Published online Mar 16, 2015. doi: 10.4253/wjge.v7.i3.247
Peer-review started: August 29, 2014
First decision: November 1, 2014
Revised: November 15, 2014
Accepted: December 16, 2014
Article in press: December 17, 2014
Published online: March 16, 2015
Processing time: 203 Days and 9.8 Hours
Double balloon enteroscopy (DBE) is an advanced type of endoscopic procedure which brings the advantage of reaching the whole small bowel using anterograde or the retrograde route. This procedure is both diagnostic and interventional for a variety of small intestinal diseases, such as vascular lesions, tumors, polyps and involvement of inflammatory bowel diseases. Main indication is the diagnosis and treatment of mid-gastrointestinal bleeding according to the recent published data all over the world. The complication rates seem to be higher than conventional procedures but growing experience is lowering them and improving the procedure to be safe and well tolerated. This review is about the technique, indications, diagnostic importance and complications of DBE according to the literature growing since 2001.
Core tip: Double balloon enteroscopy (DBE) is a novel technique of great interest as the clinician gains the opportunity of examining the whole small bowel without any surgical intervention. Diagnostic and therapeutic ability of the procedure influences the importance and common use of DBE for patients with documented or suspected small bowel disease. This review summarizes the indications, diagnostic yield and complications of the procedure according to the worldwide knowledge since 2001.
- Citation: Saygili F, Saygili SM, Oztas E. Examining the whole bowel, double balloon enteroscopy: Indications, diagnostic yield and complications. World J Gastrointest Endosc 2015; 7(3): 247-252
- URL: https://www.wjgnet.com/1948-5190/full/v7/i3/247.htm
- DOI: https://dx.doi.org/10.4253/wjge.v7.i3.247
Evolving fiber optic technology provided the opportunity of examining inner body compartments that can be reached through either a natural or an artificial orifice. Gastrointestinal (GI) endoscopy is one of the best modalities to perform further investigations for the patients with digestive complaints. However before 1980s due to lack of technological improvements physicians had chance to examine only a short portion of the GI tract. Luckily only esophagogastroduodenoscopy and colonoscopy had the ability to diagnose and treat most of GI disturbances as we still experience in our daily practice that diseases associated with small bowel are comparably less to ones that involve upper GI and colon. The initial technique for small bowel endoscopy is push enteroscopy which was needed to be improved due to restricted capability of investigation depth. Single and double balloon enteroscopy (DBE) are now better procedures with improved visualization capability that gives physicians to examine the whole small bowel. By combining either upper or lower GI investigations now we have the opportunity to visualize the whole GI tract. These novel types of endoscopic procedures increase the effectiveness of diagnosis and minimally invasive treatments of small bowel and reduce the need for surgical interventions. This review aims to summarize indications, clinical importance and complications of DBE.
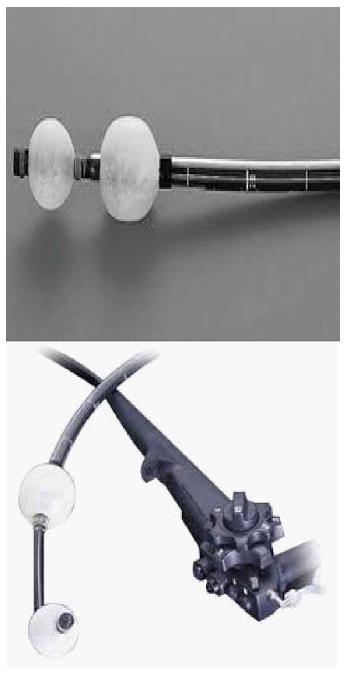
DBE system consists of a high-resolution video endoscope, with a working length of 200 cm and a flexible overtube made of polyurethane. Latex balloons are attached at the tip of the endoscope and also on the overtube, and can be filled with air or emptied using a pressure controlled pump. The principle of the DBE technique is based on alternating pushing and pulling maneuvers, in order to place the small bowel segments onto the overtube step by step[1]. DBE can be performed via oral or anal route according to the clinical decision. Twelve hours of food and approximately 4 h of clear liquid fasting will be enough for the patient preparation of oral DBE. However standard colonoscopy preparation with restricted diet and laxatives will be needed for retrograde examination[2]. Peroperative sedation is necessary as the procedure duration is long and lower patient tolerance is expected to disturb the success of the procedure. Many options can be used for sedation but conventional conscious sedation with propofol is mainly used. Deep monitored sedation (with propofol, midazolam and/or fentanyl) can be preferred for oral examination with prolonged duration of the procedure[3]. Radiologic fluoroscopic assistance can be used according to the endoscopist’s preference. The goal of the procedure is to examine the whole small bowel from duodenum to caecum or vice versa. However total enteroscopy can be performed in approximately 20% to 70% of the patients. Using both routes (oral and anal) complementary to each other by signing the furthest depth by tattooing or clip application, increases total enteroscopy rates. 230 cm beyond Treitz and 135 cm proximal to ileocecal valve can be considered as the average insertion depths for oral and anal route according to many different case series in the literature (Figure 1).
The indications of DBE mainly consist of similar pathologies of upper and lower GI system that are localized or suspected to be in the small intestine. As the procedure takes long time and is an advanced and hard intervention, it is mostly indicated after some initial investigations. The indications and some interventions due to diagnosis are summarized on Table 1.
| Indications | Therapeutic interventions |
| Mid-gastrointestinal bleeding | Endoscopic hemostatic therapies |
| Injection sclerotherapy | |
| Argon plasma coagulation | |
| Endoscopic hemostatic clip application | |
| Abnormal findings in other examinations | Diagnosis and therapy |
| Polyps of the small bowel (e.g., polyposis syndromes) | Endoscopic polypectomy |
| Crohn's diseases | Diagnostic sampling |
| Diagnosis, complications | Balloon dilatation for strictures |
| Foreign body ingestion | Foreign body removal |
| Small bowel tumors | Diagnostic sampling |
| Self-expanding stents for obstruction | |
| Endoscopic retrograde cholangiography in surgically altered anatomy | Diagnosis |
| Stone extraction | |
| Dilatation | |
| Stenting | |
| Incomplete colonoscopy due to technical difficulty | Complete colonoscopy |
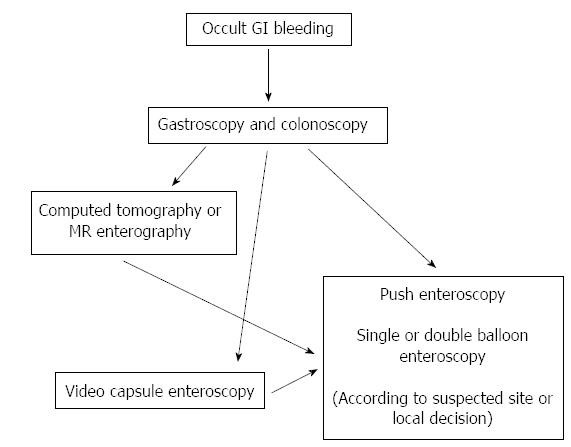
The most common indication (up to half of the procedures) for DBE is suspected or known mid-GI bleeding which refers to the blood loss from the distance between papilla Vateri and ileocecal valve. This can be either occult or obscure which may suggest an idea to choose the beginning route for the procedure, where melena encourages the oral route, the occurrence of hematochesia which cannot be defined by routine colonoscopy suggests retrograde examination for the initial management[4,5]. Video capsule endoscopy (VCE) is mostly the first choice to investigate occult mid-GI bleeding and after diagnosis of bleeding site or determining the need for additional intervention DBE is performed as a completing procedure[6]. DBE has up to 90% of diagnostic yield for mid GI bleeding which is comparable to VCE and significantly better than push enteroscopy as having the advantage of improved insertion depth[7]. As an alternative, push enteroscopy has been proven to have a diagnostic yield from 12% to 80% in investigating mid-GI bleeding, and higher rates are achieved when the bleeding is obscure (Figure 2).
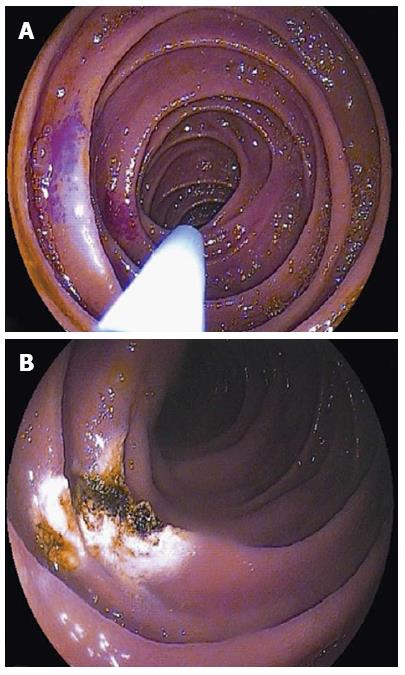
Beyond diagnostic accuracy DBE brings the advantage of therapeutic interventions and ability to obtain tissue samples which is a great advantage when compared to VCE[8]. Clinician can perform endoscopic hemostatic techniques for bleeding sites at the time of diagnosis even documented initially with another examination (i.e., radiological, scintigraphic or angiographic) or not. Also lesions that cause bleeding (i.e., angiodysplasia, polyps, small bowel tumors, foreign bodies...) diagnosed by using VCE can be reached with DBE for further tissue sampling or therapeutic interventions[9,10]. When the bleeding is severe and persistent or the probability of intervention is strong, DBE can take the first place instead of VCE (Figure 3).
The interventional advantage offers DBE to be performed after abnormal findings of an initial diagnostic modality. Computed tomography (CT), magnetic resonance imaging (MRI) and VCE findings with suspected lesions can be confirmed and further applications can be performed with DBE. Also with suspected or known strictures of the small bowel, DBE comes further than VCE in order to avoid retention of the capsule and DBE becomes the initial approach for the patient[8].
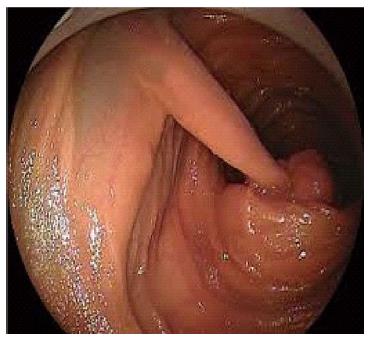
The use of DBE in polyposis syndromes such as Familial Adenomatous Polyposis and Peutz Jeghers syndrome can be for screening and interventions for symptomatic patients (i.e., bleeding or partial obstruction)[11]. Polyps larger than 15 mm are considered to bring tendency to intussusception and are recommended to be removed. VCE is mainly used for detecting the large polyps or for surveillance, but DBE is encouraged to be performed for polypectomy instead of surgery. Patients with obstruction are treated with surgery and most of these patients that underwent surgery have intraabdominal adhesions. The risk of getting stuck and iatrogenic obstruction with capsule itself limits the use of CE in this setting and DBE becomes mainly the first choice for even surveillance of the small bowel. The opportunity for polypectomy and mechanical dilatation of the intestinal strictures are the other unique advantages of DBE against other diagnostic tools[12] (Figures 4 and 5).
DBE is not the first choice for the diagnosis of Crohn’s disease (CD), but suspicion of the disease with only small bowel involvement and follow up of the strictures to confirm even inflammatory or fibrotic to modify the treatment of the patient would bring the need for using DBE in the diagnostic side of this disease. Also tissue sampling for suspected malignancy on CD and ability to dilate the strictures in the small bowel other implementations of DBE in CD[13]. Endoscopic confirmation of strictures to be inflammatory or fibrotic is of great importance to steer the treatment. Inflammatory strictures are suitable candidates for medical therapy where fibrotic strictures need mechanical interventions such as dilatation or surgery. Endoscopic dilatation therapy is an option for short (< 3-4 cm), fibrotic strictures mainly due to scar tissues. The recurrence of strictures and need for repetitive dilatation or surgery is observed in a wide range and this information needs further investigations to be determined[14] (Figure 6).
Ligament of Treitz is one of the anatomical narrow points where the intestinal passage is relatively altered. However foreign bodies may pass this anatomical site and reach small bowel easily. The foreign bodies that are beyond the reach of gastroscopy and colonoscopy are candidates for DBE. Foreign bodies can be observed in pathologically narrowed intestinal sites such as tumors, strictures and large polyps. Even wireless capsules used for VCE can get stuck and need to be removed with DBE. Potentially harmful foreign bodies such as needles can be safely removed by using DBE with the help of overtube.
Suspected small bowel lymphoma in Celiac disease and a solitary mass of small bowel documented in an initial diagnostic procedure can be the indication to perform DBE. As small bowel tumors can be seen nearly 5% of patients with mid GI bleeding, direct visualization of the lesion and histologic sampling before surgical intervention is crucial and DBE is the choice of initial procedure[15]. Also tattooing with DBE prior to surgery would be useful for surgeons to perform the most suitable surgical design (Figure 7).
DBE gives clinicians the chance to perform endoscopic retrograde cholangiopancreatography in patients with Bilroth II and Roux-en-Y anastomosis who have altered anatomy due to surgery. This approach can be both diagnostic or interventional such as stone extraction, dilatation or biliary stenting. Also patients who underwent bariatric surgery and gastric bypass have a long descending small bowel loop that lead to the afferent loop which can obtain access to the duodenum or the gastric remnant. DBE is used to pass this prolonged route in order to reach the biliary system.
DBE can also be used in patients who could not have complete ileocolonoscopy due to technical difficulties such as adhesions.
Procedure related complications differ according to the content of the examination. A procedure without therapeutic intervention brings low rates of complications. Due to prolonged procedure and air insufflation, abdominal pain can be observed in up to 20% patients. Acute pancreatitis with a rate of 0.3%-0.4% is the most common complication for oral route. It is supposed to be the result of increased pressure at the site of major papilla and ischemia of pancreas due to push and pull maneuvers. When therapeutic intervention is used complication rates increase up to 10% (perforation or bleeding following polypectomy or mucosal resection)[9,13,16]. Patients who had previous abdominal surgery and altered anatomy has greater risk of complications. Also prolonged sedation beyond from the procedure itself has the risk of respiratory depression and aspiration with a rate of 1%. Experience of the endoscopist, shorter time of procedure and inflating the balloons distal to Treitz ligament are the clues to reduce the rate of complications.
The contraindications for DBE are the same as conventional upper or lower GI endoscopic procedures. These are presence of shock, acute myocardial infarction, fulminant colitis, acute perforation and peritonitis. Intraabdominal adhesions increase the difficulty of the procedure and limit the depth of insertion but they are not counted as a contraindication.
VCE is a good alternative or an initial procedure to use as a diagnostic tool mainly investigating mid-GI bleeding. However the inability of intervention is the main drawback of VCE. Three meta-analyses in the literature of DBE vs VCE showed similar diagnostic yields in patients with obscure GI bleeding[17-19]. A retrospective study of 162 patients demonstrated an advantage of VCE where it is technically hard to reach with DBE and superiority of DBE in patients with Roux-en-Y loop anatomy and diverticula. Overall, the diagnostic yield for DBE vs VCE appears to be similar. VCE has the advantage of being noninvasive and is more likely to achieve complete small bowel enteroscopy. As VCE can be performed in outpatient setting without sedation it does not carry the additional risks of anesthesia.
In most clinical scenario the initial approach is VCE and after addressing the site of pathology DBE is used for sampling or therapeutic intervention. This sequential approach decreases the procedure duration and enhances interventional success.
Single balloon enteroscopy (SBE) is another alternative procedure for similar indications with similar capabilities. Limited number of trials that compare SBE and DBE have showed that they have similar diagnostic and therapeutic yield. However DBE seems to be more effective in performing complete enteroscopy[20-23].
Intraoperative enteroscopy (IOE) is an another alternative but after development of balloon enteroscopy techniques, IOE is not of initial choice as it is incomparably invasive.
DBE was first introduced by Yamamoto et al[1] In 2001. Evolving technologic advances and experience of the clinicians has made this particularly difficult procedure to be highly effective and safe for evaluation of the small bowel[24]. Growing experience more than a decade provided the chance to examine the whole intestinal system via oral or rectal route. DBE has reduced the need of surgery for small intestinal diseases. Despite its high diagnostic yield the complications of the procedure are reasonable and can be reduced with experience and basic precautions. Despite the easy use of VCE DBE will remain an important small intestinal examination as it has the ability of therapeutic intervention and tissue sampling. Cumulative experience of the endoscopist increase the success and insertion depth when reducing the complications and duration of the procedure. This knowledge suggest that DBE should be best performed in referral centers by educated endoscopists. Also use of carbon dioxide insufflation instead of ambient air increases insertion depth and patient tolerance during the procedure[25,26].
P- Reviewer: Botaitis SC, Chow WK, Wang DR S- Editor: Tian YL L- Editor: A E- Editor: Zhang DN
| 1. | Yamamoto H, Sekine Y, Sato Y, Higashizawa T, Miyata T, Iino S, Ido K, Sugano K. Total enteroscopy with a nonsurgical steerable double-balloon method. Gastrointest Endosc. 2001;53:216-220. |
| 2. | Gerson LB, Flodin JT, Miyabayashi K. Balloon-assisted enteroscopy: technology and troubleshooting. Gastrointest Endosc. 2008;68:1158-1167. |
| 3. | Choi H, Choi KY, Eun CS, Jang HJ, Park DI, Chang DK, Kim JO, Ko BM, Lee MS, Huh KC. Korean experience with double balloon endoscopy: Korean Association for the Study of Intestinal Diseases multi-center study. Gastrointest Endosc. 2007;66:S22-S25. |
| 4. | Sun B, Rajan E, Cheng S, Shen R, Zhang C, Zhang S, Wu Y, Zhong J. Diagnostic yield and therapeutic impact of double-balloon enteroscopy in a large cohort of patients with obscure gastrointestinal bleeding. Am J Gastroenterol. 2006;101:2011-2015. |
| 5. | May A, Nachbar L, Ell C. Double-balloon enteroscopy (push-and-pull enteroscopy) of the small bowel: feasibility and diagnostic and therapeutic yield in patients with suspected small bowel disease. Gastrointest Endosc. 2005;62:62-70. |
| 6. | Pohl J, Delvaux M, Ell C, Gay G, May A, Mulder CJ, Pennazio M, Perez-Cuadrado E, Vilmann P. European Society of Gastrointestinal Endoscopy (ESGE) Guidelines: flexible enteroscopy for diagnosis and treatment of small-bowel diseases. Endoscopy. 2008;40:609-618. |
| 7. | Heine GD, Hadithi M, Groenen MJ, Kuipers EJ, Jacobs MA, Mulder CJ. Double-balloon enteroscopy: indications, diagnostic yield, and complications in a series of 275 patients with suspected small-bowel disease. Endoscopy. 2006;38:42-48. |
| 8. | Nakamura M, Niwa Y, Ohmiya N, Miyahara R, Ohashi A, Itoh A, Hirooka Y, Goto H. Preliminary comparison of capsule endoscopy and double-balloon enteroscopy in patients with suspected small-bowel bleeding. Endoscopy. 2006;38:59-66. |
| 9. | Xin L, Liao Z, Jiang YP, Li ZS. Indications, detectability, positive findings, total enteroscopy, and complications of diagnostic double-balloon endoscopy: a systematic review of data over the first decade of use. Gastrointest Endosc. 2011;74:563-570. |
| 10. | Chen WG, Shan GD, Zhang H, Li L, Yue M, Xiang Z, Cheng Y, Wu CJ, Fang Y, Chen LH. Double-balloon enteroscopy in small bowel tumors: a Chinese single-center study. World J Gastroenterol. 2013;19:3665-3671. |
| 11. | Akarsu M, Uğur Kantar F, Akpinar H. Double-balloon endoscopy in patients with Peutz-Jeghers syndrome. Turk J Gastroenterol. 2012;23:496-502. |
| 12. | Jovanovic I, Vormbrock K, Zimmermann L, Djuranovic S, Ugljesic M, Malfertheiner P, Fry LC, Mönkemüller K. Therapeutic double-balloon enteroscopy: a binational, three-center experience. Dig Dis. 2011;29 Suppl 1:27-31. |
| 13. | Schulz C, Mönkemüller K, Salheiser M, Bellutti M, Schütte K, Malfertheiner P. Double-balloon enteroscopy in the diagnosis of suspected isolated Crohn’s disease of the small bowel. Dig Endosc. 2014;26:236-242. |
| 14. | Möschler O, May A, Müller MK, Ell C. Complications in and performance of double-balloon enteroscopy (DBE): results from a large prospective DBE database in Germany. Endoscopy. 2011;43:484-489. |
| 15. | Onal IK, Akdogan M, Arhan M, Yalinkilic ZM, Cicek B, Kacar S, Kurt M, Ibis M, Ozin YO, Sayilir A. Double balloon enteroscopy: a 3-year experience at a tertiary care center. Hepatogastroenterology. 2012;59:1851-1854. |
| 16. | Van Assche G, Vermeire S, Rutgeerts P. Endoscopic therapy of strictures in Crohn’s disease. Inflamm Bowel Dis. 2007;13:356-358; discussion 356-358. |
| 17. | Chen X, Ran ZH, Tong JL. A meta-analysis of the yield of capsule endoscopy compared to double-balloon enteroscopy in patients with small bowel diseases. World J Gastroenterol. 2007;13:4372-4378. |
| 18. | Pasha SF, Leighton JA, Das A, Harrison ME, Decker GA, Fleischer DE, Sharma VK. Double-balloon enteroscopy and capsule endoscopy have comparable diagnostic yield in small-bowel disease: a meta-analysis. Clin Gastroenterol Hepatol. 2008;6:671-676. |
| 19. | Teshima CW, Kuipers EJ, van Zanten SV, Mensink PB. Double balloon enteroscopy and capsule endoscopy for obscure gastrointestinal bleeding: an updated meta-analysis. J Gastroenterol Hepatol. 2011;26:796-801. |
| 20. | Arakawa D, Ohmiya N, Nakamura M, Honda W, Shirai O, Itoh A, Hirooka Y, Niwa Y, Maeda O, Ando T. Outcome after enteroscopy for patients with obscure GI bleeding: diagnostic comparison between double-balloon endoscopy and videocapsule endoscopy. Gastrointest Endosc. 2009;69:866-874. |
| 21. | May A, Färber M, Aschmoneit I, Pohl J, Manner H, Lotterer E, Möschler O, Kunz J, Gossner L, Mönkemüller K. Prospective multicenter trial comparing push-and-pull enteroscopy with the single- and double-balloon techniques in patients with small-bowel disorders. Am J Gastroenterol. 2010;105:575-581. |
| 22. | Domagk D, Mensink P, Aktas H, Lenz P, Meister T, Luegering A, Ullerich H, Aabakken L, Heinecke A, Domschke W. Single- vs. double-balloon enteroscopy in small-bowel diagnostics: a randomized multicenter trial. Endoscopy. 2011;43:472-476. |
| 23. | Takano N, Yamada A, Watabe H, Togo G, Yamaji Y, Yoshida H, Kawabe T, Omata M, Koike K. Single-balloon versus double-balloon endoscopy for achieving total enteroscopy: a randomized, controlled trial. Gastrointest Endosc. 2011;73:734-739. |
| 24. | Delvaux M, Gay G. International Conference on Capsule and Double-Balloon Endoscopy (ICCD). Paris, 27-28 August 2010. Endoscopy. 2011;43:533-539. |
| 25. | Domagk D, Bretthauer M, Lenz P, Aabakken L, Ullerich H, Maaser C, Domschke W, Kucharzik T. Carbon dioxide insufflation improves intubation depth in double-balloon enteroscopy: a randomized, controlled, double-blind trial. Endoscopy. 2007;39:1064-1067. |
| 26. | Hirai F, Beppu T, Nishimura T, Takatsu N, Ashizuka S, Seki T, Hisabe T, Nagahama T, Yao K, Matsui T. Carbon dioxide insufflation compared with air insufflation in double-balloon enteroscopy: a prospective, randomized, double-blind trial. Gastrointest Endosc. 2011;73:743-749. |