Published online Sep 25, 2015. doi: 10.4253/wjge.v7.i13.1107
Peer-review started: March 29, 2015
First decision: May 13, 2015
Revised: May 24, 2015
Accepted: August 30, 2015
Article in press: August 31, 2015
Published online: September 25, 2015
Processing time: 179 Days and 16.7 Hours
Pseudoaneurysm is a known complication of pancreatitis associated with significant mortality and morbidity. Imaging plays an important role in the diagnosis and management. Computed tomography (CT) helps localize the lesion and the severity of the background pancreatitis but digital subtraction angiography with coil embolization is recommended to avoid bleeding and inadvertent surgery. However, in cases where angiographic coil embolization is not feasible due to technical reasons, thrombin injection via CT or ultrasound guidance remains a viable option and often described in literature. In this series, effort has been made to highlight the role of endoscopic ultrasound guided thrombin instillation especially in patients with poorly visualized pseudoaneurysm on ultrasound thereby avoiding surgery and the associated mortality and morbidity.
Core tip: In cases where angiographic coil embolization is not feasible due to technical reasons, thrombin injection via computed tomography or ultrasound guidance remains a viable option. Endoscopic ultrasound guided thrombin injection is a new development in this realm especially in those patients where the visualization of the pseudoaneurysm is difficult on transabdominal ultrasound thereby avoiding the need of surgery and the associated morbidity.
- Citation: Gamanagatti S, Thingujam U, Garg P, Nongthombam S, Dash NR. Endoscopic ultrasound guided thrombin injection of angiographically occult pancreatitis associated visceral artery pseudoaneurysms: Case series. World J Gastrointest Endosc 2015; 7(13): 1107-1113
- URL: https://www.wjgnet.com/1948-5190/full/v7/i13/1107.htm
- DOI: https://dx.doi.org/10.4253/wjge.v7.i13.1107
Pancreatitis is associated with high morbidity and mortality. Pseudoaneurysm is a commonly seen fatal complication of pancreatitis, noted in 10% of patients with chronic pancreatitis with the risk of rupture as high as 50% and the mortality after rupture as high as 15%-40%[1,2]. Hence, prompt diagnosis and treatment of pseudoaneurysm is recommended. Diagnostic modality like computed tomography (CT) angiography helps in picking up the lesion and delineating the vessel of origin however, digital subtraction angiography (DSA) and subsequent coil embolization is necessary to occlude the pseudoaneurysm to eliminate the risk of rupture and uncontrolled bleeding. Occasionally, coil embolization is not possible due to varied reasons like inaccessible vascular territory due to small caliber vessel or short neck of pseudoaneurysm. Some pseudoaneurysms may be angiographically occult and seen on ultrasound or CT only. In such cases ultrasound or CT guided percutaneous thrombin injection can be performed. Endoscopic ultrasound (EUS) guided thrombin injection is a new development in this realm especially in those patients where the visualization of the lesion is difficult on transabdominal ultrasound thereby avoiding the need of surgery and the associated morbidity. However, it requires a great deal of expertise. We review a few cases where pseudoaneurysms were occluded using endoscopic guided thrombin injection in our hospital.
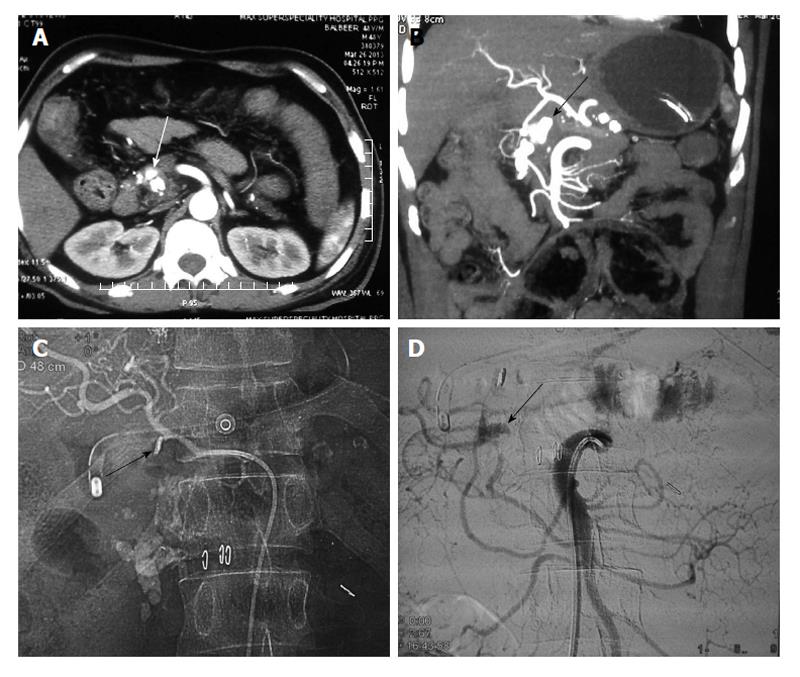
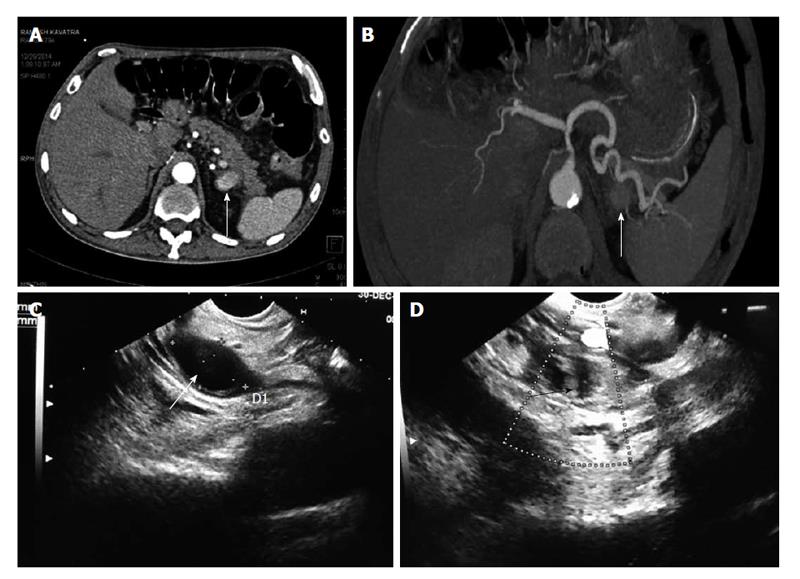
We encountered three cases of pancreatitis related pseudoaneurysms, which were technically difficult to manage by endovascular route either because of previous surgical clipping of gastroduodenal artery by a laparoscopic surgeon (Figure 1) or that were angiographically occult.
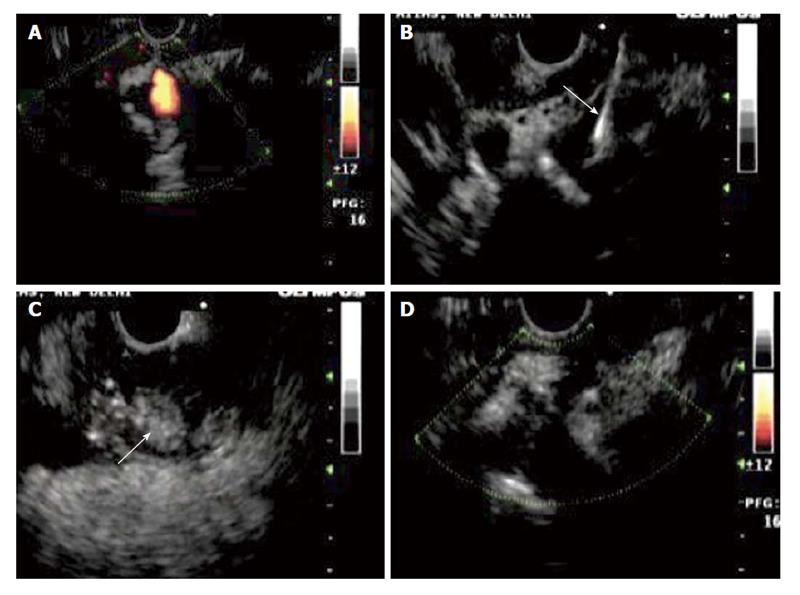
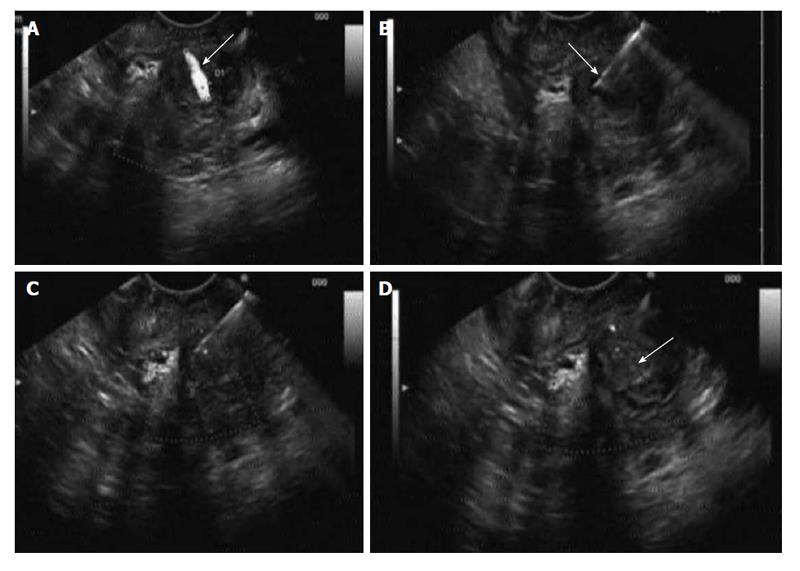
In our center, in hemodynamically stable patients, the usual approach to manage the pancreatitis related pseudoaneurysm is to perform CT angiography for localization of pseudoaneurysm and also to provide road map for endovascular/surgical approach. Subsequently DSA is performed, depending upon the location of pseudoaneurysm on CT angiography; selective cannulation of the culprit vessel is done. If we are able to reach the pseudoaneurysm, coil embolisation is done by occluding the back door, neck and front door of the pseudoaneurysm, so that there is no collateral re-filling of pseudoaneurysm. In our present series, we could not reach the pseudoaneurysm by endovascular route due to the reasons mentioned in Table 1. In all three cases, we attempted endoscopic ultrasound guided thrombin injection to treat these technically difficult pseudoaneurysms, after discussing with gastroenterologist experienced in EUS guided procedures. All these three pseudoaneurysms were easily visible on endoscopic ultrasound (Figure 2), which was performed prior to the thrombin injection for technical feasibility.
| Cases | Age/sex | Clinical presentation | Etiology of pancreatitis | Artery involved | Reason for angiographic failure | Amount of thrombin used | Follow up imaging | Figure No. |
| 1 | 56/M | Pancreatitis with UGI bleed | Chronic alcoholic | Gastroduodenal artery | Previous surgical clipping | 500 IU | Thrombosed | Figures 1-3 |
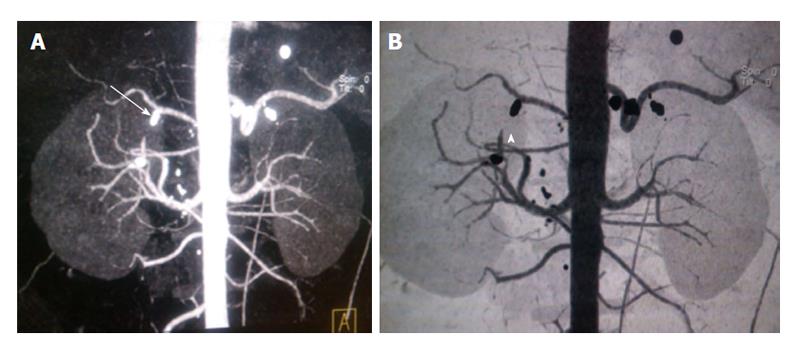
| 2 | 45/M | Pancreatitis with UGI bleed | Gall stone disease | Splenic artery | Not seen on DSA | 300 IU | Thrombosed | Figures 4 and 5 |
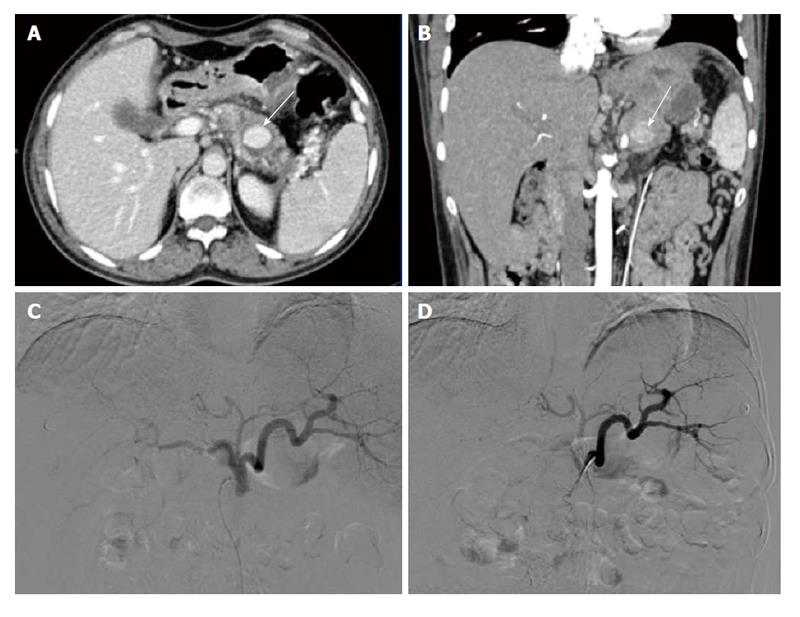
| 3 | 30/M | Pancreatitis with UGI bleed | Gall stone disease | Splenic artery | Not seen on DSA | 400 IU | Thrombosed | Figure 6 |
Gastroenterologist, who has got experience in EUS guided procedures, in collaboration with interventional radiologist performed this procedure. The procedure was performed without any anaesthesia. Initially EUS was performed using curved linear array transducer (Olympus-GF-UCT180) in conjunction with EVIS EXERA II CLV-180 light source (Olympus Medical system Corp, Tokyo, Japan) was performed, pseudoaneurysm was localized and shortest path was chosen to target the pseudoaneurysm. We used the thrombin component of a Tisseel® kit (Baxter AG; Vienna, Austria), containing thrombin 500 IU/mL. Prior to targeting the pseudoaneurysm, thrombin component of Tisseel kit was reconstituted with 1 mL of calcium chloride and the reconstituted 1 mL thrombin was further diluted with normal saline to a total of 5 mL, so that each milliliter of reconstituted solution contains 100 IU of thrombin. Now, each milliliter of reconstituted thrombin was transferred to 1 mL insulin syringe and five such thrombin-loaded syringes were kept ready. Using 22G Echo Tip Ultra endoscopic ultrasound needle (Cook Medical Endoscopy, IN, United States), pseudoaneurysm was punctured under endoscopic ultrasound guidance, and then thrombin was injected in aliquots of 100 IU till the pseudoaneurysm become echogenic resulting in thrombosis. Under color Doppler, success of thrombosis was confirmed and the needle was removed when no color filling was seen inside the pseudoaneurysm sac. The entire procedure from start of localization of pseudoaneurysm to complete thrombosis of pseudoaneurysm lasted for about 15-20 min. After the procedure, patients were monitored closely for signs of internal bleeding. None of our patients developed any immediate or late complications. The next day, repeat EUS was done to reconfirm the success of the procedure. In one case we performed, CT angiography to confirmed the success of procedure (Figure 3). All three patients showed complete thrombosis of pseudoaneurysm on next day EUS. Clinical follow up was done after a month and none of these patients had recurrence of symptoms of bleeding.
Pseudoaneurysm formation is a known vascular complication of acute pancreatitis due to vessel injury as a result of proteolytic and lipolytic enzymes released due to severe inflammation and pancreatic necrosis[3].
The management of psuedoaneurysm in the setting of pancreatitis is challenging in view of the associated risk of rupture and haemodynamic compromise besides the background association of increased morbidity in pancreatitis itself. A diagnostic modality like CT angiography remains a preliminary imaging modality in acute pancreatitis. This provides a vascular road-map to the vessel of origin of the aneurysm besides adding vital information on the background pancreatitis.
DSA with coil embolization is the gold standard treatment. This offers the advantage of avoiding the associated surgical risks. Besides, it ensures adequate thrombosis of the pseudoaneurysm in most cases.
In situations where the access to the pseudoaneurysm is not possible due to previous clipping/tortuous anatomy (case 1) or not visible on DSA due to slow filling and narrow neck (Figure 4), angiographic coil embolization may not be feasible. Some pseudoaneurysms are occult and detected only with other imaging modality such as CT or endoscopic ultrasound, as seen in one of our case (Figure 5). If left alone, these pseudoaneurysms can rupture or rebleed. The risk of rupture in pancreatic pseudoaneurysms has been as high as 15%-40%[1]. So, embolization is necessary to avoid rupture and rebleeding. Thrombin remains an alternative to coils. It can be instilled directly at the bleeding site and the flow cessation can be assessed. Thombin is a good alternative in those cases not feasible by endovascular route. The success of thrombin for embolization of peripheral pseudoaneurysms[4-6] as well as those of pancreas[7-10] have been described in literature.
Thrombin can be given through transcutaneous route through ultrasound or CT guidance. However, in our patients transabdominal ultrasound could not delineate the lesion clearly posing great challenge for thrombin instillation. EUS was the next step as most of these pseudoaneurysms were in the vascular territory in the vicinity of the peripancreatic region. The advantage of EUS lies in clearly delineating the extent and size of the pseudoaneurysm. Instillation of thrombin under EUS guidance requires a great deal of expertise. Thrombin could ensure immediate occlusion of pseudoaneurysms in all cases (Figure 6). Response assessment can also be done easily. The hallmark finding is the complete thrombosis of the pseudoaneurysm. No associated complications were noted. Follow up scans did not reveal rebleeding or rupture in our cases.
There are very few literature describing the use of EUS guided thrombin instillation of pancreatic pseudoaneurysm. In one of the earliest description Roach et al[11] described the EUS guided thrombin occlusion of a pseudoaneurysm arising from a branch of the superior mesenteric artery in a patient presenting with upper gastrointestinal bleed. This was done following failure to embolise angiographically as the feeding artery could not be catheterized.
Use of thrombin is recommended in cases of haemodynamically stable patients with small pseudoaneurysm[12]. Also it can be used in large lesions as an adjunct to coil embolization.
In haemodynamically unstable patients and those with large pseudoaneurysms or those with failure after repeated embolization, surgery remains the only option. But in the setting of pancreatitis, surgery is associated with a grim outcome. Non-invasive imaging modalities like ultrasound and CT have provided good alternatives as means of thrombin instillation. The advent of thrombin instillation through EUS guidance has opened an altogether new arena for managing the difficult pseudoaneurysms and thereby avoiding the surgical risks. Though one cannot undermine the expertise needed in EUS guidance, it offers a new hope to this special group of patients.
Some limitations of thrombin instillation, though rare, include risk of distal thrombosis though thrombin is rapidly diluted and inactivated by fast flowing blood stream[10]. Immunological reactions like sensitivities and cross-reactions are also known[10]. Recanalization after initial successful thrombosis of pseudoaneurysm is another complication. Lastly, the duration of follow-up required after treatment of pseudoaneurysms is not known.
The use of EUS guided thrombin instillation provides a new option for management of pseudoaneurysms caused by pancreatitis specially for those cohort of patients inaccessible angiographically or through transabdominal ultrasound. The avoidance of high risk surgeries, prompt occlusion of the pseudoaneurysm and ease of monitoring and follow-up are the hallmark features of this method though studies are needed to provide data as to efficacy of this method.
The three middle-aged male patients presented with similar symptom of upper gastrointestinal bleeding. One patient had surgical clipping of gastroduodenal artery.
Upon physical examination, all three patients were haemodynamically stable except for tachycardia. Pulse rates were in range of 110-120/min. No other significant physical findings noted.
Pancreatitis related bleeding pseudoaneurysm, variceal bleeding, peptic ulcer disease.
All the patients had low hemoglobin level (range of 4-7 gm/dL). Upper gastrointestinal endoscopy showed blood clots within the stomach and duodenum. No active bleeding site could be seen on endoscopy.
All three patients had contrast enhanced computed tomography showed pseudoaneurysm arising from gastroduodenal artery (patient 1) and splenic artery (patients 2 and 3). There was evidence of surgical clip at the gastroduodenal (GDA) origin and chronic calcific pancreatitis in first patient.
All the patients underwent digital substraction angiography. In first patient pseudoaneurysm could not be reached due to previous surgical clipping of GDA and tortuous collaterals feeding the pseudoaneurysm. In rest two patients, pseudoaneurysms were occult on angiography. All three patients were successfully managed by endoscopic ultrasound (EUS) guided thrombin injection in to the pseudoaneurysm.
Thrombin injection into the iatrogenic related peripheral pseudoaneurysm is well known. Very few cases describing the use of EUS guided thrombin instillation of pancreatic pseudoaneurysm have been reported in literature. The advent of thrombin instillation through EUS guidance has opened an altogether new arena for managing the difficult pseudoaneurysms and thereby avoiding the surgical risks.
Thrombin (bovine/human), is available as powder form and is reconstituted with calcium chloride solution, injected into the pseudo aneurysm after direct puncture percutaneously under image guidance. Thrombin converts fibrinogen into fibrin resulting in formation of clots.
This case series represents a new option of EUS guided thrombin instillation for management of pseudoaneurysms caused by pancreatitis especially for that cohort of patients where pseudoaneurysm is inaccessible angiographically.
This is an interesting paper highlighting a method of occluding pseudoaneurysms, which are otherwise difficult to reach.
P- Reviewer: Agresta F, Aytac E, Ciaccio EJ, Seow-Choen F, Tham T S- Editor: Tian YL L- Editor: A E- Editor: Liu SQ
| 1. | Huizinga WK, Baker LW. Surgical intervention for regional complications of chronic pancreatitis. Int Surg. 1993;78:315-319. [PubMed] |
| 2. | Gambiez LP, Ernst OJ, Merlier OA, Porte HL, Chambon JP, Quandalle PA. Arterial embolization for bleeding pseudocysts complicating chronic pancreatitis. Arch Surg. 1997;132:1016-1021. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 103] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 3. | Flati G, Andrén-Sandberg A, La Pinta M, Porowska B, Carboni M. Potentially fatal bleeding in acute pancreatitis: pathophysiology, prevention, and treatment. Pancreas. 2003;26:8-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 148] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 4. | Elford J, Burrell C, Freeman S, Roobottom C. Human thrombin injection for the percutaneous treatment of iatrogenic pseudoaneurysms. Cardiovasc Intervent Radiol. 2002;25:115-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 37] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 5. | Friedman SG, Pellerito JS, Scher L, Faust G, Burke B, Safa T. Ultrasound-guided thrombin injection is the treatment of choice for femoral pseudoaneurysms. Arch Surg. 2002;137:462-464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 48] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 6. | Jaff MR. Pseudoaneurysms. Curr Treat Options Cardiovasc Med. 2002;4:239-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Luchs SG, Antonacci VP, Reid SK, Pagan-Marin H. Vascular and interventional case of the day. Pancreatic head pseudoaneurysm treated with percutaneous thrombin injection. AJR Am J Roentgenol. 1999;173:830, 833-834. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Francisco LE, Asunción LC, Antonio CA, Ricardo RC, Manuel RP, Caridad MH. Post-traumatic hepatic artery pseudoaneurysm treated with endovascular embolization and thrombin injection. World J Hepatol. 2010;2:87-90. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 29] [Article Influence: 1.9] [Reference Citation Analysis (1)] |
| 9. | Dambrin C, Marcheix B, Birsan T, Cron C, Muscari F, Suc B, Cérène A, Rousseau H. Posttraumatic pseudoaneurysm of the hepatic artery: treatment with ultrasound-guided percutaneous transhepatic thrombin injection. J Trauma. 2005;59:239-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Sparrow P, Asquith J, Chalmers N. Ultrasonic-guided percutaneous injection of pancreatic pseudoaneurysm with thrombin. Cardiovasc Intervent Radiol. 2003;26:312-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 35] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 11. | Roach H, Roberts SA, Salter R, Williams IM, Wood AM. Endoscopic ultrasound-guided thrombin injection for the treatment of pancreatic pseudoaneurysm. Endoscopy. 2005;37:876-878. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 31] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | Carr JA, Cho JS, Shepard AD, Nypaver TJ, Reddy DJ. Visceral pseudoaneurysms due to pancreatic pseudocysts: rare but lethal complications of pancreatitis. J Vasc Surg. 2000;32:722-730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 110] [Article Influence: 4.4] [Reference Citation Analysis (0)] |