Published online May 16, 2012. doi: 10.4253/wjge.v4.i5.197
Revised: January 1, 2012
Accepted: April 27, 2012
Published online: May 16, 2012
A phytobezoar is one of the intraluminal causes of gastric outlet obstruction, especially in patients with previous gastric surgery and/or gastric motility disorders. Before the proton pump inhibitor era, vagotomy, pyloroplasty, gastrectomy and gastrojejunostomy were commonly performed procedures in peptic ulcer patients. One of the sequelae of gastrojejunostomy is phytobezoar formation. However, a bezoar causing gastric outlet obstruction is rare even with giant gastric bezoars. We report a rare case of gastric outlet obstruction due to a phytobezoar obstructing the efferent limb of the gastrojejunostomy site. This phytobezoar which consisted of a whole piece of okra (lady finger vegetable) was successfully removed by endoscopic snare. To the best of our knowledge, this is the first case of okra bezoar-related gastrojejunostomy efferent limb obstruction reported in the literature.
- Citation: Zin T, Maw M, Pai DR, Paijan RB, Kyi M. Efferent limb of gastrojejunostomy obstruction by a whole okra phytobezoar: Case report and brief review. World J Gastrointest Endosc 2012; 4(5): 197-200
- URL: https://www.wjgnet.com/1948-5190/full/v4/i5/197.htm
- DOI: https://dx.doi.org/10.4253/wjge.v4.i5.197
Gastric bezoars are a form of concretion resulting from the accumulation of ingested materials. They are relatively rare and are found in less than 1% of patients undergoing gastroscopy[1]. The nature of the contents classifies gastric bezoars into many types. Common bezoars are phytobezoars, trichobezoars and pharmacobezoars. Among the various types of bezoars, the most common type is the phytobezoars, which are composed mainly of undigested vegetable materials.
Generally, gastric phytobezoars are common in patients with dentition problems, impaired digestion, decreased gastric motility and previous gastric surgery[2,3]. They usually have a wide range of clinical presentations from abdominal discomfort and weight loss to small bowel obstruction[4]. Gastric outlet obstruction is an uncommon presentation of gastric bezoars even when they occupy the whole stomach. We report a patient who previously underwent gastrectomy and gastrojejunostomy for duodenal ulcer and who presented with signs and symptoms of partial gastric outlet obstruction due to a phytobezoar obstructing the gastrojejunostomy efferent limb.
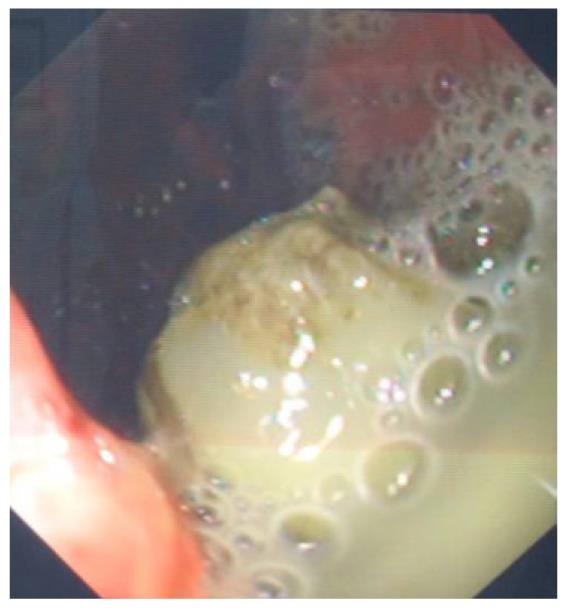
A 67-year-old gentleman presented with intermittent epigastic pain of one month duration. He was suffering from pain associated with vomiting. His vomitus contained old food particles and some bile. He had a history of gastrectomy and gastrojejunostomy for peptic ulcer disease in the previous 30 years. Clinically, he had a distended stomach with a positive succession splash. There was some tooth loss which caused mastication problems. Gastroscopy revealed a distended stomach containing undigested food particles mixed with bile and mucus. The gastrojejunostomy site appeared adequate and no signs of ulceration or stricture were noted. The afferent limb was patent with free flowing bile during intubation. A golf ball-sized phytobezoar was found obstructing the efferent limb area of the gastrojejunostomy (Figure 1). It was successfully removed using an endoscopic snare. Examination of the bezoar after removal revealed an inner core formed from a whole piece of okra (Figure 2). The patient was well following removal of the phytobezoar, and was given appropriate dietary advice upon discharge to prevent recurrence.
Gastric bezoars are formed due to the accumulation of ingested materials in the form of concretions. They are rare and found in less than 1% of patients who undergo gastroscopy[1]. The commonest type of bezoar is a phytobezoar which is composed of vegetable material[5]. In our case, the centre of the bezoar was formed by a whole piece of okra; lady finger vegetable. Trichobezoars are composed of swallowed hairs in patients with psychiatric disorders. High fibre persimmon fruits can cause diospyrobezoars, and pharmacobezoars are composed of ingested medications.
The pathogenesis of bezoar formation is usually intricate. It involves many factors such as improper mastication, dentition problems, alterations in the production of acid, pepsin and mucus, previous gastric surgery and impairments in gastric motility[6,7]. Robles et al[8] pointed out that 20% of patients have mastication and dentition problems, 70%-94% have had previous gastric surgery and 40% have a history of excessive dietary fibre intake. Most adults with phytobezoars are men between the ages of 40 and 50 years, however, trichobezoars usually occur in young women with psychiatric problems[4,9].
Patients with gastric bezoars may remain asymptomatic for many years. Common symptoms usually include abdominal pain, nausea, vomiting, early satiety, anorexia and weight loss. Some patients present with gastrointestinal bleeding from gastric ulcer formation due to bezoar-induced pressure necrosis[4]. However, gastric outlet obstruction is an uncommon presentation in patients with gastric bezoars, even though some are large enough to fill the whole stomach. Leung et al[10] reported a case of bezoar-induced gastric outlet obstruction in a patient who had a previous gastrojejunostomy for peptic ulcer disease in whom they found a stricture at the anastomotic site. In another study, a large bezoar was found to occlude the afferent loop of the gastrojejunostomy, this patient also had afferent loop syndrome which was diagnosed by ultrasound and computed tomography (CT)[11]. In our report, the patient vomited old food indicating a gastric outlet obstruction; however, the presence of bile meant that the afferent loop of the gastrojejunostomy was still patent. Gastric outlet obstruction was due to occlusion of the efferent limb by a whole okra phytobezoar.
Gastric bezoars are usually discovered incidentally in patients with non-specific abdominal symptoms. Abdominal X rays, ultrasound and CT scan can reveal mass or filling defects[12,13]. The current gold standard for diagnosis of a gastric bezoar is upper gastrointestinal endoscopy. It provides not only direct visualization of the bezoar but also allows simultaneous therapeutic intervention.
Many studies have shown successful dissolution of gastric bezoars using agents such as Coca-cola, acetylcystine, cellulase, meat tenderizer and hydrogen peroxide[5,14-19]. However, all available studies are uncontrolled trials and there are no prospective studies evaluating the medical treatment of phytobezoars in the literature.
The majority of gastric bezoars can be removed endoscopically. Endoscopic removal involves fragmenting the bezoar with a water jet, direct suction, forceps and snares[20]. A variety of other methods have been described in case reports such as Nd:YAG laser, endoscopic drills, and mechanical, electrohydraulic, extracorporeal lithotriopsy and intra-phytozoal Coca-Cola injection[21-26]. Bruzzese et al[27] pointed out that any fragments more than one centimetre in size must be extracted after fragmentation to prevent intestinal obstruction.
Surgical removal should be considered in patients who fail conservative therapy, have large bezoars which hinder endoscopic removal or have complications such as obstruction with underlying mechanical problems, as seen in Edmund Leung’s study, and associated peptic ulcer bleeding[10]. Laparoscopic removal is a promising option for the removal of gastric as well as intestinal bezoars to avoid conventional surgery which is associated with higher postoperative morbidity[28].
The reported recurrence rate after removal of a gastric bezoar is 14% in some studies, however, this will be higher if underlying risk factors are not corrected[29]. For prevention, it is necessary to educate high risk patients to chew properly, take more fluid and avoid a stringy fibrous diet. Patients with trichobezoars may need to seek psychiatric evaluation to avoid further occurrence. Patients with underlying motility problems also need to be identified and treated as necessary.
Phytobezoars are a rare cause of gastric outlet obstruction, especially in patients with previous gastrojenunostomy. Currently, gastroscopy is the best method for detecting and managing gastric bezoars by endoscopic removal. Some cases require surgical removal, especially those associated with complications. The most important points in the management of a bezoar are identification of the causative factor and prevention of recurrence by counselling.
We thank all the staff at the endoscopic centre; Hospital Pakar Sultanah Fatimah, for help obtaining the necessary information required for this paper and special thanks to the research committee; Melaka Manipal Medical College, who gave training in research paper writing and encouragement for publication.
Peer reviewer: Makoto Hashizume, MD, PhD, FACS, Professor and Chairman, Department of Advanced Medical Initiatives, Faculty of Medical Sciences, Kyushu University, 3-1-1, Maidashi, Higashi-ku, Fukuoka 812-8582, Japan
S- Editor Yang XC L- Editor Webster JR E- Editor Yang XC
| 1. | Kadian RS, Rose JF, Mann NS. Gastric bezoars--spontaneous resolution. Am J Gastroenterol. 1978;70:79-82. [PubMed] |
| 2. | Mir AM, Mir MA. Phytobezoar after vagotomy with drainage or resection. Br J Surg. 1973;60:846-849. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 21] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | Calabuig R, Navarro S, Carrió I, Artigas V, Monés J, Puig LaCalle J. Gastric emptying and bezoars. Am J Surg. 1989;157:287-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 21] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | De Bakey M, Ochsner A. Bezoars and concretions: a comprehensive review of the literature with an analysis of 303 collected cases and a presentation of 8 additional cases. Surgery. 1939;5:132-160. |
| 5. | Holloway WD, Lee SP, Nicholson GI. The composition and dissolution of phytobezoars. Arch Pathol Lab Med. 1980;104:159-161. [PubMed] |
| 6. | White NB, Gibbs KE, Goodwin A, Teixeira J. Gastric bezoar complicating laparoscopic adjustable gastric banding, and review of literature. Obes Surg. 2003;13:948-950. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Ahn YH, Maturu P, Steinheber FU, Goldman JM. Association of diabetes mellitus with gastric bezoar formation. Arch Intern Med. 1987;147:527-528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 31] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Robles R, Parrilla P, Escamilla C, Lujan JA, Torralba JA, Liron R, Moreno A. Gastrointestinal bezoars. Br J Surg. 1994;81:1000-1001. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 66] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 9. | Balik E, Ulman I, Taneli C, Demircan M. The Rapunzel syndrome: a case report and review of the literature. Eur J Pediatr Surg. 1993;3:171-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 30] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Leung E, Barnes R, Wong L. Bezoar in gastro-jejunostomy presenting with symptoms of gastric outlet obstruction: a case report and review of the literature. J Med Case Reports. 2008;2:323. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Hui MS, Perng HL, Choi WM, Chem LK, Yang KC, Chen TJ. Afferent loop syndrome complicated by a duodenal phytobezoar after Billroth-II subtotal gastrectomy. Am J Gastroenterol. 1997;92:1550-1552. [PubMed] |
| 12. | McCracken S, Jongeward R, Silver TM, Jafri SZ. Gastric trichobezoar: sonographic findings. Radiology. 1986;161:123-124. [PubMed] |
| 13. | Newman B, Girdany BR. Gastric trichobezoars--sonographic and computed tomographic appearance. Pediatr Radiol. 1990;20:526-527. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 36] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Walker-Renard P. Update on the medicinal management of phytobezoars. Am J Gastroenterol. 1993;88:1663-1666. [PubMed] |
| 15. | Schlang HA. Acetylcysteine in removal of bezoar. JAMA. 1970;214:1329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Ladas SD, Triantafyllou K, Tzathas C, Tassios P, Rokkas T, Raptis SA. Gastric phytobezoars may be treated by nasogastric Coca-Cola lavage. Eur J Gastroenterol Hepatol. 2002;14:801-803. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 95] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 17. | Kato H, Nakamura M, Orito E, Ueda R, Mizokami M. The first report of successful nasogastric Coca-Cola lavage treatment for bitter persimmon phytobezoars in Japan. Am J Gastroenterol. 2003;98:1662-1663. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 32] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 18. | Chung YW, Han DS, Park YK, Son BK, Paik CH, Jeon YC, Sohn JH. Huge gastric diospyrobezoars successfully treated by oral intake and endoscopic injection of Coca-Cola. Dig Liver Dis. 2006;38:515-517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 37] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 19. | Katsinelos P, Pilpilidis I, Chatzimavroudis G, Katsinelos T, Lazaraki G, Fasoulas K, Zavos C, Kountouras J. Huge gastric bezoar caused by honeycomb, an unusual complication of health faddism: a case report. Cases J. 2009;2:7077. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 20. | Zarling EJ, Thompson LE. Nonpersimmon gastric phytobezoar. A benign recurrent condition. Arch Intern Med. 1984;144:959-961. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 21. | Naveau S, Poynard T, Zourabichvili O, Poitrine A, Chaput JC. Gastric phytobezoar destruction by Nd: YAG laser therapy. Gastrointest Endosc. 1986;32:430-431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 22. | Benes J, Chmel J, Jodl J, Stuka C, Nevoral J. Treatment of a gastric bezoar by extracorporeal shock wave lithotripsy. Endoscopy. 1991;23:346-348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 23. | Wang YG, Seitz U, Li ZL, Soehendra N, Qiao XA. Endoscopic management of huge bezoars. Endoscopy. 1998;30:371-374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 63] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 24. | Blam ME, Lichtenstein GR. A new endoscopic technique for the removal of gastric phytobezoars. Gastrointest Endosc. 2000;52:404-408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 42] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 25. | Sechopoulos P, Robotis JF, Rokkas T. Gastric bezoar treated endoscopically with a carbonated beverage: case report. Gastrointest Endosc. 2004;60:662-664. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 26. | Gold MH, Patteson TE, Green GI. Cellulase bezoar injection: a new endoscopic technique. Gastrointest Endosc. 1976;22:200-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 27. | Bruzzese A, Chiarini S, Marchegiani C, Corbellini L, Stella S. [Endoscopic fragmentation of gastric phytobezoars as a valid alternative, in selected cases, to traditional surgery]. G Chir. 1997;18:485-487. [PubMed] |
| 28. | Sharma D, Srivastava M, Babu R, Anand R, Rohtagi A, Thomas S. Laparoscopic treatment of gastric bezoar. JSLS. 2010;14:263-267. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 33] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 29. | Krausz MM, Moriel EZ, Ayalon A, Pode D, Durst AL. Surgical aspects of gastrointestinal persimmon phytobezoar treatment. Am J Surg. 1986;152:526-530. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 73] [Article Influence: 1.9] [Reference Citation Analysis (0)] |