Published online Mar 16, 2011. doi: 10.4253/wjge.v3.i3.64
Revised: December 17, 2010
Accepted: December 24, 2010
Published online: March 16, 2011
The covered self-expandable metallic stent (SEMS) has been developed to overcome the problem of tissue ingrowth, However, stent migration is a well-known complication of covered SEMS placement. Use of a double pigtail stent to lock the movement of the SEMS and prevent migration has been advised by many experts. Unfortunately, in our case this technique led to an incidental upward migration of the SEMS. We used APC to create a side hole in the SEMS for plastic stent insertion as stent-in-stent. This led to a successful prevention of stent migration.
- Citation: Ridtitid W, Rerknimitr R, Amornsawadwattana S, Ponauthai Y, Kullavanijaya P. Stent-in-stent through a side hole to prevent biliary metallicstent migration. World J Gastrointest Endosc 2011; 3(3): 64-66
- URL: https://www.wjgnet.com/1948-5190/full/v3/i3/64.htm
- DOI: https://dx.doi.org/10.4253/wjge.v3.i3.64
Self-expandable metallic stent (SEMS) placement is widely accepted for palliative management of patients with unresectable malignant biliary obstruction. However, complications such as tumor ingrowth, overgrowth, food debris, and mucosal hyperplasia can occur. The use of covered SEMS is clearly effective in preventing tumor ingrowth[1-3]. Nevertheless, in two recently published randomized trials of covered versus uncovered metal biliary stents, outcomes such as stent patency were no different between the two stents but the risk of migration was higher with the covered stents[4,5]. Here, we report a case of stent-in-stent insertion through a side hole to prevent migration of a covered self-expandable metallic stent in a patient with distal malignant biliary obstruction.
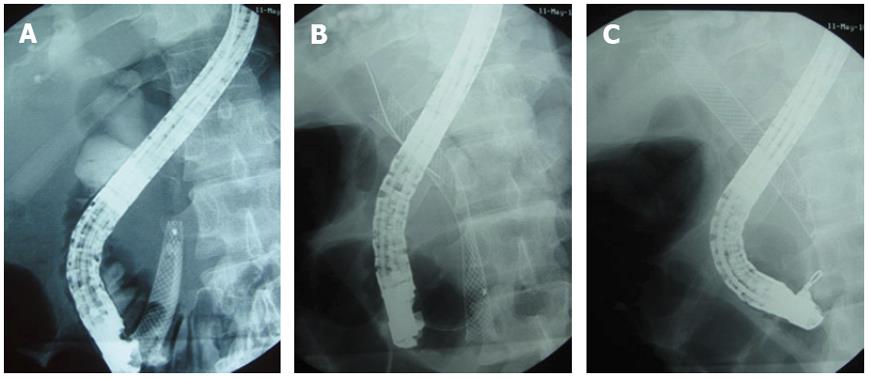
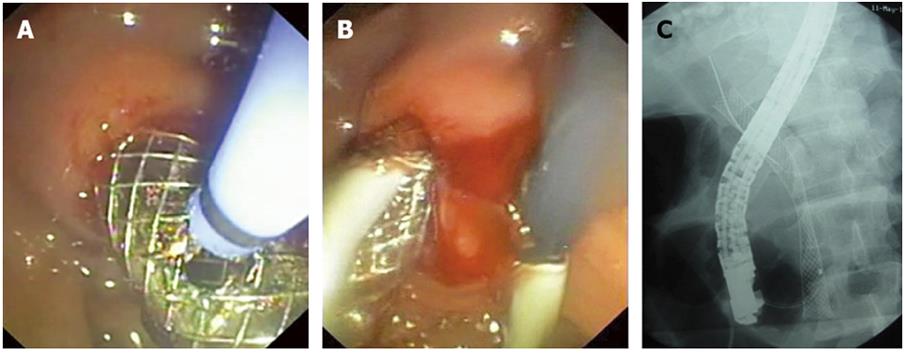
A 35-year-old man presented with obstructive jaundice resulting from metastatic pancreatic cancer. The diagnosis was confirmed by intraductal biopsy. Endoscopic retrograde cholangiopancreatography (ERCP) demonstrated a distal biliary stricture 1.5 cm in length with upstream dilatation. Placement of a 4-cm-long covered SEMS (Wallstent, Boston Scientific, Natick, MA) under conscious sedation was initially performed. Three weeks later, the patient was re-admitted due to acute cholangitis. ERCP demonstrated distal migration of the SEMS (Figure 1A). Successful removal of the first SEMS was performed using a snare and this was replaced with a new SEMS (Wallstent, Boston Scientific, Natick, MA), 8 cm in length (Figure 1B). Subsequently, placement of a double pigtail 10 Fr 10 cm plastic stent (PS) was attempted as stent-in-stent to prevent migration. However, even with cautious deployment the SEMS was accidentally displaced upwards during PS insertion. Using a rat-toothed forceps we were able to move the stent downwards to the proper position (Figure 1C). Argon plasma coagulation (APC) was then applied to create a side hole at the distal end of the SEMS (Figure 2A) and a PS was inserted through the side hole (Figure 2B). This side hole insertion was helpful in preventing the upward movement of the previously deployed SEMS (Figure 2C). Six months later the patient was doing well and was without clinical sign of biliary obstruction.
Covered SEMS placement is widely accepted for use in palliative management of patients with unresectable malignant distal biliary obstruction. Although covered stents are designed to overcome tissue ingrowth, failure to embed in the bile duct wall can result in proximal and distal migration, at a reported frequency of 6%-8%[1-5]. Migration of a biliary SEMS may occur proximally or distally after stent insertion and may cause complications such as ulceration, perforation and intestinal obstruction[1-3].
Generally, correct positioning of the SEMS at the initial stent placement is important in preventing migration. Nevertheless, a high shortening ratio of the covered SEMS is thought to favour migration after deployment of the stent[6]. New covered stents, therefore, have been developed for the prevention of stent migration. These include the nitinol SEMS (Wallflex; Boston Scientific, Natick, Massachusetts, USA or Niti-S; Taewoong Medical, Seoul, South Korea) which is flared at the uncovered ends and the fully-coverd Zeostent (Zeon Medical Inc., Tokyo, Japan) which has a wavy contour after full expansion[6,7]. Some previous work of expert endoscopists suggested that putting a double pigtail stent as stent-in-stent to lock the movement of the SEMS could prevent migration[8]. However, this technique for preventing biliary stent migration has not been well established. We have reported a case with malignant distal biliary obstruction after covered SEMS placement. In our case, the insertion of a double pigtail stent was perform to lock the movement of the SEMS and thereby prevent its migration. However, due to upward force exerted during PS insertion as stent-in-stent, this technique led to an incidental upward migration of the covered SEMS.
Argon plasma (APC) has been described as a useful tool for trimming the stent or making a hole[9-12]. Studies done on Wallstent, have recommended a power setting of 70-80 W and argon flow of 0.8 L/min. In this case, we used APC to make a side hole in the SEMS for PS insertion without complication. After the force angle of PS insertion was changed, the distal end of double pigtail stent was able to lock the distal end of the SEMS and to prevent upward migration of SEMS during PS placement.
In conclusion, we report a successful technique of stent-in-stent insertion through the side hole to change an angle of PS insertion for preventing upward covered SEMS migration in a patient with distal malignant biliary obstruction. With this tangential stent insertion, the chance of upward stent migration during deployment should be less.
Peer reviewers: Tony Chiew Keong Tham, MD, Consultant Gastroenterologist, Ulster Hospital, Dundonald, Belfast BT16 1RH, Northern Ireland, United Kingdom; Iruru Maetani, MD, Professor and Chairman, Division of Gastroenterology, Department of Internal Medicine, Toho University Ohashi Medical Center, 2-17-6 Ohashi Meguro-ku, Tokyo 153-8515, Japan
S- Editor Zhang HN L- Editor Hughes D E- Editor Liu N
| 1. | Isayama H, Nakai Y, Togawa O, Kogure H, Ito Y, Sasaki T, Sasahira N, Hirano K, Tsujino T, Tada M. Covered metallic stents in the management of malignant and benign pancreatobiliary strictures. J Hepatobiliary Pancreat Surg. 2009;16:624-627. |
| 2. | Nakai Y, Isayama H, Komatsu Y, Tsujino T, Toda N, Sasahira N, Yamamoto N, Hirano K, Tada M, Yoshida H. Efficacy and safety of the covered Wallstent in patients with distal malignant biliary obstruction. Gastrointest Endosc. 2005;62:742-748. |
| 3. | Leung J, Rahim N. The role of covered self-expandable metallic stents in malignant biliary strictures. Gastrointest Endosc. 2006;63:1001-1003. |
| 4. | Telford JJ, Carr-Locke DL, Baron TH, Poneros JM, Bounds BC, Kelsey PB, Schapiro RH, Huang CS, Lichtenstein DR, Jacobson BC. A randomized trial comparing uncovered and partially covered self-expandable metal stents in the palliation of distal malignant biliary obstruction. Gastrointest Endosc. 2010;72:907-914. |
| 5. | Kullman E, Frozanpor F, Söderlund C, Linder S, Sandström P, Lindhoff-Larsson A, Toth E, Lindell G, Jonas E, Freedman J. Covered versus uncovered self-expandable nitinol stents in the palliative treatment of malignant distal biliary obstruction: results from a randomized, multicenter study. Gastrointest Endosc. 2010;72:915-923. |
| 6. | Ito K, Fujita N, Noda Y, Kobayashi G, Obana T, Horaguchi J, Koshita S, Kanno Y, Ogawa T, Kato Y. Newly developed fully covered metal stent for unresectable malignant biliary stricture. Diagn Ther Endosc. 2010;2010:903520. |
| 7. | Raijman I. Biliary and pancreatic stents. Gastrointest Endosc Clin N Am. 2003;13:561-592, vii-viii. |
| 8. | Talreja JP, Shami VM, Ku J, Morris TD, Ellen K, Kahaleh M. Transenteric drainage of pancreatic-fluid collections with fully covered self-expanding metallic stents (with video). Gastrointest Endosc. 2008;68:1199-1203. |
| 9. | Rerknimitr R, Naprasert P, Kongkam P, Kullavanijaya P. Trimming a metallic biliary stent using an argon plasma coagulator. Cardiovasc Intervent Radiol. 2007;30:534-536. |
| 10. | Christiaens P, Decock S, Buchel O, Bulté K, Moons V, D’Haens G, Van Olmen G. Endoscopic trimming of metallic stents with the use of argon plasma. Gastrointest Endosc. 2008;67:369-371. |
| 11. | Vanbiervliet G, Piche T, Caroli-Bosc FX, Dumas R, Peten EP, Huet PM, Tran A, Demarquay JF. Endoscopic argon plasma trimming of biliary and gastrointestinal metallic stents. Endoscopy. 2005;37:434-438. |
| 12. | Matsubayashi H, Hasuike N, Tanaka M, Takizawa K, Yamaguchi Y, Ono H. Trimming of a migrated nitinol stent using argon plasma. Case Rep Gastroenterol. 2009;3:202-206. |