Published online Jul 16, 2011. doi: 10.4253/wjge.v3.i7.151
Revised: June 27, 2011
Accepted: July 5, 2011
Published online: July 16, 2011
A 78-year-old woman was referred to our department for treatment of an early gastric cancer. Esophagogastroduodenoscopy (EGD) demonstrated a flat elevated lesion and a polypoid lesion on the greater curvature of the antrum. Histological analysis of, endoscopic biopsy samples taken from these lesions revealed an adenocarcinoma and a hyperplastic polyp, respectively. ESD was conducted for removal of the lesions. Carbon dioxide (CO2) instead of room air was used for insufflation, and the patient was adequately sedated without struggling or vomiting during the treatment. No significant bleeding from the lesion was observed during ESD, but fresh blood was identified endoscopically. Surprisingly, a Mallory-Weiss tear with active bleeding was detected on the lesser curvature of the gastric corpus. A total of eight hemoclips were applied for hemostasis. Both lesions were completely removed en bloc, and no bleeding or perforation developed after ESD. Histologically, the first lesion was a papillary carcinoma limited to the mucosal layer and without lymphovascular invasion or involvement of the surgical margins, while the second lesion was a benign hyperplastic polyp.
- Citation: Hongou H, Fu K, Ueyama H, Takahashi T, Takeda T, Miyazaki A, Watanabe S. Mallory-Weiss tear during gastric endoscopic submucosal dissection. World J Gastrointest Endosc 2011; 3(7): 151-153
- URL: https://www.wjgnet.com/1948-5190/full/v3/i7/151.htm
- DOI: https://dx.doi.org/10.4253/wjge.v3.i7.151
Endoscopic submucosal dissection (ESD) has gained acceptance for the treatment of early gastric cancers without lymph node metastasis, as this technique enables en bloc resection of lesions regardless of their size[1]. Complications associated with ESD include bleeding, perforation and stenosis. Perhaps the most frequently encountered complication is immediate bleeding from vessels in the submucosal layer of the lesions during ESD. This can be managed with coagulation using an electrocautery knife and/or electrocautery forceps[2]. We herein report on a patient who developed Mallory-Weiss tears (MWT), an extremely rare source of active bleeding associated with gastric ESD.
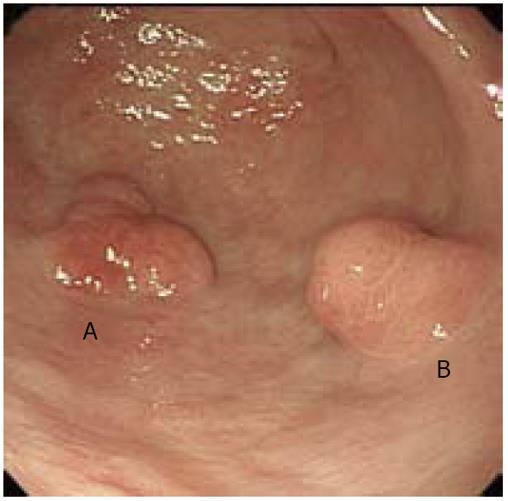
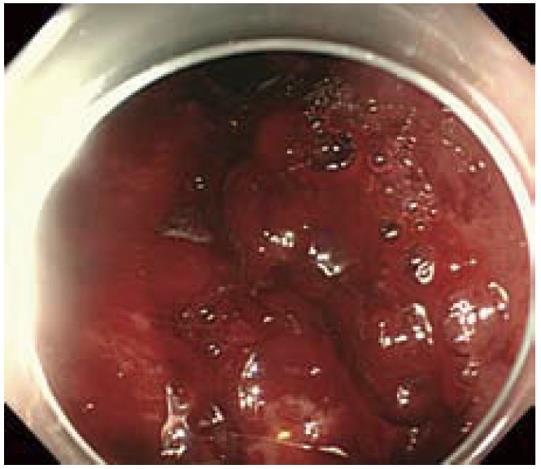
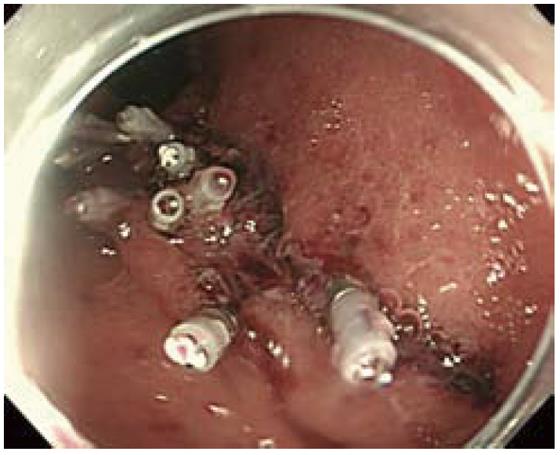
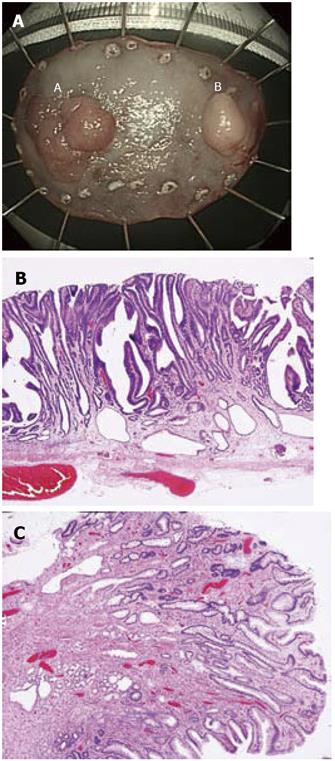
A 78-year-old woman was referred to our department for treatment of an early gastric cancer. She was asymptomatic and received the esophagogastroduodenoscopy at a local hospital during a medical checkup. Her medical history included hypertension and hyperlipidemia, for which she was receiving medication. No anticoagulant which might contribute to a bleeding tendency was prescribed for this patient. On July 22, 2010, esophagogastroduodenoscopy (EGD) demonstrated mild hiatal hernia and gastric atrophy. Furthermore, a flat elevated lesion about 20 mm in size, and a polypoid lesion about 15 mm in size were detected on the greater curvature of the antrum (Figure 1). Histological analysis of endoscopic biopsy samples taken from these lesions revealed adenocarcinoma and hyperplastic polyp, respectively. No lymph node swelling was detected by abdominal computed tomography conducted before endoscopic treatment. On August 11, 2010, ESD was carried out for removal of the lesions. Carbon dioxide (CO2) instead of room air was used for insufflation, and the patient was adequately sedated with intravenous administration of midazolam (5 mg) and pentazocine (15 mg) without struggling or vomiting during the treatment. CO2 insufflation was set at a constant rate of 1.2 L/min, which is a moderate level in the CO2 regulator (UCR, Olympus Tokyo). Although significant bleeding from the lesion was not observed during ESD, fresh blood was identified at endoscopy. After retroflexion of the scope tip, longitudinal mucosal tears (MWT) (maximal length; about 50 mm in length) with active bleeding were detected on the lesser curvature of the gastric corpus (Figure 2). A total of eight hemoclips were applied for hemostasis (Figure 3). Both of the lesions were completely removed en bloc within an hour, and no bleeding or perforation developed after ESD. The patient was discharged uneventfully after staying in the hospital for one week. Histologically, the first lesion was a papillary carcinoma limited to the mucosal layer and without lymphovascular invasion or involvement of the surgical margins, while the second lesion was a benign hyperplastic polyp (Figure 4).
MWT which is characterized by longitudinal mucosal lacerations in the distal esophagus and proximal stomach, was first described in 1929 as a syndrome of upper gastrointestinal bleeding (UGIB) caused by nausea and vomiting[3]. The reported incidence of MWT is 5%-15% of all cases of UGIB, although MWT may also occur iatrogenically during endoscopic examination, and its incidence has been estimated to be 0.007%-0.49% of all such procedures[4,5]. MWT usually occurs secondarily to a sudden increase in intra-abdominal pressure, and several predisposing factors including hiatal hernia, alcoholism, gastric atrophy and ageing have been suggested[6]. We used CO2 for insufflation during ESD, as it is absorbed faster in the body than air and then rapidly expelled through respiration[7]. On the basis of a retrospective review of the video of the procedure in this case, we suspected that the upper esophageal sphincter did not relax during ESD under sedation. This resulted in a high intra-gastric pressure which caused laceration of the vulnerable atrophic gastric mucosa in this elderly woman, even though CO2 was used instead of room air for insufflation. Adjustment of the intra-gastric pressure with suction and insufflation during ESD may have made it possible to avoid MWT in this case.
Most patients with iatrogenic MWT can be treated conservatively, with or without endoscopic hemostasis, using techniques including injection, electrocautery and mechanical therapies. Although serious complications such as massive bleeding and perforation are rarely encountered, they are possible[8]. In order to avoid deeper tissue damage which could result in perforation, possibly after a delay, we applied hemoclips instead of thermal or injection therapies to arrest any active bleeding[5].
In conclusion, we have reported the first case of MWT which is a rarely encountered but possible complication of gastric ESD. Iatrogenic MWT should be kept in mind as another possible source of bleeding during gastric ESD, even if CO2 instead of room air is used for insufflation. Adjustment of the intra-gastric pressure during ESD may be necessary to avoid this kind of complication.
Peer reviewers: Jaekyu Sung, MD, PhD, Assistant Professor, Division of Gastroenterology, Department of Internal Medicine, Chungnam National University Hospital, 33 Munhwa-ro, Jung-gu, Daejeon 301-721, South Korea; Naoto Sakamoto, Associate Professor, Department of Gastroenterology, Juntendo University, 2-1-1 Hongo Bunkyo-ku Tokyo, 113-8421, Japan; Dae Kyung Sohn, MD, Center for Colorectal Cancer, Research Institute and Hospital, National Cancer Center, 809 Madu 1-dong, Ilsandong-gu, Goyang, Gyeonggi 411-769, South Korea
S-Editor Wang JL L-Editor Hughes D E-Editor Zhang L
| 1. | Oda I, Saito D, Tada M, Iishi H, Tanabe S, Oyama T, Doi T, Otani Y, Fujisaki J, Ajioka Y. A multicenter retrospective study of endoscopic resection for early gastric cancer. Gastric Cancer. 2006;9:262-270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 291] [Cited by in RCA: 314] [Article Influence: 17.4] [Reference Citation Analysis (0)] |
| 2. | Takizawa K, Oda I, Gotoda T, Yokoi C, Matsuda T, Saito Y, Saito D, Ono H. Routine coagulation of visible vessels may prevent delayed bleeding after endoscopic submucosal dissection--an analysis of risk factors. Endoscopy. 2008;40:179-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 235] [Cited by in RCA: 271] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 3. | DECKER JP, ZAMCHECK N, MALLORY GK. Mallory-Weiss syndrome: hemorrhage from gastroesophageal lacerations at the cardiac orifice of the stomach. N Engl J Med. 1953;249:957-963. [PubMed] |
| 4. | Adler DG, Leighton JA, Davila RE, Hirota WK, Jacobson BC, Qureshi WA, Rajan E, Zuckerman MJ, Fanelli RD, Hambrick RD. ASGE guideline: The role of endoscopy in acute non-variceal upper-GI hemorrhage. Gastrointest Endosc. 2004;60:497-504. [PubMed] |
| 5. | Shimoda R, Iwakiri R, Sakata H, Ogata S, Ootani H, Sakata Y, Fujise T, Yamaguchi K, Mannen K, Arima S. Endoscopic hemostasis with metallic hemoclips for iatrogenic Mallory-Weiss tear caused by endoscopic examination. Dig Endosc. 2009;21:20-23. [PubMed] |
| 6. | Penston JG, Boyd EJ, Wormsley KG. Mallory-Weiss tears occurring during endoscopy: a report of seven cases. Endoscopy. 1992;24:262-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 34] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Nonaka S, Saito Y, Takisawa H, Kim Y, Kikuchi T, Oda I. Safety of carbon dioxide insufflation for upper gastrointestinal tract endoscopic treatment of patients under deep sedation. Surg Endosc. 2010;24:1638-1645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 55] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 8. | O’Kelly F, Lim KT, Cooke F, Ravi N, Reynolds JV. An unusual presentation of Boerhaave Syndrome: a case report. Cases J. 2009;2:8000. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |