Published online Dec 16, 2013. doi: 10.4253/wjge.v5.i12.590
Revised: November 14, 2013
Accepted: December 9, 2013
Published online: December 16, 2013
Processing time: 80 Days and 20 Hours
AIM: To report the prevalence of Subsquamous intestinal metaplasia (SSIM) in patients undergoing endoscopic mucosal resection (EMR) for staging of Barrett’s esophagus (BE).
METHODS: Thirty-three patients with BE associated neoplasia underwent EMR at our institution between September 2009 and September 2011; 22 of these patients met study inclusion criteria. EMR was targeted at focal abnormalities within the BE segment. EMR was performed in standardized fashion using a cap-assisted band ligation technique, and resection specimens were assessed for the presence of SSIM. Demographic and clinical data were analyzed to determine predictors of SSIM.
RESULTS: SSIM was detected in 59% of patients. SSIM was detected in 73% of patients with short segment (< 3 cm) BE, and in 45% of patients with long-segment (≥ 3 cm) BE (P = NS). There was no association between presence/absence of SSIM and age, gender, or stage of BE-associated neoplasia.
CONCLUSION: EMR detects SSIM in a majority of patients with BE-associated neoplasia. While the long-term clinical significance of SSIM remains uncertain, these results highlight the importance of EMR as an optimal diagnostic tool for staging of BE and detection of SSIM, and should further limit concerns that SSIM is purely a post-ablation phenomenon.
Core tip: Subsquamous intestinal metaplasia (SSIM) is the term used to describe glandular Barrett’s tissue which is buried beneath overlying squamous mucosa and not visible endoscopically. Esophageal forceps which fail to contain lamina propria are of insufficient depth to assess for the presence of SSIM. This study of patients with Barrett’s esophagus (BE) undergoing endoscopic mucosal resection, previously naïve to endoscopic therapy, detected SSIM in 59% of patients. These findings demonstrate that SSIM is a common occurrence in the natural history of BE, and should limit concerns that SSIM is purely a post-ablation phenonomenon.
- Citation: Yachimski P, Shi C, Slaughter JC, Washington MK. Endoscopic mucosal resection of Barrett’s esophagus detects high prevalence of subsquamous intestinal metaplasia. World J Gastrointest Endosc 2013; 5(12): 590-594
- URL: https://www.wjgnet.com/1948-5190/full/v5/i12/590.htm
- DOI: https://dx.doi.org/10.4253/wjge.v5.i12.590
Barrett’s esophagus (BE) is defined as intestinal metaplasia of the esophageal mucosa, and is recognized as the major known risk factor for esophageal adenocarcinoma[1]. Criteria for the diagnosis of BE have typically included the presence of endoscopically visible mucosal changes proximal to the gastroesophageal junction, with histopathology demonstrating columnar epithelium with goblet cells. The concept of subsquamous intestinal metaplasia (SSIM), often referred to as “buried Barrett’s”, challenges these criteria by implying that metaplastic, glandular BE tissue beneath intact surface squamous mucosa may not be endoscopically apparent, and may be detectable only by histopathologic analysis of mucosal tissue specimens containing lamina propria. A theoretical concern is that SSIM may harbor neoplastic tissue which eludes standard endoscopic surveillance.
SSIM has been reported in BE patients who have received long-term pharmacologic acid suppression therapy[2], and both before and after endoscopic therapy in cohorts across a range of endoscopic ablation modalities including photodynamic therapy (PDT)[3] and radiofrequency ablation (RFA)[4,5]. Estimates of the prevalence of SSIM have varied widely across studies, with a recent systematic review indicating a prevalence ranging between 0 and 28%[6]. This variability may in part reflect inconsistencies in biopsy technique and depth across studies.
The majority of prior studies reporting the prevalence of SSIM have been based on mucosal specimens obtained by forceps biopsy, with the high-end estimate (28%) originating from a study of endoscopic mucosal resection (EMR). EMR, frequently employed for staging of BE-associated neoplasia, offers both a greater depth and surface area of tissue acquisition when compared with forceps biopsies, and therefore may have a higher yield for detection of SSIM. Our hypothesis was that prior reports have underestimated the prevalence of SSIM, and the aim of this study was to determine the prevalence of SSIM in patients undergoing EMR for staging of BE.
Approval to conduct this retrospective study was granted by the Vanderbilt University Institutional Review Board. A database query was performed to identify patients with BE who had undergone EMR between September 2009 and September 2011. Clinical and endoscopic data were extracted from the electronic medical record.
Endoscopic evaluations were performed by a single endoscopist (PY). Candidates for EMR included patients referred for staging of BE-associated neoplasia, with prior biopsies documenting the presence of low-grade dysplasia (LGD), high-grade dysplasia (HGD), and/or adenocarcinoma within the BE segment. EMR is performed as previously described[7]. EMR are performed with a cap-assisted device (Duette Multi-Band Mucosectomy, Cook Medical, Limerick, Ireland). Resections are completed using a snare at a blended current setting (ERBE VIO 200-S electrosurgical unit, set to snare hot biopsy mode with coag effect 1 and maximum Watts 20). If necessary, piecemeal EMR is repeated until the target area has been resected.
The pathology laboratory is notified of specimen submission, and specimens are sectioned in order to preserve tissue orientation and architecture. Formalin-fixed and paraffin-embedded specimens are reviewed by two expert gastrointestinal pathologists (CS and MKW) as previously described[7]. In cases of dysplasia, dysplasia is graded as LGD or HGD. For adenocarcinoma, a local stage is assigned (pT1a, pT1b, etc.) according to American Joint Committee on Cancer 7th edition staging manual.
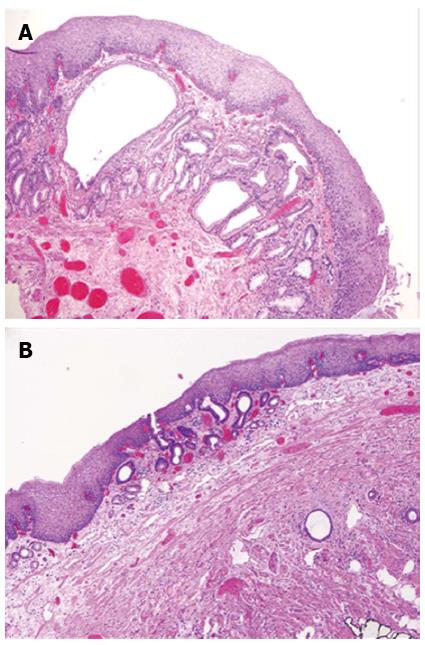
For the purposes of this study, the presence of SSIM was assessed in each EMR specimen. SSIM was defined as glandular intestinal metaplasia within the lamina propria and without apparent continuity with surface BE. Two morphologic subtypes were identified: (1) SSIM with no direct extension to the mucosa (Figure 1A); and (2) SSIM with glands penetrating through the overlying squamous epithelium and onto the luminal surface, surrounded completely by squamous epithelium (Figure 1B).
Exclusion criteria were: (1) prior endoscopic or surgical therapy for BE; (2) the presence of invasive carcinoma detected by histopathologic analysis of the EMR specimen; and (3) the absence of squamous mucosa in the EMR specimen. With respect to the last exclusion criteria, by definition squamous mucosa must be present in the resected in specimen in order to assess for SSIM. Therefore, only EMR specimens obtained in proximity to the endoscopically visible squamocolumnar junction and including squamous tissue were eligible for analysis. EMR specimens obtained entirely from within a BE segment and not containing squamous mucosa were therefore not included.
Descriptive and univariate statistical analysis was performed using the R statistics program. A two-sided P < 0.05 was considered significant.
Thirty-three patients underwent EMR during the study time period. One patient who had undergone radiofrequency ablation prior to EMR and one patient who had undergone prior surgical esophagectomy were excluded. Five patients were excluded due to the absence of squamous tissue in the EMR specimen. An additional four patients were found to have invasive cancer (T1b or greater) and were excluded on this basis. Therefore, the final cohort consisted of 22 subjects. These 22 patients underwent a total of 26 EMR sessions (mean sessions 1.2 per patient, range 1-2). Eighty-two percent of subjects were male, and the mean age of subjects was 64 (range 41-80) years. Mean maximum BE length among the subjects was 3.8 (range 0-12) cm. Pre-EMR histopathologic diagnosis, based on forceps biopsies, was LGD in 5% (1/22), HGD in 41% (9/22), intramucosal (T1a) adenocarcinoma in 36% (8/22), and invasive adenocarcinoma in 18% (4/22) of subjects, respectively.
SSIM was detected in EMR specimens in 59% (13/22) of patients. SSIM was detected in 73% (8/11) of patients with short segment (< 3 cm length) BE and 45% (5/11) of patients with long segment (≥ 3 cm length) BE (P = NS). There was no association between presence/absence of SSIM and age or gender. There was no association between presence/absence of SSIM and stage of neoplasia.
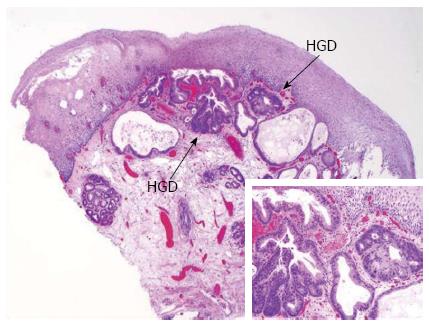
Of the 13 cases with SSIM, 3 (23%) contained high-grade dysplasia in SSIM (Figure 2). Four patients underwent two EMR sessions separated in each case by 2-3 mo intervals, and SSIM was present in the index EMR specimen in each of these patients. Adverse events of EMR were limited to esophageal stricture requiring endoscopic dilation in 5% (1/22) of patients; bleeding requiring endoscopic therapy, hospital admission and packed red blood cell transfusion in one patient; delayed bleeding requiring endoscopic evaluation but no endoscopic therapy and no transfusion in one patient; and aspiration requiring hospital admission in one patient.
This study demonstrates that SSIM is present in the majority of patients undergoing EMR for staging of BE-associated neoplasia. The prevalence of SSIM in this cohort (59%) is considerably higher than previously reported from tissue-based analysis. Prior studies have reported prevalence of SSIM ranging between 0 and 28%[6]. The majority of these studies were based on results of forceps biopsies, which may underestimate prevalence of SSIM due to inadequate sampling of the lamina propria. A 28% prevalence rate of SSIM, often detected at or just proximal to the squamocolumnar junction, was reported in a prior study with EMR as the tissue sampling method[8]. Our findings approach the high SSIM prevalence rate (73%) detected by optical coherence tomography imaging in a recently reported study[9].
Our protocol consisted of focal EMR targeted at specific lesions within the BE segment. Single-session resection is confined to less than 50% of the mural circumference, in order to limit the risk of post-EMR stricture. These focal EMRs do not resect the entirety of the squamocolumnar junction, as might be achieved with a widefield EMR or endoscopic submucosal dissection technique-therefore, it is likely that our study underestimates the true prevalence of SSIM in the cohort.
This study features a systematic, regimented approach to the staging of BE-associated neoplasia, which includes close collaboration between an endoscopist trained in BE endotherapy and expert gastrointestinal pathologists, and which we believe facilitates detection of SSIM. EMR specimens were obtained and evaluated according to set protocol, which included use of specific electrocautery settings. Electrocautery settings for esophageal EMR are not standardized across practices, and may vary by endoscopist and institution, including use of “cut” versus “coag” application for resection and variations in this regard may influence the degree of thermal injury and artifact at lateral resection margins including squamous mucosa, potentially influencing the ability to detect SSIM in proximity to these margins.
This study is limited by its small size and retrospective nature, which limits the ability to assess predictors of SSIM. Details of prior duration of exposure to pharmacologic gastric acid suppression and extent of prior endoscopic biopsy surveillance of BE, both factors which can promote ingrowth of squamous islands within BE, are not available. The study also does not include control groups, for instance to assess the prevalence of SSIM in patients with BE staged by forceps biopsy alone or the prevalence of SSIM in BE patients without neoplasia. The results of this study may not be generalizable to patients with BE without dysplasia or carcinoma.
The long-term clinical significance of SSIM remains a topic of uncertainty, particularly with respect to patients who have undergone endotherapy for BE. Cases of dysplasia and adenocarcinoma arising from SSIM have been reported following treatment of BE-associated neoplasia with PDT[10,11] and argon plasma coagulation[12]. A recent systematic review tallied a total of 34 reported cases of neoplasia (ranging from LGD to invasive adenocarcinoma) arising within SSIM following BE endotherapy[6]. In some cases when neoplasia is present and involving both surface and subsquamous structures, however, it may be difficult to precisely and definitively implicate a subsquamous origin of neoplasia. In follow-up of patients treated in a randomized study of PDT, among patients with biopsies demonstrating recurrence of neoplasia, the highest grade of dysplasia/cancer was always present in surface epithelium and not contained solely in SSIM[3].
On the other hand, SSIM is phenotypically distinct from surface BE on a molecular level. For instance, SSIM following PDT has low Ki-67 crypt proliferation rates and lower rates of aneuploidy when compared with pre-treatment BE[13]. Additional alterations in biomarker expression in SSIM may be a consequence of relative protection from exposure to mutagenic gastric and bile acid reflux[14]. In this regard, SSIM may in theory have a lower malignant potential than surface BE.
While the current study is not informative regarding the long-term malignant potential of SSIM, it does fundamentally alter estimates of the native prevalence of SSIM in an endotherapy-naïve cohort. This creates a critical context for the emerging role of widespread endotherapy for BE, as we aim to understand how endotherapy alters the prevalence and natural history of SSIM. Estimates of SSIM prevalence following BE endotherapy have varied widely, both within and across ablation modalities. Among a randomized study of patients treated with PDT, the prevalence of SSIM was reported to increase from 5.8% pre-treatment to 30% at 5-years post-treatment[3]. In the AIM-Dysplasia trial, a randomized study of RFA plus proton pump inhibitor versus proton pump inhibitor alone, the prevalence of SSIM in the RFA arm was 25.2% pre-treatment, 5.1% at 12 mo post-treatment, and 3.8% at 24 mo post-treatment[4,5]. A prospective study of RFA for treatment of nondysplastic BE, however, reported no SSIM in any of 1473 biopsy specimens from 50 subjects at 5 years post-treatment[15].
An important variable which may influence the ability to identify SSIM, detectable only in specimens containing lamina propria structures, is biopsy depth following BE endotherapy. A recent study reported that lamina propria is present in fewer than 40% of biopsy specimens obtained from neosquamous esophageal epithelium following BE endotherapy[16]. Given this significant limitation, the optimal comparison would be comparison of SSIM in EMR specimens pre-therapy and EMR specimens of neosquamous epithelium post-therapy. A high-volume European center reported no SSIM in EMR specimens from 14 patients following RFA or combined EMR/RFA therapy for BE[17].
Yet EMR is not likely to be acceptable for routine post-treatment surveillance of BE. As the current study demonstrates, although EMR is well-tolerated by the majority of patients, there is a limited but real risk of adverse events including bleeding and esophageal stricture formation. The potential need for improved means of detection and surveillance of SSIM may present an opportunity for endoscopic imaging modalities currently in development and capable of detailed intraluminal imaging of subsurface esophageal structures, including optical coherence tomography or optical frequency domain imaging[9,18-20]. Ultimately, a full understanding of the clinical importance of SSIM will be achievable only through future study of SSIM in tissue specimens obtained from BE patients longitudinally at multiple time points during the course of disease[21].
In summary, this study demonstrates that EMR detects SSIM in a majority of patients with BE-associated neoplasia. This finding should further dampen concerns that SSIM is a post-ablation phenomenon, and may fundamentally alter our understanding of the natural history of BE. As EMR becomes an increasingly important and widely utilized tool in the staging and therapy of BE, further attention to the detection and reporting of SSIM is necessary in order to define the clinical significance of this variant of intestinal metaplasia.
Barrett’s esophagus (BE) refers to intestinal metaplasia of the esophageal mucosa, and is the principal risk factor for esophageal adenocarcinoma. BE has a characteristic salmon-colored appearance and is typically readily visible on endoscopic inspection. Subsquamous intestinal metaplasia (SSIM) is the term used to describe BE tissue which is buried beneath overlying squamous mucosa and not visible endoscopically. Esophageal neoplasia arising from SSIM has been reported. As the use of endoscopic ablation therapies for BE has grown, there are concerns that ablation will accelerate development of SSIM and lead to risk of neoplasia which is invisible or elusive to standard endoscopic surveillance.
There are limited data regarding the prevalence and natural history of SSIM, particularly among BE patients who have not previously undergone endoscopic treatment. Esophageal biopsies may underestimate the prevalence of SSIM due to limited depth of biopsy samples. The aim of this study was to assess the prevalence of BE among patients undergoing endoscopic mucosal resection, an endoscopic technique which allows for removal of a tissue sample of much greater surface area and depth compared to a forceps biopsy
This is the highest reported prevalence of SSIM in patients with BE naïve to endoscopic therapy.
The finding of a high prevalence of SSIM among patients with BE may alter the authors’ understanding of the natural history of BE, and provide an opportunity for new technologies capable of imaging subepithelial structures to play a role in endoscopic surveillance of BE.
Endoscopic mucosal resection (EMR), is an esophageal tissue resection technique which has important diagnostic and therapeutic value in the endoscopic management of Barrett’s esophagus neoplasia. Subsquamous intestinal metaplasia (SSIM), informally referred to as “buried Barrett’s”, is the term used to describe glandular esophageal epithelium which is buried beneath overlying squamous mucosa and not visible endoscopically.
The authors present a study describing their reporting of intestinal metaplasia at levels deeper than the mucosa. While a small sample size was used in the study, they discovered a significant prevalence of subsquamous intestinal metaplasia in their patients. They provide a rationale approach to the workup of these patents, and explain the importance of deeper tissue biopsy using EMR without overstating the significance of such findings.
P- Reviewers: Bago J, Marks J S- Editor: Qi Y L- Editor: A E- Editor: Zhang DN
| 1. | Falk GW. Barrett’s esophagus. Gastroenterology. 2002;122:1569-1591. |
| 2. | Sharma P, Morales TG, Bhattacharyya A, Garewal HS, Sampliner RE. Squamous islands in Barrett’s esophagus: what lies underneath? Am J Gastroenterol. 1998;93:332-335. |
| 3. | Bronner MP, Overholt BF, Taylor SL, Haggitt RC, Wang KK, Burdick JS, Lightdale CJ, Kimmey M, Nava HR, Sivak MV. Squamous overgrowth is not a safety concern for photodynamic therapy for Barrett’s esophagus with high-grade dysplasia. Gastroenterology. 2009;136:56-64; quiz 351-2. |
| 4. | Shaheen NJ, Sharma P, Overholt BF, Wolfsen HC, Sampliner RE, Wang KK, Galanko JA, Bronner MP, Goldblum JR, Bennett AE. Radiofrequency ablation in Barrett’s esophagus with dysplasia. N Engl J Med. 2009;360:2277-2288. |
| 5. | Shaheen NJ, Overholt BF, Sampliner RE, Wolfsen HC, Wang KK, Fleischer DE, Sharma VK, Eisen GM, Fennerty MB, Hunter JG. Durability of radiofrequency ablation in Barrett’s esophagus with dysplasia. Gastroenterology. 2011;141:460-468. |
| 6. | Gray NA, Odze RD, Spechler SJ. Buried metaplasia after endoscopic ablation of Barrett’s esophagus: a systematic review. Am J Gastroenterol. 2011;106:1899-908; quiz 1909. |
| 7. | Ayers K, Shi C, Washington K, Yachimski P. Expert pathology review and endoscopic mucosal resection alters the diagnosis of patients referred to undergo therapy for Barrett’s esophagus. Surg Endosc. 2013;27:2836-2840. |
| 8. | Chennat J, Ross AS, Konda VJ, Lin S, Noffsinger A, Hart J, Waxman I. Advanced pathology under squamous epithelium on initial EMR specimens in patients with Barrett’s esophagus and high-grade dysplasia or intramucosal carcinoma: implications for surveillance and endotherapy management. Gastrointest Endosc. 2009;70:417-421. |
| 9. | Zhou C, Tsai TH, Lee HC, Kirtane T, Figueiredo M, Tao YK, Ahsen OO, Adler DC, Schmitt JM, Huang Q. Characterization of buried glands before and after radiofrequency ablation by using 3-dimensional optical coherence tomography (with videos). Gastrointest Endosc. 2012;76:32-40. |
| 10. | Mino-Kenudson M, Ban S, Ohana M, Puricelli W, Deshpande V, Shimizu M, Nishioka NS, Lauwers GY. Buried dysplasia and early adenocarcinoma arising in barrett esophagus after porfimer-photodynamic therapy. Am J Surg Pathol. 2007;31:403-409. |
| 11. | Overholt BF, Panjehpour M, Halberg DL. Photodynamic therapy for Barrett’s esophagus with dysplasia and/or early stage carcinoma: long-term results. Gastrointest Endosc. 2003;58:183-188. |
| 12. | Van Laethem JL, Peny MO, Salmon I, Cremer M, Devière J. Intramucosal adenocarcinoma arising under squamous re-epithelialisation of Barrett’s oesophagus. Gut. 2000;46:574-577. |
| 13. | Hornick JL, Mino-Kenudson M, Lauwers GY, Liu W, Goyal R, Odze RD. Buried Barrett’s epithelium following photodynamic therapy shows reduced crypt proliferation and absence of DNA content abnormalities. Am J Gastroenterol. 2008;103:38-47. |
| 14. | Odze RD, Lauwers GY. Histopathology of Barrett’s esophagus after ablation and endoscopic mucosal resection therapy. Endoscopy. 2008;40:1008-1015. |
| 15. | Fleischer DE, Overholt BF, Sharma VK, Reymunde A, Kimmey MB, Chuttani R, Chang KJ, Muthasamy R, Lightdale CJ, Santiago N. Endoscopic radiofrequency ablation for Barrett’s esophagus: 5-year outcomes from a prospective multicenter trial. Endoscopy. 2010;42:781-789. |
| 16. | Gupta N, Mathur SC, Dumot JA, Singh V, Gaddam S, Wani SB, Bansal A, Rastogi A, Goldblum JR, Sharma P. Adequacy of esophageal squamous mucosa specimens obtained during endoscopy: are standard biopsies sufficient for postablation surveillance in Barrett’s esophagus? Gastrointest Endosc. 2012;75:11-18. |
| 17. | Pouw RE, Gondrie JJ, Rygiel AM, Sondermeijer CM, ten Kate FJ, Odze RD, Vieth M, Krishnadath KK, Bergman JJ. Properties of the neosquamous epithelium after radiofrequency ablation of Barrett’s esophagus containing neoplasia. Am J Gastroenterol. 2009;104:1366-1373. |
| 18. | Mori Y, Itoh Y, Tajima N. Angiotensin II receptor blockers downsize adipocytes in spontaneously type 2 diabetic rats with visceral fat obesity. Am J Hypertens. 2007;20:431-436. |
| 19. | Suter MJ, Vakoc BJ, Yachimski PS, Shishkov M, Lauwers GY, Mino-Kenudson M, Bouma BE, Nishioka NS, Tearney GJ. Comprehensive microscopy of the esophagus in human patients with optical frequency domain imaging. Gastrointest Endosc. 2008;68:745-753. |
| 20. | Adler DC, Zhou C, Tsai TH, Lee HC, Becker L, Schmitt JM, Huang Q, Fujimoto JG, Mashimo H. Three-dimensional optical coherence tomography of Barrett’s esophagus and buried glands beneath neosquamous epithelium following radiofrequency ablation. Endoscopy. 2009;41:773-776. |
| 21. | Yachimski P, Falk GW. Subsquamous intestinal metaplasia: implications for endoscopic management of Barrett’s esophagus. Clin Gastroenterol Hepatol. 2012;10:220-224. |