Published online Sep 16, 2010. doi: 10.4253/wjge.v2.i9.318
Revised: July 2, 2010
Accepted: July 9, 2010
Published online: September 16, 2010
Duodenal duplication cysts are rare congenital abnormalities which are more commonly diagnosed in infancy and childhood. However, in rare cases, these lesions can remain asymptomatic until adulthood. The combination of duplication cyst and pancreas divisum is extremely rare and both conditions have been linked with acute recurrent pancreatitis. We present the case of a 37 years-old patient who presented with repeated episodes of acute pancreatitis. By means of magnetic resonance imaging and endoscopic ultrasonography we discovered a duplication cyst whose cavity received drainage from the dorsal pancreas. After opening the cyst cavity to the duodenal lumen with a needle knife the patient presented no further episodes in the clinical follow-up. Comparable literature findings and therapeutic options for these abnormalities are discussed with regard to the presented case.
- Citation: Redondo-Cerezo E, Pleguezuelo-Díaz J, Hierro ML, Macias-Sánchez JF, Ubiña CV, Martín-Rodríguez MDM, Teresa-Galván JD. Duodenal duplication cyst and pancreas divisum causing acute pancreatitis in an adult male. World J Gastrointest Endosc 2010; 2(9): 318-320
- URL: https://www.wjgnet.com/1948-5190/full/v2/i9/318.htm
- DOI: https://dx.doi.org/10.4253/wjge.v2.i9.318
Recurrent idiopathic pancreatitis is defined as repeated episodes of pancreatitis in a patient in which the cause has not been identified by the usual diagnostic workup. Nevertheless, after a single episode of acute pancreatitis of unexplained origin, a repeated attack is unlikely[1]. However, a variety of additional investigations have been advocated before considering the pancreatitis as idiopathic, and they offer the possibility of finding a probable cause in the vast majority of these patients[2]. Duodenal duplication cysts are rare congenital abnormalities which are more commonly diagnosed in infancy and childhood. However, in exceptional cases, the lesion can remain asymptomatic until adulthood[3]. We present a singular case of the coincident occurrence of a duplication cyst with pancreas divisum, and drainage of the dorsal pancreas inside the cyst, causing recurrent acute pancreatitis in a 37 years-old male. There are a few similar cases in the previous literature but none with the features we found, and with such a simple and successful endoscopic treatment.
A 37 year-old male with a previous history recurrent acute pancreatitis came to the emergency room because of a new episode of acute pancreatitis. He had presented with attacks of abdominal pain attributable to pancreatitis and biliary colic in the previous three years, with repeated admission to the ER. He did not drink or smoke and had no medical intolerances. No previous surgeries were reported. He had undergone multiple abdominal ultrasound procedures with no significant findings. Abdominal exam showed a mild tenderness in epigastrium with neither masses nor peritoneal signs. Laboratory analysis revealed elevated amylase levels (861 U/L) with no other abnormalities.
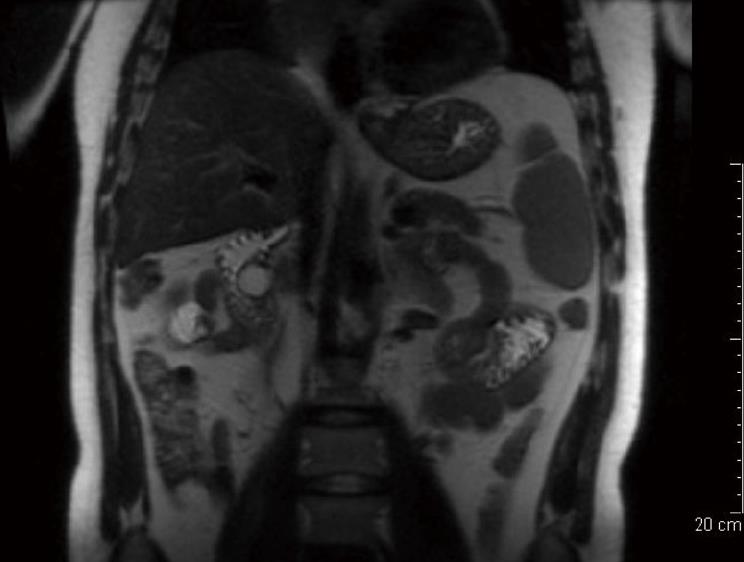
Abdominal ultrasonography was once again normal. An magnetic resonance imaging (MRI) (Figure 1) indicated a normal gallbladder with a cystic dilatation at the distal, periampullary common bile duct, protruding in the duodenal lumen, that was considered by the radiologist to be a choledococele or Todany’s type III choledocal cyst.
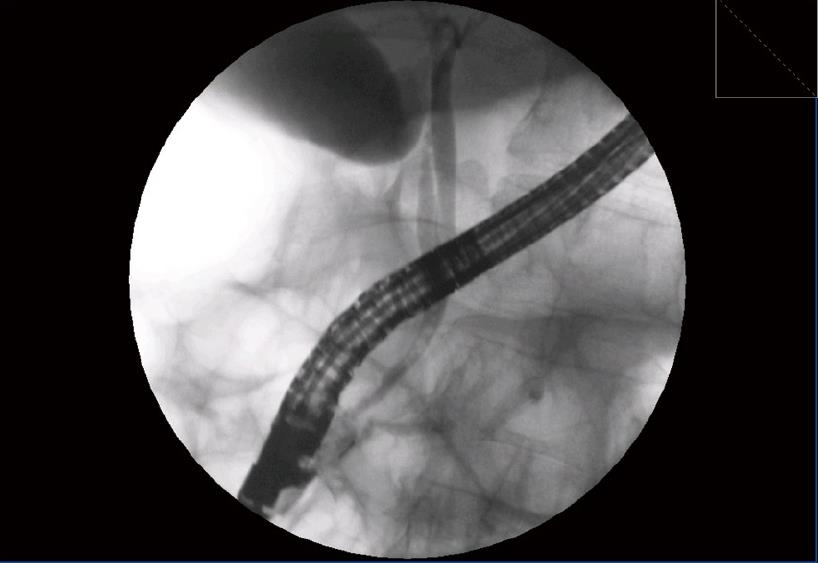
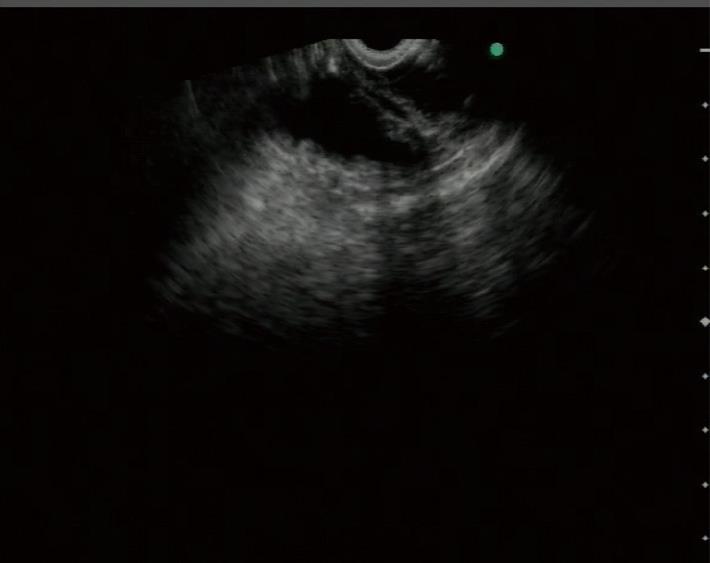
The patient was sent to the endoscopy unit for an ERCP under general anesthesia. From the second duodenal portion a protruding duodenal mass, with normal overlying mucosa, was seen cranial and slightly lateral to the choledocal fold. Cholangiography was normal, but pancreatography showed a blockage in the first third of the pancreatic duct highly suggestive of pancreas divisum (Figure 2). Minor papilla could not be found even after careful examination. Taking into account these findings, a linear endoscopic ultrasound (EUS) probe was inserted. The procedure revealed a cystic cavity, with a small amount of debris inside, and a wall in which three layers could be identified (Figure 3). With the endosonographic diagnosis of duplication cyst and the absence of an evident minor papilla we inserted a needle knife inside the cyst, injecting contrast medium into the cystic cavity, which showed no communication with the duodenal lumen (Figure 4). We then opened the cyst into the duodenal lumen with the same needle knife, achieving a complete drainage of its content.
A repeat radial EUS, one month later, failed to find the cyst, indicating that it was completely drained. A repeat MRI confirmed the presence of a pancreas divisum, after consultation with the radiologist.
The patient is now doing well, with no recurrent episodes of acute pancreatitis, three months after the procedure.
Duplication cysts are benign, rare anomalies that arise during early embryonic development[4]. Usually, these cysts present in childhood with obstructive or bleeding symptoms. Clinical findings of this entity may be non-specific, such as mild abdominal pain, or more specific, such as acute or chronic pancreatitis. A variety of possible mechanisms might be responsible for pancreatitis: a transitory and mobility-related duodenal obstruction of the major papilla outflow by the cyst; the migration of biliary sludge and/or microstones from the cyst to the biliary tree, as observed in biliary pancreatitis; the communication of the dorsal pancreatic duct with the cystic cavity[5-6]. Diagnosis can be made without ERCP in most cases, given the increased availability of MRCP and EUS[7].
These cysts are lined with stratified, ciliated, or columnar epithelium and contain a mucoid fluid[8,9]. They are typically discovered incidentally on endoscopy or radiologic imaging since they only rarely cause symptoms. Complications are rare but may include pancreatitis when cycts are located near the ampulla of Vater[8]. While they are believed to have a low malignant potential, case reports have described malignant transformation[10]. The endoscopic exam may reveal a bulge with normal overlying mucosa, or a diverticulum. Cycts have a regular appearance without mucosal irregularities. On EUS, duplication cysts are usually anechoic homogeneous lesions with regular margins arising from the submucosa (third layer) or extrinsic to the gastrointestinal wall. Their wall can be characterized by three- to five-layer structures. They may contain septae, fluid, or echogenic material consisting of layering debris or mucin. EUS is helpful in discriminating a duplication cyst from a solid mass. The diagnosis can usually be made by the characteristic endoscopic and endosonographic appearance. Management of asymptomatic cysts is usually expectant. Nevertheless, prospective studies evaluating the natural history of duplication cysts are lacking. When symptomatic, duplication cysts can be treated surgically or endoscopically[7,11]. Although therapy has classically involved surgical resection, different endoscopic methods, such as resection of the cystic roof by using a standard polypectomy snare, or a large incision of the roof, are probably sufficient to cure the patient. Additional sphincterotomy is not necessary, because the sphincter area is intact in cases of duodenal duplication, in contrast to what happens with choledococele, in which biliary sphincterotomy is the treatment of choice[12]. Concerns may arise around the potential of malignant transformation of duplication cysts but, although endoscopic therapy does not achieve a complete mucosal resection, it avoids stasis of secretions inside the cyst with a potential protective effect[7,10,12]. Indeed, some authors recommend an endoscopic review of the area with follow up biopsies, after endoscopic therapy[7].
In summary, we present an extraordinarily infrequent case of recurrent pancreatitis caused by a duplication cyst connected with the minor papilla in a patient with pancreas divisum.
Peer reviewer: Everson Luiz de Almeida Artifon, MD, PhD, FASGE, University of Sao Paulo School of Medicine, Rua Guimaraes Passos, Sao Paulo 04107030, Brazil
S- Editor Zhang HN L- Editor Hughes D E- Editor Liu N
| 1. | Ballinger AB, Barnes E, Alstead EM, Fairclough PD. Is intervention necessary after first episode of idiopathic acute pancreatitis. Gut. 1996;38:293-295. |
| 2. | Kaw M, Brodmerkel GJ Jr. ERCP, biliary crystal analysis, and sphincter of Oddi manometry in idiopathic recurrent pancreatitis. Gastrointest Endosc. 2002;55:157-162. |
| 3. | Arulprakash S, Balamurali R, Pugazhendhi T, Kumar SJ. Pancreas divisum and choledochal cyst. Indian J Med Sci. 2009;63:198-201. |
| 4. | Rizzo RJ, Szucs RA, Turner MA. Congenital abnormalities of the pancreas and biliary tree in adults. Radiographics. 1995;15:49-68; quiz 147-148. |
| 5. | Hwang JH, Saunders MD, Rulyak SJ, Shaw S, Nietsch H, Kimmey MB. A prospective study comparing endoscopy and EUS in the evaluation of GI subepithelial masses. Gastrointest Endosc. 2005;62:202-208. |
| 6. | Carbognin G, Guarise A, Biasiutti C, Pagnotta N, Procacci C. Duodenal duplication cyst identified with MRCP. Eur Radiol. 2000;10:1277-1279. |
| 7. | Antaki F, Tringali A, Deprez P, Kwan V, Costamagna G, Le Moine O, Delhaye M, Cremer M, Devière J. A case series of symptomatic intraluminal duodenal duplication cysts: presentation, endoscopic therapy, and long-term outcome (with video). Gastrointest Endosc. 2008;67:163-168. |
| 8. | Woolfolk GM, McClave SA, Jones WF, Oukrop RB, Mark MD. Use of endoscopic ultrasound to guide the diagnosis and endoscopic management of a large gastric duplication cyst. Gastrointest Endosc. 1998;47:76-79. |
| 9. | Faigel DO, Burke A, Ginsberg GG, Stotland BR, Kadish SL, Kochman ML. The role of endoscopic ultrasound in the evaluation and management of foregut duplications. Gastrointest Endosc. 1997;45:99-103. |
| 10. | Coit DG, Mies C. Adenocarcinoma arising within a gastric duplication cyst. J Surg Oncol. 1992;50:274-277. |
| 11. | Banner K, Helft S, Kadam J, Miah A, Kaushik N. An unusual cause of dysphagia in a young woman: esophageal duplication cyst. Gastrointest Endosc. 2008;68:793-795. |
| 12. | Inoue M, Nishimura O, Andachi H, Koga S. Early cancer of duodenal duplication. A case report. Gastroenterol Jpn. 1979;14:233-237. |