signs. Intravenous sedation was administered. An UGIE allowed identification of the esophageal papilloma. The total length of the area was calculated. Esophageal lumen was pre-treated with N-acetycysteine 1% (MucomystTM). A new designed catheter (Channel RFA Endoscopic Catheter, Barrx™, Covidien) was inserted through the working channel of a standard flexible gastroscope (Figure 3). The electric pad of the catheter was placed under direct visualization so that the entire suspected area was covered. Radiofrequency was applied at 300 W and 12 J/cm2. The wound along the ablation zone was cleaned from debris using Barrx™ RFA Cleaning cup mounted on distal end of endoscope. The ablation was repeated using the same procedure (Figure 4). The patient was discharged the same day. An UGIE was repeated after one months, showing a whitish area suggestive of scarring at the site of ablation without macroscopical evidence of residual papilloma. A second UGIE with biopsies, at 3 mo, excluded the presence of recurrent disease.
RFA has been recently reported to be more effective and less costly than photodynamic therapy in the treatment of Barrett’s related dysplasia[14]. On the other hand, an important advantage of RFA lays on simplicity and safety of the procedure suggesting the treatment can be effective with potential lower complications rates than more invasive techniques such as endoscopic resection. In this case an asymptomatic patient was discovered to have an esophageal papilloma in course of preoperative EGDS before bariatric treatment.
In this case, the efficacy was reached by a single session of RFA, with a minimal discomfort for the patient and a relatively low impact on the endoscopic center. Our initial experience supports the feasibility and safety of a new potential indication for BarrxTM RFA in patients with esophageal papilloma. Further cases and a longer follow up will be needed to drive a definitive conclusion.
“Considerate la vostra semenza: Fatti non foste a viver come bruti, ma per seguir virtute e canoscenza.” (Consider well the seed that gave you birth: you were not made to live as brutes, but to follow virtue and knowledge). Ulysses in The Divine Comedy. Dante Alighieri, Canto XXVI, 1308-21.
A 52-year-old female with esophageal papilloma.
The tumor was diagnosed during routine gastroscopy for preoperative assessment before placing intragastric baloon.
Esophageal high grade dysplasia, metaplasia, early adenocarcimona or squamous cell carcinoma.
All blood test were within normal limits.
Upper endoscopy showed the lesion, byopsies were taken.
Histologic examination showed the presence of micropapilloma of the esophagus surrounded by cilindric epithelium with congestion and flogosis.
Single treatment of endoscopic ablation by radiofrequency.
Endoscopic curative treatment is becoming more popular. This is the first report of squamous esophageal papilome treated by a new catheter radiofrequency technology.
RFA: Radiofrequency ablation is a relatively new technique generally used to treat Barrett’s esophagus related high grade dysplasia. This technology uses bipolar energy associated to impedance to automatically controll the energy output.
The new technical possibility allows a less invasive approach with a reduced risks of potentially serious complication and a faster return to normal life.
The manuscript is very well.
P- Reviewer: de Mello RA S- Editor: Ji FF L- Editor: A E- Editor: Zhang DN
| 1. | Del Genio G, Tolone S, Del Genio F, D’Alessandro A, Brusciano L, Aggarwal R, Conzo G, Orditura M, Docimo L, Del Genio A. Impact of total fundoplication on esophageal transit: analysis by combined multichannel intraluminal impedance and manometry. J Clin Gastroenterol. 2012;46:e1-e5. |
| 2. | Phoa KN, Pouw RE, van Vilsteren FG, Sondermeijer CM, Ten Kate FJ, Visser M, Meijer SL, van Berge Henegouwen MI, Weusten BL, Schoon EJ. Remission of Barrett’s esophagus with early neoplasia 5 years after radiofrequency ablation with endoscopic resection: a Netherlands cohort study. Gastroenterology. 2013;145:96-104. |
| 3. | van Vilsteren FG, Pouw RE, Seewald S, Alvarez Herrero L, Sondermeijer CM, Visser M, Ten Kate FJ, Yu Kim Teng KC, Soehendra N, Rösch T. Stepwise radical endoscopic resection versus radiofrequency ablation for Barrett’s oesophagus with high-grade dysplasia or early cancer: a multicentre randomised trial. Gut. 2011;60:765-773. |
| 4. | Pouw RE, Wirths K, Eisendrath P, Sondermeijer CM, Ten Kate FJ, Fockens P, Devière J, Neuhaus H, Bergman JJ. Efficacy of radiofrequency ablation combined with endoscopic resection for barrett’s esophagus with early neoplasia. Clin Gastroenterol Hepatol. 2010;8:23-29. |
| 5. | Shaheen NJ, Sharma P, Overholt BF, Wolfsen HC, Sampliner RE, Wang KK, Galanko JA, Bronner MP, Goldblum JR, Bennett AE. Radiofrequency ablation in Barrett’s esophagus with dysplasia. N Engl J Med. 2009;360:2277-2288. |
| 6. | Fleischer DE, Overholt BF, Sharma VK, Reymunde A, Kimmey MB, Chuttani R, Chang KJ, Muthasamy R, Lightdale CJ, Santiago N. Endoscopic radiofrequency ablation for Barrett’s esophagus: 5-year outcomes from a prospective multicenter trial. Endoscopy. 2010;42:781-789. |
| 7. | Phoa KN, van Vilsteren FG, Weusten BL, Bisschops R, Schoon EJ, Ragunath K, Fullarton G, Di Pietro M, Ravi N, Visser M. Radiofrequency ablation vs endoscopic surveillance for patients with Barrett esophagus and low-grade dysplasia: a randomized clinical trial. JAMA. 2014;311:1209-1217. |
| 8. | Takeshita K, Murata S, Mitsufuji S, Wakabayashi N, Kataoka K, Tsuchihashi Y, Okanoue T. Clinicopathological characteristics of esophageal squamous papillomas in Japanese patients--with comparison of findings from Western countries. Acta Histochem Cytochem. 2006;39:23-30. |
| 9. | Lewin KJ, Appelman HD. Tumors of the esophagus & stomach: atlas of tumor pathology. 3rd Series, Vol. 18. American Registry of Pathology. Washington, DC: Armed forced Institute of Pathology 1995; 31-32. |
| 10. | Del Genio G, Tolone S, Limongelli P, Brusciano L, D’Alessandro A, Docimo G, Rossetti G, Silecchia G, Iannelli A, del Genio A. Sleeve gastrectomy and development of “de novo” gastroesophageal reflux. Obes Surg. 2014;24:71-77. |
| 11. | Odze R, Antonioli D, Shocket D, Noble-Topham S, Goldman H, Upton M. Esophageal squamous papillomas. A clinicopathologic study of 38 lesions and analysis for human papillomavirus by the polymerase chain reaction. Am J Surg Pathol. 1993;17:803-812. |
| 12. | Kim E, Byrne MF, Donnellan F. Endoscopic mucosal resection of esophageal squamous papillomatosis. Can J Gastroenterol. 2012;26:780-781. |
| 13. | del Genio G, Rossetti G, Brusciano L, Limongelli P, Pizza F, Tolone S, Fei L, Maffettone V, Napolitano V, del Genio A. Laparoscopic Nissen-Rossetti fundoplication with routine use of intraoperative endoscopy and manometry: technical aspects of a standardized technique. World J Surg. 2007;31:1099-1106. |
| 14. | Ertan A, Zaheer I, Correa AM, Thosani N, Blackmon SH. Photodynamic therapy vs radiofrequency ablation for Barrett’s dysplasia: efficacy, safety and cost-comparison. World J Gastroenterol. 2013;19:7106-7113. |