Published online May 16, 2012. doi: 10.4253/wjge.v4.i5.194
Revised: September 12, 2011
Accepted: March 30, 2012
Published online: May 16, 2012
Churg-Strauss syndrome (CSS) is a systemic vascular disorder characterized by severe bronchial asthma, hypereosinophilia, and allergic rhinitis. Small intestinal ulcers associated with CSS are a relatively rare manifestation that causes gastrointestinal bleeding. Multiple deep ulcers with an irregular shape are characteristic of small intestinal involvement of CSS. Video-capsule-endoscopy (VCE), double-balloon endoscopy (DBE) and Spirus assisted enteroscopy have been developed recently and enabled observation of the small intestine. In this case report, we have described a patient with CSS who had multiple deep ulcers in the jejunum detected by oral DBE. Since severe gastrointestinal (GI) involvement has been identified as an independent factor associated with poor outcome, the careful investigation of GI tract must be needed for CSS patients with GI symptoms. We describe the usefulness of DBE for diagnosis of small intestinal ulcers in patient with CSS.
- Citation: Suzuki T, Matsushima M, Arase Y, Fujisawa M, Okita I, Igarashi M, Koike J, Mine T. Double-balloon endoscopy-diagnosed multiple small intestinal ulcers in a Churg-Strauss syndrome patient. World J Gastrointest Endosc 2012; 4(5): 194-196
- URL: https://www.wjgnet.com/1948-5190/full/v4/i5/194.htm
- DOI: https://dx.doi.org/10.4253/wjge.v4.i5.194
Churg-Strauss syndrome (CSS), also known as allergic granulomatous angiitis, is a relatively rare systemic vascular disorder. The organ most often affected is the lung, followed by the skin. The gastrointestinal (GI) tract may be involved in approximately 20%-50% of the patients with CSS[1]. The main GI tract symptoms are abdominal pain, diarrhea, and bleeding. However, the involvement of the small intestine is a rare complication, often detected during an emergent operation for treatment of intestinal perforation[2-4]. Previous reports of CSS provided only a few details regarding small intestinal ulcerations.
Double-balloon endoscopy (DBE) is a relatively new endoscopic device designed to visualize the entire small intestine[5]. Observation of the entire small intestine can be performed using an oral and/or anal DBE approach. Endoscopic interventions, such as biopsy, clipping, argon plasma coagulation, balloon dilatation, and endoscopic mucosal resection, can also be performed by DBE. In Japan, DBE is mainly used to find the origin of obscure GI bleeding in cases where the bleeding cause cannot be revealed by the usual methods, such as esophagogastroduodenoscopy, colonoscopy, or radiologic evaluation of small intestine[6].
We report a case of CSS with multiple small intestinal ulcers that were successfully detected by DBE without a surgical procedure.
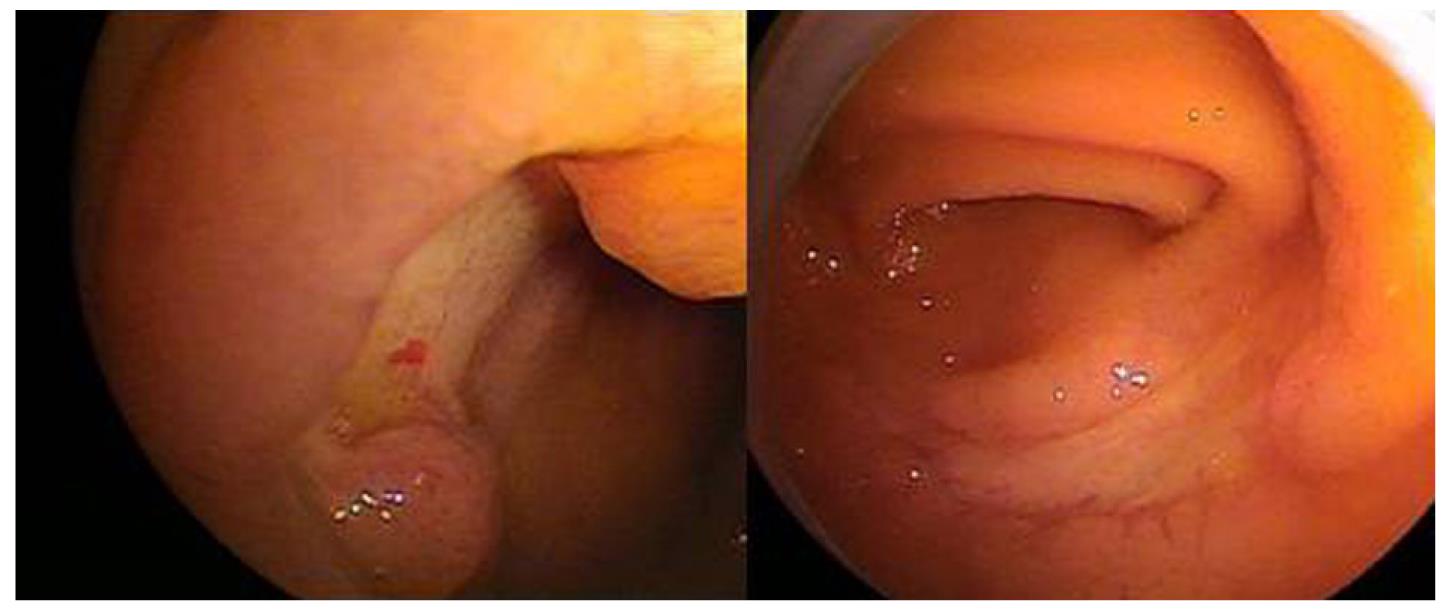
A 79 year-old man with a 2 year history of severe CSS that had been treated by corticosteroids was admitted to Tokai University Hospital because of a 3 d history of tarry stool, edema of the lower extremities and facial swelling. His medical records showed that he had a 7 year history of bronchial asthma and a 2 year history of chronic renal failure. A physical examination revealed severe anemia, facial swelling, and edema of the lower limbs. His blood pressure was 130/60 mmHg, his pulse was 90/min and regular, and his body temperature was 36.3 °C. No tenderness on palpation of the abdomen was observed; bowel sounds were noted. Digital examination revealed tarry stool. Neurological examination revealed sensory and motor disturbance of both legs, which is compatible with mononeuritis multiplex. Laboratory analyses included the following: white blood cell count, 6400/mm3 (4000-8000/mm3) with 0.2% eosinophils (1%-4%); hemoglobin, 4.6 g/dL (13.5-17.5 g/dL); platelet count, 127 000/mm3 (140 000-400 000/ mm3); erythrocyte sedimentation rate, 10 mm/h (1- 10 mm/h); C-reactive protein, 0.2 mg/dL (-0.3 mg/dL); IgE, 504 U/mL (-500 U/mL); myeloperoxidase-antineutrophil cytoplasmic antibodies (p-ANCA), 226 EU (< -20 EU). A computed tomographic scan of the abdomen showed no abnormalities. Emergency esophagogastroduodenoscopy showed that there was no bleeding source in the esophagus, duodenum, or stomach, but that gastritis was present. Since 1st DBE consensus meeting in Japan had recommended that DBE with oral approach had been indicated in the cases with overt ongoing bleeding, oral DBE (EN-450T5/20; Fujinon Co, Ltd, Saitama City, Japan) was performed on the 2nd day after his admission; “punched-out” multiple ulcers without visible vessels at the ulcer floor were observed (Figure 1) in the upper jejunum. There were no procedure-related complications. It is quite difficult to diagnose a possible pathological condition from the findings of small intestinal ulcers, because small intestinal ulcers are observed in a number of pathological conditions, such as Crohn’s disease, mesenteric ischemia, lymphoma, ulcerated cancer, drug-related injuries, vasculitides, connective tissue disorders, and infections[7]. In this case, biopsy specimens obtained from the ulcerative lesions on DBE did not reveal any specific findings such as eosinophilic infiltration, ischemic change, or malignancy. Because his medical history documented that he had not recently received any medication involving non-steroidal anti-inflammatory drugs or antibiotics, drug-related small intestinal injuries were excluded. Developing tarry stool, edema and mononeuritis multiplex suggested that his condition should be considered a relapse of his CSS. Therefore, prednisolone (30 mg daily) was delivered intravenously for 20 d; the tarry stool improved and gradually tapered off without relapse.
CSS is classified as a systemic vasculitis that affects small- to medium- sized vessels associated with bronchial asthma, hypereosinophilia, and allergic rhinitis. The American College of Rheumatology has proposed the following six criteria for defining CSS: asthma; eosinophilia greater than 10% on differential white blood cell count; paranasal sinus abnormality; migratory or transient pulmonary infiltrates detected radiographically; mononeuropathy (including multiplex) or polyneuropathy; and biopsy containing a blood vessel showing the accumulation of eosinophils in extravascular areas. The presence of four or more of these criteria yields a sensitivity of 85% and a specificity of 99.7% for CSS[8]. In the present case, the diagnosis was arrived at by the presence of five of these six criteria, paranasal sinusitis being the exception, when he was 77 years old. At that time, a skin biopsy was performed on his left lower extremity, and the section showed marked infiltration of eosinophils at the perivascular and peri-adnexal regions in the dermis.
The clinical elements of CSS occur in three sequential phases: prodromal, eosinophilic, and vasculitic. The prodromal phase is characterized by atopic disease, allergic rhinitis, and asthma. Features of the eosinophilic phase include peripheral blood eosinophilia and eosinophilic infiltration of multiple organs, especially of the lung and GI tract. In the vasculitic phase, a life-threatening systemic vasculitis of the medium and small vessels frequently occurs. The vasculitic phase may be heralded by disparate nonspecific signs and symptoms related to the cardiovascular, gastrointestinal, epidermal, renal, musculoskeletal, and nervous systems. This patient was in the vasculitic phase; he had variety of symptoms, such as GI bleeding, weight loss, malaise, sensory and motor disturbance of both legs, and dyspnea resulting from chronic cardiac failure. A long-term follow-up study conducted by Guillevin et al[9] revealed that the presence of renal insufficiency, proteinuria (> 1 g/d), central nervous system or cardiac involvement, and GI disease are indicators of poor prognosis. When the patient in the present case was admitted to our hospital, he already had all these clinical factors, suggesting that his five-year survival rate was approximately 54%.
Among the GI signs reported in a study by Lanham et al[10] abdominal pain occurred in 59%, diarrhea in 33%, and bleeding in 18% of patients with CSS. Ulceration, perforation, and stenosis of the GI tract are assumed to be the results of ischemia caused by vasculitis. Although the stomach, duodenum, or colon is often involved in those lesions in patients, the small intestine is rarely involved. A recent report showed video-capsule-endoscopy (VCE) to be a useful tool for diagnosis of GI involvement, especially in the small intestine in a patient with CSS[11]. However this procedure has limitations, such as the unavailability of taking biopsy specimens and of performing therapeutic intervention. There has been no report on an image of small intestinal ulcers associated with CSS detected by balloon-endoscopy. To the best of our knowledge, this is the first report using DBE to show an image of multiple ulcers in the small intestine in a case of CSS. Since typical histological findings such as vasculitis or granuloma could be obtained in approximately one fourth of CSS patients by taking a biopsy from gastrointestinal tissue and therapeutic intervention could subsequently be performed, DBE could represent an important diagnostic and therapeutic tool for small intestinal involvement. In conclusion, DBE in combination with VCE might become a complimentary procedure to diagnose the small intestinal involvement in patients with CSS.
Peer reviewers: Reena Sidhu, MRCP, MD, Department of Gastroenterology, Royal Hallamshire Hospital, 15 Barncliffe Road, Fulwood, Sheffield S10 4DF, United Kingdom; Sherman M Chamberlain, Associate Professor of Medicine, Section of Gastroenterology, BBR-2538, Medical College of Georgia, Augusta, GA 30912, United States; Sheng-Lei Yan, MD, Division of Gastroenterology, Department of Internal Medicine, Chang Bing Show Chwan Memorial Hospital, No.6, Lugong Rd., Lugang Township, Changhua County 505, Taiwan, China
S- Editor Yang XC L- Editor A E- Editor Yang XC
| 1. | Chumbley LC, Harrison EG, DeRemee RA. Allergic granulomatosis and angiitis (Churg-Strauss syndrome). Report and analysis of 30 cases. Mayo Clin Proc. 1977;52:477-484. [PubMed] |
| 2. | Murakami S, Misumi M, Sakata H, Hirayama R, Kubojima Y, Nomura K, Ban S. Churg-Strauss syndrome manifesting as perforation of the small intestine: report of a case. Surg Today. 2004;34:788-792. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Nakamura Y, Sakurai Y, Matsubara T, Nagai T, Fukaya S, Imazu H, Hasegawa S, Ochiai M, Funabiki T, Mizoguchi Y. Multiple perforated ulcers of the small intestine associated with allergic granulomatous angiitis: report of a case. Surg Today. 2002;32:541-546. [PubMed] |
| 4. | Ahn E, Luk A, Chetty R, Butany J. Vasculitides of the gastrointestinal tract. Semin Diagn Pathol. 2009;26:77-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 5. | Yamamoto H, Sekine Y, Sato Y, Higashizawa T, Miyata T, Iino S, Ido K, Sugano K. Total enteroscopy with a nonsurgical steerable double-balloon method. Gastrointest Endosc. 2001;53:216-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 896] [Cited by in RCA: 861] [Article Influence: 35.9] [Reference Citation Analysis (0)] |
| 6. | Yamamoto H, Kita H, Sunada K, Hayashi Y, Sato H, Yano T, Iwamoto M, Sekine Y, Miyata T, Kuno A. Clinical outcomes of double-balloon endoscopy for the diagnosis and treatment of small-intestinal diseases. Clin Gastroenterol Hepatol. 2004;2:1010-1016. [PubMed] |
| 7. | Gay G, Delvaux M, Frederic M. Capsule endoscopy in non-steroidal anti-inflammatory drugs-enteropathy and miscellaneous, rare intestinal diseases. World J Gastroenterol. 2008;14:5237-5244. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 17] [Cited by in RCA: 17] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Masi AT, Hunder GG, Lie JT, Michel BA, Bloch DA, Arend WP, Calabrese LH, Edworthy SM, Fauci AS, Leavitt RY. The American College of Rheumatology 1990 criteria for the classification of Churg-Strauss syndrome (allergic granulomatosis and angiitis). Arthritis Rheum. 1990;33:1094-1100. [PubMed] |
| 9. | Guillevin L, Cohen P, Gayraud M, Lhote F, Jarrousse B, Casassus P. Churg-Strauss syndrome. Clinical study and long-term follow-up of 96 patients. Medicine (Baltimore). 1999;78:26-37. [PubMed] |
| 10. | Lanham JG, Elkon KB, Pusey CD, Hughes GR. Systemic vasculitis with asthma and eosinophilia: a clinical approach to the Churg-Strauss syndrome. Medicine (Baltimore). 1984;63:65-81. [PubMed] |
| 11. | Sánchez R, Aparicio JR, Baeza T, Calero Y. Capsule endoscopy diagnosis of intestinal involvement in a patient with Churg-Strauss syndrome. Gastrointest Endosc. 2006;63:1082-1084. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |