INTRODUCTION
Colonic diverticula are a common cause of gastrointestinal bleeding. Compared to colonic diverticula, however, the prevalence of jejunoileal diverticula is quite low, and it is usually difficult to identify the source of the bleeding if the hemorrhage stems from a jejunoileal diverticulum[1]. Here, we report the case of a small bowel hemorrhage from an ileal diverticulum diagnosed by computed tomography (CT) scans. Endoscopic hemostasis was successfully carried out by colonoscopy with metal clips. The management of hemorrhaging from small intestinal diverticula is discussed.
CASE REPORT
A 59-year-old Japanese male presented to Hiroshima City Hospital with hematochezia that had begun 3 h previously. The patient had been taking medication for hyperuricemia and hypertension, but had never taken anticoagulants. He had a prior history of obscure gastrointestinal bleeding, which had occurred five years earlier. At the time, he had undergone esophagogastroduodenoscopic and colonoscopic examinations at another hospital, but the hemorrhagic source was not determined, and the bleeding stopped spontaneously. On admission to our hospital, a physical examination revealed no abnormalities. The patient’s blood pressure was 132/81 mmHg, and his pulse was 64/min. Laboratory examinations revealed slight anemia (red blood cell count, 434 × 104/mm3; hemoglobin, 13.1 mg/dl), though he had no symptoms related to anemia. Abdominal CT scans demonstrated colonic diverticula and an ileal diverticulum, and leakage of the contrast medium into the ileal lumen around the diverticulum of the terminal ileum (Figure 1). The diagnosis of a hemorrhage from an ileal diverticulum was made. Colonoscopic examination, instead of double-balloon endoscopy, was then carried out, because the bleeding point was close to the ileocecal valve. On colonoscopy, active bleeding from the diverticulum in the terminal ileum was demonstrated (Figure 2). Closure of the diverticulum was successfully performed with three metal clips, resulting in hemostasis. The patient remained well and no recurrence of gastrointestinal hemorrhaging was reported for the following nine months.
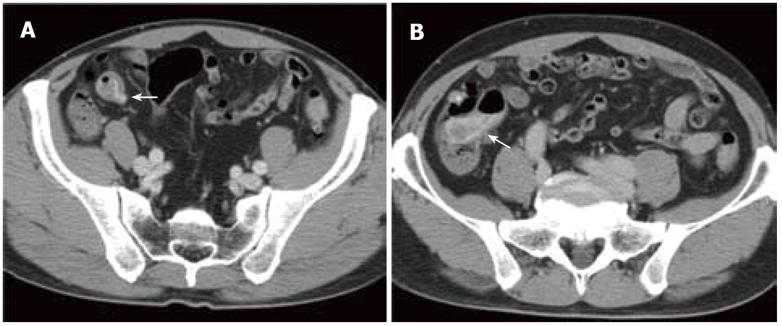
Figure 1 Contrast-enhanced computed tomography scans on admission.
A: In the arterial phase, a diverticulum of the terminal ileum was seen and leakage of the contrast medium into the ileal lumen around the diverticulum was also visualized (arrow); B: In the venous phase, the contrast medium spread to the ileocecal valve (arrow).
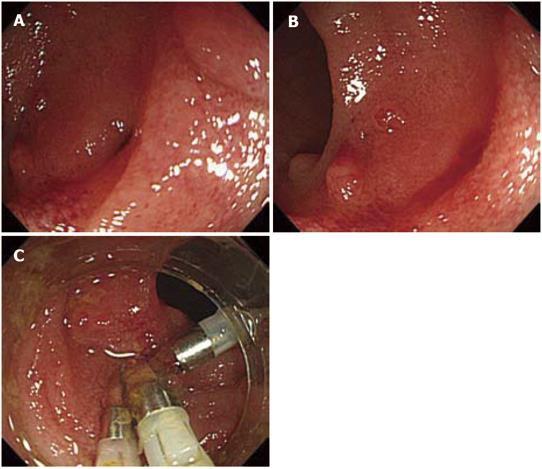
Figure 2 Colonoscopic findings.
In the terminal ileum, a diverticulum was seen (A) and active hemorrhage from the diverticulum was demonstrated (B). Closure of the diverticulum was carried out endoscopically with three metal clips (C).
DISCUSSION
Small intestinal non-Meckelian diverticuloses are identified in 2% to 2.3% of fluoroscopic X-ray studies of the small intestine[2,3]. Among small intestinal non-Meckelian diverticuloses, those located in the jejunum are considerably more frequently present than those in the ileum. Their prevalence increases with age, peaking in the sixth and seventh decades[4]. The pathogenesis of non-Meckelian jejunoileal diverticula is not yet fully known. It is commonly believed that an acquired defect of the intestinal smooth muscle or myenteric plexus causes jejunoileal diverticula[4]. In most cases, jejunoileal diverticula are asymptomatic and are discovered incidentally during autopsy, laparotomy or fluoroscopic X-ray studies. However, they can sometimes cause severe complications such as hemorraging, inflammation, perforation or intestinal obstruction, as do colonic diverticula[5-8].
CT scans, angiography, capsule endoscopy, and doubleballoon endoscopy are available to identify the source of the bleeding, such as a hemorrhage from a jejunoileal diverticulum. In contrast to colonic diverticula, non-Meckelian jejunoileal diverticula are a rare cause of gastrointestinal bleeding[9]. Due to the low incidence of the condition and the difficulty of evaluating the small bowel, a pre-operative diagnosis of bleeding from non-Meckelian jejunoileal diverticula is hard to achieve. Thus, this condition often requires laparotomy[10]; few case reports describe a successful preoperative diagnosis. Zuber-Jerger et al report a patient with hemorrhaging from jejunal diverticula that was diagnosed by capsule endoscopy and double-balloon endoscopy[10]. Jejunoileal diverticula sometimes arise in the terminal ileum, such as in our case, and in such patients, the diverticula may sometimes be found by colonoscopic examination[11,12]. Angiography[13] and CT scans[14] are also useful to specify the bleeding focus from a jejunoileal diverticulum. To the best of our knowledge, the present case is only the second report describing a hemorrhage from a jejunoileal diverticulum which was diagnosed by means of CT scans[14].
In our patient, the bleeding spot was detected in the distal ileum, approximately 5 cm from the ileocecal valve. We therefore diagnosed it as a non-Meckelian ileal diverticula rather than Meckel’s diverticulum, which is usually located within 60-100 cm of the ileocecal valve. Endoscopic hemostasis was successfully performed using metal clips, as in other reported cases[11-14]. Generally, for hemorrhaging from colonic diverticula, an injection of epinephrine, thermocoagulation or mechanical devices such as metal clips and band ligation[11] enables hemostasis[15,16]. Angiography and the following embolization are used if colonoscopic hemostasis fails, or cannot be performed[15]. This strategy could be applicable to hemorrhaging from non-Meckelian jejunoileal diverticula, even though double-balloon endoscopy must be performed for all jejunoileal diverticula except those in the terminal ileum.
In conclusion, in the present case of a hemorrhage from an ileal diverticulum, contrast CT scans visualized the diverticulum and extravasation of the contrast media, allowing accurate diagnosis. A treatment of endoscopic hemostasis with metal clips was successful.
Peer reviewers: Philip Wai Yan Chiu, Associate Professor, Department of Surgery, Institute of Digestive Disease, Chinese University of Hong Kong, Prince of Wales Hospital, 30-32 Ngan Shing Street, Shatin, Hong Kong, China; Carlo M Girelli, MD, 1st Department of Internal Medicine, Service of Gastroenterology and Digestive Endoscopy, Hospital of Busto Arsizio, Via Arnaldo da Brescia, 121052 Busto Arsizio (VA), Italy; Kenneth Kak Yuen Wong, MD, PhD, Assistant Professor, Department of Surgery, The University of Hong Kong, Queen Mary Hospital, Pokfulam Road, Hong Kong, China
S- Editor Zhang HN L- Editor Herholdt A E- Editor Zhang L