Published online Jan 16, 2013. doi: 10.4253/wjge.v5.i1.34
Revised: August 28, 2012
Accepted: September 18, 2012
Published online: January 16, 2013
Processing time: 190 Days and 11.8 Hours
A 69-year-old Japanese female was diagnosed with primary intestinal follicular lymphoma. Esophagogastroduodenoscopy with high-definition imaging revealed not only the typical feature of whitish polyps of up to 2 mm in diameter in the duodenal second and third portions, but also more detailed morphology, such as enlarged whitish villi and tiny whitish depositions. These findings appeared to reflect the pathological structures; infiltration of lymphoma cells into the villi were probably seen as enlargement of the villi, and the formation of lymphoid follicles were shown as opaque white spots or tiny white depositions. Thus, the above features might contribute to the distinct diagnosis of intestinal follicular lymphoma. This case indicates that routine esophagogastroduodenoscopy can visualize microsurface structures, which can be pathognomonic and help to diagnose intestinal follicular lymphoma, even without magnifying endoscopy.
- Citation: Iwamuro M, Kawai Y, Takata K, Kawano S, Yoshino T, Okada H, Yamamoto K. Primary intestinal follicular lymphoma: How to identify follicular lymphoma by routine endoscopy. World J Gastrointest Endosc 2013; 5(1): 34-38
- URL: https://www.wjgnet.com/1948-5190/full/v5/i1/34.htm
- DOI: https://dx.doi.org/10.4253/wjge.v5.i1.34
The number of patients newly diagnosed with primary intestinal follicular lymphoma is increasing as increasing numbers of endoscopists and gastroenterologists become familiar with this entity. The duodenum is the most frequently affected site, and the representative endoscopic feature, small whitish polypoid nodules up to 2 mm in diameter, is well known[1]. This feature has been described as “multiple polypoid lesions,”“multiple small polyps,”“multiple nodules” and “multiple granules”[2,3]. The ongoing development of magnifying endoscopy has provided more detailed endoscopic images of intestinal follicular lymphoma, enabling the identification of features such as enlarged villi, opaque whitish spots, and coiled vascular pattern within the villi[4-9].
We recently treated a patient with a typical case of primary duodenal follicular lymphoma. Her diagnosis was based on routine esophagogastroduodenoscopy findings without magnifying observations. The endoscopy findings were of a characteristic morphology, including enlarged whitish villi, tiny submucosal whitish depositions and multiple sites of involvement, in addition to the typical macroscopic features of whitish polypoid nodules. This case indicates that routine endoscopy can identify not only well known features such as whitish polyps or nodules, but also more detailed images that help to diagnose this disease, even without magnifying endoscopy.
A 69-year-old Japanese female presented to Onomichi Municipal Hospital in April 2012 with intermittent vague abdominal pain that had been present for the previous week. She had been taking betahistine mesilate for the prevention of Meniere’s syndrome. The patient had no previous history of gastrointestinal or hematopoietic diseases. Physical examination revealed no abnormalities, and there was no evidence of hepatosplenomegaly or peripheral lymphadenopathy. All laboratory findings, including the levels of lactate dehydrogenase (LDH) and soluble interleukin-2 receptor (sIL-2R), were within the normal ranges.
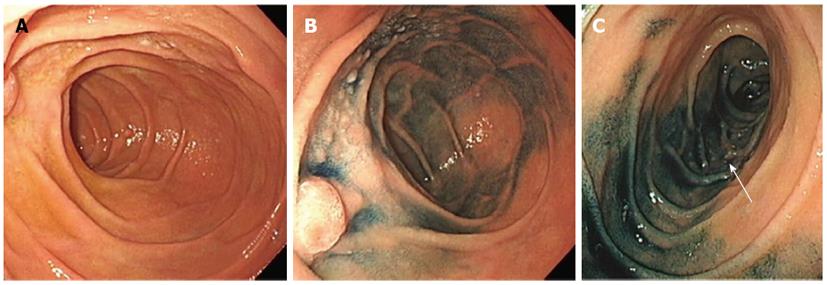
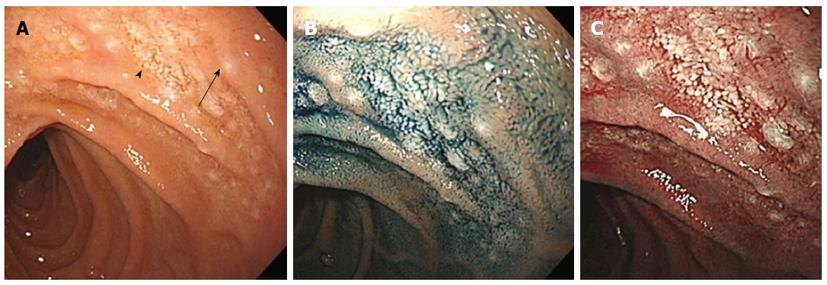
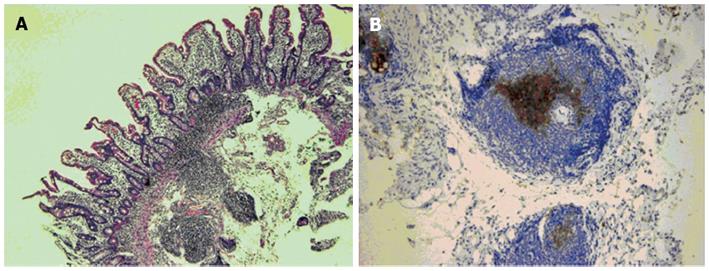
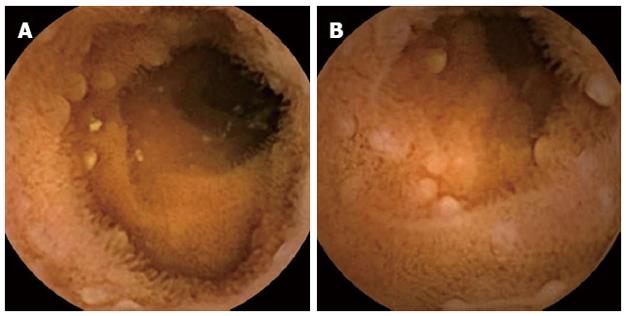
Esophagogastroduodenoscopy was performed with a high-definition imaging system (CV-260SL, Olympus, Tokyo) and a videoendoscope (GIF-H260, Olympus). Esophagogastroduodenoscopy revealed whitish polyps around the ampulla of Vater (Figure 1A and B). Polyps were also noticed in the third portion of the duodenum (Figure 1C). A close-up view of the lesion in the second portion of the duodenum revealed that the lesion was composed of two components: enlarged whitish villi and tiny submucosal whitish depositions (Figure 2A and B). These structures were more clearly visualized with a narrow-band imaging view (Figure 2C). Based on these endoscopic features, duodenal follicular lymphoma was highly suspected. Biopsy samples contained lymphoid follicles in the duodenal mucosa, and these were comprised of small to medium-sized lymphoid cells which had also infiltrated into the villi (Figure 3). The lymphoid cells were positive for CD20, CD10, and BCL2, but negative for CD3. Small bowel involvement was evaluated by video capsule endoscopy, and whitish polyps were detected as multiple jejunal lesions (Figure 4). A colonoscopy revealed no abnormality.
A bone marrow aspirate and biopsy were performed, and revealed that there was no infiltration of lymphoma cells in the bone marrow. Computed tomography (CT) scans of the neck, chest, abdomen and pelvis detected neither lymphadenopathy nor a thickened gastrointestinal wall (including the duodenum). An 18F-fluorodeoxyglucose positron emission tomography scan showed no abnormal accumulations of 18F-fluorodeoxyglucose. Consequently, the patient was diagnosed with primary intestinal follicular lymphoma, which was localized to the duodenum and the jejunum. The clinical stage was considered to be stage I, based on the Lugano staging system for the classification of gastrointestinal tract lymphomas[10,11].
The use of high-definition imaging systems is well established in the field of gastrointestinal endoscopy, and such systems are now also widely used as a routine examination tool. High-definition imaging technologies provide high-resolution pictures to reveal more detail than the traditional video endoscopy systems. In the present patient, several key features, such as whitish enlarged villi and tiny whitish depositions under the mucosa, were visualized by high-definition imaging without a magnifying endoscopy system. To our knowledge, this is the first report to describe these microsurface structures as characteristic findings of intestinal follicular lymphoma being detected by routine esophagogastroduodenoscopy without magnifying observation.
Primary intestinal follicular lymphoma is a distinct variant of systemic follicular lymphoma that was established within the last decade[1,12]. The representative feature in the conventional endoscopic observation is well known as small whitish polypoid nodules that can be up to 2 mm in diameter[2,3]. More detailed microsurface structures have been reported by several authors, based on magnified endoscopic findings of intestinal follicular lymphoma[4-9]. Norimura et al[8] summarized the magnified endoscopic findings of six patients with intestinal follicular lymphoma, and they reported that abnormalities of the villi and the presence of opaque white spots are possible pathognomonic features of this disease. Our patient’s endoscopic findings are in concordance with the report by Norimura. We speculate that these findings reflect pathological structures; infiltration of lymphoma cells into the villi are seen as enlargement of the villi, and lymphoid follicle formations are observed as opaque white spots or tiny white depositions. Thus, the above features might contribute to making the definite diagnosis of intestinal follicular lymphoma, although the sensitivity and specificity of these endoscopic features require further investigations.
In the present patient, esophagogastroduodenoscopy revealed multiple lesions, i.e., one lesion in the second portion and another lesion in the third portion of the duodenum. Video capsule endoscopy revealed additional lesions in the jejunum. Multiple sites of the gastrointestinal tract are frequently involved in patients with intestinal follicular lymphoma. Our previous study revealed that 46 out of 54 duodenal follicular lymphoma patients (85.2%) who underwent whole gastrointestinal tract surveillance had extensive involvement of the small intestine[13]. Other researchers also reported that the percentage of patients with multiple lymphoma lesions in the small intestine ranged from 66.7% to 100%[5,14-17]. Consequently, multiple lesions in the duodenum are another feature that is suggestive of intestinal follicular lymphoma.
Pathologically, the major differential diagnoses of follicular lymphoma include mucosa-associated lymphoid tumors (MALT) lymphoma, mantle cell lymphoma and reactive lymphoid hyperplasia. Neoplastic cells in low-grade B-cell lymphomas, namely, follicular lymphoma, MALT lymphoma and mantle cell lymphoma, share morphological features to some extent. Such lymphomas are primarily composed of small- to medium-sized lymphoid cells of B cell origin. Generally, subcategorizing low-grade B-cell lymphomas requires immunohistochemical staining. Typical follicular lymphoma consists of CD10-positive neoplastic lymphoid cells. In mantle cell lymphoma, the lymphoma cells are positive for CD5 and cyclin D1. In contrast, the lymphoma cells in MALT lymphoma are negative for CD10, CD5 and cyclin D1. Therefore, biopsy and immunohistochemical examination should be performed to make the distinct diagnosis of follicular lymphoma, when endoscopists find the aforementioned endoscopic features of small whitish polyps, enlarged whitish villi, tiny submucosal whitish depositions and/or multiple sites of involvement in the intestine.
In conclusion, we present a case of primary intestinal follicular lymphoma. Enlarged whitish villi, tiny submucosal whitish depositions, and multiple sites of involvement, were demonstrated in addition to the typical macroscopic morphology of whitish polyps. Routine esophagogastroduodenoscopy by a high-definition imaging system can provide detailed features, helping to diagnose intestinal follicular lymphoma even without magnifying endoscopy.
P- Reviewers Tandon RK, Nakase H S- Editor Jiang L L- Editor A E- Editor Zhang DN
| 1. | Harris NL, Swerdlow SH, Jaffe ES, Ott G, Nathwani BN, de Jong D, Yoshino T, Spagnolo D. Follicular lymphoma. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. Lyon: IARC 2008; 220-226. |
| 2. | Shia J, Teruya-Feldstein J, Pan D, Hegde A, Klimstra DS, Chaganti RS, Qin J, Portlock CS, Filippa DA. Primary follicular lymphoma of the gastrointestinal tract: a clinical and pathologic study of 26 cases. Am J Surg Pathol. 2002;26:216-224. [PubMed] |
| 3. | Yamamoto S, Nakase H, Yamashita K, Matsuura M, Takada M, Kawanami C, Chiba T. Gastrointestinal follicular lymphoma: review of the literature. J Gastroenterol. 2010;45:370-388. [PubMed] |
| 4. | Nakase H, Matsuura M, Mikami S, Chiba T. Magnified endoscopic view of primary follicular lymphoma at the duodenal papilla. Intern Med. 2007;46:141-142. [PubMed] |
| 5. | Higuchi N, Sumida Y, Nakamura K, Itaba S, Yoshinaga S, Mizutani T, Honda K, Taki K, Murao H, Ogino H. Impact of double-balloon endoscopy on the diagnosis of jejunoileal involvement in primary intestinal follicular lymphomas: a case series. Endoscopy. 2009;41:175-178. [PubMed] |
| 6. | Inoue N, Isomoto H, Shikuwa S, Mizuta Y, Hayashi T, Kohno S. Magnifying endoscopic observation of primary follicular lymphoma of the duodenum by using the narrow-band imaging system. Gastrointest Endosc. 2009;69:158-159; discussion 159. [PubMed] |
| 7. | Chowdhury M, Endo M, Chiba T, Kudara N, Oana S, Sato K, Akasaka R, Tomita K, Fujiwara S, Mizutani T. Characterization of follicular lymphoma in the small intestine using double-balloon endoscopy. Gastroenterol Res Pract. 2009;2009:835258. [PubMed] |
| 8. | Norimura D, Isomoto H, Imaizumi Y, Akazawa Y, Matsushima K, Inoue N, Yamaguchi N, Ohnita K, Shikuwa S, Arima T. Case series of duodenal follicular lymphoma, observed by magnified endoscopy with narrow-band imaging. Gastrointest Endosc. 2011;74:428-434. [PubMed] |
| 9. | Iwamuro M, Okuda M, Yumoto E, Suzuki S, Shirakawa A, Takata K, Yoshino T, Okada H, Yamamoto K. Magnifying endoscopy for intestinal follicular lymphoma is helpful for prompt diagnosis. Gut Liver. 2013;In press. |
| 10. | Zucca E, Roggero E, Bertoni F, Cavalli F. Primary extranodal non-Hodgkin’s lymphomas. Part 1: Gastrointestinal, cutaneous and genitourinary lymphomas. Ann Oncol. 1997;8:727-737. [PubMed] |
| 11. | Rohatiner A, d’Amore F, Coiffier B, Crowther D, Gospodarowicz M, Isaacson P, Lister TA, Norton A, Salem P, Shipp M. Report on a workshop convened to discuss the pathological and staging classifications of gastrointestinal tract lymphoma. Ann Oncol. 1994;5:397-400. [PubMed] |
| 12. | Yoshino T, Miyake K, Ichimura K, Mannami T, Ohara N, Hamazaki S, Akagi T. Increased incidence of follicular lymphoma in the duodenum. Am J Surg Pathol. 2000;24:688-693. [PubMed] |
| 13. | Takata K, Okada H, Ohmiya N, Nakamura S, Kitadai Y, Tari A, Akamatsu T, Kawai H, Tanaka S, Araki H. Primary gastrointestinal follicular lymphoma involving the duodenal second portion is a distinct entity: a multicenter, retrospective analysis in Japan. Cancer Sci. 2011;102:1532-1536. [PubMed] |
| 14. | Schmatz AI, Streubel B, Kretschmer-Chott E, Püspök A, Jäger U, Mannhalter C, Tiemann M, Ott G, Fischbach W, Herzog P. Primary follicular lymphoma of the duodenum is a distinct mucosal/submucosal variant of follicular lymphoma: a retrospective study of 63 cases. J Clin Oncol. 2011;29:1445-1451. [PubMed] |
| 15. | Akamatsu T, Kaneko Y, Ota H, Miyabayashi H, Arakura N, Tanaka E. Usefulness of double balloon enteroscopy and video capsule endoscopy for the diagnosis and management of primary follicular lymphoma of the gastrointestinal tract in its early stages. Dig Endosc. 2010;22:33-38. [PubMed] |