INTRODUCTION
Endoscopic ultrasound (EUS) was developed as a useful diagnosis modality and is used in the treatment of gastrointestinal and pancreatobiliary diseases. Since the development of EUS-guided fine needle aspiration (EUS-FNA) with a curved linear array echoendoscope, there have been many reports about the use of EUS-FNA for the treatment of various kinds of lesions. Subsequently, many authors have described other therapeutic uses for EUS, including EUS-guided biliary drainage, ethanol injection, and anti-tumor agent injection, etc., and these EUS-guided techniques have been termed “interventional EUS” procedures. In this article, we report the various applications of interventional EUS, especially focusing on recent updates.
EUS-GUIDED BILIARY ACCESS/DRAINAGE
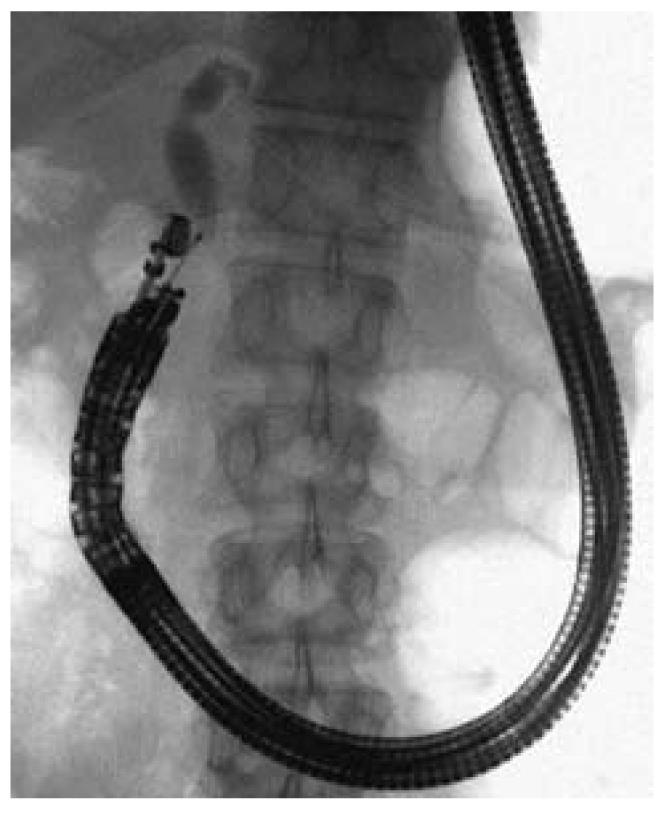
EUS-guided biliary drainage, which includes EUS-guided transpapillary rendezvous[1], choledochoduodenostomy[2], and hepatogastrostomy[3], has been described previously. Since endoscopic retrograde cholangiopancreatography (ERCP) is a transpapillary technique, these alternative techniques are indispensable when ERCP is unsuccessful in patients with obstructive jaundice or acute cholangitis. In 1996, Wiersema et al[4] first described EUS-guided cholangiography. Since then, various case studies have been reported; however, it still carries a risk of serious morbidity, including bile leakage, bleeding, or pneumoperitoneum[5,6]. In most series, the procedure has been described as follows: an echoendoscope is used, the bile duct is punctured with a 22-gauge needle under fluoroscopic guidance, and a guidewire is inserted into the bile duct. Then, a needle knife is used in incision mode under EUS guidance, and the bile duct is dilated up to 9-Fr by placing a dilator over the guidewire, before a self-expanding metallic stent is pushed through the choledochoduodenostomy site and into the extrahepatic bile duct[6]. The success rate has been reported to range from 50%-100%[7-10] in recent series, which suggests that EUS-guided biliary drainage is a feasible alternative to transpapillary drainage (Figure 1).
Figure 1 Endoscopic ultrasound-guided biliary drainage[5].
EUS-GUIDED PANCREATIC PSEUDOCYST DRAINAGE PROCEDURE
EUS-guided drainage has emerged as a treatment for pancreatic pseudocyst drainage, and the development of a large-channel echoendoscope has enabled it to be accomplished as a single step procedure[11]. Pancreatic pseudocysts sometimes become huge and symptomatic, and only a few cases are spontaneously resolved without effective treatment. For many years, surgical or percutaneous drainage has been the standard treatment. Recently, EUS-guided cystogastrostomy was developed and is now considered to be a feasible option for endoscopic treatment, as it is a very effective and minimally invasive approach for the management of symptomatic pancreatic pseudocysts. First, a linear echoendoscope is inserted into the stomach transorally, and pancreatic pseudocysts or fluid collections are identified. After it has been confirmed that the distance between the gastric wall and the cyst wall is less than 1 cm, a 19 G needle is inserted under EUS-guidance into the pseudocyst, and a guidewire is placed into and coiled within the pseudocyst under fluoroscopic guidance. Subsequently, the needle is retrieved, and the gastric wall is dilated with a dilator; and finally, a nasocystic drainage tube or double pig-tail tube is put in place to drain the pseudocyst into the intestine. Some high quality case reports involving this procedure have been published[12]. Varadarajulu compared the clinical outcomes of EUS-guided cystogastrostomy with surgical cystogastrostomy for the management of patients with uncomplicated pancreatic pseudocysts. There were no significant differences in success rates (100% vs 95%, P = 0.36), procedural complications (none in either cohort), or reinterventions (10% vs 0%, P = 0.13) between the surgery and EUS-guided cystogastrostomy[13]. Varadarajulu also performed a cohort study involving a total of 60 cases to evaluate the rates of technical success, treatment success, and complications and reported that the rates of technical and treatment success were 95% and 93%, respectively. The minor complication of stent migration was encountered in 1 of 60 patients (1.7%)[14]. These reports demonstrate that EUS-guided cystogastrostomy is technically feasible and is associated with a clinically similar outcome to surgical treatment.
FORWARD-VIEWING ENDOSCOPIC ULTRASOUND FOR INTERVENTIONAL EUS
Recently, a forward-viewing curved echoendoscope, which is expected to encourage the development of novel procedural techniques for interventional EUS, has been developed as an alternative to the linear array echoendoscope. The forward-viewing curved echoendoscope was first introduced for pancreatic pseudocyst drainage in 2007[15]. Its main modifications are forward-viewing options and a curved-linear array with a narrow field of vision. However, the working channel does not have a forceps elevator. Voermans et al[15,16] reported that this echoendoscope has the advantage of enabling the creation of a cystogastrostomy and/or duodenostomy guided by EUS without having to puncture at an angle. The straight line configuration of the scope enables the axial application of force during needle insertion and stenting. Some cases in which the forward-viewing echoendoscope was used for pancreatic pseudocyst drainage have been reported[2,16,17]. In these cases, the pseudocyst was visualized via the forward-viewing echoendoscope with color Doppler to allow the vasculature to be avoided, and then a 19-gauge needle was inserted into the pseudocyst under EUS guidance. Alternatively, a technique similar to that used for cystogastrostomy with a linear array echoendoscope was employed. Since the echoendoscope and the needle are held in a straight line, the device can be maintained in the same position throughout the procedure, making it less difficult than using a linear array echoendoscope. However, the forward-viewing echoendoscope has some limitations including its narrow imaging range and the absence of a forceps elevator[18], and so further large-scale studies are needed to evaluate the forward-viewing echoendoscope.
EUS-GUIDED ONCOLOGIC INTERVENTIONS
EUS-guided fine needle injection of chemotherapeutics, fiducial marker placement, and brachytherapy have also been described. TNFrade (GenVec, Gaithersburg, Md) is an injectable agent that is injected into unresectable pancreatic tumors under EUS-guidance[19]. Then, conventional chemoradiotherapy is added to facilitate tumor death. Despite significant effectiveness being noted at 1 year, overall survival was not significantly improved. Another group reported on EUS-guided paclitaxel injection using OncoGel (ReGel/paclitaxel, BTG International, West Conshocken, PA), which resulted in the high localization of paclitaxel in the pancreas without pancreatitis[20]. The same group has also used LC beads (Biocompatibles International plc, Farnham, Surrey, United Kingdom), which are designed for the delivery of the chemotherapeutic agent irinotecan, to transport the agent into the pig pancreas. In addition, the delivery of OncoVex-GMCSF or 5-FU sustained polymer into the pancreas has also been described[21].
Gold fiducial marker placement has been described for stereotactic body radiotherapy for locally advanced pancreatic cancer[22] or other abdominal applications, often in combination with the Cyberknife system. Pishvaian et al[23] reported their experiences of EUS-guided fiducial marker placement, which was successful in 84.6% of cases. In addition, a 19 gauge needle was used in previous series, and some recent reports described the use of a 22 gauge needle for fiducial placement into multiple sites; therefore, and further large series are needed to evaluate which needle is most useful for treating pancreatic cancer.
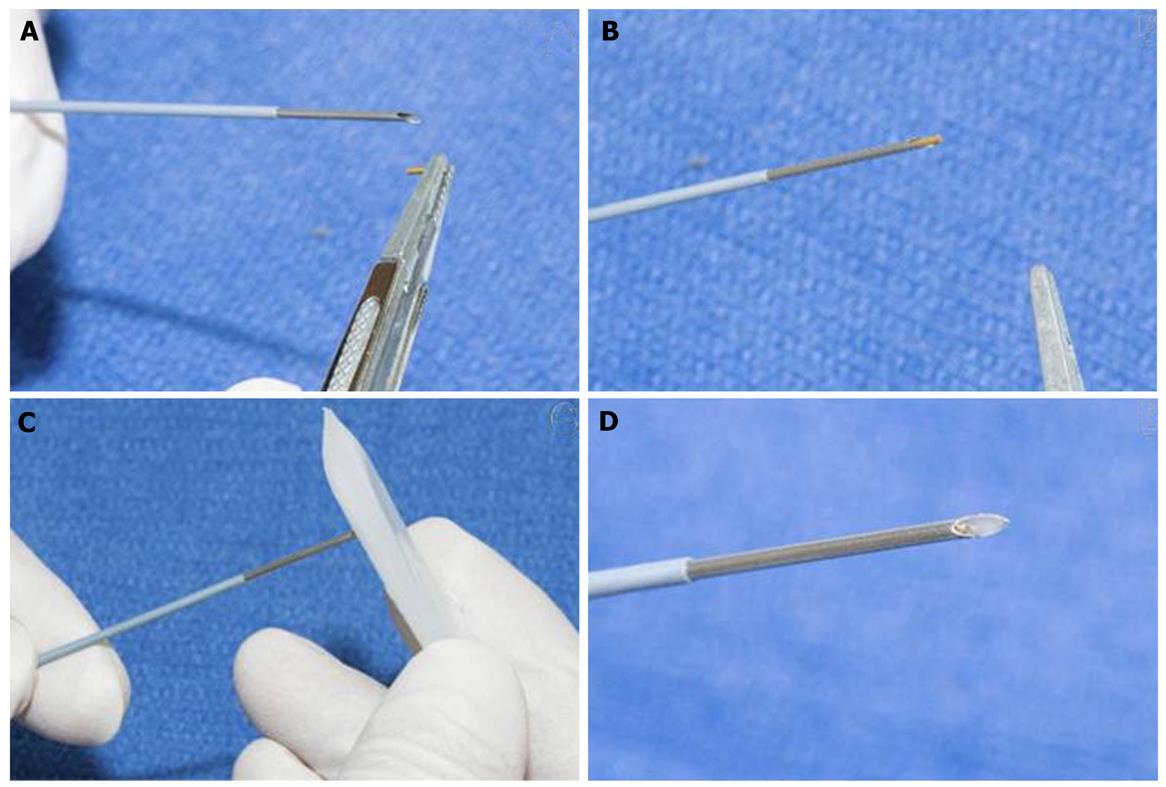
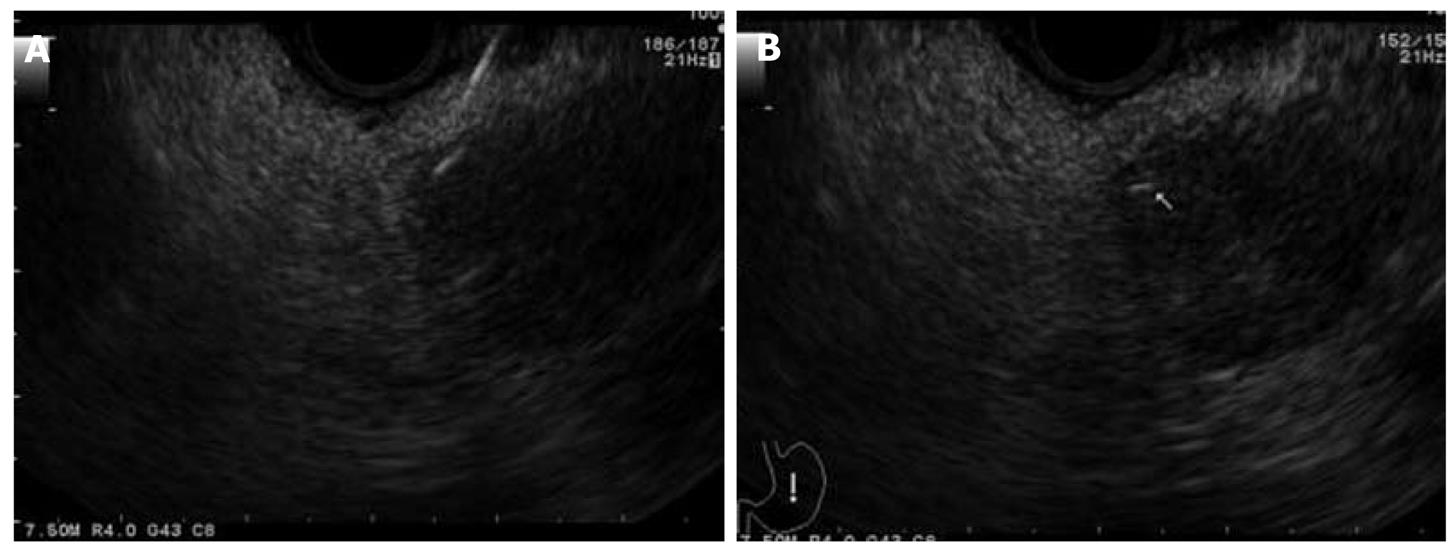
EUS-guided brachytherapy (EUS-BrTx) was first reported in 1999[24] and is still limited to small case series, which revealed that this technique results in temporary pain relief and a marginal survival benefit. EUS-BrTx is currently widely used for treating tumors in various locations such as head and neck cancer, esophageal cancer, rectal cancer, and pancreatic cancer. Sun et al[25] reported their experience of EUS-BrTx in a total of 15 cases of unresectable pancreatic cancer in which 11 to 33 seeds were implanted per patient. They reported a mean radioactivity of 0.89 mCi per seed and a mean total implanted activity of 20 mCi, and the treatment resulted in a partial response rate of 26.7%, a minor response rate of 20%, a stable disease rate of 33.3%, and a disease progression rate of 20%. These reports are still preliminary experiences, and further development and larger series are needed to evaluate these techniques in more detail (Figures 2 and 3).
Figure 2 Endoscopic ultrasound-guided fiducial marker placement for locally advanced pancreatic cancer[22].
Figure 3 Endoscopic ultrasound-guided fiducial marker placement for locally advanced pancreatic cancer[22].
EUS-GUIDED PANCREATIC CYST ABLATION
EUS-guided pancreatic cyst ablation using ethanol has recently been reported. In this procedure, 80%-99% ethanol is injected using an EUS-guided fine needle with or without chemotherapeutic agents. The complete cyst eradication rates are 33% to 79% at the 3 mo to 12 mo follow-up periods; however, complications, including mild pancreatitis or abdominal pain, have been reported to be associated with this procedure[26-28]. In addition, experience of this method is limited, and further evaluations are needed.
EUS-GUIDED GASTROINTESTINAL TRACT INTERVENTIONS
EUS-guided luminal anastomosis has been reported in some small studies. Fritscher-Ravens et al[29] reported the feasibility of EUS-guided gastrojejunostomy in a swine model. Sakamoto et al[30] reported on the use of endoscopic pancreaticogastrostomy reconstruction with pancreatic stent placement for pancreatic stenosis after surgery. A 19 gauge needle was inserted into the main pancreatic duct via the gastric wall under EUS guidance, and after guidewire placement and dilatation using a 6-Fr dilator, followed by a 5-Fr dilator, a 5 cm pancreatic stent was put in place. Kamaka et al[31] reported endoscopic ultrasound guided transluminal removal of gallstones. To do this, they employed EUS-guided choledochoduodenostomy; i.e., a 19 gauge needle was used to puncture the gallbladder, a 0.035-inch guidewire was placed and coiled inside the gallbladder, the gastric wall was dilated to 9-Fr using dilators, and a pig-tail type stent was deployed in the gallbladder. After 11 d, a 4 cm covered metal stent was inserted via the fistula, and the gallstones were removed via the choledochoduodenostomy. However, these reports are preliminary and experimental, and further clinical trials are needed; however, it has been proven that EUS-guided interventions in the gastrointestinal tract are feasible.
CONCLUSION
Most of these EUS-guided interventions are experimental. More innovations to facilitate safe EUS-guided interventions are needed including novel techniques and devices. Well-designed clinical trials are also necessary, and EUS-guided interventions could be applied to many applications in future.
Peer reviewer: David J Desilets, MD, PhD, Chief, Assistant Professor of Clinical Medicine, Tufts University School of Medicine, Springfield Campus, Baystate Medical Center, Springfield, MA 01199, United States
S- Editor Yang XC L- Editor A E- Editor Yang XC