Published online Nov 16, 2013. doi: 10.4253/wjge.v5.i11.568
Revised: October 9, 2013
Accepted: November 2, 2013
Published online: November 16, 2013
Processing time: 92 Days and 13.6 Hours
AIM: To postoperative endoscopic retrograde cholangiopancreatography (ERCP) failure, we describe a modified Rendezvous technique for an ERCP in patients operated on for common bile duct stone (CBDS) having a T-tube with retained CBDSs.
METHODS: Five cases operated on for CBDSs and having retained stones with a T-tube were referred from other hospitals located in or around Istanbul city to the ERCP unit at the Haydarpasa Numune Education and Research Hospital. Under sedation anesthesia, a sterile guide-wire was inserted via the T-tube into the common bile duct (CBD) then to the papilla. A guide-wire was held by a loop snare and removed through the mouth. The guide-wire was inserted into the sphincterotome via the duodenoscope from the tip to the handle. The duodenoscope was inserted down to the duodenum with a sphincterotome and a guide-wire in the working channel. With the guidance of a guide-wire, the ERCP and sphincterotomy were successfully performed, the guide-wire was removed from the T-tube, the stones were removed and the CBD was reexamined for retained stones by contrast.
RESULTS: An ERCP can be used either preoperatively or postoperatively. Although the success rate in an isolated ERCP treatment ranges from up to 87%-97%, 5%-10% of the patients require two or more ERCP treatments. If a secondary ERCP fails, the clinicians must be ready for a laparoscopic or open exploration. A duodenal diverticulum is one of the most common failures in an ERCP, especially in patients with an intradiverticular papilla. For this small group of patients, an antegrade cannulation via a T-tube can improve the success rate up to nearly 100%.
CONCLUSION: The modified Rendezvous technique is a very easy method and increases the success of postoperative ERCP, especially in patients with large duodenal diverticula and with intradiverticular papilla.
Core tip: A postoperative endoscopic retrograde cholangiopancreatography (ERCP) is used as a treatment modality for common bile duct stone (CBDS) clearance when a laparoscopic common bile duct exploration has failed or retained stones are discovered after an operation. If a secondary ERCP fails, the clinicians must be ready for a laparoscopic or open exploration. Because of this, different techniques are required to exclude surgical intervention. We describe a modified Rendezvous technique for an ERCP in patients operated on for CBDSs having a T-tube with retained CBDSs and with intradiverticular papilla. The modified Rendezvous technique is a very easy method and increases the success of postoperative ERCP, especially in patients with large duodenal diverticula and with intradiverticular papilla.
- Citation: Odabasi M, Yildiz MK, Abuoglu HH, Eris C, Ozkan E, Gunay E, Aktekin A, Muftuoglu MT. A modified Rendezvous ERCP technique in duodenal diverticulum. World J Gastrointest Endosc 2013; 5(11): 568-573
- URL: https://www.wjgnet.com/1948-5190/full/v5/i11/568.htm
- DOI: https://dx.doi.org/10.4253/wjge.v5.i11.568
Common bile duct stones (CBDSs) can precipitate a variety of clinical events such as biliary colic, jaundice, and sepsis. In the treatment of this condition, stone removal is the primary intervention for dealing with clinical symptoms. The treatment options are an endoscopic retrograde cholangiopancreatography (ERCP) with endoscopic sphincterotomy (ES) and a laparoscopic or open surgical intervention[1].
Postoperative ERCP is used as a treatment modality for CBDS clearance when a laparoscopic common bile duct exploration (LCBDE) has failed or retained stones are discovered after an operation (2.5%)[2]. If a secondary ERCP fails, the clinicians must be ready for a laparoscopic or open exploration. A duodenal diverticulum is one of the most common failures of an ERCP, especially in patients with an intradiverticular papilla[3]. Because of this condition, we need different techniques to exclude surgical intervention. Percutaneous techniques are used for this purpose. The Rendezvous technique combines an endoscopy with a percutaneous transhepatic cholangiography to facilitate cannulation of the bile duct when previous attempts have failed[1,4]. We describe a modified Rendezvous technique for an ERCP in patients operated on for CBDSs having a T-tube with retained CBDSs.
Five cases operated on for CBDSs and having retained stones with a T-tube were referred to the ERCP unit at the Haydarpasa Numune Education and Research Hospital from other hospitals located in or around Istanbul city.
The preoperative findings were unclear because we could not obtain reliable information about the patients’ preoperative status. All of the patients had a history of failed ERCP attempts at other ERCP units before surgery; five of these cases had papilla in their duodenal diverticulum. To prevent possible complications associated with a premature extraction of the T-tube, we waited three weeks before it was removed.
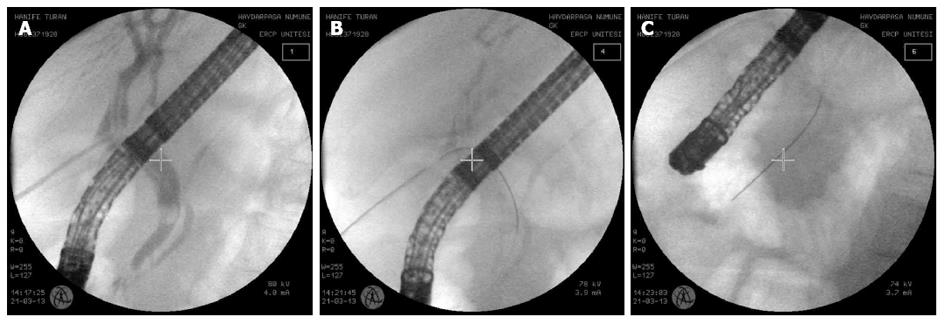
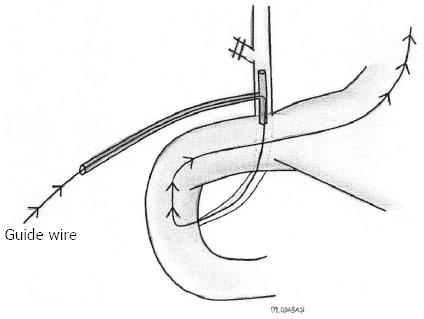
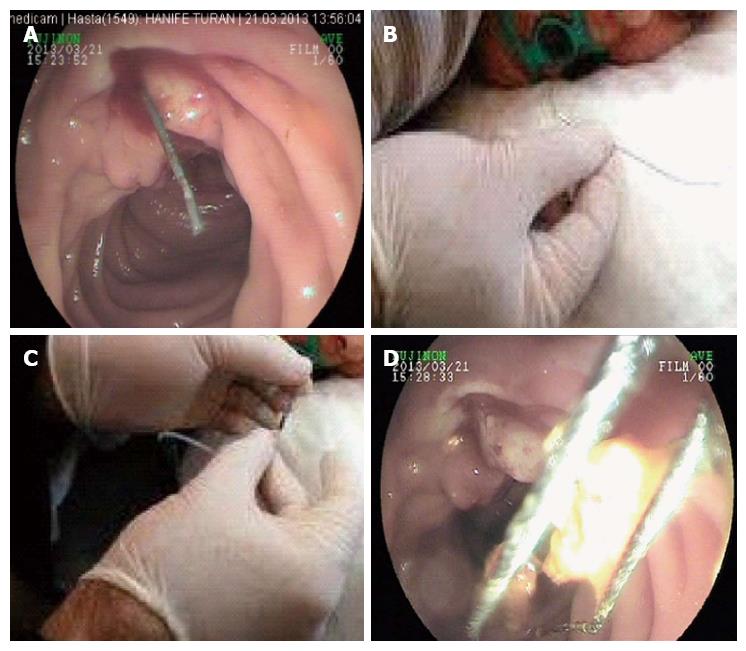
A contrast material was injected via the T-tube, and the stone was observed in the common bile duct (CBD). Under sedation anesthesia with midazolam 3-5 mg and meperidine 30-50 mg by the intravenous route, a sterile guide-wire was inserted via the T-tube to the CBD then to the papilla (Figure 1). All of the patients with a diverticulum had a large diverticulum with an intradiverticular papilla. In our cases, the guide-wire was held by a loop snare and removed through the mouth (Figure 2). The sphincterotome was inserted into the working channel. The guide-wire was inserted into the sphincterotome via the duodenoscope from the tip to the handle (Figure 3). Subsequently, the duodenoscope was inserted down to the duodenum. Using the guidance of the guide-wire, the ERCP and sphincterotomy were successfully performed, the guide-wire was removed through the mouth, the stones were removed and the CBD was reexamined for retained stones by contrast (Figure 4). The T-tube was removed after 1-2 d because of the possibility of edema at the papilla.
In the time period between August 2009 and March 2012, 5 patients who underwent CBD exploration and who had retained stones with a T-tube were referred to the ERCP unit at our institution.
There were 1 man and 4 women ranging in age from 51 to 78 years with a mean age of 65 years. The patients all had a successful stone removal by a modified rendezvous technique.
The length of the hospital stay was 3.4 d. The T-tubes were removed. The patients were followed up for possible complications of the ERCP and T-tube removal. No morbidity or mortality occurred.
All the patients were followed up regularly through the first postoperative year. There has been no incidence of residual disease, and all the patients who were regularly followed-up have been asymptomatic.
An ERCP should be used as a therapy rather than a diagnosis; it should be therapeutic in more than 90% of cases[5]. An ERCP can be used either preoperatively or postoperatively. Although the success rate in isolated ERCP treatments ranges from 87% to 97%, 5%-10% of patients require two or more ERCP treatments[6]. This method is associated with morbidity and mortality rates of 15% and 1%, respectively[7,8]. ERCP is not possible in 3%-10% of all patients[9]. These patients need laparoscopic or open surgical intervention.
An LCBDE is the treatment of choice in many centers with successful stone clearance rates ranging from 85% to 95%, a morbidity rate of 4%-16% and a mortality rate of approximately 0%-2%[10,11]. If this fails, alternate approaches such as an intraoperative or postoperative ERCP/EST, laparoscopic choledochotomy, or open CBDE may be used[12]. A transcystic approach is generally used for small stones in a small bile duct whereas a transductal approach is preferred for large occluding stones in a large duct, for intrahepatic stones, or a tortuous cystic duct[9]. If the transcystic approach fails, a laparoscopic choledocholithotomy is recommended. After the stones are removed under endoscopic visualization, the ductotomy is usually closed either primarily or over an appropriately sized T-tube. The indication for a T-tube insertion is a decompression of the duct in patients with a residual distal obstruction, ductal imaging in the postoperative period to provide an access route for the removal of residual CBDSs[13-16]. When an LCBDS and a postoperative ERCP have failed, the surgeon must use the open approach to surgery. In the era of open cholecystectomy, open bile duct surgery was superior to ERCP in achieving CBD stone clearance. In the laparoscopic era, the data are close to excluding a significant difference between the laparoscopic and ERCP clearance of CBD stones. The use of an ERCP necessitates an increased number of procedures per patient[14].
The routine use of intraoperative cholangiography (IOC) is still controversial. However, it can be a useful tool for identifying choledochal stones[17]. Supporters of the IOC routine claim that this practice ensures fewer retained stones, fewer postoperative ERCPs, and a reduction in the number of CBD injuries[18]. One drawback is the consequent lengthening of the operation time by approximately 15 min[19].
Although an LCBDE or open surgical explorations are performed, 2.5% of the patients still have retained stones[2]. Percutaneous transhepatic therapies can be considered for CBDS under US guidance in selected patients[17]. The extraction of stones, a sphincterotomy, or percutaneous drainage can be performed using this method[20]. A percutaneous extraction is successful in more than 95% of the patients with retained stones; otherwise a postoperative ERCP can be required[21].
A T-tube cholangiography should be performed before the removal of the tube (6-18 d postoperatively). The removal of the T-tube has been suggested as early as 5-6 d postoperatively and as late as 4-5 wk after surgery. Retained stones identified by a T-tube cholangiography may be effectively removed percutaneously after allowing for the maturation of the T-tube tract. Although all these techniques have high success rates, there is still a group of patients who need a second surgical intervention because of CBDSs. A duodenal diverticulum is one of the most common failures of an ERCP, especially in patients with an intradiverticular papilla[3]. The prevalence of a duodenal diverticulum is approximately 5% in postmortem studies, but endoscopic evaluations have documented higher rates (5%-23%)[22]. For this small group of patients, antegrade cannulation via a T-tube can raise the success rate up to nearly 100%[23].
When a selective CBD cannulation cannot be performed by ERCP despite trying various endoscopic techniques, a percutaneous transhepatic biliary drainage (PTBD) followed by a combined rendezvous technique is often successful. This combined technique increases the success rate of the biliary tract cannulation and facilitates the diagnosis and treatment of biliary tract diseases.
Antegrade cannulation via a T-tube is a modified rendezvous technique described by our ERCP unit. This technique can be performed using sedation anesthesia; this is a very easy technique that increases the success rate and decreases the complications of an ERCP. In this technique, because there is no false insertion of a catheter and a guide-wire to the pancreatic duct, the accidental occurrence of symptoms of pancreatitis is low and, unlike in a normal ERCP, the success rate appears to be higher[24].
In other Rendezvous techniques, the guide-wire is grasped with a snare or forceps and pulled back through the working channel of the duodenoscope for subsequent over the wire cannulation[25]. However, it is not always easy to grasp the guide-wire, which may be kinked, and its coating can be damaged during the withdrawal through the working channel of the duodenoscope, thus making it difficult, sometimes impossible, to pass a catheter over it[26].
Although this patient group is small, this technique should be kept in mind. Percutaneous techniques are used worldwide but cannot be applied in all centers, and they require experienced personnel. Even beginners can apply our technique. You can examine the CBD with a contrast material via a T-tube. We recommend our technique, especially in cases of an intradiverticular papilla.
In conclusion, the antegrade cannulation of a guide-wire passing via a T-tube to the papilla is a very easy method and increases the success rate of postoperative ERCP, especially in patients with large duodenal diverticula with an intradiverticular papilla. Because the number of participants is small, this study must be supported by further studies. We recommend this modified technique for the centers that have an ERCP unit because other techniques are not appropriate for all clinical circumstances in all centers.
A postoperative endoscopic retrograde cholangiopancreatography (ERCP) is used as a treatment modality for common bile duct stone clearance when a laparoscopic common bile duct exploration has failed or retained stones are discovered after an operation. If a secondary ERCP fails, the clinicians must be ready for a laparoscopic or open exploration. Because of this condition, the authors need different techniques to exclude surgical intervention. The rendezvous technique combines an endoscopy with a percutaneous transhepatic cholangiography to facilitate the cannulation of the bile duct when previous attempts have failed.
The antegrade cannulation of a guide-wire passing via a T-tube to the papilla is a very easy method and increases the success of postoperative ERCP, especially in patients with large duodenal diverticula with an intradiverticular papilla.
Antegrade cannulation via a T-tube is a modified rendezvous technique described by our ERCP unit. This technique can be performed under sedation anesthesia, and it is a very easy technique that increases the success rate and decreases the complications of an ERCP. In this technique, because there is no false insertion of a catheter and a guide-wire to the pancreatic duct, the accidental occurrence of the symptoms of pancreatitis is low and, unlike a normal ERCP, the success rate appears to be higher.
The study recommends the modified technique for centers that have an ERCP unit because other techniques are not appropriate for all clinical circumstances at all centers.
Rendezvous technique: The rendezvous technique combines an endoscopy with a percutaneous transhepatic cholangiography to facilitate the cannulation of the bile duct when previous attempts have failed.
The concept of this technique seems logical and promising; the study conclusions are based on preliminary experience with a small number of participants. Therefore, caution should be taken in regard to the widespread use of the technique before further studies are pursued.
P- Reviewers: Fornari F, Hussain A S- Editor: Qi Y L- Editor: A E- Editor: Zhang DN
| 1. | Lee JH, Kim HW, Kang DH, Choi CW, Park SB, Kim SH, Jeon UB. Usefulness of percutaneous transhepatic cholangioscopic lithotomy for removal of difficult common bile duct stones. Clin Endosc. 2013;46:65-70. |
| 2. | Anwar S, Rahim R, Agwunobi A, Bancewicz J. The role of ERCP in management of retained bile duct stones after laparoscopic cholecystectomy. N Z Med J. 2004;117:U1102. |
| 3. | Boix J, Lorenzo-Zúñiga V, Añaños F, Domènech E, Morillas RM, Gassull MA. Impact of periampullary duodenal diverticula at endoscopic retrograde cholangiopancreatography: a proposed classification of periampullary duodenal diverticula. Surg Laparosc Endosc Percutan Tech. 2006;16:208-211. |
| 4. | Neuhaus H. Endoscopic and percutaneous treatment of difficult bile duct stones. Endoscopy. 2003;35:S31-S34. |
| 5. | Caddy GR, Tham TC. Gallstone disease: Symptoms, diagnosis and endoscopic management of common bile duct stones. Best Pract Res Clin Gastroenterol. 2006;20:1085-1101. |
| 6. | Deng DH, Zuo HM, Wang JF, Gu ZE, Chen H, Luo Y, Chen M, Huang WN, Wang L, Lu W. New precut sphincterotomy for endoscopic retrograde cholangiopancreatography in difficult biliary duct cannulation. World J Gastroenterol. 2007;13:4385-4390. |
| 7. | Christensen M, Matzen P, Schulze S, Rosenberg J. Complications of ERCP: a prospective study. Gastrointest Endosc. 2004;60:721-731. |
| 8. | Andriulli A, Loperfido S, Napolitano G, Niro G, Valvano MR, Spirito F, Pilotto A, Forlano R. Incidence rates of post-ERCP complications: a systematic survey of prospective studies. Am J Gastroenterol. 2007;102:1781-1788. |
| 9. | Martin IJ, Bailey IS, Rhodes M, O’Rourke N, Nathanson L, Fielding G. Towards T-tube free laparoscopic bile duct exploration: a methodologic evolution during 300 consecutive procedures. Ann Surg. 1998;228:29-34. |
| 10. | Rojas-Ortega S, Arizpe-Bravo D, Marín López ER, Cesin-Sánchez R, Roman GR, Gómez C. Transcystic common bile duct exploration in the management of patients with choledocholithiasis. J Gastrointest Surg. 2003;7:492-496. |
| 11. | Thompson MH, Tranter SE. All-comers policy for laparoscopic exploration of the common bile duct. Br J Surg. 2002;89:1608-1612. |
| 12. | Phillips EH, Toouli J, Pitt HA, Soper NJ. Treatment of common bile duct stones discovered during cholecystectomy. J Gastrointest Surg. 2008;12:624-628. |
| 13. | Petelin JB. Laparoscopic common bile duct exploration. Surg Endosc. 2003;17:1705-1715. |
| 14. | Martin DJ, Vernon DR, Toouli J. Surgical versus endoscopic treatment of bile duct stones. Cochrane Database Syst Rev. 2006;CD003327. |
| 15. | Baker AR, Neoptolemos JP, Leese T, James DC, Fossard DP. Long term follow-up of patients with side to side choledochoduodenostomy and transduodenal sphincteroplasty. Ann R Coll Surg Engl. 1987;69:253-257. |
| 16. | Tabone LE, Sarker S, Fisichella PM, Conlon M, Fernando E, Yi S, Luchette FA. To ‘gram or not’? Indications for intraoperative cholangiogram. Surgery. 2011;150:810-819. |
| 17. | Freitas ML, Bell RL, Duffy AJ. Choledocholithiasis: evolving standards for diagnosis and management. World J Gastroenterol. 2006;12:3162-3167. |
| 18. | Flum DR, Flowers C, Veenstra DL. A cost-effectiveness analysis of intraoperative cholangiography in the prevention of bile duct injury during laparoscopic cholecystectomy. J Am Coll Surg. 2003;196:385-393. |
| 19. | Halpin VJ, Dunnegan D, Soper NJ. Laparoscopic intracorporeal ultrasound versus fluoroscopic intraoperative cholangiography: after the learning curve. Surg Endosc. 2002;16:336-341. |
| 20. | Itoi T, Shinohara Y, Takeda K, Nakamura K, Sofuni A, Itokawa F, Moriyasu F, Tsuchida A. A novel technique for endoscopic sphincterotomy when using a percutaneous transhepatic cholangioscope in patients with an endoscopically inaccessible papilla. Gastrointest Endosc. 2004;59:708-711. |
| 21. | Hungness ES, Soper NJ. Management of common bile duct stones. J Gastrointest Surg. 2006;10:612-619. |
| 22. | Kirk AP, Summerfield JA. Incidence and significance of juxtapapillary diverticula at endoscopic retrograde cholangiopancreatography. Digestion. 1980;20:31-35. |
| 23. | Kawakubo K, Isayama H, Sasahira N, Nakai Y, Kogure H, Hamada T, Miyabayashi K, Mizuno S, Sasaki T, Ito Y. Clinical utility of an endoscopic ultrasound-guided rendezvous technique via various approach routes. Surg Endosc. 2013;27:3437-3443. |
| 24. | La Greca G, Barbagallo F, Di Blasi M, Di Stefano M, Castello G, Gagliardo S, Latteri S, Russello D. Rendezvous technique versus endoscopic retrograde cholangiopancreatography to treat bile duct stones reduces endoscopic time and pancreatic damage. J Laparoendosc Adv Surg Tech A. 2007;17:167-171. |
| 25. | Calvo MM, Bujanda L, Heras I, Cabriada JL, Bernal A, Orive V, Miguelez J. The rendezvous technique for the treatment of choledocholithiasis. Gastrointest Endosc. 2001;54:511-513. |
| 26. | Dickey W. Parallel cannulation technique at ERCP rendezvous. Gastrointest Endosc. 2006;63:686-687. |