Published online Apr 16, 2012. doi: 10.4253/wjge.v4.i4.148
Revised: January 10, 2012
Accepted: March 30, 2012
Published online: April 16, 2012
Endoscopic ultrasound-guided drainage has recently been recommended for increasing the drainage rate of endoscopically managed pancreatic fluid collections and decreasing the morbidity associated with conventional endoscopic trans-mural drainage. The type of stent used for endoscopic drainage is currently a major area of interest. A covered self expandable metallic stent (CSEMS) is an alternative to conventional drainage with plastic stents because it offers the option of providing a larger-diameter access fistula for drainage, and may increase the final success rate. One problem with CSEMS is dislodgement, so a metallic stent with flared or looped ends at both extremities may be the best option. An 85-year-old woman with severe co-morbidity was treated with percutaneous approach for a large (20 cm) pancreatic pseudocyst with corpuscolated material inside. This approach failed. The patient was transferred to our institute for EUS-guided transmural drainage. EUS confirmed a large, anechoic cyst with hyperechoic material inside. Because the cyst was large and contained mixed and corpusculated fluid, we used a metallic stent for drainage. To avoid migration of the stent and potential mucosal growth above the stent, a plastic prosthesis (7 cm, 10 Fr) with flaps at the tips was inserted inside the CSEMS. Two months later an esophagogastroduodenoscopy was done, and showed patency of the SEMS and plastic stents, which were then removed with a polypectomy snare. The patient experienced no further problems.
- Citation: Tarantino I, Di Pisa M, Barresi L, Curcio G, Granata A, Traina M. Covered self expandable metallic stent with flared plastic one inside for pancreatic pseudocyst avoiding stent dislodgement. World J Gastrointest Endosc 2012; 4(4): 148-150
- URL: https://www.wjgnet.com/1948-5190/full/v4/i4/148.htm
- DOI: https://dx.doi.org/10.4253/wjge.v4.i4.148
Pancreatic fluid collections (PFCs) are a complication of acute and chronic pancreatitis or pancreatic trauma. It has gradually been recognized that endoscopic treatment may be the preferred first-line approach for managing symptomatic PFCs because of a lower morbidity rate compared to surgical and percutaneous approaches[1-4]. Endoscopic ultrasound-guided drainage has recently been recommended as a way of increasing the drainage rate of endoscopically managed PFCs and of decreasing the morbidity rate with respect to conventional endoscopic trans-mural drainage[1,4,5]. The disadvantages, especially when the content of the collection is non-fluid, are: (1) the small diameter of the 10 Fr plastic stents in use, which limits the efficacy in draining; (2) the need, in some cases, to place multiple stents for drainage, which has been associated with the need for multiple revisions because of obstruction; and (3) patient discomfort and dislodgement of the catheter, often reported, when the placement of a nose-cystic catheter is required[3,4,6]. For these reasons, the type of stent used for endoscopic drainage is currently a major area of interest. A covered self expandable metallic stent (CSEMS) is an alternative to conventional drainage with plastic stents because it offers the option of providing a larger-diameter access fistula for drainage and may increase the final success rate. One problem with CSEMS is the dislodgement, so a metallic stent with flared or looped ends at both ends is perhaps the best option.
We report a case of a large, infected, pancreatic pseudocyst, which was drained in one step, under EUS guidance, with a covered metallic stent into which a plastic stent with flaps at both ends was placed to maintain the metal stent in proper place.
An 85-year-old woman was admitted to another facility because of an episode of acute pancreatitis. Her comorbidities were obesity, ischemic cardiomiopathy, chronic renal failure and diabetes. During her hospitalization, a CT scan was done, and showed, a large pseudocyst (20 cm) in the pancreatic head, with a solid component inside. Under antibiotic therapy, a percutaneous approach to the cyst was done with a temporary and partial reduction in size. She was then transferred to our institute for an attempt at EUS-guided transmural drainage. At admission, she was in poor general condition and dyspnoic because of severe pleural effusion. She was also experiencing nausea, fever, abdominal pain and vomiting. Laboratory tests (blood count, amylase and lipase levels, liver function tests) were normal. A new CT scan confirmed the presence of a large cyst (20 cm) involving the head of the pancreas, with debris inside but no signs of pancreatic necrosis. Given the mixed fluid and corpusculated content of the cyst, we planned to use a CSEMS for drainage.
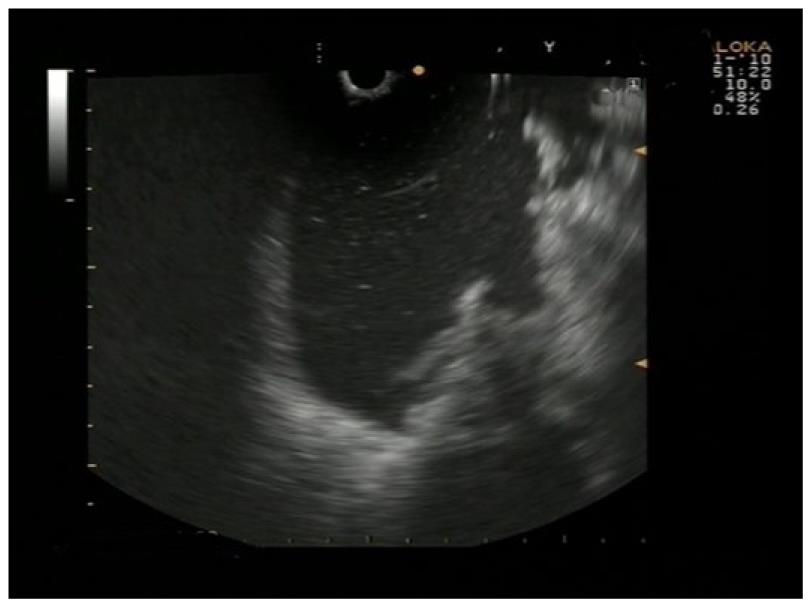
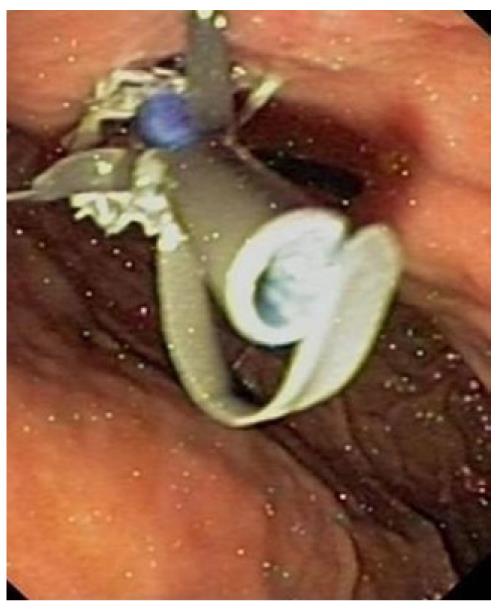
Under general anesthesia, EUS (Olympus UCT-160; Olympus Optical Corp. Ltd, Tokyo, Japan) was done, confirming a large, anechoic cyst with hyperechoic material inside (Figure 1). Transgastric puncture with a 19 Gauge needle (EUSN-19-T; Wilson Cook Medical, Inc, Winston-Salem, NC) was done under Doppler guidance. After that, a 0.035-inch wire (Jagwire, Microvasive Endoscopy, Boston Scientific Corp, Natick, Mass.) was positioned in the cystic cavity, and a pre-cut was done to create a gastro-cystic fistula. Finally, a totally covered metallic stent, 4 cm in length and 8 mm in diameter (Taewoong Medical Co., LTD, GOYANG-SI, KYUNGGI-DO) was introduced for immediate drainage of pus (Figure 2). A large amount of fluid and debris was immediately seen draining from the prosthesis into the gastric cavity. To avoid the migration of the stent and a potential mucosal growth above the stent, a plastic prosthesis (7 cm, 10 Fr) with flaps at both ends was inserted inside the CSEMS (Figure 3). Finally, given the quantity of drained fluid into the stomach, a nasogastric tube was placed to prevent vomiting.
The patient recovered from fever and abdominal pain in a few days, and at the CT, done 10 d after the procedure, total resolution of the pseudocyst was observed. Two months later, the patient was admitted to remove the stents, and an esophagogastroduodenoscopy was planned. The SEMS and the plastic stent inside were seen. They were patent and were removed with a polypectomy snare. The patient experience no further problems.
Covered SEMS have recently been adopted for the drainage of PFCs[7-10]. With respect to plastic stents, CSEMSs provide a larger diameter access fistula for drainage and may increase the final success rate and reduce the time necessary for resolution of PFC[9]. Another distinct advantage is that only one session is required to achieve drainage.
One problem with the use of CSEMS is the risk of stent migration. We believe that the placement of a plastic stent with flaps inside the CSEMS is a safe and useful method for avoiding dislodgement of the metal stent until a new, dedicated, flared CSEMS, or one with loops at both ends, becomes available.
Peer reviewers: Viktor Ernst Eysselein, MD, Professor of Medicine, Division of Gastroenterology, Harbor-UCLA Medical Center, 1000 W. Carson Street, Box 483, Torrance, CA 90509, United States; Omar Javed Shah, Professor, Department of Surgical Gastroenterology, Sher-i-Kashmir Institute of Medical Sciences, Srinagar, Kashmir 190006, India
S- Editor Yang XC L- Editor A E- Editor Yang XC
| 1. | Jacobson BC, Baron TH, Adler DG, Davila RE, Egan J, Hirota WK, Leighton JA, Qureshi W, Rajan E, Zuckerman MJ. ASGE guideline: The role of endoscopy in the diagnosis and the management of cystic lesions and inflammatory fluid collections of the pancreas. Gastrointest Endosc. 2005;61:363-370. [PubMed] |
| 2. | Habashi S, Draganov PV. Pancreatic pseudocyst. World J Gastroenterol. 2009;15:38-47. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 174] [Cited by in RCA: 188] [Article Influence: 11.8] [Reference Citation Analysis (7)] |
| 3. | Seewald S, Ang TL, Kida M, Teng KY, Soehendra N. EUS 2008 Working Group document: evaluation of EUS-guided drainage of pancreatic-fluid collections (with video). Gastrointest Endosc. 2009;69:S13-S21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 55] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 4. | Fockens P. EUS and pancreatic cyst drainage: an update. Dig Endosc. 2004;16:S201–205. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 5. | Giovannini M, Pesenti C, Rolland AL, Moutardier V, Delpero JR. Endoscopic ultrasound-guided drainage of pancreatic pseudocysts or pancreatic abscesses using a therapeutic echo endoscope. Endoscopy. 2001;33:473-477. [PubMed] |
| 6. | Chak A. Endosonographic-guided therapy of pancreatic pseudocysts. Gastrointest Endosc. 2000;52:S23-S27. [PubMed] [DOI] [Full Text] |
| 7. | Talreja JP, Shami VM, Ku J, Morris TD, Ellen K, Kahaleh M. Transenteric drainage of pancreatic-fluid collections with fully covered self-expanding metallic stents (with video). Gastrointest Endosc. 2008;68:1199-1203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 123] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 8. | Tarantino I, Barresi L, Fazio V, Di Pisa M, Traina M. EUS-guided self-expandable stent placement in 1 step: a new method to treat pancreatic abscess. Gastrointest Endosc. 2009;69:1401-1403. [PubMed] [DOI] [Full Text] |