Published online Jul 16, 2014. doi: 10.4253/wjge.v6.i7.324
Revised: May 10, 2014
Accepted: June 10, 2014
Published online: July 16, 2014
Processing time: 143 Days and 7.3 Hours
The use of hyaluronic acid and dextranomer (Solesta, Salix) injection in the anal canal is an emerging modality in the treatment of fecal incontinence. However, little is known regarding the endoscopic and radiological appearance following injection of this ano-rectal bulking agent. We report computed tomography and endoscopic findings after hyaluronic acid/dextranomer injection in the ano-rectal area.
Core tip: The use of hyaluronic acid and dextranomer (Solesta, Salix) injection in the ano-rectum is an emerging modality in the treatment of fecal incontinence. Our case discusses the endoscopic and radiological findings after injection of this bulking agent in the ano-rectal area.
- Citation: Papafragkakis H, Changela K, Bhatia T, Ona MA, Malieckal A, Paleti V, Fuksbrumer MS, Anand S. Endoscopic and imaging appearance after injection of an ano-rectal bulking agent. World J Gastrointest Endosc 2014; 6(7): 324-327
- URL: https://www.wjgnet.com/1948-5190/full/v6/i7/324.htm
- DOI: https://dx.doi.org/10.4253/wjge.v6.i7.324
Fecal incontinence (FI) is defined as the involuntary loss of liquid or solid stool for more than one month. The prevalence of FI ranges between 1.6% and 15%[1,2]. FI is an underdiagnosed condition that may cause psycho-social stigma and poses a clinical challenge to treat. The use of hyaluronic acid and dextranomer (Solesta, Salix) injection in the anal canal is an emerging modality in the treatment of fecal incontinence. However, little is known regarding the endoscopic and radiological appearance following injection of this ano-rectal bulking agent.
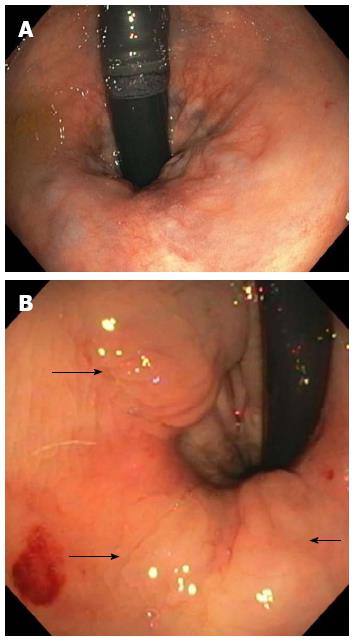
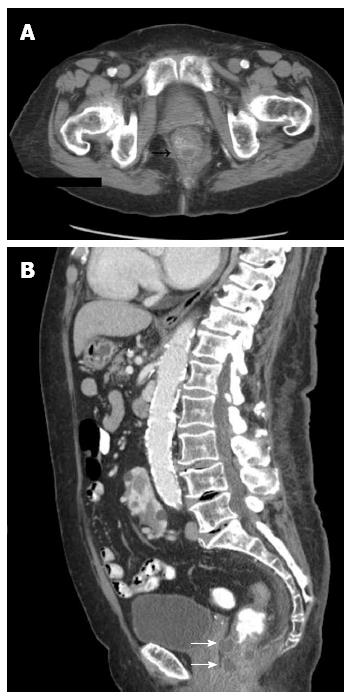
An 89-years-old woman underwent injection of hyaluronic acid/dextranomer in the anal canal for fecal incontinence under endoscopic guidance (Figure 1). Two days later, the patient had computed tomography (CT) scan of the abdomen and pelvis, which showed mural rectal thickening with multiple round hypodense foci within the rectal wall (Figure 2). Mucinous mural adenocarcinoma and abscess were among the radiological differential diagnosis.
We report a case of CT and endoscopic findings after hyaluronic acid/dextranomer injection in the ano-rectal area.
Current treatment options for FI include conservative measures, medications and surgery. Conservative approaches include pelvic floor muscle training, diet modifications, use of pads or plugs and biofeedback[3-5]. Biofeedback, assisted by a therapist and using electrodes placed on the abdomen and in the rectum, can help patients gain control of the pelvic musculature and improve FI symptoms. A study by Lacima et al[6] demonstrated that the majority of patients managed with biofeedback achieved 75% reduction in incontinence episodes or fully recovered compared to controls.
Medical management of FI commonly begins with antidiarrheals, such as loperamide, although their use is often limited by the development of constipation[7]. Amitriptyline, a tricyclic antidepressant, is also used for the management of FI, however, with modest efficacy[8]. Clonidine, a centrally acting α2 adrenergic agonist, has been demonstrated to reduce symptoms and increase incontinence-free days in women with predominantly urge-related fecal incontinence[9].
Invasive interventions are currently the last resort for the management of FI. They include sacral nerve stimulation, radiofrequency treatment and surgery. The exact mechanism of action of sacral nerve stimulators is not fully understood, but it is thought to be related to improved ano-rectal angulation and amplification of anal closing pressures[10]. Radiofrequency treatment causes a topical burn with subsequent remodeling and tightening of the ano-rectal muscles and has shown conflicting results in the management of FI[11]. More studies are needed to establish the efficacy and application of this treatment modality. Surgery remains the last resort for refractory FI. The long term results after sphincter repair are modest[12-14]. In patients with internal rectal prolapse, anterior rectopexy may be promising as an alternative surgical approach[15]. The use of an artificial anal sphincter or a magnetic anal sphincter are other novel surgical approaches, but more studies are needed to establish their use[16].
The use of hyaluronic acid/dextranomer (Solesta, Salix), a non-allergenic, biocompatible bulking agent, which causes a tissue-like formation in the anal canal can provide an alternative to surgical treatment when conservative management has failed. Hyaluronic acid/dextranomer (Solesta, Salix) applied through transanal submucosal injection provides support for the ingrowth of fibroblasts and collagen[17]. The 12-mo efficacy and safety of this ano-rectal bulking agent has been demonstrated in trials[10,18]. A recent study by La Torre et al[19] demonstrated the efficacy and durability of a hyaluronic acid/dextranomer agent 24 mo after use. Almost 63% of the patients demonstrated good response and had more than 50% reduction of incontinence episodes 24 mo after injection.
Hyaluronic acid/dextranomer application is increasing as more physicians are aware of its efficacy in the management of FI. However, little is known regarding the radiological and endoscopic appearance after its use. As demonstrated in our report, the CT findings may show mural rectal thickening with hypodense foci within the ano-rectal wall, which may mimic abscess or tumor. There have been anecdotal reports of surgical removal of ano-rectal bulking agent implants due to confusion about its appearance. These changes are likely permanent and therefore, it is important for gastroenterologists, surgeons and radiologists to be cognizant of the endoscopic and radiological appearance of the ano-rectum after hyaluronic acid/dextranomer injection and inquire about previous bulking agent injection in that area.
An 89-years-old woman underwent injection of hyaluronic acid/dextranomer in the anal canal for fecal incontinence under endoscopic guidance.
Fecal incontinence.
Mucinous mural adenocarcinoma, abscess.
Computed tomography (CT) scan axial view showed mural thickening with multiple rounded hypodense foci within the posterior rectal wall. CT scan sagittal view showed multiple rounded foci within the anterior and posterior rectal wall. Endoscopic view of post-hyaluronic acid/dextranomer (Solesta, Salix) injection showed the submucosal bulking property of the agent.
Submucosal injection of hyaluronic acid/dextranomer (Solesta, Salix) into the ano-rectum.
Little is known regarding the endoscopic and radiological appearance following injection of this ano-rectal bulking agent.
Hyaluronic acid/dextranomer (Solesta, Salix) is a non-allergenic, biocompatible bulking agent, which causes a tissue-like formation in the anal canal that can provide an alternative to surgical treatment when conservative management for fecal incontinence has failed.
As demonstrated in our report, computed tomography findings may show mural rectal thickening with hypodense foci within the ano-rectal wall after injection of the ano-rectal bulking agent, which may mimic the appearance of an abscess or tumor; thus, it is important for clinicians to be cognizant of the endoscopic and radiological appearance of the ano-rectum after hyaluronic acid/dextranomer injection, to inquire about previous bulking agent injection in the anal canal, and to include this in the differential diagnosis.
These authors showed the interesting finding of computed tomography and endoscopic findings after hyaluronic acid/dextranomer injection in the ano-rectal area. As it is demonstrated in their report, the computed tomography findings may show mural rectal thickening with hypodense foci within the ano-rectal wall, which may mimic abscess or tumor.
P- Reviewers: Kang SB, Milito G S- Editor: Song XX L- Editor: A E- Editor: Zhang DN
| 1. | Halland M, Talley NJ. Fecal incontinence: mechanisms and management. Curr Opin Gastroenterol. 2012;28:57-62. |
| 2. | Maeda Y, Laurberg S, Norton C. Perianal injectable bulking agents as treatment for faecal incontinence in adults. Cochrane Database Syst Rev. 2013;2:CD007959. |
| 3. | Deutekom M, Dobben AC. Plugs for containing faecal incontinence. Cochrane Database Syst Rev. 2012;4:CD005086. |
| 4. | Fader M, Cottenden AM, Getliffe K. Absorbent products for moderate-heavy urinary and/or faecal incontinence in women and men. Cochrane Database Syst Rev. 2008;CD007408. |
| 5. | Norton C, Cody JD. Biofeedback and/or sphincter exercises for the treatment of faecal incontinence in adults. Cochrane Database Syst Rev. 2012;7:CD002111. |
| 6. | Lacima G, Pera M, Amador A, Escaramís G, Piqué JM. Long-term results of biofeedback treatment for faecal incontinence: a comparative study with untreated controls. Colorectal Dis. 2010;12:742-749. |
| 7. | Read M, Read NW, Barber DC, Duthie HL. Effects of loperamide on anal sphincter function in patients complaining of chronic diarrhea with fecal incontinence and urgency. Dig Dis Sci. 1982;27:807-814. |
| 8. | Santoro GA, Eitan BZ, Pryde A, Bartolo DC. Open study of low-dose amitriptyline in the treatment of patients with idiopathic fecal incontinence. Dis Colon Rectum. 2000;43:1676-181; discussion 1676-181;. |
| 9. | Bharucha AE, Seide BM, Zinsmeister AR. The effects of clonidine on symptoms and anorectal sensorimotor function in women with faecal incontinence. Aliment Pharmacol Ther. 2010;32:681-688. |
| 10. | Graf W, Mellgren A, Matzel KE, Hull T, Johansson C, Bernstein M. Efficacy of dextranomer in stabilised hyaluronic acid for treatment of faecal incontinence: a randomised, sham-controlled trial. Lancet. 2011;377:997-1003. |
| 11. | Ruiz D, Pinto RA, Hull TL, Efron JE, Wexner SD. Does the radiofrequency procedure for fecal incontinence improve quality of life and incontinence at 1-year follow-up? Dis Colon Rectum. 2010;53:1041-1046. |
| 12. | Hool GR, Lieber ML, Church JM. Postoperative anal canal length predicts outcome in patients having sphincter repair for fecal incontinence. Dis Colon Rectum. 1999;42:313-318. |
| 13. | Londono-Schimmer EE, Garcia-Duperly R, Nicholls RJ, Ritchie JK, Hawley PR, Thomson JP. Overlapping anal sphincter repair for faecal incontinence due to sphincter trauma: five year follow-up functional results. Int J Colorectal Dis. 1994;9:110-113. |
| 14. | Vaizey CJ, Norton C, Thornton MJ, Nicholls RJ, Kamm MA. Long-term results of repeat anterior anal sphincter repair. Dis Colon Rectum. 2004;47:858-863. |
| 15. | Collinson R, Harmston C, Cunningham C, Lindsey I. The emerging role of internal rectal prolapse in the aetiology of faecal incontinence. Gastroenterol Clin Biol. 2010;34:584-586. |
| 16. | Wong MT, Meurette G, Stangherlin P, Lehur PA. The magnetic anal sphincter versus the artificial bowel sphincter: a comparison of 2 treatments for fecal incontinence. Dis Colon Rectum. 2011;54:773-779. |
| 17. | Stenberg A, Larsson E, Läckgren G. Endoscopic treatment with dextranomer-hyaluronic acid for vesicoureteral reflux: histological findings. J Urol. 2003;169:1109-1113. |
| 18. | Dodi G, Jongen J, de la Portilla F, Raval M, Altomare DF, Lehur PA. An Open-Label, Noncomparative, Multicenter Study to Evaluate Efficacy and Safety of NASHA/Dx Gel as a Bulking Agent for the Treatment of Fecal Incontinence. Gastroenterol Res Pract. 2010;2010:467136. |
| 19. | La Torre F, de la Portilla F. Long-term efficacy of dextranomer in stabilized hyaluronic acid (NASHA/Dx) for treatment of faecal incontinence. Colorectal Dis. 2013;15:569-574. |