Published online Jul 16, 2024. doi: 10.4253/wjge.v16.i7.432
Revised: May 30, 2024
Accepted: June 27, 2024
Published online: July 16, 2024
Processing time: 66 Days and 23.2 Hours
Portal vein injury is an uncommon complication of endoscopic retrograde cholangiopancreatography (ERCP), for which stent malpositioning in the portal vein is very rare and can lead to fatal events. We report a case of biliary stent migration to the portal vein and a novel method for its safe removal under the guidance of portal angiography. Moreover, we reviewed the literature and summarized reports on the identification and management of this condition.
A 59-year-old woman with pancreatic cancer presented with abdominal pain and a high fever 20 days after the placement of two plastic biliary stents under the guidance of ERCP. Blood cultures and laboratory tests revealed sepsis, which was treated with antibiotics. A contrast-enhanced computed tomography scan reveal
The combination of endoscopic and angiographic techniques allowed uneventful management of stent malposition in the portal vein.
Core Tip: Stent malpositioning in the portal vein is a very rare complication of endoscopic retrograde cholangiopancreatography and can be fatal. We report a case of stent migration into the portal vein and a novel method for its safe removal under the surveillance of portal angiography. After reviewing the literature, we summarized the characteristics of reported cases, including predisposing factors and manifestations of stent malposition in the portal vein, and other treatments, such as immediate stent removal, metal stent placement in the bile duct, urgent surgery, and covered stent placement in the portal vein.
- Citation: Wu R, Zhang F, Zhu H, Liu MD, Zhuge YZ, Wang L, Zhang B. Recognition and management of stent malposition in the portal vein during endoscopic retrograde cholangiopancreatography: A case report. World J Gastrointest Endosc 2024; 16(7): 432-438
- URL: https://www.wjgnet.com/1948-5190/full/v16/i7/432.htm
- DOI: https://dx.doi.org/10.4253/wjge.v16.i7.432
Endoscopic retrograde cholangiopancreatography (ERCP) is widely used in the diagnosis and management of pancreaticobiliary diseases. Portal vein injury is a rare complication of ERCP that can occur at any step during or after the procedure, including cannulation, sphincterotomy, stent placement, and nasobiliary drainage[1-5]. Stent malpositioning in the portal vein is extremely rare and may lead to fatal complications such as venous air embolism and fatal hemorrhage. This report describes a case of biliary stent migration into the portal vein and a novel method for its safe removal under the guidance of portal angiography. After searching PubMed for previously reported cases, we reviewed the literature on the identification and management of this complication[3,4,6-12].
A 59-year-old woman suffered from abdominal pain and a high fever for 10 days.
Ten days prior, the patient suffered a sudden onset of fever (41.0 °C) and abdominal pain. A 6-day course of antibiotics consisting of cefoperazone, sulbactam and metronidazole was undertaken at the local hospital, but the symptoms did not improve. Before admission, the patient presented with a fever fluctuating between 37.5 °C and 39.0 °C with chills. She had no history of hematemesis, melena, nausea, vomiting, diarrhea, or dark urine.
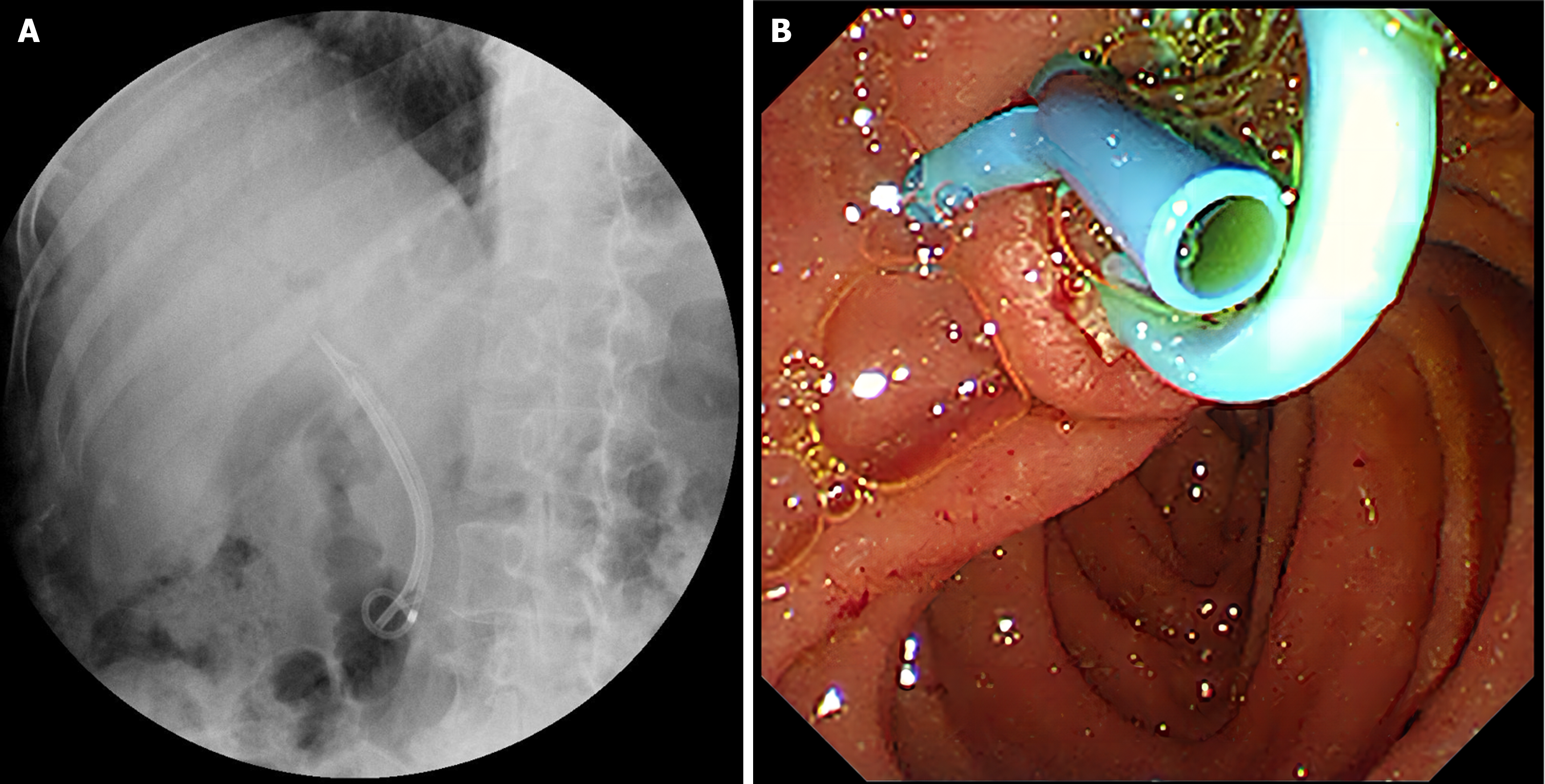
She was diagnosed with unresectable pancreatic cancer 6 months prior and had a history of duodenal ulceration. She underwent ERCP for biliary drainage at the time of cancer diagnosis 6 months prior and has since received 4 months of immunotherapy, 5 months of chemotherapy and 50 Gy/10 F local radiotherapy. One month prior, she underwent ERCP for replacement of plastic biliary stents (an 8.5 F, 7 cm single external flap stent and a 7 F, 7 cm single pigtail stent), as shown in Figure 1.
The patient’s personal and family history was not significant.
Body temperature, 37.5 °C; blood pressure, 108/69 mmHg; heart rate, 98 beats/min; respiratory rate, 20 breaths/min. Physical examination revealed moderate tenderness in the right upper quadrant without rebound tenderness and a negative Murphy’s sign.
The relevant laboratory findings were as follows: White blood cell count, 11800/mm3; hemoglobin level, 9.00 g/dL; alanine aminotransferase level, 54.00 IU/L; total bilirubin level, 0.35 mg/dL; alkaline phosphatase level, 286.80 U/L; lactate dehydrogenase level, 327.00 U/L; and albumin level, 2.86 g/dL. The serum amylase level was normal. Blood culture revealed Eshcerichia hermannii and Enterococcus faecalis. Her C-reactive protein level was 212.90 mg/L, and her procalcitonin level was 2.90 ng/mL.
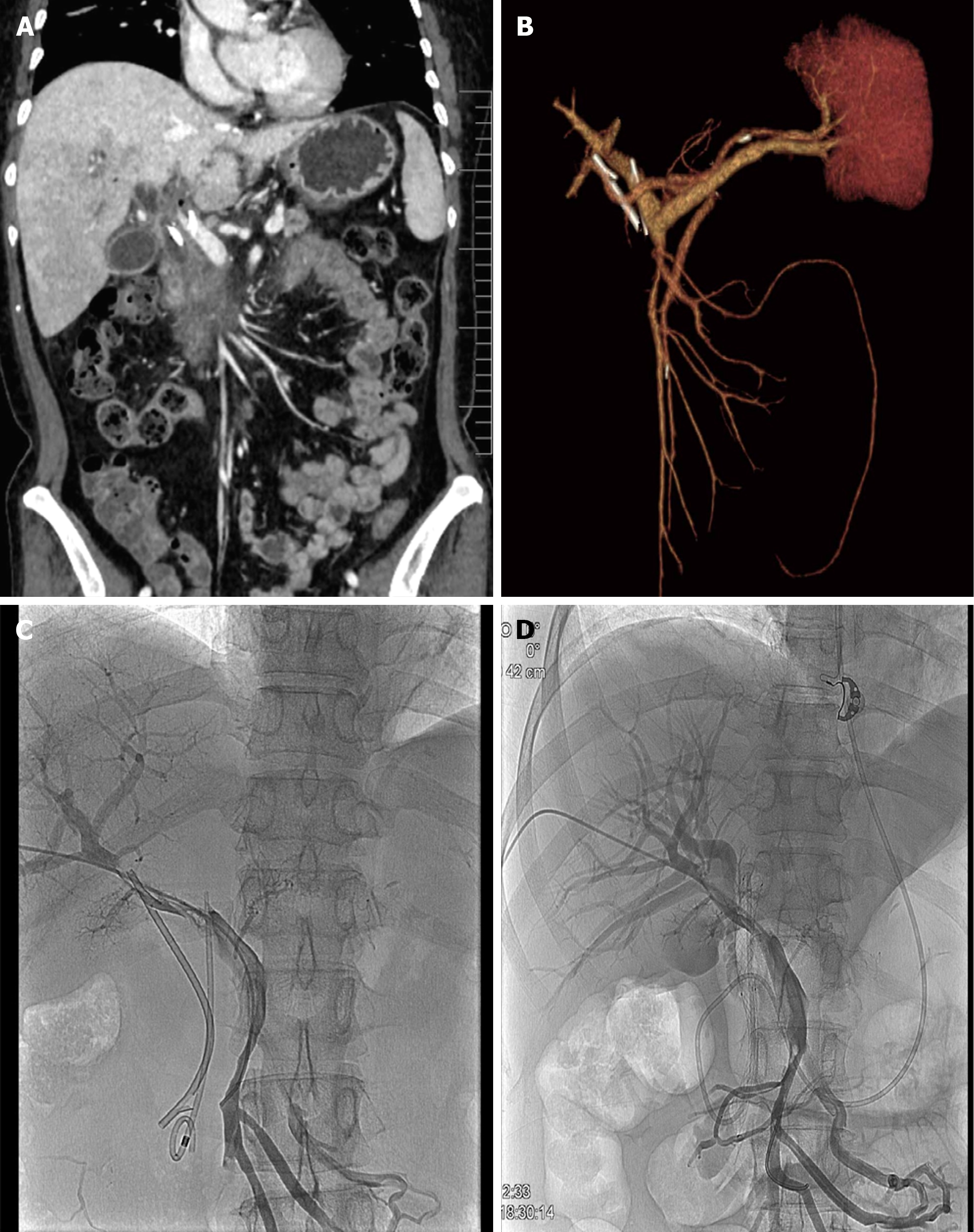
A contrast-enhanced computed tomography (CT) scan revealed a biliary stent in the main portal vein (Figure 2A and B).
The diagnosis was portal vein injury caused by biliary stent malposition and consequent sepsis.
The patient’s temperature returned to normal after imipenem treatment, according to the drug susceptibility test. After discussion with a multidisciplinary team, we decided to remove the stent endoscopically under the guidance of portal angiography. During the procedure, portal angiography was first performed to visualize the portal vein and its relationship to the stents. As shown in Figure 2C, the single pigtail stent separated from the single flap stent and migrated straight up the spine into the portal vein. The two stents were then carefully removed, and there was no obvious bleeding from the papilla. An uncovered self-expanding metal stent was then placed in the common bile duct for drainage. Finally, repeated portal angiography revealed no active bleeding (Figure 2D), and endoscopic nasobiliary drainage was perfor
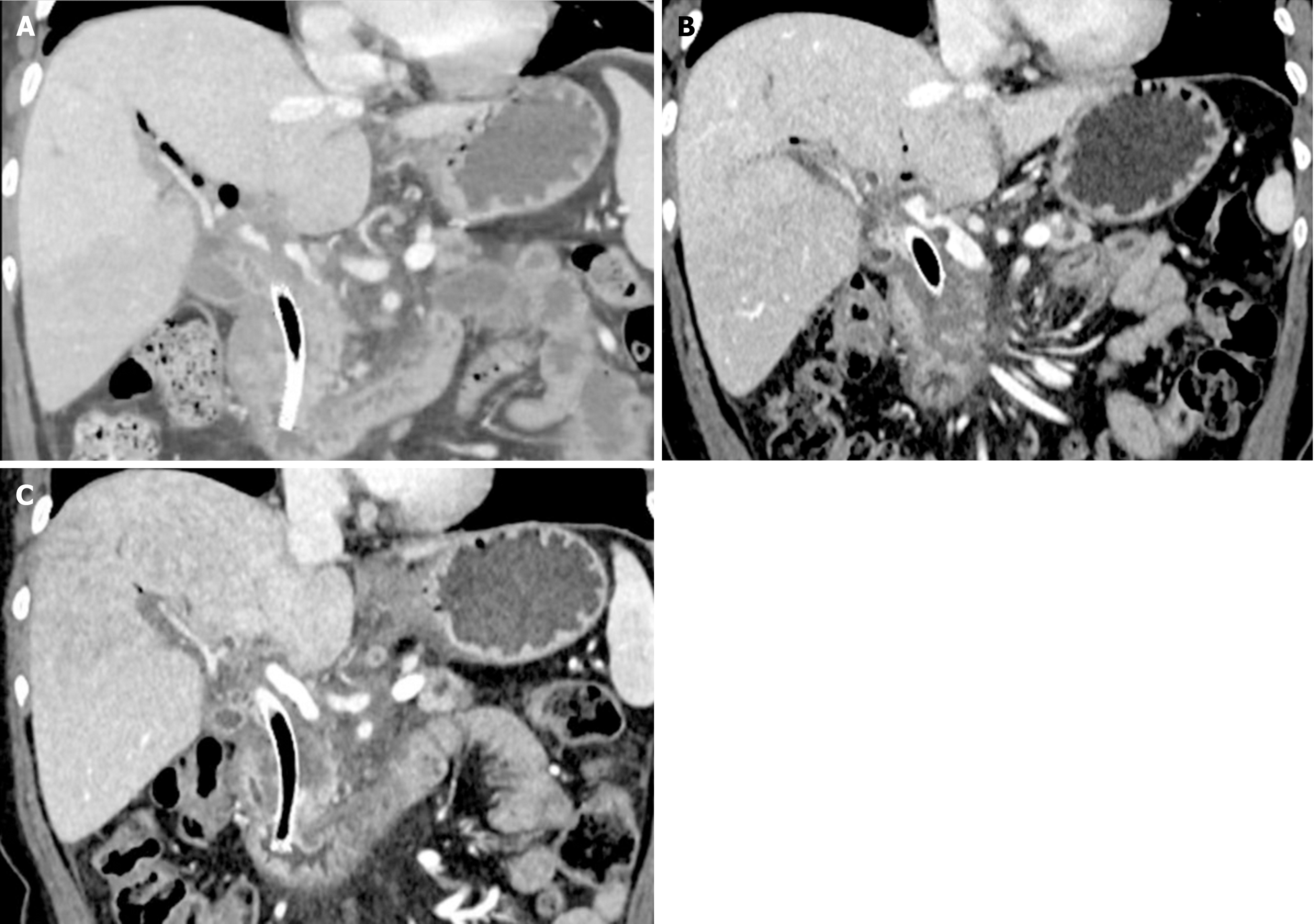
After the procedure, the patient had a transient fever that did not recur. The patient did not complain of abdominal pain, melena, nausea or vomiting, and her amylase level after ERCP was normal. Four days after ERCP, a repeat contrast-enhanced CT scan revealed portal vein thrombosis (Figure 3A), and the nasobiliary drain was removed. The patient did not receive anticoagulant therapy due to duodenal ulcers and fecal occult blood. The thrombus was noticeably reduced in size at the first month follow-up (Figure 3B) and was no longer present at the third month follow-up (Figure 3C). The patient continued to receive chemotherapy and experienced an uneventful 6-month follow-up period.
Portal vein injury is a rare complication of ERCP and can result in bleeding, sepsis, portal vein thrombosis and air embolism[13-18]. Among all types of portal vein injury, stent malpositioning into the portal vein is very rare and comparatively severe, with only a few cases reported in the literature (Table 1). Stent malpositioning tended to occur in patients with cholangitis or tumors, probably due to tissue fragility caused by inflammation or tumor invasion. In the case of malignancy, combining chemotherapy or adding radiotherapy may also increase the fragility of the tissue. In these cases, difficult cannulation and sphincterotomy often accompany the procedure and therefore increase the risk of stent malpositioning into the portal system. Stents may enter the portal vein during the procedure or migrate into the portal vein days or months after the procedure. During ERCP, there are several signs that a stent may have been placed in the portal vein. First, the endoscopist may feel resistance when placing the catheter or stent. Second, the injected contrast material may rapidly flow toward the liver and disappear within seconds. Third, the stent appears “straight up” along the portal vein and parallel to the spine on X-ray. Figure 2A clearly shows the position of the migrated stent in relation to the other well-positioned stent in the CBD. Finally, the aspiration of blood helps to confirm whether the cannula entered the portal vein. After ERCP, if stent malpositioning is not immediately detected during the procedure, patients may present with abdominal pain, fever, melena and unimproved jaundice. Abdominal ultrasound and CT usually help clinicians confirm the diagnosis. In this particularly rare case, the stent was correctly placed during the procedure and functioned normally for one month until it migrated to the portal vein. The patient presented with fever and abdominal pain, and the CT scan clearly showed the migration of the stent. It was reasonable to assume that the stent migrated after penetrating the fragile bile duct wall because of tumor growth, chemotherapy and radiotherapy. In addition, tension from the pigtail can easily cause perforation and induce stent migration.
| Ref. | Gender, age | Indication for ERCP | Procedure | Stent | Clinical manifestation | Treatment | Follow-up | Outcome |
| Stableforth et al[6], 2011 | Male, 73 | Pancreatic cancer | PBS replacement | 7-Fr, 10-cm straight | Consistent jaundice; Brisk bleeding after removal of the stent; Filling of the portal vein and rapid washout of contrast material; confirmed by CT | PBS left in situ; metal stent placement via PTC | 2 months | No complications |
| Miloudi et al[7], 2011 | Female, 60 | Benign narrowing of the CBD after transplantation | PBS replacement | 10-Fr, 10-cm | Difficult insertion of the new PBS; Fever and abdominal pain shortly after ERCP; Confirmed by abdominal ultrasound and CT | Surgery to remove the prosthesis, close the fistula, repair the portal vein, and develop hepatico-jejunal anastomosis | Several days | Uneventful |
| Leung et al[8], 2012 | Female, 10 | Recurrent pancreatitis | Pancreatic sphincterotomy, pancreatic stent placement | 3-Fr, 6 cm, pigtail | Fever, abdominal pain, and elevated amylase; Confirmed by ultrasound and CT | Remove the stent by ERCP on the 3rd postoperative day | 3 months | Portal vein thrombosis gradually resolved |
| Dawwas et al[9], 2013 | Male, 69 | CBD stones | Difficult cannulation, biliary sphincterotomy, PBS placement | 7-Fr, 4-cm, double pigtail | Bleeding after removal of previous stent, and faint, rapidly dissipating, biliary-like opacification on contrast injections | Abandon the procedure immediately | 2 months | Gas and thrombosis in the portal vein gradually resolved |
| So et al[10], 2015 | Male, 55 | Hilar invasion of hepatocellular carcinoma | PBS replacement | NA | Recurrent melena and bacteremia; Exacerbated bleeding after removing the stent; Cholangiography revealed leakage of contrast dye into the portal vein | Placing fully covered self-expandable metal stent in the bile duct | Several days | Recovering from recurrent bacteremia and bleeding |
| Russo et al[11], 2017 | Female, 39 | Acute cholangitis | Biliary sphincterotomy, failed sweeping of stones by a ballon, and PBS placement | 7-Fr, 7-cm | Resistance on stent placement, bleeding upon stent deployment | PBS left in situ, emergent laparotomy to repair the injury and T-tube placement | Several days | Resolve from the surgery |
| João et al[12], 2022 | Female, 60 | Biliary anastomotic stenosis after liver transplantation | Difficult cannulation, biliary sphincterotomy, balloon dilation, PBS placement | Two 8.5-Fr, 9.0-cm | Spurting hemorrhage when removing the stent | Endoscopic removal of stent, percutaneous transhepatic fully covered self-expanded metal stent in the portal vein | 1 month | Clinically stable, no bleeding relapse |
| Lin et al[3], 2023 | Male, 34 | CBD stones, cholangitis | Difficult cannulation, sphincterotomy, balloon dilation, PBS placement | 7-Fr | Hemobilia upon inserting the stent; Confirmed by CT scan | Surgery: Cholecystectomy and CBD stones removement, endoscopic removal of stent | 9 months | Uneventful |
| Taşar et al[4], 2023 | Female, 54 | CBD stones, cholangitis | Difficult cannulation, sphincterotomy, stone extraction, PBS placement | 10-Fr, 7-cm | Hemorrhage, fever and persistent jaundice; Confirmed by CT scan | Laparoscopic exploration with ERCP | Several months | Chronic portal thrombus |
The table shows several treatment options, including immediate stent removal, metal stent placement in the bile duct, emergency laparotomy and surgical repair, and the placement of a fully covered metal stent in the portal vein via a percutaneous or transjugular approach. In this case, the stents were removed endoscopically under the guidance of portal angiography. In the event of portal bleeding, covered, self-expanding metal stents could be delivered into the portal vein and expanded to close the fistula and stop the bleeding. This method was safer than direct endoscopic removal of the stent for timely management of bleeding and less invasive than surgery.
Of the cases that have been reported, few rare cases of fatal bleeding after stent migration to the portal vein or stent removal from the portal vein have been reported, and in most cases, this can be managed uneventfully. There are several explanations. First, the pressure in the portal vein (5-10 mmHg) is lower than that in the bile duct (10-15 mmHg), so blood cannot flow strongly against the pressure gradient[16]. Second, the formation of portal vein thrombosis can occlude the vessel and control bleeding. Third, the portal vein and common bile duct pass together within the hepatoduodenal ligament, and after stent removal, these tissues may shrink to seal the site of injury. However, portal hypertension, large French stents and coagulation disorders can increase the risk of fatal bleeding.
To avoid stent migration to the portal vein, endoscopists must proceed with caution in patients with cancer or cholangitis, especially if cannulation and sphincterotomy are difficult. The sensation of resistance when passing the catheter or stent, the rapid washing out of contrast agent, and the aspiration of blood will reveal portal vein injury, thus stopping the procedure without force is critical. If stent migration to the portal vein occurs, portal vein angiography or surgery can be considered, and the stent can be removed endoscopically to manage potentially fatal bleeding.
In conclusion, we report a case of stent migration into the portal vein after ERCP in a patient who presented with fever and abdominal pain after pancreatic cancer diagnosis. The combination of endoscopic and angiographic techniques allowed uneventful management. Literature was reviewed for reported cases in which this rare complication was identified and managed.
| 1. | Nakahara K, Komatsu T, Matsumoto N. Successful biliary stenting after portal vein cannulation during endoscopic retrograde cholangiopancreatography. J Hepatobiliary Pancreat Sci. 2022;29:e61-e62. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 2. | Espinel J, Pinedo ME, Calleja JL. Portal vein filling: an unusual complication of needle-knife sphincterotomy. Endoscopy. 2007;39 Suppl 1:E245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Lin PY, Wang SH, Tian YF, Chen MJ, Sun DP, Shiau J, Ong KH. Incidentally portal vein penetration during cannulation in endoscopic retrograde cholangiopancreatography: a case report. J Surg Case Rep. 2023;2023:rjad298. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 4. | Taşar P, Kılıçturgay SA. Portal vein injury following endoscopic retrograde cholangiopancreatography: A case report. Ulus Travma Acil Cerrahi Derg. 2023;29:443-447. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 5. | Furuzono M, Hirata N, Saitou J, Nakaji S. A rare complication during ERCP and sphincterotomy: placement of an endoscopic nasobiliary drainage tube in the portal vein. Gastrointest Endosc. 2009;70:588-590. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Stableforth WD, Pathmakanthan S, Holt A, Haydon G, Freshwater D, Mangat K. Iatrogenic portobiliary fistula complicating endoscopic stenting of a pancreatic cyst, with possible carcinoma: a case report. Gastrointest Endosc. 2011;73:630-632. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Miloudi N, Hefaiedh R, Mzoughi Z, Ben Abid S, Mestiri H, Ghorbel A, Khalfallah T. Accidental insertion of biliary endoprosthesis in the portal vein: a case report. Clin Res Hepatol Gastroenterol. 2011;35:144-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 8. | Leung WD, Parashette KR, Molleston JP, Sherman S. Pancreatic stent migration into the portal vein causing portal vein thrombosis: a rare complication of a prophylactic pancreatic stent. Pancreatology. 2012;12:463-465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Dawwas MF, Oppong KW, John SK, Vallance AE, French JJ, Scott J, Nayar MK. Endoscopic ultrasound diagnosis of an ERCP-related portobiliary fistula. Endoscopy. 2013;45 Suppl 2 UCTN:E214-E216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 10. | So H, Song TJ, Lee D, Jung K, Gong EJ, Oh D, Lee SS. Endoscopic treatment of recurrent bleeding from a portobiliary fistula with a fully covered self-expandable metal stent. Endoscopy. 2015;47 Suppl 1:E616-E617. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Russo SM, Patel S, Abubakar I, Kahloon A, Kessler S, Lambiase L. Iatrogenic Portal Vein Injury During Biliary Stent Placement. Am J Gastroenterol. 2017;112:S1137. [DOI] [Full Text] |
| 12. | João M, Gravito-Soares M, Gravito-Soares E, Figueiredo P. Hemobilia due to porto-biliary fistula complicating endoscopic retrograde cholangiopancreatography after a recent liver transplantation. Rev Esp Enferm Dig. 2022;114:502-503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Kawakami H, Kuwatani M, Kudo T, Ehira N, Yamato H, Asaka M. Portobiliary fistula: unusual complication of wire-guided cannulation during endoscopic retrograde cholangiopancreatography. Endoscopy. 2011;43 Suppl 2 UCTN:E98-E99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Kalaitzakis E, Stern N, Sturgess R. Portal vein cannulation: an uncommon complication of endoscopic retrograde cholangiopancreatography. World J Gastroenterol. 2011;17:5131-5132. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 13] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 15. | Kawaguchi Y, Lin JC, Kawashima Y, Maruno A, Ito H, Ogawa M, Mine T. Accessory Pancreatic Duct-Portal Vein Fistula: A Rare Complication of Chronic Pancreatitis during Endoscopic Retrograde Cholangiopancreatography. Case Rep Gastroenterol. 2014;8:291-296. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 16. | Yared RA, Gkolfakis P, Lemmers A, Huberty V, Degrez T, Devière J, Blero D. Portal cavernography during endoscopic retrograde cholangiopancreatography: from bilhemia to hemobilia. Clin Endosc. 2023;56:521-526. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 17. | Tighe M, Jacobson I. Bleeding from bile duct varices: an unexpected hazard during therapeutic ERCP. Gastrointest Endosc. 1996;43:250-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 18. | Kennedy C, Larvin M, Linsell J. Fatal hepatic air embolism following ERCP. Gastrointest Endosc. 1997;45:187-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 35] [Article Influence: 1.3] [Reference Citation Analysis (0)] |