Published online Oct 16, 2014. doi: 10.4253/wjge.v6.i10.506
Revised: August 8, 2014
Accepted: September 4, 2014
Published online: October 16, 2014
Processing time: 117 Days and 5.7 Hours
Although insulinomas are rare, they are the most common pancreatic neuroendocrine tumor, with an incidence of four cases per million population. Insulinomas are generally benign indolent intrapancreatic tumors. Surgical resection remains the main option for treatment. However, up to 67% of a pancreatic head insulinomas are nonpalpable, thus surgical resection of the nonplapable insulinoma in this area could become problematic resulting in prolonged surgical time, increased risk of pancreatic duct injury and need for pancreaticoduodenectomy. Endoscopic ultrasound-guided fine- needle tattooing (EUS-FNT), has been shown to have a crucial role for localization of pancreatic body and tail lesions, facilitating laparoscopic distal pancreatectomy and helping surgeons identify the location of the tumor. EUS-FNT might have a role for preoperative localization of pancreatic head insulinomas which are likely to be nonpalpable. We report a case of preoperative EUS-FNT for localization of a nonplapable pancreatic head insulinoma. This report demonstrates that EUS-FNT of pancreatic head insulinomas may facilitate surgical resection, reduce operative time and decrease surgical complications.
Core tip: Preoperative endoscopic ultrasound-guided fine- needle tattooing (EUS-FNT) pancreatic body and tail lesion has shown to decrease operative time and facilitate laparoscopic distal pancreatectomy. We reported that preoperative EUS-FNT can effectively help localizing non-palpable pancreatic head insulinoma, especially in deep pancreatic parenchymal tissue. EUS-FNT helps precisely localizing the tumor and avoiding pancreatic duct and vascular injury from surgery. Furthermore this technique may help in preserving normal pancreatic tissue, reducing operative time and most importantly minimizing risks of pancreaticoduodenectomy. EUS-FNT represents a safe and useful role for the preoperative localization and surgical planning of the pancreatic head insulinoma.
- Citation: Leelasinjaroen P, Manatsathit W, Berri R, Barawi M, Gress FG. Role of preoperative endoscopic ultrasound-guided fine-needle tattooing of a pancreatic head insulinoma. World J Gastrointest Endosc 2014; 6(10): 506-509
- URL: https://www.wjgnet.com/1948-5190/full/v6/i10/506.htm
- DOI: https://dx.doi.org/10.4253/wjge.v6.i10.506
Endoscopic ultrasound (EUS) is a widespread imaging technique providing highly accurate localization of several pancreatic lesions. Endoscopic ultrasound-guided fine-needle tattooing (EUS-FNT) has been shown to have a role for localization of pancreatic body and tail lesions, facilitating laparoscopic distal pancreatectomy and helping surgeons identify the location of the tumor[1,2]. Although EUS-FNT has been widely used for localizing pancreatic lesions in the body and tail, the role of EUS-FNT for pancreatic head lesions has never been established or reported. We report a case of preoperative EUS-FNT for localization of a nonpalpable pancreatic head insulinoma.
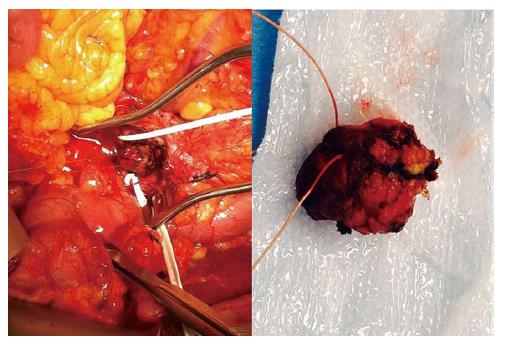
A 70-year-old female, with history of hypertension and Parkinson’s disease, presented to the hospital with neuroglycopenic symptoms, including confusion and weakness. A serum glucose level ranged between 22-65 mg/dL (normal: 73-107 mg/dL). She had persistent episodes of hypoglycemia which required aggressive intravenous dextrose replacement and ICU monitoring. Laboratory evaluation showed a C-peptide of 7.7 ng/mL (1.1-4.4 ng/mL), Insulin level of 20.9 MCiU/mL (0-20 MCiU/mL), Proinsulin of 19.9 pmol/L (3-20 pmol/L) and urine sulfonylurea screening was negative. Computer tomographic of the abdomen and pelvis with pancreas protocol revealed a 1.7 cm × 1.2 cm × 1.6 cm hypervascular lesion in the head of the pancreas located just medial to the gastroduodenal artery (GDA) and lateral to the superior mesenteric vein (SMV) (Figure 1). Endoscopic ultrasound (EUS) revealed a 15.5 mm hypoechoic, homogeneous tumor lesion in the head of pancreas. The tumor was adjacent to GDA and close to the pancreatic duct. EUS-guided fine-needle aspiration (EUS-FNA) biopsy was performed to confirm the diagnosis. Considering the location of the tumor in relation to the SMV and GDA, EUS-FNT was performed using a 22-gauge needle (Echo-Tip, Wilson-Cook). Two mL of sterile carbon-based ink (Spot; GI supply, Camp hill, PA) was injected slowly beginning in the center of the lesion and continuing until the needle exited the pancreas (Figure 2). Two days later, the patient underwent exploratory laparotomy. Intraoperatively, the insulinoma was nonpalpable and located deep in the pancreatic parenchyma between GDA and SMV. This was confirmed by intraoperative ultrasound. During dissection with bi-polar cautery between the GDA and the SMV, the preoperative tattooing was easily identified. The insulinoma was meticulously dissected with the guidance of the tattoo marker to preserve the pancreatic duct located posteriorly. During the procedure, the patient was given 10% dextrose water intravenously and blood sugar was checked every 15 min in order to prevent hypoglycemia. Finally, enucleation of the 2 cm pancreatic head insulinoma was performed without complication (Figure 3). Preoperative random insulin levels decreased significantly to10.6 MCiU/mL compared with preoperative insulin level of 23.8 MCiU/mL. Pathologic evaluation of the resected tumor revealed a pancreatic neuroendocrine tumor, consistent with an insulinoma. The patient had an uneventful postoperative hospitalization and remained euglycemic during outpatient follow-up at 6 mo.
After an insulinoma is diagnosed based on clinical and laboratory findings, surgical resection still remains the treatment of choice in the patient without metastasis. The type of surgical resection, which includes open or laparoscopic enucleation, pancreaticoduodenectomy and distal pancreatectomy are dictated by the location of the insulinoma. Therefore, methods for localizing insulinomas are very important. The preoperative localization of insulinoma which include CT, MRI and EUS, has a very high sensitivity 98%-100% especially after the widespread use of EUS[3,4]. In contrast, the rate of intraoperative detection, including intraoperative palpation and intraoperative ultrasound (IOUS) varies between studies, ranging from 83%-98%[3,5-8]. Hence, preoperative localization of the insulinoma is preferable and crucial for surgical planning and minimizing unnecessary surgery[3]. EUS, provides not only diagnosis by FNA biopsy but also localization of the tumor and has a sensitivity to detect neuroendocrine tumors ranging from 86% to 94%[4,9]. In general, EUS is recommended in patients with a high clinical index of suspicion where CT or MRI failed to localize tumor[3]. EUS-FNT accurately localizes small pancreatic tumors, facilitates identification of pancreatic lesions intraoperatively, and decreases operative time[10,11]. This was confirmed by studies that showed preoperative EUS-FNT of pancreatic body and tail lesions decreased operative time for laparoscopic distal pancreatectomy[1,2]. Although EUS-FNT has been widely used for localizing pancreatic lesions in the body and tail, the role of EUS-FNT for pancreatic head lesions has never been established or reported.
Even though surgery can a have minimal invasive approach, surgical resection of the insulinoma in the pancreatic head still may require an exploratory laparotomy and a pancreaticoduodenectomy (Whipple procedure) due to the structural complexity of this area. Thirty percent of insulinomas are located in the head and uncinate process of the pancreas[3,12]. There are reports that up to 67% of pancreatic head insulinomas are nonpalpable and 80% of nonpalpable insulinomas were located in pancreatic head[3,7]. This can result in a dilemma when intraoperative tumor localization fails and causes the need for unnecessary or extended blind resections. In 4 out of 61 patients from a case series, with and without preoperative EUS localization, a second operation was required to remove a tumor that was unidentifiable intraoperatively during the first operation[3]. Another study also showed that in 1 out of 26 patients, who underwent laparoscopic distal pancreatectomy (LDP) without EUS-FNT, required a second operation to remove the unidentifiable insulinoma by IOUS[2]. EUS-FNT appears to have a role for preoperative localization of pancreatic head insulinoma particularly in cases when a mass could not be palpable and identifiable even with IOUS during surgery.
EUS-FNA complications, include pancreatitis and infection, occur in approximate 0%-2.2%[13,14]. EUS-FNT is technically feasible and safe for pancreatic body and tail lesions. There is only a case of mild pancreatitis reported after EUS-FNT in a case series[1,2]. Since this is the first case report of EUS-FNT performed in the pancreatic head, our case demonstrates the safety of EUS-FNT in pancreatic head area. There was no evidence of pancreatitis or infection after the EUS-FNT procedure and during the intraoperative period.
Our report is the first to describe the use of EUS-FNT for the preoperative localization of a nonpalpable pancreatic head insulinoma. This case differs from previously described reports in the literature in several ways. First, the insulinoma, that we localized, was intraoperatively nonpalpable and located in the head of pancreas. Second, the patient had a moderate to large size tumor (1.55 cm) which was located very close to a major vessel and the pancreatic duct. EUS-FNT can play a role in precisely localizing the tumor margin, in the pancreatic head area, which can help facilitate surgery in nonpalpable insulinoma intraoperatively and helps avoid pancreatic duct and local vascular injury while preserving normal pancreatic tissue. Furthermore, it can help reduce operative time and most importantly decreases the chance for the need to perform pancreaticoduodenectomy.
In conclusion, EUS-FNT represents a useful and safe technique for the preoperative localization and surgical planning of the pancreatic head insulinomas. Further studies will need to be performed to confirm the efficacy and safety of EUS-FNT in the pancreatic head and confirm whether EUS-FNT of these pancreatic head lesions will be able to decrease the rate of pancreaticoduodenectomy and facilitate successful minimal invasive resection.
A 70-year-old female presented with neuroglycopenic symptoms and was found to have a pancreatic head insulinoma.
The patient who has insulinoma could present with either neuroglycopenic symptoms or adrenergic manifestations included shakiness, anxiety, nervousness, palpitations and sweating. Physical examination is usually unremarkable.
Sulfonylurea-induced hypoglycemia, Insulin autoimmune hypoglycemia, Noninsulinoma pancreatogenous hypoglycemia syndrome (NIPHS), other pancreatic neoplasms.
Laboratory evaluation showed a C-peptide of 7.7 ng/mL (1.1-4.4 ng/mL), Insulin level of 20.9 MCiU/mL (0-20 MCiU/mL), Proinsulin of 19.9 pmol/L (3-20 pmol/L) and urine sulfonylurea screening was negative suggesting diagnosis of the insulinoma.
Computed tomography and Endoscopic ultrasound revealed a hypervascular lesion in the pancreatic head located just medial to the gastroduodenal artery and lateral to the superior mesenteric vein.
Pathologic evaluation of the resected tumor revealed a pancreatic neuroendocrine tumor. Immunohistochemistry staining is positive for synaptophysin, chromogranin and insulin, consistent with an insulinoma.
The patient underwent exploratory laparotomy and enucleation of the 2 cm pancreatic head insulinoma without complication.
Endoscopic ultrasound-guided fine-needle tattooing (EUS-FNT) has been shown to have a role for localization of pancreatic body and tail lesions, facilitating laparoscopic distal pancreatectomy and helping surgeons identify the location of the tumor.
Sterile carbon-based ink (GI Spot), is endoscopic non india-ink marker, contains high purity suspended carbon particles providing safe, proven, permanent endoscopic tattooing.
This report demonstrates that EUS-FNT of pancreatic head insulinomas facilitate surgical resection, may reduce operative time and decrease surgical complications.
It is an interesting case.
P- Reviewer: Akyuz F, Appetecchia M, Bloomston M, Tonelli F S- Editor: Ji FF L- Editor: A E- Editor: Zhang DN
| 1. | Lennon AM, Newman N, Makary MA, Edil BH, Shin EJ, Khashab MA, Hruban RH, Wolfgang CL, Schulick RD, Giday S. EUS-guided tattooing before laparoscopic distal pancreatic resection (with video). Gastrointest Endosc. 2010;72:1089-1094. |
| 2. | Newman NA, Lennon AM, Edil BH, Gilson MM, Giday SA, Canto MI, Schulick RD, Makary MA. Preoperative endoscopic tattooing of pancreatic body and tail lesions decreases operative time for laparoscopic distal pancreatectomy. Surgery. 2010;148:371-377. |
| 3. | Nikfarjam M, Warshaw AL, Axelrod L, Deshpande V, Thayer SP, Ferrone CR, Fernández-del Castillo C. Improved contemporary surgical management of insulinomas: a 25-year experience at the Massachusetts General Hospital. Ann Surg. 2008;247:165-172. |
| 4. | McLean AM, Fairclough PD. Endoscopic ultrasound in the localisation of pancreatic islet cell tumours. Best Pract Res Clin Endocrinol Metab. 2005;19:177-193. |
| 5. | Boukhman MP, Karam JH, Shaver J, Siperstein AE, Duh QY, Clark OH. Insulinoma--experience from 1950 to 1995. West J Med. 1998;169:98-104. |
| 6. | Proye C, Boissel P. Preoperative imaging versus intraoperative localization of tumors in adult surgical patients with hyperinsulinemia: a multicenter study of 338 patients. World J Surg. 1988;12:685-690. |
| 7. | Norton JA. Intraoperative methods to stage and localize pancreatic and duodenal tumors. Ann Oncol. 1999;10 Suppl 4:182-184. |
| 8. | Norton JA, Shawker TH, Doppman JL, Miller DL, Fraker DL, Cromack DT, Gorden P, Jensen RT. Localization and surgical treatment of occult insulinomas. Ann Surg. 1990;212:615-620. |
| 9. | Anderson MA, Carpenter S, Thompson NW, Nostrant TT, Elta GH, Scheiman JM. Endoscopic ultrasound is highly accurate and directs management in patients with neuroendocrine tumors of the pancreas. Am J Gastroenterol. 2000;95:2271-2277. |
| 10. | Gress FG, Barawi M, Kim D, Grendell JH. Preoperative localization of a neuroendocrine tumor of the pancreas with EUS-guided fine needle tattooing. Gastrointest Endosc. 2002;55:594-597. |
| 11. | Farrell JJ, Sherrod A, Parekh D. EUS-guided fine-needle tattooing for preoperative localization of early pancreatic adenocarcinoma. Gastrointest Endosc. 2009;69:176-177. |
| 12. | Galbut DL, Markowitz AM. Insulinoma: diagnosis, surgical management and long-term follow-up. Review of 41 cases. Am J Surg. 1980;139:682-690. |
| 13. | Al-Haddad M, Wallace MB, Woodward TA, Gross SA, Hodgens CM, Toton RD, Raimondo M. The safety of fine-needle aspiration guided by endoscopic ultrasound: a prospective study. Endoscopy. 2008;40:204-208. |
| 14. | Fisher L, Segarajasingam DS, Stewart C, Deboer WB, Yusoff IF. Endoscopic ultrasound guided fine needle aspiration of solid pancreatic lesions: Performance and outcomes. J Gastroenterol Hepatol. 2009;24:90-96. |