Published online May 16, 2014. doi: 10.4253/wjge.v6.i5.148
Revised: March 31, 2014
Accepted: April 17, 2014
Published online: May 16, 2014
Processing time: 165 Days and 0.9 Hours
Laparoscopy, minimally invasive and minimal access surgery with more surgeons performing these advanced procedures. We highlight in the review several key emerging technologies such as the telementoring and virtual reality simulators, that provide a solid ground for delivering surgical education to rural area and allow young surgeons a safety net and confidence while operating on a newly learned technique.
Core tip: Telemedicine is becoming used more and more in today’s surgical practice. We highlight a new low cost telementoring prototype we developed that allows the delivery of better surgical education and delivering specialized expertise to rural areas. Telemedicine is a global term for a computer technology that allows medical information exchange from one location to another via telecommunication. Telemedicine helps in eliminating the distance barriers and provides medical expertise to rural communities.
- Citation: Bogen EM, Augestad KM, Patel HR, Lindsetmo RO. Telementoring in education of laparoscopic surgeons: An emerging technology. World J Gastrointest Endosc 2014; 6(5): 148-155
- URL: https://www.wjgnet.com/1948-5190/full/v6/i5/148.htm
- DOI: https://dx.doi.org/10.4253/wjge.v6.i5.148
Telemedicine is a global term for a computer technology that allows medical information exchange from one location to another via telecommunication. Telemedicine helps in eliminating the distance barriers and provides medical expertise to rural communities. There are several definitions of telemedicine, but a commonly used definition was proposed by The Society of American Gastrointestinal and Endoscopic Surgeons (SAGES): ‘‘The practice of medicine and/or teaching of the medical art, without direct physical physician-patient or physician-student interaction, via an interactive audio-video communication system employing tele-electronic devices’’[1].
Populations around the world are expanding; with the population of the United States of America expected to increase 50% by 2050, yet between 1980 and 2005 there was no increase in medical school enrollments. The funding of all postgraduate positions including general surgery has not changed significantly in the past 20 years[2]. Unless the rate at which general surgeons are trained increases, the number of general surgeons per population will continue to decline[3]. In 2003, Etzioni et al[4] found that as a result of an expanding/aging population, there would be a 31% increase in surgical work between 2001 and 2020. More recently, Williams et al[5] estimated that in 2030 there would be a 9% shortage in the general surgical workforce, with greater shortages in other surgical specialties. Due to the future shortage of surgeons, novel ways of surgical education should be explored. Surgical telementoring may be a solution to enhance and improve surgical education.
Surgical technique and technology has rapidly advanced, especially in the areas of laparoscopy. These advanced procedures of minimally invasive and minimal access surgeries are being performed by a greater number of surgeons. Learning to perform a new laparoscopic surgical technique can be extremely challenging, as it relies on the local mentor’s knowledge, skill level, and ability to communicate instructions to guide surgical students in their initial experience[6]. Sixty years ago, Gershon-Cohen began to send X-rays using facsimiles over a distance of 28 miles by using simple telephone service to transmit the images[7]. In 1962, DeBakey pioneered the field of telemedicine with the first video conferencing (VC) demonstration of open-heart surgery (Houston, Texas, United States) transmitted overseas via satellite, allowing real time viewing of an aortic valve replacement by medical staff in Geneva (Switzerland)[8]. Advances in both communication and computing technologies have allowed the development of a low cost and reliable solution for conveying telemedicine over great distances[2,9,10].
This paper is a semi systematic review. It is based on a PubMed search as well as the experience from the co-authors who are core researchers at the Norwegian National Centre of Telemedicine in the use of videoconferencing (KAM, HRHP, ROL). The search terms were: Telementoring, tele-mentoring, videoconferencing, video-conferencing. These terms were then combined with the search terms such as laparoscopic surgery and surgical education. Selected key articles and studies were chosen to emphasize the role of videoconferencing and telementoring in surgical education.
The objective of this paper is to explore the use of telementoring in surgical education.
VC has been in use in medical and surgical fields for many years. In recent years the technology has improved and become more accessible. Today almost every personal computer is able to perform basic videoconferencing at a low cost with relatively high quality.
The International Telecommunication Union (ITU) has defined several technical standards for videoconferencing equipment. ITU defined a standard to establish if the equipment can communicate properly and handle the data load sufficiently. Clear regulations for sound, video, parallel video streams, and data encryption as well patient security, confidentiality, and privacy were set under those standards[11].
Five methods for data transmission during videoconferencing are available today (Table 1): satellite communication, Internet Protocol (IP)-based communication, Integrated Services Digital Network (ISDN), third-generation (3G) and forth-generation (4G/LTE) Mobile phones.
| Type of technology used for VC communication | Bandwidth | Pros | Cons | Suitable for | Price |
| Satellite | ≥ 128 kb/s | Portable | Price time latency risk of poor video and audio quality | Disasters remote areas | 30-35000 USD |
| Worldwide use (i.e., areas with poor infrastructure) | Worldwide use (i.e., areas with poor infrastructure) | ||||
| IP-based/internet | Standard ≥ 768 kb/s | Easy access good quality of video | Varying quality of video dependable on internet traffic | Telementoring follow-up medical education standard VC | 50 USD/month - 70 Mbit line |
| Low prices for VC equipment and line rental | |||||
| ISDN | Normally 3 × 128 kb/s | Reasonably good video quality | Abandoned in the Western world in favor of 3G mobile phone and IP based telephony | Telementoring follow-up medical education | |
| 3G mobile phone | 3G mobile phone /modems | 64-500 kb/s | Portable rapidly evolving new networks | No data encryption low quality on video poor lens quality | 30 USD/month for 5Gb data plan |
| Unique mobile standard not compatible with ordinary VC equipment | Low prices for VC equipment and carrier subscription | ||||
| Emergency medicine | |||||
| 4G /LTE | 4G mobile phones / modems | 299.6 Mbit/s download and up to 75 Mbit/s upload | Varying quality of video dependable on internet traffic | Telementoring follow-up medical education standard VC |
VC has been in use among different specialties for many years. Common use of VC is in post-operative treatment and follow-up due to the relatively low costs, advancements in technology and the development of network infrastructures. Reported results of telementoring which is described as a natural fit in surgery[12], are improved surgical practice, education, treatment and postoperative care[13].
Remote presents and telementoring: The RP-7 (RP-7; Intouch Health, Santa Barbara, California) is an example of a high-end robotic remote presence system that can be controlled by a portable personal computer linked via Internet connection. Its dimensions are 165 cm in height and 63 cm × 76 cm at its base, comparable in size to that of an average human. The head of the robot is equipped with two advanced digital cameras, audio microphone and sophisticated engineering allows a real-time, two-way audio-video link. In addition the robot is highly maneuverable and allow a wide range of motions, e.g., panning and tilting[10].
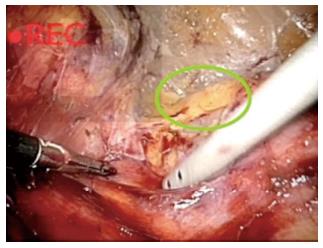
Sereno et al[14] Described a successful experiment using the previous version of the remote presence robot the RP-6 (predecessor to the RP-7). They have used two type of mentoring methods (1) the standard assistance called “active onsite mentoring” where the expert surgeon provides assistance with verbal instructions and practical support by manipulating or changing the position of instruments and camera when necessary (Figure 1); and (2) “Passive onsite mentoring” where the expert limited his or her support to verbal assistance without using hands to correct the positioning of instruments or camera (a method that is more similar to the one provided by the robot). They concluded that even though “human” mentoring is considered superior over remote “robotic” mentoring, the difference between the two groups was not as large as they had expected. Although it is clear that a remote presence robot may not replace the local mentors, they have been shown that it is a valuable tool in telementoring minimally invasive procedures[14].
Postoperative follow-up: VC is used as an application for the follow-up of patients during the postoperative period and for outpatient consultation. In our institution, in partnership with the Norwegian Center of Integrated Care and Telemedicine, VC is being used for the follow-up of hemodialysis patients[15], dermatology and orthopedics[8,16,17].
A current RCT for stoma patients and postoperative wound problems is in progress at our institution. Stoma patients are a large and resource-demanding group with most of these patients experiencing long and time consuming travel time to and from our hospital in order to attend follow-up consultations (Figure 2). A specialized nurse is able to conduct an examination of a patient stoma whilst not being within the vicinity of the patient, then guide another nurse located within the vicinity of the patient on how to proceed with the stomas change and follow up. The visual component during the clinical examination is important to assess the stoma and postoperative wound. Early results point toward high patient compliance and satisfaction, reduced costs related to traveling are also recorded. Tele-consultation will therefore be well suited for this patient group[17,18]. We believe that an increased usage of tele-consultation and VC technology will improve the post-operative efficiency as well as reduce the costs associated to post-operative treatments for cancer patients, especially those living in rural areas that have to travel great distances to receive treatment.
Telementoring uses similar technological technique of VC. Telementoring permits an expert surgeon, who remains in his/her own hospital, to instruct a non-expert from a peripheral location on how to perform a new laparoscopic technique. The application can be expanded to offer quality control with new or existing procedures[9].
Telementoring has been used worldwide, yet in recent years telementoring has been embraced as a viable method to enhance surgical education and has been carried over to the surgical subspecialties. Feasibility studies started in the second half of the 20th century. In the infancy of teleconferencing, Ranshaw et al[19] Successfully telementored a rural surgeon in more than 24 cases of laparoscopic herniorrhaphy. All of which were completed successfully. In 2003, telementoring between Brazil and the United States was performed successfully for a laparoscopic bilateral varicocelectomy and percutaneous nephrolithotomy. Over the last 15 years, several studies have shown that telementoring is possible and has positive outcomes.
Mentoring a surgical resident can be conveyed at several levels: (1) Oral instructions: while watching a transmitted real-time video of the mentee surgeon operating and guiding him using only voice. This method is considered inferior since it depends on the mentor’s ability to verbally deliver his instructions accurately so the mentee will understand exactly the intended action; and (2) Visual assisted mentoring: Uses a technology called telestration (Figure 3), this technology has been used mostly in weather forecasts and broadcasted sport events since the early sixties. Telestrators allow surgeons to draw a freehand sketch over the live video stream[20], which enables the mentors to convey their teaching both visually as well as verbally.
Current design limitations: Current existing telestration systems such as the one used in the Da VinciTM. Enables a remote surgeon to point on the local surgeon’s display at the master console. However, it does not allow actively drawing lines that would keep their position on the live feed. Telestration however does have the capability as a teaching tool in robotic surgery, yet a proper robotic telemedicine platform does not currently exist[20].
Laparoscopic surgery requires a high degree of special resolution, dexterity, and technical skills. An initial training period is usually required for the majority of surgeons to become expert in these complex techniques by continuous repetition of these tasks. As a result, one would anticipate that to become technically proficient at laparoscopic colorectal resections may require a much longer training period than simpler procedures such as cholecystectomy[21,22]. A number of studies have reported on the length of the learning curve by using different methods and end points over the past 20 years, resulting in suggested numbers between 11 and 110 cases[23,24]. We believe that telementoring can contribute in reducing the learning curve in complex laparoscopic surgeries, however no study has been performed so far to confirm this claim.
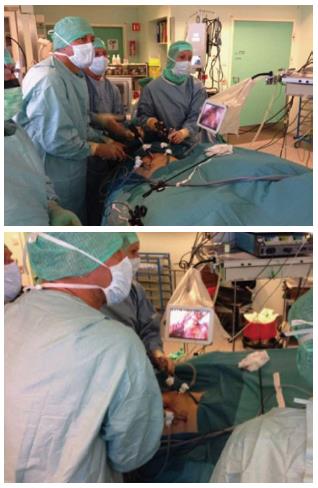
We have conducted several successful pilot experiments at our department with a low cost telementoring prototype based on a common home personal computer and a tablet (Figure 4), with the telementoring performed over regular internet lines. We have developed a unique software and hardware solution that allow us to capture the laparoscopic image directly from the laparoscopic camera and perform several image manipulations in real time. The software we are using provides us with a secure platform that follows and complies with the The Health Insurance Portability and Accountability Act of 1996 Privacy, Security and Breach Notification Rules and regualations(HIPAA). This unique technique is trasferable and repreducable on all laparoscopic disiplenaries e.g., robotic surgery and endoscopy. So far we have conducted successfully in colorectal surgery: abdominoperineal resection and in urological surgery: Adrenectomy, Nephropexy,and Roboitc assisted laparoscopic prostatectomy. Three mentoring methods were used: (1) Active “hands-on” telementoring: the mentor was scrubbed and assisting in the surgery, using the tablet as a tool to enhance his verbal instructions with telestration using the tablet (Figure 4); (2) Passive/on-site mentoring-the mentor was present in the operaitng room but unscrubbed using the tablet to draw illustrations while guiding the mentee surgeons through the operation (Figure 5); and (3) Bed-side mentoring in robotic sugery: the mentor was scrubbed-in and assisting bed-side (Figure 6). All experiments were successful, we are planning in the near future off-site telementoring both short distances and transcontinental.
Networking and Latency: Latency is defined as the amount of time it takes a packet to travel from source to destination; high latency resulted in extreme degradation of performance and has been a major setback in every live videoconferencing session. Telementoring requires a secure high-speed connection with sufficient bandwidth to provide high quality video and audio at both the mentor and mentees station. It has been shown that surgeons are generally able to compensate for delays of up to 700 ms, but delays over 500 ms (half a second) are quite noticeable and potentially detrimental[25]. Mentoring carries inherent limitations and some potential risks. The telementoring process is dependent on primarily the technological adequacy of telecommunication systems; failure of the latter may have clinical implications, which could result in operative errors and the need for conversion.
Cost of generic telementoring systems: The cost of the telementoring system, its software and complete installation (including its secure connection components), ranges from 50000 to 85000 USD. Whereas annual costs for equipment maintenance and broadband services hosting reach approximately 15000 USD[26]. Therefore installation of a telementoring system exclusively for the incorporation of advanced laparoscopic procedures within the setting of a community hospital seems rather unjustified[26]. Evidence exists for cost-effectiveness[27] and safety[28] of telementoring systems, yet there is insufficient data on educational outcomes.
Ethical and legal considerations: The physician-patient relationship nowadays has become challenged by several factors, including technological evolution, novel diagnostic, and treatment modalities. Active involvement of a remote physician in surgery may disturb the therapeutic relationship with the patient and potentially challenge professional collaboration. Prior communication between treating surgeon, the remote mentor, and the patient may need to be included. Matters such as medical liability require a legal framework that would clarify the responsibilities of each part as well as the reliability of the telementoring systems and their integration in routine use. Due to the medical qualifications and licensing in different countries often not being mutually recognized, telementoring projects are currently restricted to national borders[26]. The issue of patient privacy also represents a significant concern and presents a challenge for clinical implementation of telementoring projects. We have been using a HIPPA compliant solution based on a 256-bit encryption (a VPN alternative). This encryption method is considered the best encryption standard existing for civilian medical systems and is relatively inexpensive and not as limited as a standard dedicated VPN-line.
Virtual reality simulators: Standard surgical training has traditionally been one of apprenticeship, where the surgical trainee learns surgery under the supervision of an experienced and qualified surgeon[29]. Simulation is the replication and modeling of real-life situations for training purposes, such as testing scenario planning and design verification. “Simulation” can be any educational program or technology which removes the live patients from the equation to allow a trainee to learn and master skills in a low-stress, high-feedback environment[30]. The large range of procedures to be learned along with the different learning curves associated with the different procedures raises the problem in which a surgeon experienced in one procedure may not be experienced in another. Therefore the availability of expert surgeons for simulation training might be difficult especially in the periphery[5].
Laparoscopic surgery is different from open surgery because of complex the movements and the need for good hand-eye coordination. The fundamentals of laparoscopic surgery (FLS) box trainer is the gold standard for development of laparoscopic technical skills. However, the scoring metrics require a trained mentor and do not allow for immediate and objective feedback[31]. Virtual reality training is one of the many methods used in laparoscopic surgical training and is currently aimed at improving cognitive, psychomotor and technical skills, of both surgical residents during their studies and for maintaining overall skill of experienced surgeons[32].
Another proven advantage of surgical simulators, virtual reality (VR) simulators in specific, is a routine “warm-up” exercise before “performing” in the operating room. Despite adequate mental preparation, unlike other performers, surgeons do not routinely engage in technical “warm-up” exercises before surgery[33]. The concept of “warm-up” exercises is relatively new and is not applied as standard in today’s practice[33]. Short-term practice “warm-up” for 15-20 min with tasks designed to target both psychomotor and cognitive skills that are involved in surgical procedures can greatly enhance skill proficiencies during a the follow-up procedure[34], and is shown to decrease the operative times among experienced surgeons in the operating room[35]. A recent prospective RCT done by Lendvay et al[36] Observed significant performance improvement and error reduction rates among surgeons of varying experience after VR warm-up for basic robotic laparoscopic surgical tasks.
Technology limitations: Learning surgical practices with an unrealistic model may lead to a negative training transfer because of the different learning abilities and limitations of the sensory, motor and cognitive system of the trainees. Another disadvantage is the initial setup cost and costs of consumables and maintenance, especially when it is not possible to simulate each and every learning task[30].
The role of computer games in surgical education and training: Minimally invasive operations provide a set of challenges that are not inherent in open operations, such as decreased tactile feedback, the fulcrum effect, and working in a 3-dimensional space while focusing on 2-dimensions. Training residents to be proficient in these specialized skills goes beyond what hands-on experience in the operating room can achieve[37].
Video games have been shown to improve hand-eye coordination, spatial visualization, manual dexterity, and rapid mental processing, which are important in the development of laparoscopic skills[38]. Middleton et al[38] Conducted a prospective, single-blinded RCT to determine if playing a computer game over a short duration improved VR surgical simulator performance. Their results, when compared with the control, indicated that the group playing video games significantly improved their simulator performances. Most notable findings included significantly higher scores in accuracy, time to completion, number of left-handed movements, left-handed total path length, and left-handed economy of movement for the hand-eye coordination and bimanual clipping and grasping tasks[38].
The practical aspects of telementoring have not been clarified. Telementoring licensure issues are significant medico legal obstacles in the US but to a lesser degree in Europe. Telementors need to have appropriate privileges from the local hospital where the procedure is performed. During a telementored surgical procedure the primary surgeon, at the operational theatre, has primary medical authority and is the sole responsible surgeon ultimately liable for malpractice during the surgery. The premise is that the mentoring surgeon is providing only recommendations and a professional opinion[6].
Remote telementoring is more then just a real-time extension of providing surgical subspecialty advices. It allows young surgeons a safety net and builds confidence while implementing a newly learned technique. Low cost has been one of our primary goals when designing our prototypes for telementoring, in which we managed to have no significant additional expenses. Most operating rooms come replete with laparoscopic equipment, including monitors and a computer with internet capability.
The benefits of telemedicine in the areas of surgical telementoring are potentially large. Remote surgeons/mentors can facilitate procedures that would otherwise not be attempted due to complexity, difficulty, and lack of local surgeon experience. They can also give assistance when unexpected operative findings are discovered and assist in emergencies due to their previous experiences. Developed countries with remote populations such as Australia, United States (Alaska), Canada and Norway are ideal for telesurgical and telementoring technology studies.
P- Reviewer: Fabre JM S- Editor: Wen LL L- Editor: A E- Editor: Zhang DN
| 1. | Guidelines for the surgical practice of telemedicine. Society of American Gastrointestinal Endoscopic Surgeons. Surg Endosc. 2000;14:975-979. |
| 2. | Williams TE, Ellison EC. Population analysis predicts a future critical shortage of general surgeons. Surgery. 2008;144:548-54; discussion 554-6. |
| 3. | Etzioni DA, Finlayson SR, Ricketts TC, Lynge DC, Dimick JB. Getting the science right on the surgeon workforce issue. Arch Surg. 2011;146:381-384. |
| 4. | Etzioni DA, Liu JH, Maggard MA, Ko CY. The aging population and its impact on the surgery workforce. Ann Surg. 2003;238:170-177. |
| 5. | Williams TE, Satiani B, Thomas A, Ellison EC. The impending shortage and the estimated cost of training the future surgical workforce. Ann Surg. 2009;250:590-597. |
| 6. | Treter S, Perrier N, Sosa JA, Roman S. Telementoring: a multi-institutional experience with the introduction of a novel surgical approach for adrenalectomy. Ann Surg Oncol. 2013;20:2754-2758. |
| 7. | Gershon-Cohen J. How rural hospitals can have services of topflight x-ray department. Hosp Manage. 1950;70:116-118. |
| 8. | Augestad KM, Lindsetmo RO. Overcoming distance: video-conferencing as a clinical and educational tool among surgeons. World J Surg. 2009;33:1356-1365. |
| 9. | Augestad KM, Bellika JG, Budrionis A, Chomutare T, Lindsetmo RO, Patel H, Delaney C. Surgical telementoring in knowledge translation--clinical outcomes and educational benefits: a comprehensive review. Surg Innov. 2013;20:273-281. |
| 10. | Bogen EM, Aarsæther E, Augestad KM, Lindsetmo RO, Patel HR. Telemedical technologies in urological cancer care: past, present and future applications. Expert Rev Anticancer Ther. 2013;13:795-809. |
| 11. | ITU: Committed to connecting the world [Internet]. itu.int [cited 2013 Feb 26]. Available from: http://www.itu.int/en/pages/default.aspx. |
| 12. | Doarn CR. Telemedicine in tomorrow’s operating room: a natural fit. Semin Laparosc Surg. 2003;10:121-126. |
| 13. | Bruschi M, Micali S, Porpiglia F, Celia A, De Stefani S, Grande M, Scarpa RM, Bianchi G. Laparoscopic telementored adrenalectomy: the Italian experience. Surg Endosc. 2005;19:836-840. |
| 14. | Sereno S, Mutter D, Dallemagne B, Smith CD, Marescaux J. Telementoring for minimally invasive surgical training by wireless robot. Surg Innov. 2007;14:184-191. |
| 15. | Rumpsfeld M, Arild E, Norum J, Breivik E. Telemedicine in haemodialysis: a university department and two remote satellites linked together as one common workplace. J Telemed Telecare. 2005;11:251-255. |
| 16. | Nordal EJ, Moseng D, Kvammen B, Løchen ML. A comparative study of teleconsultations versus face-to-face consultations. J Telemed Telecare. 2001;7:257-265. |
| 17. | Shannon RJ. Telemedicine in wound healing. Int Wound J. 2005;2:239-240. |
| 18. | Wilbright WA, Birke JA, Patout CA, Varnado M, Horswell R. The use of telemedicine in the management of diabetes-related foot ulceration: a pilot study. Adv Skin Wound Care. 2004;17:232-238. |
| 19. | Ranshaw B, Tucker J, Duncan T. Laparoscopic herniorrhaphy: a review of 900 cases. Surg Endosc. 1996;10:255. |
| 20. | Santomauro M, Reina GA, Stroup SP, L’Esperance JO. Telementoring in robotic surgery. Curr Opin Urol. 2013;23:141-145. |
| 21. | Schlachta CM, Mamazza J, Seshadri PA, Cadeddu M, Gregoire R, Poulin EC. Defining a learning curve for laparoscopic colorectal resections. Dis Colon Rectum. 2001;44:217-222. |
| 22. | Tekkis PP, Senagore AJ, Delaney CP, Fazio VW. Evaluation of the learning curve in laparoscopic colorectal surgery: comparison of right-sided and left-sided resections. Ann Surg. 2005;242:83-91. |
| 23. | Dinçler S, Koller MT, Steurer J, Bachmann LM, Christen D, Buchmann P. Multidimensional analysis of learning curves in laparoscopic sigmoid resection: eight-year results. Dis Colon Rectum. 2003;46:1371-138; discussion 1371-138;. |
| 24. | Miskovic D, Ni M, Wyles SM, Tekkis P, Hanna GB. Learning curve and case selection in laparoscopic colorectal surgery: systematic review and international multicenter analysis of 4852 cases. Dis Colon Rectum. 2012;55:1300-1310. |
| 25. | Micali S, Virgili G, Vannozzi E, Grassi N, Jarrett TW, Bauer JJ, Vespasiani G, Kavoussi LR. Feasibility of telementoring between Baltimore (USA) and Rome (Italy): the first five cases. J Endourol. 2000;14:493-496. |
| 26. | Antoniou SA, Antoniou GA, Franzen J, Bollmann S, Koch OO, Pointner R, Granderath FA. A comprehensive review of telementoring applications in laparoscopic general surgery. Surg Endosc. 2012;26:2111-2116. |
| 27. | Ohinmaa A, Vuolio S, Haukipuro K, Winblad I. A cost-minimization analysis of orthopaedic consultations using videoconferencing in comparison with conventional consulting. J Telemed Telecare. 2002;8:283-289. |
| 28. | Schulam PG, Docimo SG, Saleh W, Breitenbach C, Moore RG, Kavoussi L. Telesurgical mentoring. Initial clinical experience. Surg Endosc. 1997;11:1001-1005. |
| 29. | Nagendran M, Gurusamy KS, Aggarwal R, Loizidou M, Davidson BR. Virtual reality training for surgical trainees in laparoscopic surgery. Cochrane Database Syst Rev. 2013;8:CD006575. |
| 30. | Patel HR, Patel BP. Virtual reality surgical simulation in training. Expert Rev Anticancer Ther. 2012;12:417-420. |
| 31. | Pitzul KB, Grantcharov TP, Okrainec A. Validation of three virtual reality Fundamentals of Laparoscopic Surgery (FLS) modules. Stud Health Technol Inform. 2012;173:349-355. |
| 32. | Patel HRH, Joseph JV. Simulation Training in Laparoscopy and Robotic Surgery. Berlin: Springer 2012; . |
| 33. | Lee JY, Mucksavage P, Kerbl DC, Osann KE, Winfield HN, Kahol K, McDougall EM. Laparoscopic warm-up exercises improve performance of senior-level trainees during laparoscopic renal surgery. J Endourol. 2012;26:545-550. |
| 34. | Kahol K, Satava RM, Ferrara J, Smith ML. Effect of short-term pretrial practice on surgical proficiency in simulated environments: a randomized trial of the “preoperative warm-up” effect. J Am Coll Surg. 2009;208:255-268. |
| 35. | Mucksavage P, Lee J, Kerbl DC, Clayman RV, McDougall EM. Preoperative warming up exercises improve laparoscopic operative times in an experienced laparoscopic surgeon. J Endourol. 2012;26:765-768. |
| 36. | Lendvay TS, Brand TC, White L, Kowalewski T, Jonnadula S, Mercer LD, Khorsand D, Andros J, Hannaford B, Satava RM. Virtual reality robotic surgery warm-up improves task performance in a dry laboratory environment: a prospective randomized controlled study. J Am Coll Surg. 2013;216:1181-1192. |
| 37. | Adams BJ, Margaron F, Kaplan BJ. Comparing video games and laparoscopic simulators in the development of laparoscopic skills in surgical residents. J Surg Educ. 2012;69:714-717. |
| 38. | Middleton KK, Hamilton T, Tsai PC, Middleton DB, Falcone JL, Hamad G. Improved nondominant hand performance on a laparoscopic virtual reality simulator after playing the Nintendo Wii. Surg Endosc. 2013;27:4224-4231. |