Published online Mar 16, 2010. doi: 10.4253/wjge.v2.i3.104
Revised: January 22, 2010
Accepted: January 29, 2010
Published online: March 16, 2010
Heterotopic bone formation (osseous metaplasia) is rarely detected in the gastrointestinal tract. Most of reported cases are associated with malignant lesions. We herein report a case of osseous metaplasia in a rectal inflammatory polyp and a review of the literature on suggested mechanisms for its aetiology. A 39-year-old man visited our hospital with a chief complaint of melena. Total colonoscopy revealed a slightly reddish subpedunculated polyp, about 12 mm in diameter, in the lower rectum. Endoscopic resection was performed. Histologically, several foci of heterotopic bone formation were found. From the review of the literature, all of the polyps described were larger than 10mm in diameter, 55.6% showed inflammatory changes, and 62.5% were detected in the rectum. Osteogenic stimulation was considered to be a result of the inflammatory process. As our inflammatory polyp was located in the rectum, the pathogenesis could be a reactive change stimulated by the repeated local trauma, or be on a peculiar characteristic of the rectal mucosa itself.
- Citation: Oono Y, Fu KL, Nakamura H, Iriguchi Y, Oda J, Mizutani M, Yamamura A, Kishi D. Bone formation in a rectal inflammatory polyp. World J Gastrointest Endosc 2010; 2(3): 104-106
- URL: https://www.wjgnet.com/1948-5190/full/v2/i3/104.htm
- DOI: https://dx.doi.org/10.4253/wjge.v2.i3.104
Heterotopic bone formation (osseous metaplasia) is rarely detected in the gastrointestinal tract. Most of reported cases are associated with malignant lesions[1,2]. We herein report a case of osseous metaplasia in a rectal inflammatory polyp and review the literature on suggested mechanisms for its aetiology.
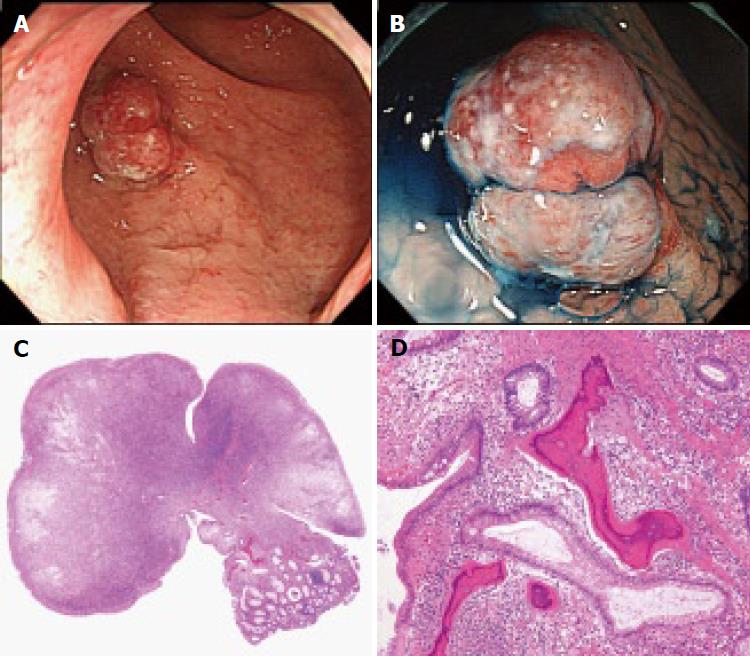
A 39-year-old man visited our hospital with a chief complaint of melena. Total colonoscopy was carried out on the cecum uneventfully, and nothing but a slightly reddish subpedunculated polyp (Paris classification Isp), about 12 mm in diameter, was detected in the lower rectum (Figure 1A). The surface of the polyp was covered with whitish exudate, which suggested inflammatory change. Magnifying observation with dye-spraying using 0.4% indigo carmine revealed a type Ipit pattern according to the Kudo’s classification, which indicated that this polyp was non-neoplastic (Figure 1B). Therefore, an endoscopic diagnosis of an inflammatory polyp was established. However, endoscopic resection was performed for histological evaluation, as the polyp was larger than 10 mm. The polyp was completely removed en bloc with EMR (the lift and cut technique) without complication. Histologically, the surface of the resected specimen was mostly covered by inflammatory exudate and partly by regenerating epithelium (Figure 1C). Moreover, the polyp was composed of inflammatory granulation tissues with numerous capillaries and marked acute and chronic inflammatory cells infiltration. Several foci of heterotopic bone formation were also found on histology (Figure 1D). A pathological diagnosis of a rectal inflammatory polyp with osseous metaplasia was finally made.
Stromal ossification often occurs in gastrointestinal cancers from the stomach to the rectum and appears to result from tumor production of bone morphogenic protein[2]. Heterotopic ossification in benign colon polyps has, however, been documented only rarely. To the best of our knowledge, there are only nine cases other than ours which have been reported[3-10]. We have reviewed and summarized the related literature on osseous metaplasia in benign colon polyps (Table 1). The patients comprised 4 men and 4 women, plus two who gender was not described, with a mean age of 47 yr (range: 3 to 85 y). All of the polyps were larger than 10mm in diameter, and the mean size was 16.3 mm (range: 10-25 mm). Histologically, 6 lesions were neoplastic (3 tubular adenomas and 3 tubulovillous adenomas), whilst the remaining 4 lesions were non-neoplastic (3 inflammatory polyps and a juvenile polyp). In addition, 5 out of 9 lesions (55.6%) showed inflammatory changes, and 2 out of 9 lesions (22.2%) demonstrated mucindeposition, whilst information was lacking for one case. The most commonly involved site was rectum where 5 out of 8 polyps (62.5%) were detected.
| Case | Author | Year | Age | Gender | Size (mm) | Location | Histology | Inflammation | Mucin deposition | Ref. |
| 1 | Sperling | 1981 | 25 | M | 10 | Rectum | Inflammatory polyp | + | + | [3] |
| 2 | Castelli | 1992 | 22 | F | 10 | Rectum | Inflammatory polyp | + | - | [4] |
| 3 | Groisman | 1994 | 67 | M | 18 | Rectum | Tubulovillous adenoma | - | - | [5] |
| 4 | Groisman | 1994 | 3 | F | 20 | Rectum | Juvenile polyp | + | + | [5] |
| 5 | Cavazza | 1996 | NI | NI | NI | NI | Tubulovillous adenoma | NI | NI | [6] |
| 6 | McPherson | 1999 | 73 | M | 20 | Cecum | Tubulovillous adenoma | - | - | [7] |
| 7 | Rothstein | 2000 | NI | NI | 25 | Sigmoid colon | Tubular adenoma | - | - | [8] |
| 8 | AI-daraji | 2005 | 85 | F | 15 | Sigmoid colon | Tubular adenoma | - | - | [9] |
| 9 | White | 2008 | 63 | F | NI | Transverse colon | Tubular adenoma | + | - | [10] |
| 10 | Present case | 2009 | 39 | M | 12 | Rectum | Inflammatory polyp | + | - | Present case |
Histologically, necrosis, inflammation, pre-existing calcification, increased vascularity, and extracellular mucindeposition were reported to be associated with heterotopic bone formation in tumors[2]. Various mechanisms have been suggested although the pathogenesis of osseous metaplasia still remains unknown. The tumor cells may secrete an unknown substance that stimulates bone formation. The largest case review (52 cases) of osseous metaplasia in the gastrointestinal tract (excluding liver and pancreas) was by Ansari et al[11] in 1992. In this review, the mean subject age was 55 years, and the diagnosis in 47 of the 52 cases was that of an adenocarcinoma. The majority of cases were documented in the colon, the most common site being the rectum (21/52 cases). Osseous metaplasia seemed to occur more frequently in the primary tumor. Histologically, both benign and malignant lesions with osseous metaplasia were commonly seen with the presence of mucin production and extravasation. On the other hand, benign lesions with osseous metaplasia were often seen with a histological background of active chronic inflammation and/or ulceration[2].
From the review of the literature, all of the polyps were larger than 10 mm in diameter, 55.6% showed inflammatory changes, and 62.5% were detected in the rectum. Persistent inflammation may also play a role in osseous metaplasia in benign colonic lesions. Osteogenic stimulation was considered to be a result of the inflammatory process. Our inflammatory polyp was located in the rectum, and composed of inflammatory granulation tissues with numerous capillaries and marked acute and chronic inflammatory cells infiltration. The pathogenesis could, therefore, be a reactive change stimulated by the repeated local trauma, or be a peculiar characteristic of the rectal mucosa itself. Clinically, the presence of the metaplastic bone seems to be innocent.
In conclusion, we have reported an extremely rare case of heterotopic bone formation in a rectal inflammatory polyp where persistent inflammation may also play a role in the pathogenesis of osseous metaplasia.
Peer reviewer: Hugh J Freeman, Professor, MD, CM, FRCPC, FACP, Department of Medicine, University of British Columbia, UBC Hospital2211 Wesbrook Mall, Vancouver, BC V6T 1W5, Canada
| 1. | Van Patter HT, Whittick JW. Heterotopic ossification in intestinal neoplasms. Am J Pathol. 1955;71:73-91. |
| 2. | Haque S, Eisen RN, West AB. Heterotopic bone formation in the gastrointestinal tract. Arch Pathol Lab Med. 1996;120:666-670. |
| 3. | Sperling MH, Friedman CJ. Osseous metaplasia in a benign colon polyp. Gastrointest Endosc. 1981;27:198-199. |
| 4. | Castelli MF, Roberts J. Ossification in a benign rectal polyp. Am J Gastroenterol. 1992;87:543-544. |
| 5. | Groisman GM, Benkov KJ, Adsay V, Dische MR. Osseous metaplasia in benign colorectal polyps. Arch Pathol Lab Med. 1994;118:64-65. |
| 6. | Cavazza A, Sassatelli R, De Marco L. [Bone metaplasia in adenomatous intestinal polyp. Report of a case and review of the literature]. Pathologica. 1996;88:511-513. |
| 7. | McPherson F, Maldonado M, Truitt CA, Mamel JJ, Morgan MB. Metaplastic ossification of a benign colonic polyp: case report. Gastrointest Endosc. 1999;49:654-656. |
| 8. | Rothstein RD, LiVolsi VA. Metaplastic ossification of a benign colonic polyp. Gastrointest Endosc. 2000;51:254. |
| 9. | Al-Daraji WI, Abdellaoui A, Salman WD. Osseous metaplasia in a tubular adenoma of the colon. J Clin Pathol. 2005;58:220-221. |
| 10. | White V, Shaw AG, Tierney GM, Lund JN, Semeraro D. Osseous metaplasia in an ulcerating tubular adenoma of the colon: a case report. J Med Case Reports. 2008;2:130. |
| 11. | Ansari MQ, Sachs IL, Max E, Alpert LC. Heterotopic bone formation in rectal carcinoma. Case report and literature review. Dig Dis Sci. 1992;37:1624-1629. |