Published online Jan 16, 2025. doi: 10.4253/wjge.v17.i1.101534
Revised: December 2, 2024
Accepted: December 27, 2024
Published online: January 16, 2025
Processing time: 120 Days and 0.8 Hours
Bouveret’s syndrome is a rare (1%-4%) form of cholelithiasis characterized by gastric outlet obstruction. It presents mainly in elderly women with nausea, vomiting, and abdominal pain. On physical examination, common findings include dehydration signs such as tachycardia, decreased urine output, abdo
A 60-year-old male patient presented with a three-day history of nausea, vomiting, upper abdominal pain, and loss of appetite. An upright abdominal X-ray revealed a gas shadow in the intrahepatic and extrahepatic bile ducts. Endos
This case highlights the importance of timely diagnosis and adaptable endoscopic and surgical approaches for effectively managing Bouveret’s syndrome.
Core Tip: Bouveret’s syndrome is a rare form of cholelithiasis leading to gastric outlet obstruction. Diagnosis is confirmed through imaging, particularly abdominal computed tomography, with Rigler's triad serving as a key diagnostic indicator. Endoscopic removal of the gallstone is the first-line treatment, but surgery is required if endoscopic methods fail, especially in cases with severe adhesions. In this case, a 60-year-old male had successful endoscopic stone removal. Laparotomy was later performed for fistula repair and cholecystectomy after laparoscopy failed. This case highlights the importance of early diagnosis and flexible treatment, combining endoscopy and surgery for the best outcomes.
- Citation: Yang Y, Zhong DF. Cholecystogastric fistula presenting as pyloric obstruction - a Bouveret’s syndrome: A case report. World J Gastrointest Endosc 2025; 17(1): 101534
- URL: https://www.wjgnet.com/1948-5190/full/v17/i1/101534.htm
- DOI: https://dx.doi.org/10.4253/wjge.v17.i1.101534
Bouveret’s syndrome is a rare but serious condition caused by gallstones migrating through a cholecystoenteric fistula and obstructing the gastric outlet, resulting in intestinal ileus[1]. Typically, in elderly patients with a history of cho
A 60-year-old male patient presented with a three-day history of nausea, vomiting, upper abdominal pain, and loss of appetite.
The patient experienced nausea and vomiting for the past three days. He was vomiting gastric contents without blood and experienced upper abdominal pain. The patient reported no fever, chills, diarrhea, hematemesis, pruritus, or melena.
The patient’s past medical history included diabetes.
The patient’s personal and family history did not indicate any factors relevant to his current illness.
On physical examination, the abdomen was soft, and slight tenderness was observed in the epigastric region.
Laboratory tests revealed high levels of C-reactive protein (37.67 mg/L), a white blood cell count of 8.97 × 109/L with neutrophilia (69.90%), total bilirubin level of 21.9 μmol/L, direct bilirubin levels of 4.3 μmol/L, alanine aminotransferase level of 20.8 U/L, and aspartate aminotransferase level of 23 U/L.
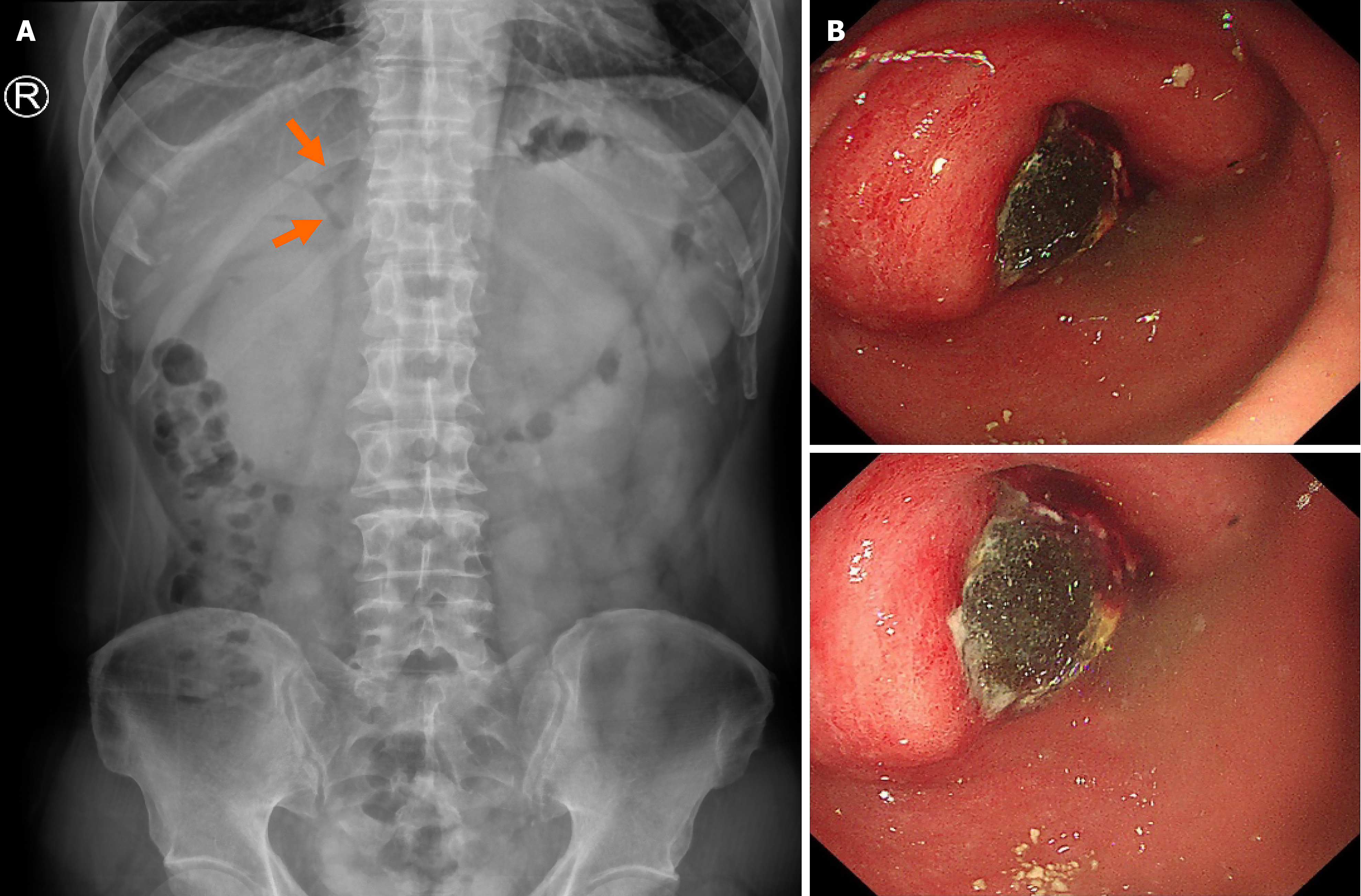
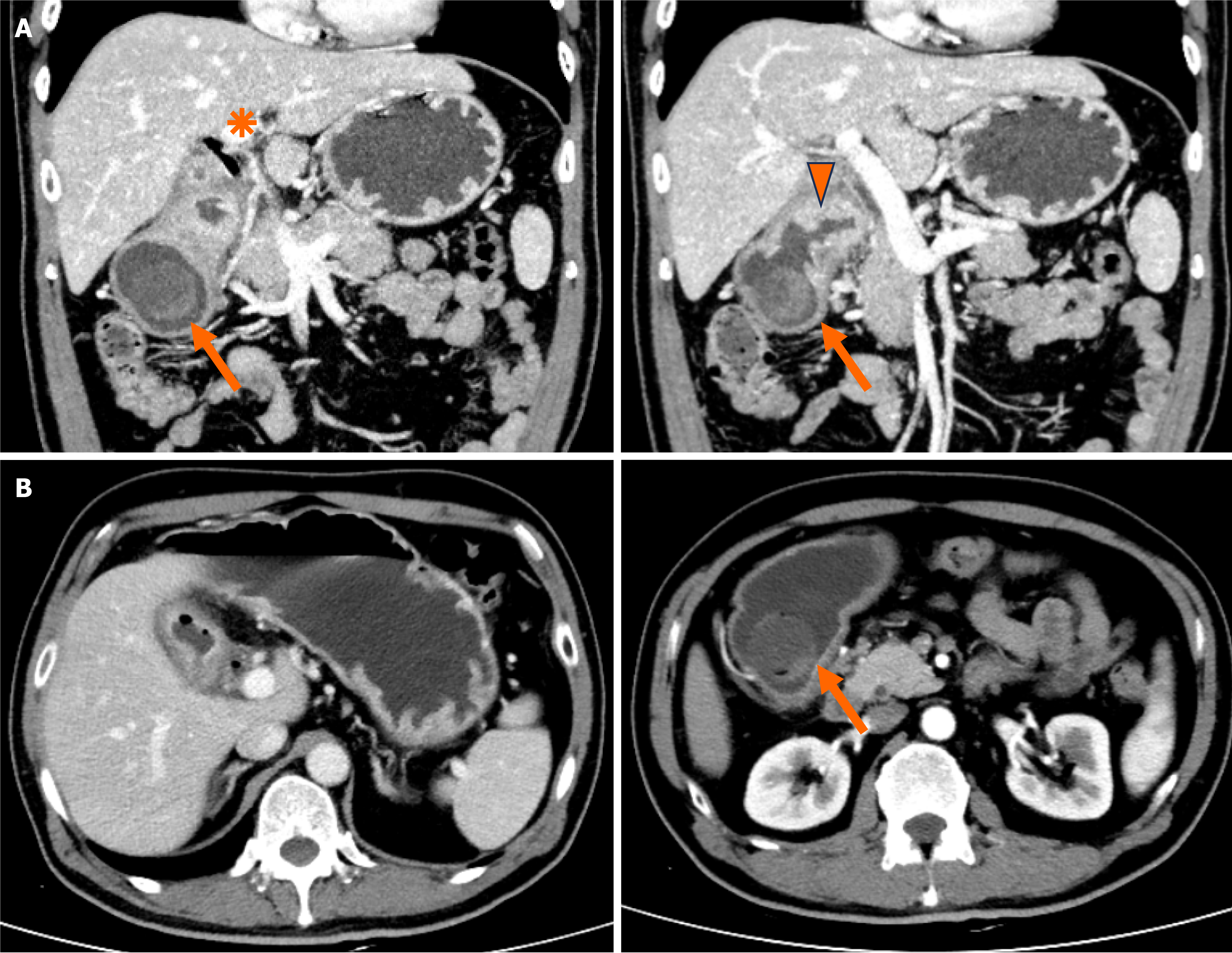
An upright abdominal X-ray revealed a gas shadow in the intrahepatic and extrahepatic bile ducts. Esophagogastroduodenoscopy revealed a brown and black stone measuring approximately 3030 mm in diameter in the gastric pylorus, incompletely obstructing the gastric outlet (Figure 1). An abdominal computed tomography (CT) scan revealed a circular low-density shadow measuring approximately 3028 mm in size in the antrum of the stomach, and no obvious enhancement was observed in the enhanced scan. A cystic low-density shadow in the gallbladder fossa area was observing communicating with the pyloric part of the stomach. The gastric antrum wall and gallbladder wall were edematous and thickened (Figure 2).
On the basis of the findings described above, Bouveret’s syndrome was considered a possible diagnosis.
Endoscopic removal of the stone was successful. The stone was fragmented and removed piecemeal using a crushing basket. Laparoscopy was attempted three weeks later; however, severe tissue adhesions were present. The procedure was converted to a laparotomy, and fistula repair and cholecystectomy were performed. During the surgery, we encountered several challenges. First, the presence of a biliary-enteric fistula complicated the procedure, as inflammation and chronic fistulous communication had altered its anatomy. To address this, we carefully repaired the fistula, ensuring minimal disruption to surrounding structures to avoid additional complications. Additionally, the patient had significant adhesions due to chronic biliary disease, which made dissection challenging. These adhesions involved the gallbladder, bile ducts, and intestines, requiring meticulous separation to prevent injury to critical structures. In areas with severe adhesions, we employed careful dissection techniques and, when necessary, adjusted our surgical strategy to minimize trauma and ensure safe removal of the gallstone and restoration of normal anatomy.
The patient recovered well and was discharged on the 9th day following surgery. The patient returned to the outpatient clinic for follow-up, and no further concerns were noted.
Bouveret’s syndrome is a rare form of cholelithiasis characterized by gastric outlet obstruction due to a gallstone entering the digestive tract. Gallstones may migrate via fistulas into various parts of the gastrointestinal tract, including the ileocecal region (50%-90%), proximal jejunum and ileum (20%-40%), and the colon, stomach and duodenum (< 5%)[2]. The risk factors for Bouveret’s syndrome include female sex, advanced age (> 70 years), gallstone diameter > 2.5 cm, and postoperative alterations in gastrointestinal anatomy[3,4]. Approximately 70% of patients present with nausea/vomiting (86%) and abdominal pain (70%)[4]. Imaging examinations may reveal Rigler's triad: Gastric dilation, pneumobilia, and an ectopic gallstone[4]. In the differential diagnosis of Bouveret syndrome, several conditions presenting with similar symptoms, such as upper gastrointestinal obstruction or gastrointestinal bleeding, must be considered. These include gallstone ileus, where a gallstone migrates into the intestine, typically causing small bowel obstruction rather than duodenal obstruction, which can be differentiated through imaging. Peptic ulcer disease, especially with complications like perforation or gastric outlet obstruction, shares symptoms such as epigastric pain and vomiting but can be distinguished through endoscopy and imaging. Early recognition of Bouveret’s syndrome is essential, as delayed diagnosis and treatment can lead to significant complications. Given the condition's rarity and complexity, a multidisciplinary approach is recommended to ensure accurate diagnosis and optimal management, especially in elderly patients with multiple comorbidities.
Bouveret’s syndrome can be treated endoscopically, surgically, or using a combination of two methods. Endoscopy can aid in both diagnosis and treatment. Generally, endoscopy and lithotripsy modalities are recommended first. Smaller stones (< 2-3 cm) can be effectively removed endoscopically with nets or baskets[1]. Larger stones are difficult to remove endoscopically, often necessitating lithotripsy techniques such as extracorporeal shockwave, electrohydraulic lithotripsy, and laser lithotripsy[5]. Endoscopic procedures are associated with complications such as intestinal wall bleeding, perforation, or distal gallstone ileus due to stone fragments. However, endoscopic visualization of the stone is possible in only approximately 69% of cases, as the stone may be embedded in the submucosa[6]. The success rate of endoscopic stone retrieval is reported to be no higher than 58%[5]. If endoscopic therapy fails or does not allow complete clearance of all stones, surgery remains the main treatment option. Common surgical procedures include enterolithotomy, fistula repair and cholecystectomy and can be performed in either one or two stages depending upon the patient’s physical condition, location of the obstruction and size of the stone and fistula. Enterolithotomy, cholecystectomy, and repair of the concomitant fistula should be considered primarily for younger, healthier patients, where the risk of disease recurrence outweighs the potential perioperative risks[1]. In this case, the stone was successfully removed endoscopically. Three weeks later, fistula repair and cholecystectomy were performed. The patient experienced a smooth recovery and is in good health at the time of reporting. Follow-up care for patients with Bouveret’s syndrome involves monitoring for recurrence of symptoms such as nausea, vomiting, or abdominal pain, as well as ensuring the healing of any fistulas or gastrointestinal lesions. Nutritional support is important, particularly for older patients who may have dehydration or malnutrition. Regular imaging, including CT or magnetic resonance imaging, helps detect the recurrence of gallstones or complications. Ongoing assessment ensures that the patient remains free of symptoms and maintains optimal recovery after treatment.
Bouveret’s syndrome is a rare condition characterized by gastric outlet obstruction with a high mortality rate. Timely diagnosis and a personalized treatment are essential for the successful management of this disease.
The authors express their sincere gratitude to the participants for their assistance and willingness to be part of this study.
| 1. | Caldwell KM, Lee SJ, Leggett PL, Bajwa KS, Mehta SS, Shah SK. Bouveret syndrome: current management strategies. Clin Exp Gastroenterol. 2018;11:69-75. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 84] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 2. | Khuwaja S, Azeem A, Semkhayev BA, Afthinos J, Guttmann S. Bouveret Syndrome: When a Stone Cannot Pass the Pylorus. ACG Case Rep J. 2019;6:e00176. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Kalwaniya DS, Arya SV, Guha S, Kuppuswamy M, Chaggar JG, Ralte L, Chejera R, Sharma A. A rare presentation of gastric outlet obstruction (GOO) - The Bouveret's syndrome. Ann Med Surg (Lond). 2015;4:67-71. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Cappell MS, Davis M. Characterization of Bouveret's syndrome: a comprehensive review of 128 cases. Am J Gastroenterol. 2006;101:2139-2146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 148] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 5. | Dumonceau JM, Devière J. Novel treatment options for Bouveret's syndrome: a comprehensive review of 61 cases of successful endoscopic treatment. Expert Rev Gastroenterol Hepatol. 2016;10:1245-1255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 6. | Watson RS, Folkers TE, Van Every MJ. A Multidisciplinary Approach to Management of Bouveret Syndrome. Clin Med Res. 2018;16:73-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |